Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5241
Peer-review started: December 13, 2021
First decision: January 10, 2022
Revised: January 21, 2022
Accepted: April 3, 2022
Article in press: April 3, 2022
Published online: June 6, 2022
Processing time: 171 Days and 1.8 Hours
In 2016, the Chinese government issued the Healthy China 2030 plan, which also produced the initiative practice for health (IPFH) concept. However, people’s knowledge and awareness of the IPFH are unclear.
To investigate awareness of IPFH in the Chinese population and explore the relevant influential factors.
An internet-based self-designed questionnaire survey was used to collect respondents’ demographic characteristics and awareness of health and the IPFH from March 26 to April 18, 2020. IPFH consciousness was assessed by the scores for different related questions. The Student’s t test, the Chi-square test, and multiple logistic regression analysis were performed to analyze the differences and influencing factors.
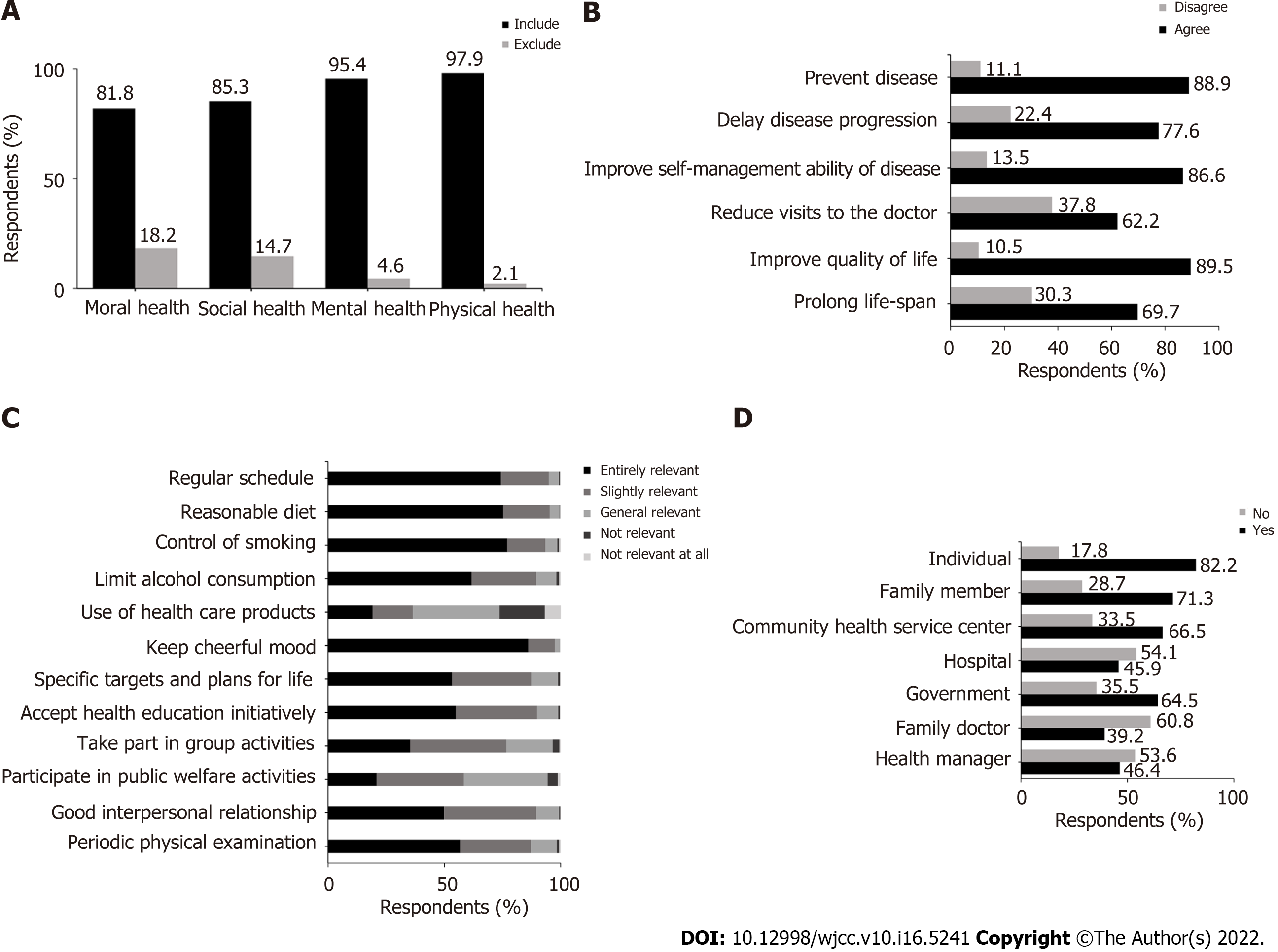
A total of 2678 valid questionnaires were collected. Of the respondents, 973 (36.3%) had heard of the IPFH concept. In addition, 89.5% of participants agreed with the view that the IPFH is beneficial to improving quality of life, and over half thought that a regular schedule, a reasonable diet, tobacco and alcohol control, a cheerful mood, specific life goals and plans, taking the initiative to accept health-related education and implement health knowledge, good interpersonal relationships, and regular physical examinations were closely related to the IPFH. The majority of respondents paid attention to their health and usually obtained health-related knowledge via social media and were also willing to promote the IPFH. Most of the participants underestimated the role of hospitals, family doctors, and health managers in promoting the IPFH. Age, monthly income, and medical-related work experience were the influencing factors for IPFH awareness.
The Chinese population has limited knowledge of the IPFH. People with strong IPFH awareness are older, earn more, and have medical-related work experience.
Core Tip: This is a survey by a self-designed questionnaire to investigate the awareness of initiative practice for health (IPFH) and related knowledge in the Chinese population. IPFH is a process whereby people take the initiative to improve health. The Chinese population has limited knowledge of the IPFH, although most citizens are concerned about health in their daily lives. Age, medical-related work experience, and monthly income are the influencing factors of IPFH awareness.
- Citation: Zhang YQ, Zhou MY, Jiang MY, Zhang XY, Wang X, Wang BG. Awareness of initiative practice for health in the Chinese population: A questionnaire survey based on a network platform. World J Clin Cases 2022; 10(16): 5241-5252
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5241.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5241
Population health is a common theme worldwide. In 2015, the United Nations published the Sustainable Development Goals (SDGs) to ensure sustainable development globally and to solve predictable challenges by 2030. The SDGs have over 100 targets in different fields, including medicine and health[1,2]. As the largest developing country with a population of over 1.4 billion, China has achieved most of the targets and has made great achievements in promoting health, such as ensuring nutrition for children, decreasing neonatal and under-5 year mortality rates as well as the maternal mortality rate, reducing physical maldevelopment of children, and extending people’s lifespan[3]. However, there are still challenges, such as industrialization and environmental problems, that threaten the health of the Chinese population, especially the aging society and the increasing burden of various age-related chronic diseases[4,5]. It is predicted that the number of people aged ≥ 65 years will be 400 million by 2050, accounting for approximately 26.9% of the total population, and the number of people aged ≥ 80 years will increase to 150 million by 2050[6].
To address health challenges effectively, countries around the world, including China, have adopted different policies[7-9]. In October 2016, the Central Committee of the Communist Party of China and the State Council released the Healthy China 2030 plan, which aims to address the challenges posed by the United Nations SDGs, as well as the accompanying economic burden, and to improve people’s health by promoting healthy lifestyles, optimizing health services, improving health security, building a healthy environment, and developing health industries by 2030[10]. The Healthy China 2030 plan aims to improve the health system of China and make China a modern and healthy country[11]. First, the focus of health services will shift from the treatment of diseases to health management and disease intervention to decrease health-related costs to some extent[12]. The Chinese government’s investment in health has continuously increased in recent decades, with nearly 70% of the investment being for treatment[4]. Additionally, the Healthy China 2030 plan is beneficial for establishing a system in which all citizens participate on a government-led basis and for improving health awareness and enhancing the concept of taking responsibility for one’s own health. Furthermore, the plan may be conducive to promoting the rapid development of health-related industries such as health monitoring and management consulting services, thus promoting economic development. In addition, by taking the opportunity that the plan represents, traditional Chinese medicine will develop rapidly.
Health is an inevitable requirement for promoting all-around human development, and it is a basic condition for economic and social development. Different people have different understandings of health. The World Health Organization definition of health-“a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity”-mainly includes four different dimensions, the physical, the psychological, the socially adaptable, and the moral, and it has been accepted worldwide[13]. The “initiative practice for health” (IPFH) concept derives from the Healthy China 2030 blueprint. IPFH is a process in which people take the initiative to gain health-related knowledge, improve their lifestyle, and ensure their health status. It is based on health management and emphasizes the long-term continuous and dynamic tracking of the individuals’ entire life cycle behavioral systems as well as comprehensive detection, assessment, effective intervention, and continuous follow-up services for individual or group health conditions and their risk factors affecting health. It highlights the active participation of individuals in personal health management and citizen participation in the healthy development of China. It encourages individuals to find personal ways and to acquire effective knowledge to promote modifiable health-related behaviors in terms of diet, exercise, society, and mentality to enable healthier lives.
The Chinese government has made great efforts to promote the Healthy China 2030 plan and IPFH. However, few surveys have explored people’s awareness, knowledge, and understanding of IPFH. Therefore, we investigated the relevant knowledge and behaviors related to IPFH as well as the attitudes of people using a self-designed questionnaire to improve the promotion of IPFH and indirectly improve the health of all people.
Based on the literatures and suggestions of experts in health management, epidemiology, and clinical medicine, a self-designed questionnaire including 49 questions was compiled based on the purpose of this research after the group discussion and the preliminary investigation of 55 samples. The survey items mainly covered four parts: (1) Demographic characteristics and socioeconomic status, including respondents’ gender, place of residence, age, educational level, work experience, personal income per month, height, weight, body mass index (BMI), etc; (2) knowledge related to health and IPFH; (3) health-related behaviors; and (4) the will to promote IPFH.
IPFH awareness was assessed in terms of five aspects: The view on the aging population in China; knowing about IPFH; the frequency with which the respondent receives health-related science information; the frequency of health consultations; and the will to promote IPFH. The IPFH awareness was evaluated based on the sum of the scores on these five aspects. According to the results of the preliminary investigation, respondents were considered to have strong IPFH awareness if the score was ≥ 8 points (75% of the median). Otherwise, they were considered to have weak IPFH awareness.
The self-designed electronic questionnaire was administered on an online crowdsourcing platform from March 26 to April 18, 2020, and it was sent to Moments and WeChat groups in the form of network links by researchers who voluntarily transmitted the links. Before starting the survey, the aims of the questionnaire were shown, informed consent was obtained, and people could refuse to participate. All information was guaranteed to be confidential. The content could not be changed after completion.
The content was exported from the network platform. Demographic characteristics are represented as the mean ± standard deviation for continuous variables based on a normal distribution; otherwise, the median (P25-P75) was used. The differences in continuous variables between the two groups were tested by a Student’s t-test or Mann–Whitney U test. Categorical variables are represented as n (%), and the differences between the two groups were tested by the χ2 test or Fisher’s exact test. Multiple logistic regression analysis was performed, and the odds ratios (ORs) and 95% confidence intervals (CIs) of the variables are reported. Data analysis and analysis of the credibility of the questionnaire were performed using SPSS for Windows version 25.0 (IBM Corp., Armonk, NY, United States). All reported P values are two-tailed, and P < 0.05 was considered statistically significant.
This survey was approved by the Academic Ethics Committee of the Sanbo Brain Hospital, Capital Medical University. This survey was voluntary, and residents could refuse to participate. All were assured of the confidentiality of their information.
The Cronbach’s alpha coefficient for the questionnaire was 0.823 and > 0.7 for all dimensions, indicating that the self-designed questionnaire had high credibility. Through expert discussion and evaluation, it was considered that the questionnaire had a certain validity. In total, 2699 questionnaires were collected, with 21 incomplete questionnaires. Thus, 2678 questionnaires were included in our analyses.
The sociodemographic characteristics of the participants are listed in Table 1. In terms of gender, 1566 (58.5%) were female, and 1112 (41.5%) were male, for a gender ratio of 1:1.4. The mean age and BMI were 43.3 ± 11.7 years and 23.54 ± 3.15 years, respectively. The respondents were from 31 provinces, autonomous regions, and municipalities directly under the central government, with 1291 (48.2%) from northern China, followed by 463 (17.3%) and 328 (12.2%) from central and eastern China, respectively. Most of the participants (93.6%) lived in urban areas. With regard to educational level, 1770 (66.1%) of the respondents had a college education, and 652 (24.3%) had a master’s degree or above. Nearly three-quarters of the participants (74.2%) had medical-related work experience. For personal income, 1738 (64.9%) of the participants earned > ¥5000/mo.
| Characteristics | Participants (n = 2678) | Percentage (%) | mean ± SD | |
| Gender | ||||
| Male | 1112 | 41.5 | ||
| Female | 1566 | 58.5 | ||
| Distribution in China | ||||
| Eastern | 328 | 12.2 | ||
| Southern | 209 | 7.8 | ||
| Central | 463 | 17.3 | ||
| Northern | 1291 | 48.2 | ||
| Northwest | 146 | 5.5 | ||
| Southwest | 159 | 5.9 | ||
| Northeast | 82 | 3.1 | ||
| Place of work or residence | ||||
| Urban | 2507 | 93.6 | ||
| Rural | 171 | 6.4 | ||
| Level of education | ||||
| Junior high school and below | 69 | 2.6 | ||
| Technical secondary school and high school | 187 | 7.0 | ||
| College and bachelor’s degree | 1770 | 66.1 | ||
| Master’s degree or above | 652 | 24.3 | ||
| Medical-related work experience | ||||
| Yes | 1986 | 74.2 | ||
| No | 692 | 25.8 | ||
| Personal income per month (¥) | ||||
| < 1000 | 35 | 1.3 | ||
| 1001-3000 | 270 | 10.1 | ||
| 3001-5000 | 635 | 23.7 | ||
| 5001-10000 | 877 | 32.7 | ||
| > 10000 | 861 | 32.2 | ||
| Age | 43.30 ± 11.70 | |||
| BMI (kg/m2) | 23.54 ± 3.15 |
Regarding the statement “China’s aging population exerts or will exert great pressure on society, families, and individuals”, 2286 (85.4%) of the respondents expressed agreement, 121 (4.5%) disagreed, and 271 (10.1%) felt unsure. Only 973 (36.3%) of the participants had heard of the IPFH.
Over 95% of the respondents thought that health status included physical and mental health, and 85.3% and 81.8% of the respondents thought that good social adaptability and moral health, respe
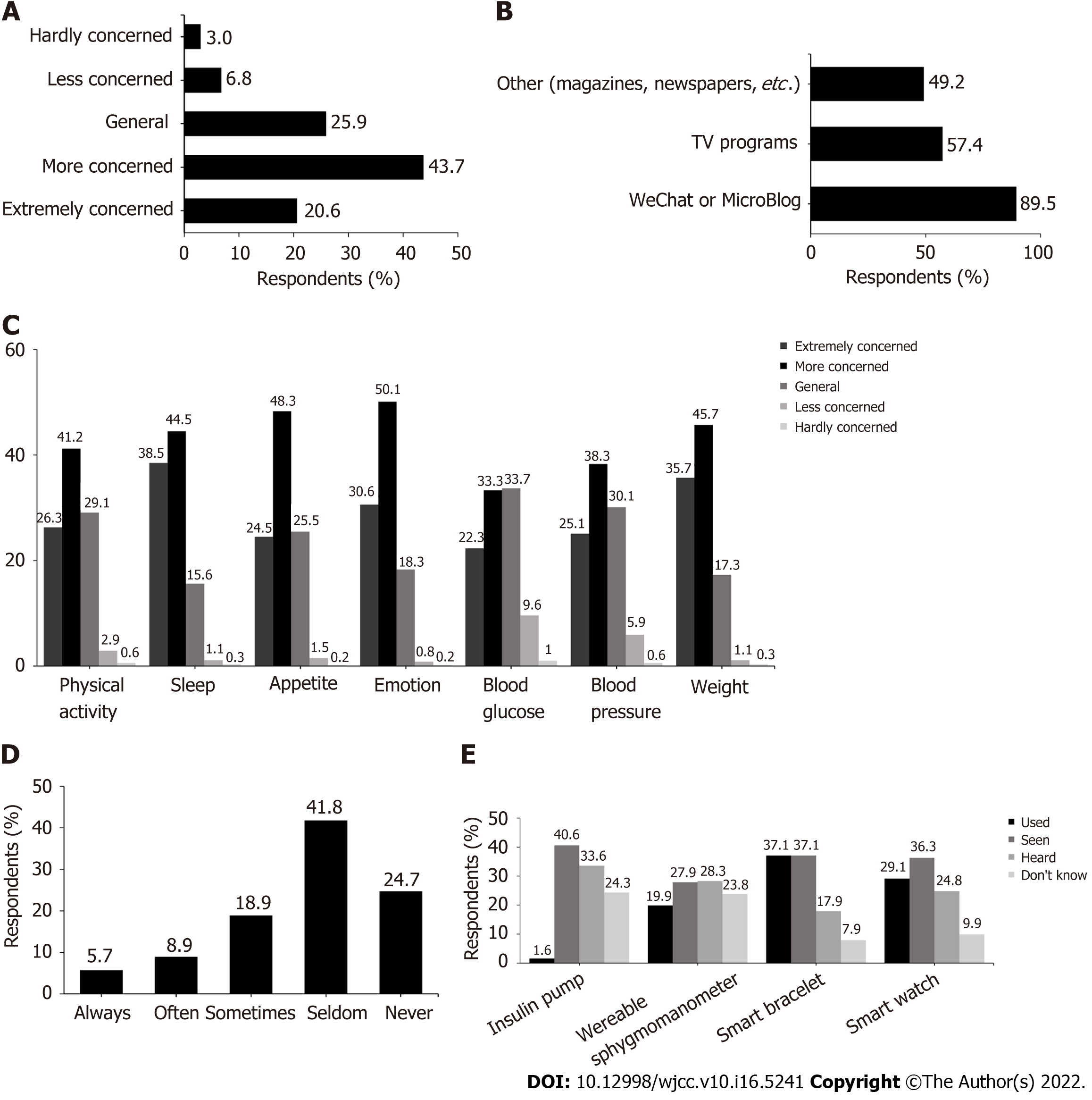
As shown in Figure 2A, the majority of the respondents usually paid close attention to health-related knowledge in their daily lives. In addition, 89.5% of the subjects usually acquired health-related popular science knowledge via WeChat official accounts or MicroBlogs, and 57.4% and 49.2% of the respondents received such knowledge via television and print publications, such as magazines and newspapers, respectively (Figure 2B). Over 70% of the respondents were more concerned about aspects such as weight, emotion, appetite, and sleep (Figure 2C). Only 33.5% of the participants discussed their own health promotion plans with professionals such as dieticians, fitness instructors, and health managers (Figure 2D). With regard to common wearable devices, such as smart watches, bracelets, sphygmomanometers, and insulin pumps, only 71 (2.7%) of the participants had no thoughts about them (Figure 2E).
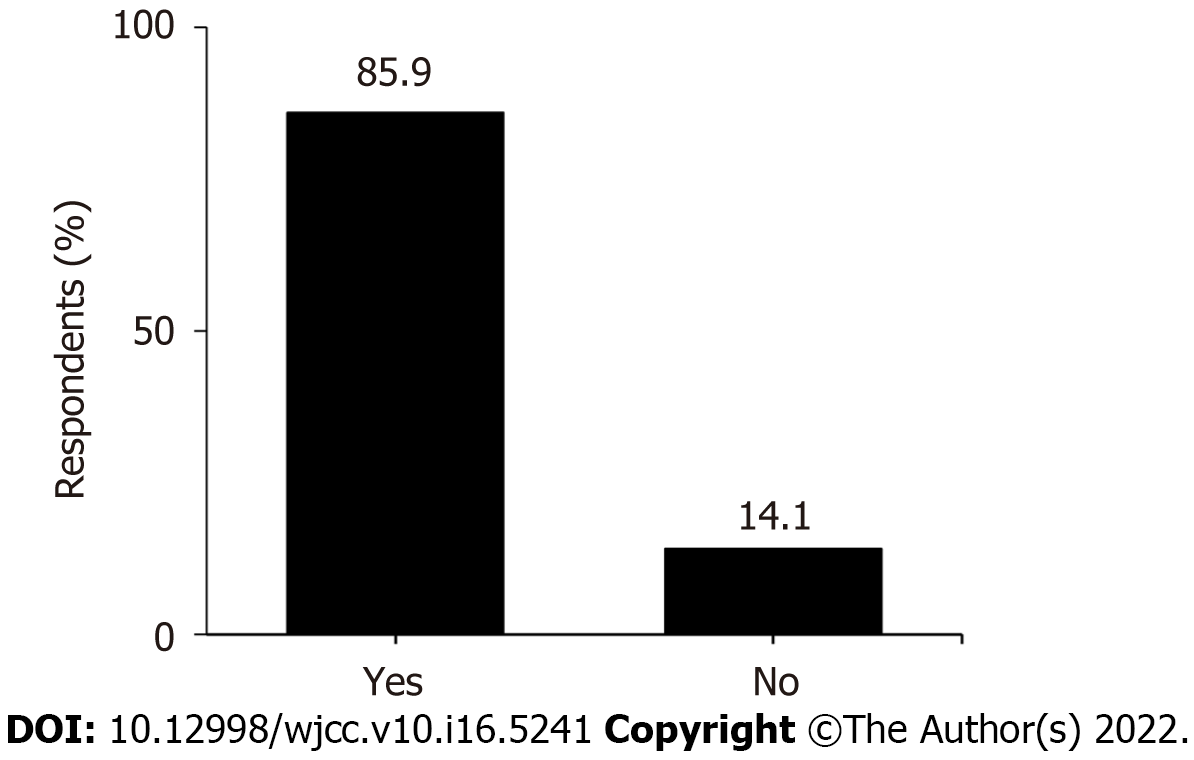
A total of 85.9% of the participants had a desire to become promoters and pioneers of IPFH (Figure 3).
Based on the methods mentioned above, IPFH awareness was divided into the “strong group” and the “weak group”. As illustrated in Table 2, 1065 participants had strong IPFH awareness and 1613 had weak awareness. Age, place of work or residence, medical-related work experience, monthly income, and BMI were significant factors (P < 0.05).
| Variables | Case, n (%) | Awareness | χ2 | P value | |
| Weak, n (%) | Strong, n (%) | ||||
| Total | 2678 | 1613 (60.2) | 1065 (39.8) | ||
| Gender | 1.598 | 0.206 | |||
| Male | 1112 (41.5) | 654 (58.8) | 458 (41.2) | ||
| Female | 1566 (58.5) | 959 (61.2) | 607 (38.8) | ||
| Age (yr) | 45.256 | < 0.001 | |||
| < 40 | 1088 (40.6) | 739 (67.9) | 349 (32.1) | ||
| > 40 | 1590 (59.4) | 874 (55.0) | 716 (45.0) | ||
| Place of work or residence | 5.115 | 0.024 | |||
| Urban | 2507 (93.6) | 1496 (59.7) | 1011 (40.3) | ||
| Rural | 171 (6.4) | 117 (68.4) | 54 (31.6) | ||
| Level of education | 4.694 | 0.196 | |||
| Junior high school and below | 69 (2.6) | 50 (72.5) | 19 (27.5) | ||
| Technical secondary school and high school | 187 (7.0) | 109 (58.3) | 78 (41.7) | ||
| College and bachelor’s degree | 1770 (66.1) | 1065 (60.2) | 705 (39.8) | ||
| Master’s degree or above | 652 (24.3) | 389 (59.7) | 263 (40.3) | ||
| Medical-related work experience | 22.165 | < 0.001 | |||
| Yes | 1986 (74.2) | 1144 (57.6) | 842 (42.4) | ||
| No | 692 (25.8) | 469 (67.8) | 223 (32.2) | ||
| Personal income per month (¥) | 21.443 | < 0.001 | |||
| < 1000 | 35 (1.3) | 28 (80.0) | 7 (20.0) | ||
| 1001-3000 | 270 (10.1) | 181 (67.0) | 89 (33.0) | ||
| 3001-5000 | 635 (23.7) | 407 (64.1) | 228 (35.9) | ||
| 5001-10000 | 877 (32.7) | 511 (58.3) | 366 (41.7) | ||
| > 10000 | 861 (32.2) | 486 (56.4) | 375 (43.6) | ||
| BMI (kg/m2) | 11.392 | 0.01 | |||
| < 18.5 | 101 (3.8) | 77 (76.2) | 24 (23.8) | ||
| 18.5-23.9 | 1440 (53.8) | 857 (59.5) | 583 (40.5) | ||
| 24-27.9 | 907 (33.8) | 539 (59.4) | 368 (40.6) | ||
| > 28 | 230 (8.6) | 140 (60.9) | 90 (39.1) | ||
| Variables | B | OR (95%CI) | P value |
| Age | 0.561 | 1.752 (1.485-2.067) | < 0.001 |
| Place of work or residence | -0.145 | 0.865 (0.610-1.227) | 0.416 |
| Medical-related work experience | 0.456 | 1.577 (1.308-1.902) | < 0.001 |
| Personal income per month (¥) | 0.116 | 1.123 (1.035-1.217) | 0.005 |
| BMI | 0.013 | 1.013 (0.905-1.134) | 0.823 |
The multivariate logistic regression model used the strength of IPFH awareness as the dependent variable and the factors significantly associated with IPFH awareness (age, place of work or residence, medical-related work experience, monthly income and BMI) as independent variables. Age (OR = 1.752, 95%CI: 1.485-2.067, P < 0.001), medical-related work experience (OR = 1.577, 95%CI: 1.308-1.902, P < 0.001), and monthly income (OR = 1.123, 95%CI: 1.035-1.217, P = 0.002) significantly affected the strength of IPFH awareness (Table 3).
This study is one of the first to examine IPFH awareness and related knowledge among Chinese people by using a network platform. It is of importance to understand and promote China’s development of IPFH and raise awareness of it. Based on the multivariable binary logistic regression, age, monthly income, and medical-related work experience were factors influencing IPFH awareness. Specifically, participants who were older, had a higher monthly income, and had medical-related work experience had strong IPFH awareness. It is not difficult to think that people who are older and who have worked in the medical industry are more inclined to pay more attention to their health and acquire more health knowledge, which makes their IPFH awareness higher. Participants who have a higher monthly income usually experience less life pressure and, at the same time, usually pay attention to all kinds of information in their daily lives. Thus, they may have more chances and energy to pay attention to their body and gain access to health knowledge as well as related policies, resulting in a relatively high IPFH awareness. This is consistent with the views of Braveman and Gottlieb[14] who stated that lower income is associated with lower health awareness and health status. However, it is different from the survey about the awareness of health knowledge among rural residents in western China conducted by Yuan et al[15] from July 2011 to April 2012. It indicated that the health knowledge level of lower income families was higher than that of rich families, and it declined with increasing age. This may be because the rural population has particular characteristics and the respondents we surveyed lived in urban areas. We think that more attention should be paid to people with poor IPFH awareness. Finding the reasons for their poor health awareness and improving the reasons individually will contribute to the development and improvement of the health of the whole population.
Although older people are healthier than in the past, aging of the population is still a huge burden at the societal and individual levels because the number of older people is increasing and they are characterized as being more fragile and susceptible to disease[16]. According to the Healthy China Action Promotion Committee, older people have been suffering from different diseases for approximately 8.3 years, and approximately 75% of the population had various chronic diseases in 2018[17]. The annual economic burden of age-related diseases will account for > 40% of the whole population. Our research showed that 85.4% of the participants agreed with the view “China’s aging population exerts or will exert great pressure on society, families, and individuals”, although some of the participants (4.5%) held the opposite view, which may mean that most citizens in China and worldwide could realize this serious situation. Therefore, they may be more likely to handle this challenge by taking the initiative through related policies led by the government.
Health management is a medical practice and a process of comprehensive detection, assessment, effective intervention and follow-up services for health status, and the risk factors for individuals and groups[18]. IPFH is a process based on health management in which people take the initiative to learn health-related knowledge, improve their lifestyle, and ensure their own health status. It emphasizes the active participation of individuals in personal health management and citizen participation in the development of a healthy China. With the coordinated development of the internet and IPFH, a population information platform for internet and health care and health-related big data systems are expected to be established, thereby executing the plan for internet-based Chinese health services. According to our research, only 36.3% of the respondents had heard of IPFH, which is unsatisfactory for promoting IPFH and, moreover, the Healthy China 2030 plan. The reason for this may be that, on the one hand, the plan is at the early stage in this long-term project, and thus far, the main task has been to build infrastructure and content. Additionally, IPFH appeared based on the implementation of the plan; thus, only a small number of people had heard of it. On the other hand, it is possible that many people may have acquired related knowledge and put it into practice in their daily lives without knowing that the knowledge was related to IPFH. This reminds us that it is better to be specific and comprehensive during the promotion of IPFH.
Over 30% of the participants in our study thought that participating in IPFH was unable to decrease the chance of hospitalization or extend the lifespan. Over 20% of the respondents denied that IPFH would have an impact on the progression of diseases. Most participants thought that the use of healthcare products and participation in relevant activities were related to IPFH, which was similar to the results shown by Yang and Meng[17]. This may be because, on the one hand, some people lack knowledge and awareness of IPFH as well as the occurrence and development of some diseases and lifespan. On the other hand, some people neglect the role of health-related factors such as lifestyle and the environment in the development of diseases and overlook the role of social adaptation in maintaining health status. Fewer than half of the respondents in our survey agreed with the role of health professionals including hospitals, family doctors, and health managers in promoting IPFH, and only 33.5% wanted to discuss their own health plan with professionals. The reasons may be as follows: First, the traditional opinion holds that hospitals and doctors are merely related to treating diseases, ignoring the role of health professionals in health improvement. In fact, the role of hospitals as well as doctors has already shifted[19] from only treating diseases to addressing the entire health and lifespan process. Second, health managers are unpopular because IPFH has not spread widely; thus, many people do not accept this occupation. Finally, this result shows that although family doctors have already been advocated by the government, people have less knowledge about the role of family doctors. Despite the importance of family doctors in improving disease management and health awareness[20], the rate of enjoying contractual services from family doctors is still low[21-23]. It is reassuring that most participants wanted to be promoters and practitioners of IPFH and health projects. We have every reason to look forward to the development and optimistic results of the Healthy China 2030 plan and IPFH because individuals are willing to take responsibility as members of the health industry. It is not difficult to imagine that with the wide publicity and smooth implementation of the plan and IPFH, people will accept and know this concept better and take the initiative to put their knowledge into practice.
Our survey showed that most participants paid close attention to health-related information and almost every health-related indicator, and there were hardly any participants who did not know about health-related wearable devices. This means that, with the development of society and improved living standards, as well as the promotion of health awareness, people are increasingly paying more attention to their health, and there are more chances to know things about high-tech health-related equipment. This is a good condition for promoting the Healthy China 2030 plan and IPFH.
As one of the most important components of IPFH, health knowledge and health behaviors are important to improving health status[19,24,25]. We found that the main approach to obtaining health information was via a network platform. This is related to the fact that people are inclined to spend more time on and obtain various information from mobile devices rather than from magazines and newspapers[26,27]. With the development of 5G and various applications on mobile devices, there should be more ways to promote IPFH and health monitoring, except for the traditional approaches such as Health Days, Media Publicity, etc. Mobile phone technology can be a possible solution to improve healthcare outcomes, and it has already been used in the management of some diseases and health monitoring[28,29]. This reminds us that it is better to promote the Healthy China 2030 plan and IPFH by using network platforms on mobile devices such as WeChat and MicroBlogs, which are some of the most common applications for all ages. A comprehensive, effective, and low-cost health management network-platform may be a good way. As an essential component of health projects, numerous types of high-tech wearable equipment can be applied, and individuals can acquire health information and indicators quickly so that they know their own body status in a timely manner and result in a healthy life condition[30-33]. This has the potential for the development and promotion of the Healthy China 2030 plan and IPFH to popularize and rapidly develop the health industry in the future.
This survey-based study had several limitations. Firstly, although the self-designed questionnaire that we used to collect data on the network platform was proven to be reliable based on statistical testing, there were still some disadvantages. For example, we cannot guarantee the authenticity of the data and the distribution of the participants. The participants’ distribution was biased. Most were from urban areas, had a college degree or above, and had medical-related work experience. The reason for this may be that we administered the questionnaire over the internet and its network link spread mainly via WeChat and Moments, leading to a limitation of the survey population. This reminds us that we have ignored the population who are disconnected from the internet and missed some people who really need to raise IPFH awareness, such as those in rural areas. There should be further surveys with comprehensive methods to assess the situation of the entire population. In addition, we have ignored the possibility that many individuals have knowledge related to IPFH and put it into practice in their daily lives but have never heard of the concept. Further studies require us to expand the methods and content of the survey in the form of questionnaires. Despite these limitations, this survey provides key insights to promote IPFH and develop health programs in China, and the results may affect future interventions to promote the health status of the Chinese population, as a whole, as well as the development of the global health industry.
The Chinese population has limited knowledge about IPFH, although most people in the population are concerned about health in their daily lives. People with strong IPFH awareness are older, earn more, and have medical-related work experience. To ensure the rapid popularization of IPFH and smooth development of the Healthy China 2030 plan, more focus should be given to young people, the low-income populations, rural populations, and people with a low level of education by the government, medical-related personnel, and health managers.
To address health challenges effectively, the Chinese government issued the Healthy China 2030 as well as the concept of the initiative practice for health (IPFH) to improve health among the Chinese population. However, there is no related survey investigating the IPFH awareness, and the knowledge and understanding of IPFH are still unclear.
The awareness of IPFH is directly related to health status. At the same time, identifying the factors influencing IPFH awareness is of great importance to improving the health status of the Chinese population as a whole and the development of the global health industry in the future.
To investigate awareness of IPFH in the Chinese population and explore the relevant influential factors and identify the at-risk population and effective interventions to improve health.
Based on the statistical testing, a network-platform electronic survey conducted by a self-designed questionnaire, which is a comprehensive and objective method involving different people, was used to investigate.
Fewer than half of the participants had heard about the IPFH. There was a lack of knowledge about IPFH among the participants. Age, monthly income, and medical-related work experience were the factors influencing IPFH awareness.
The Chinese population has limited knowledge of the IPFH. People with strong IPFH awareness are older, earn more, and have medical-related work experience.
Further surveys with comprehensive methods to assess the situation of the entire population are needed, and effective interventions should be conducted for people who have weak IPFH awareness.
Thanks to all who contributed to the investigation and Ms. Yang XR and Mr. Jiao GY for their careful revision and guidance for the manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Public, environmental and occupational health
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Duca FD, Germany; Galindo-Ferreiro A, Spain S-Editor: Guo XR L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Ramirez-Rubio O, Daher C, Fanjul G, Gascon M, Mueller N, Pajín L, Plasencia A, Rojas-Rueda D, Thondoo M, Nieuwenhuijsen MJ. Urban health: an example of a "health in all policies" approach in the context of SDGs implementation. Global Health. 2019;15:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | Morton S, Pencheon D, Squires N. Sustainable Development Goals (SDGs), and their implementation: A national global framework for health, development and equity needs a systems approach at every level. Br Med Bull. 2017;124:81-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 3. | Chen H, Qian Y, Dong Y, Yang Z, Guo L, Liu J, Shen Q, Wang L. Patterns and changes in life expectancy in China, 1990-2016. PLoS One. 2020;15:e0231007. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Chen S, Guo L, Wang Z, Mao W, Ge Y, Ying X, Fang J, Long Q, Liu Q, Xiang H, Wu C, Fu C, Dong D, Zhang J, Sun J, Tian L, Wang L, Zhou M, Zhang M, Qian M, Liu W, Jiang W, Feng W, Zeng X, Ding X, Lei X, Tolhurst R, Xu L, Wang H, Ziegeweid F, Glenn S, Ji JS, Story M, Yamey G, Tang S. Current situation and progress toward the 2030 health-related Sustainable Development Goals in China: A systematic analysis. PLoS Med. 2019;16:e1002975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 5. | He X, Song M, Qu J, Guo Y, Cao H, Sun R, Liu GH, Shen Y; Major Program Expert Group. Basic and translational aging research in China: present and future. Protein Cell. 2019;10:476-484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, Zhu X, Preedy V, Lu H, Bohr VA, Chan WY, Liu Y, Ng TB. A research agenda for aging in China in the 21st century. Ageing Res Rev. 2015;24:197-205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 331] [Cited by in RCA: 420] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 7. | Gase LN, Schooley T, Lee M, Rotakhina S, Vick J, Caplan J. A Practice-Grounded Approach for Evaluating Health in All Policies Initiatives in the United States. J Public Health Manag Pract. 2017;23:339-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Bolton KA, Kremer P, Gibbs L, Waters E, Swinburn B, de Silva A. The outcomes of health-promoting communities: being active eating well initiative-a community-based obesity prevention intervention in Victoria, Australia. Int J Obes (Lond). 2017;41:1080-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Tan X, Wu Q, Shao H. Global commitments and China's endeavors to promote health and achieve sustainable development goals. J Health Popul Nutr. 2018;37:8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Tan X, Kong S, Shao H. New strategies to improve the health of Chinese people by 2030. Aust J Prim Health. 2017;23:307-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Tan X, Zhang Y, Shao H. Healthy China 2030, a breakthrough for improving health. Glob Health Promot. 2019;26:96-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 104] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 12. | Fu W, Zhao S, Zhang Y, Chai P, Goss J. Research in health policy making in China: out-of-pocket payments in Healthy China 2030. BMJ. 2018;360:k234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 13. | Rattan SI. Healthy ageing, but what is health? Biogerontology. 2013;14:673-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;129 Suppl 2:19-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1957] [Cited by in RCA: 1958] [Article Influence: 178.0] [Reference Citation Analysis (0)] |
| 15. | Yuan F, Qian D, Huang C, Tian M, Xiang Y, He Z, Feng Z. Analysis of awareness of health knowledge among rural residents in Western China. BMC Public Health. 2015;15:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 16. | Fang EF, Xie C, Schenkel JA, Wu C, Long Q, Cui H, Aman Y, Frank J, Liao J, Zou H, Wang NY, Wu J, Liu X, Li T, Fang Y, Niu Z, Yang G, Hong J, Wang Q, Chen G, Li J, Chen HZ, Kang L, Su H, Gilmour BC, Zhu X, Jiang H, He N, Tao J, Leng SX, Tong T, Woo J. A research agenda for ageing in China in the 21st century (2nd edition): Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. 2020;64:101174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 304] [Cited by in RCA: 337] [Article Influence: 67.4] [Reference Citation Analysis (0)] |
| 17. | Yang Y, Meng Y. Is China Moving toward Healthy Aging? Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Steenkamer BM, Drewes HW, Heijink R, Baan CA, Struijs JN. Defining Population Health Management: A Scoping Review of the Literature. Popul Health Manag. 2017;20:74-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 19. | Owen N, Healy GN, Dempsey PC, Salmon J, Timperio A, Clark BK, Goode AD, Koorts H, Ridgers ND, Hadgraft NT, Lambert G, Eakin EG, Kingwell BA, Dunstan DW. Sedentary Behavior and Public Health: Integrating the Evidence and Identifying Potential Solutions. Annu Rev Public Health. 2020;41:265-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 20. | Lam CL. The role of the family doctor in the era of multi-disciplinary primary care. Fam Pract. 2016;33:447-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Huang J, Zhang T, Wang L, Guo D, Liu S, Lu W, Liang H, Zhang Y, Liu C. The effect of family doctor-contracted services on noncommunicable disease self-management in Shanghai, China. Int J Health Plann Manage. 2019;34:935-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 22. | Shang X, Huang Y, Li B, Yang Q, Zhao Y, Wang W, Liu Y, Lin J, Hu C, Qiu Y. Residents' Awareness of Family Doctor Contract Services, Status of Contract with a Family Doctor, and Contract Service Needs in Zhejiang Province, China: A Cross-Sectional Study. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 63] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 23. | Huang J, Liu S, He R, Fang S, Lu W, Wu J, Liang H, Zhang Y. Factors associated with residents' contract behavior with family doctors in community health service centers: A longitudinal survey from China. PLoS One. 2018;13:e0208200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 24. | Liu YB, Liu L, Li YF, Chen YL. Relationship between Health Literacy, Health-Related Behaviors and Health Status: A Survey of Elderly Chinese. Int J Environ Res Public Health. 2015;12:9714-9725. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 175] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 25. | Mulder JWCM, Galema-Boers AMH, de Jong-Verweij LM, Hazelzet JA, Roeters van Lennep JE. The development and first results of a health-related outcomes set in familial hypercholesterolemia (FH) patients: Knowledge is health. Atherosclerosis. 2020;293:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Christensen MA, Bettencourt L, Kaye L, Moturu ST, Nguyen KT, Olgin JE, Pletcher MJ, Marcus GM. Direct Measurements of Smartphone Screen-Time: Relationships with Demographics and Sleep. PLoS One. 2016;11:e0165331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 153] [Cited by in RCA: 142] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 27. | Panova T, Carbonell X. Is smartphone addiction really an addiction? J Behav Addict. 2018;7:252-259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 342] [Cited by in RCA: 393] [Article Influence: 56.1] [Reference Citation Analysis (0)] |
| 28. | Sahu M, Grover A, Joshi A. Role of mobile phone technology in health education in Asian and African countries: a systematic review. Int J Electron Healthc. 2014;7:269-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Chauhan V, Negi PC, Raina S, Bhatnagar M, Guleri R, Kanwar V, Pandey KS. Smartphone-based tele-electrocardiography support for primary care physicians reduces the pain-to-treatment time in acute coronary syndrome. J Telemed Telecare. 2018;24:540-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Styles CE, Cheng A, Hoad VC, Kiely P, Watson M, Seed CR. Excluding Occult Hepatitis B Infection before Assigning False-Positive Status to Non-Repeatable NAT Reactivity: Concerning Stolz et al. "Safe-Testing Algorithm for Individual-Donation Nucleic Acid Testing: 10 Years of Experience in a Low-Prevalence Country" [Transfus Med Hemother. 2019 Apr;46(2):104-10]. Transfus Med Hemother. 2020;47:272-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Xin Q, Wu J. A novel wearable device for continuous, non-invasion blood pressure measurement. Comput Biol Chem. 2017;69:134-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 32. | Sun J, Guo Y, Wang X, Zeng Q. mHealth For Aging China: Opportunities and Challenges. Aging Dis. 2016;7:53-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 33. | Kekade S, Hseieh CH, Islam MM, Atique S, Mohammed Khalfan A, Li YC, Abdul SS. The usefulness and actual use of wearable devices among the elderly population. Comput Methods Programs Biomed. 2018;153:137-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 92] [Article Influence: 13.1] [Reference Citation Analysis (0)] |