Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5185
Peer-review started: August 14, 2021
First decision: November 17, 2021
Revised: November 21, 2021
Accepted: April 2, 2022
Article in press: April 2, 2022
Published online: June 6, 2022
Processing time: 291 Days and 17.3 Hours
The number of patients with bronchial trauma (BT) who survived to hospital admission has increased with the improvement of prehospital care; early diagnosis and treatment should be considered, especially among blunt trauma patients, whose diagnosis is frequently delayed.
To describe the early recognition and surgical management considerations of blunt and penetrating BTs, and to elaborate the differences between them.
All patients with BTs during the past 15 years were reviewed, and data were retrospectively analyzed regarding the mechanism of injury, diagnostic and therapeutic procedures, and outcomes. According to the injury mechanisms, the patients were divided into two groups: Blunt BT (BBT) group and penetrating BT (PBT) group. The injury severity, treatment procedures, and prognoses of the two groups were compared.
A total of 73 patients with BT were admitted during the study period. The proportion of BTs among the entire cohort with chest trauma was 2.4% (73/3018), and all 73 underwent thoracotomy. Polytrauma patients accounted for 81.6% in the BBT group and 22.9% in the PBT group, and the mean Injury Severity Score was 38.22 ± 8.13 and 21.33 ± 6.12, respectively. Preoperative three-dimensional spiral computed tomography (CT) and/or fiberoptic bronchoscopy (FB) were performed in 92.1% of cases in the BBT group (n = 38) and 34.3% in the PBT group (n = 35). In the BBT group, a delay in diagnosis for over 48 h occurred in 55.3% of patients. In the PBT group, 31 patients underwent emergency thoracotomy due to massive hemothorax, and BT was confirmed during the operation. Among them, 22 underwent pulmo-tractotomy for hemostasis, avoiding partial pneumonectomy. In this series, the overall mortality rate was 6.9% (5/73), and it was 7.9% (3/38) and 5.7% (2/35) in the BBT group and PBT group, respectively (P > 0.05). All 68 survivors were followed for 6 to 42 (23 ± 6.4) mo, and CT, FB, and pulmonary function examinations were performed as planned. All patients exhibited normal lung function and healthy conditions except three who required reoperations.
The difference between blunt and penetrating BTs is obvious. In BBT, patients generally have no vessel injury, and the diagnosis is easily missed, leading to delayed treatment. The main cause of death is ventilation disturbance due to tension pneumothorax early and refractory atelectasis with pneumonia late. However, in PBT, most patients require emergency thoracotomy because of simultaneous vessel trauma and massive hemothorax, and delays in diagnosis are infrequent. The leading cause of death is hemorrhagic shock.
Core Tip: There are significant differences between blunt and penetrating bronchial traumas (BTs), particularly the severity of the injury, the site of the injury, the incidence of shock, the time before surgery, and the surgical procedure. From our experiences, single lumen intubation should be performed immediately after BT injury to reach the contralateral main bronchus to ensure ventilation of the healthy lung. We also summarize the four functions of temporary clamping of the pulmonary hilus during thoracotomy. In addition, pneumonectomy should be avoided, especially in penetrating BT patients, due to the limited lung tissue damage.
- Citation: Gao JM, Li H, Du DY, Yang J, Kong LW, Wang JB, He P, Wei GB. Management and outcome of bronchial trauma due to blunt versus penetrating injuries. World J Clin Cases 2022; 10(16): 5185-5195
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5185.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5185
Tracheobronchial injury has long been considered a rare occurrence. The incidence of tracheobronchial injury is 2%-6% among patients with chest trauma[1-5]. Of these patients, approximately 80% die before they arrive at the hospital[5-9]. With the improvement of prehospital care, the number of patients who arrive at the hospital alive has increased[4,6,10]; thus, early diagnosis and treatment should be considered to improve their survival. In view of some differences between the trachea and bronchus, this study examined only bronchial trauma (BT).
Data from all patients with chest trauma treated at the Chongqing Emergency Medical Center from July 2005 to June 2020 were reviewed, and BT data were screened for inclusion in a retrospective analysis according to sex, age, injury mechanism, diagnostic and therapeutic methods, and outcome. Patients were divided into two groups according to the injury mechanism: Blunt BT (BBT) and penetrating BT (PBT).
Because no human subjects were involved in this study and because only deidentified data were used, the requirements for ethical review and informed consent were waived by the Institutional Review Board of Chongqing Emergency Medical Center (CEMC), China.
Included cases: Injury involving the main bronchus (grade I branch), lobar bronchus (grade II branch), and segmental bronchus (grade III branch).
Excluded cases: Blunt and penetrating lung injury combined with subsegmental bronchus (≤ grade IV) injury.
In the BBT group, among patients sustaining severe chest trauma, the clinical manifestations and physical signs were closely observed. Focused assessment with sonography for trauma (FAST) was performed, but a few patients had to undergo emergency department thoracotomy (EDT) due to tension pneumothorax. Once a BT was suspected, spiral computed tomography (CT) with three-dimensional (3D) reconstruction and fiberoptic bronchoscopy (FB) were performed.
In the PBT group, using FAST examinations, hemothorax with shock was observed, emergency thoracotomy was performed, and a BT diagnosis was obtained intraoperatively in all patients; however, a few patients without hemothorax were submitted to CT and FB.
Chest tube drainage was performed for tension pneumothorax or hemothorax cases; in this process, if respiratory distress worsened, single lumen intubation was immediately performed to reach the contralateral main bronchus to ensure ventilation. Mediastinal drainage was performed for tension pneumomediastinum. Massive hemothorax in penetrating injuries required blood transfusion. In moribund patients, emergency thoracotomy including EDT was required without any preoperative treatment.
When a diagnosis of BT was confirmed or highly suspected, emergency or delayed posterolateral thoracotomy was performed. Repair procedures for bronchial injury included simple suture, debridement and end-to-end anastomosis (including simultaneous repair of vascular injury), partial pneumonectomy (lobe or segment), sleeve resection, or pulmonary tractotomy for ligation of injured vessels and bronchi.
All data are expressed as the mean ± SD. Comparisons between groups were performed using SPSS 17 by Student’s t test or the chi-square test, as appropriate. Differences were considered significant at P < 0.05.
A total of 73 patients with BT were admitted during the study period. The proportion of BTs in the entire cohort of chest trauma was 2.4% (73/3018). There were 49 men and 24 women with ages ranging from 16 to 62 years (average, 36.68 ± 11.32 years). In the BBT group (n = 38), the cause of injury was traffic accidents in 17, falls in 10, impacts in 6, and collapses in 5. In the PBT group (n = 35), there were 32 stab wounds and 3 gunshot wounds.
Polytrauma patients accounted for 81.6% of patients in the BBT group and 22.9% in the PBT group; the mean Injury Severity Score was 38.22 ± 8.13 and 21.33 ± 6.12, respectively. The most common intrathoracic-associated injury was pulmonary contusion. On admission, 31.6% of BBT group patients had hemorrhagic shock due to associated injuries, and 88.6% of PBT group patients had shock due to hemothorax.
In the BBT group, the injury was on the left in 16 and on the right in 22, including 18 main bronchi (6 left, 12 right), 12 lobar bronchi (5 left, 7 right), and 8 segmental bronchi (5 left, 3 right). Of the 12 patients with right main bronchial injury, one had simultaneous left lobar bronchial rupture. In the PBT group, there were 25 left and 10 right bronchi, including 2 main bronchi (1 left, 1 right), 11 lobar bronchi (6 left, 5 right), and 22 segmental bronchi (18 left, 4 right).
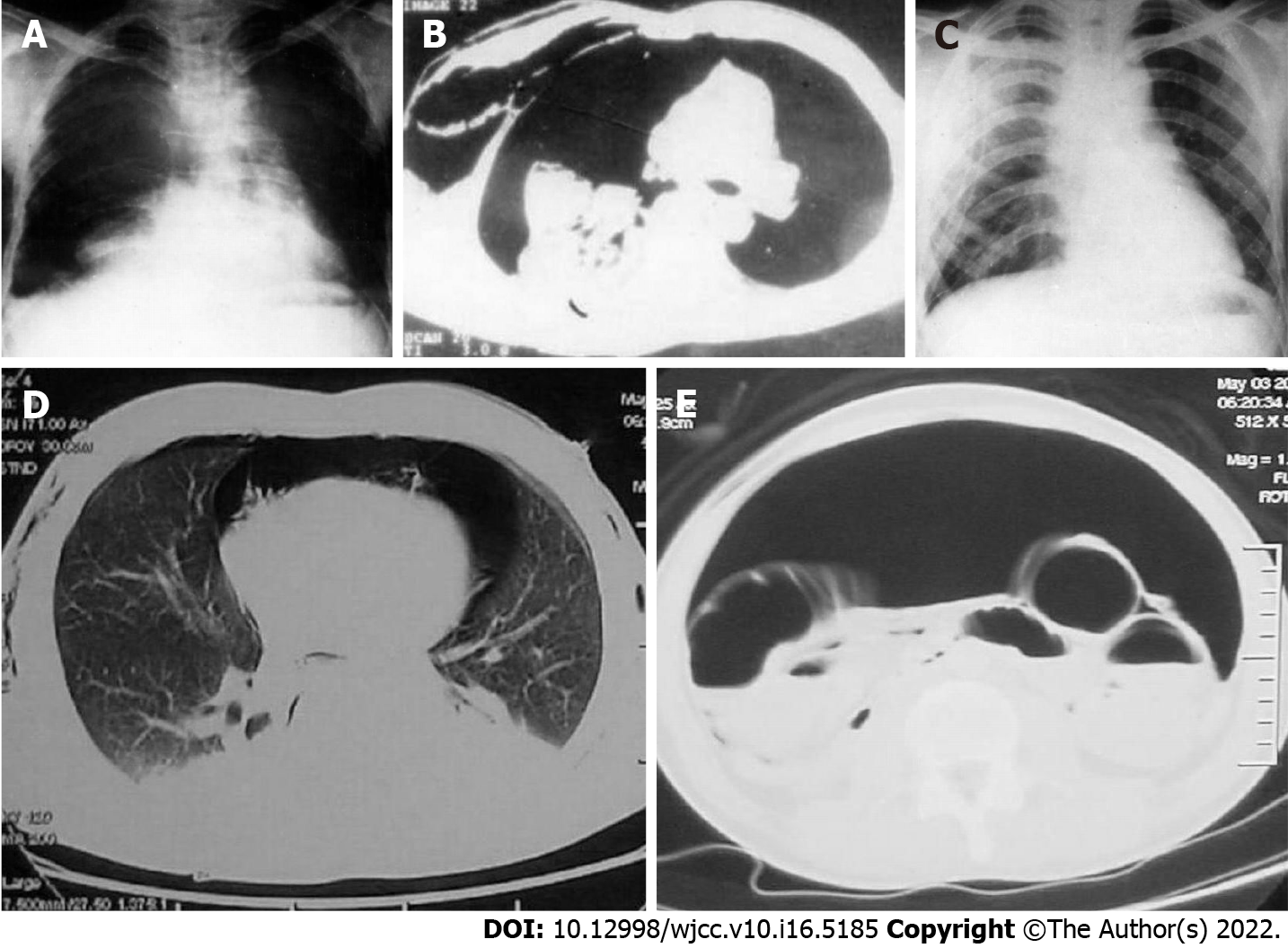
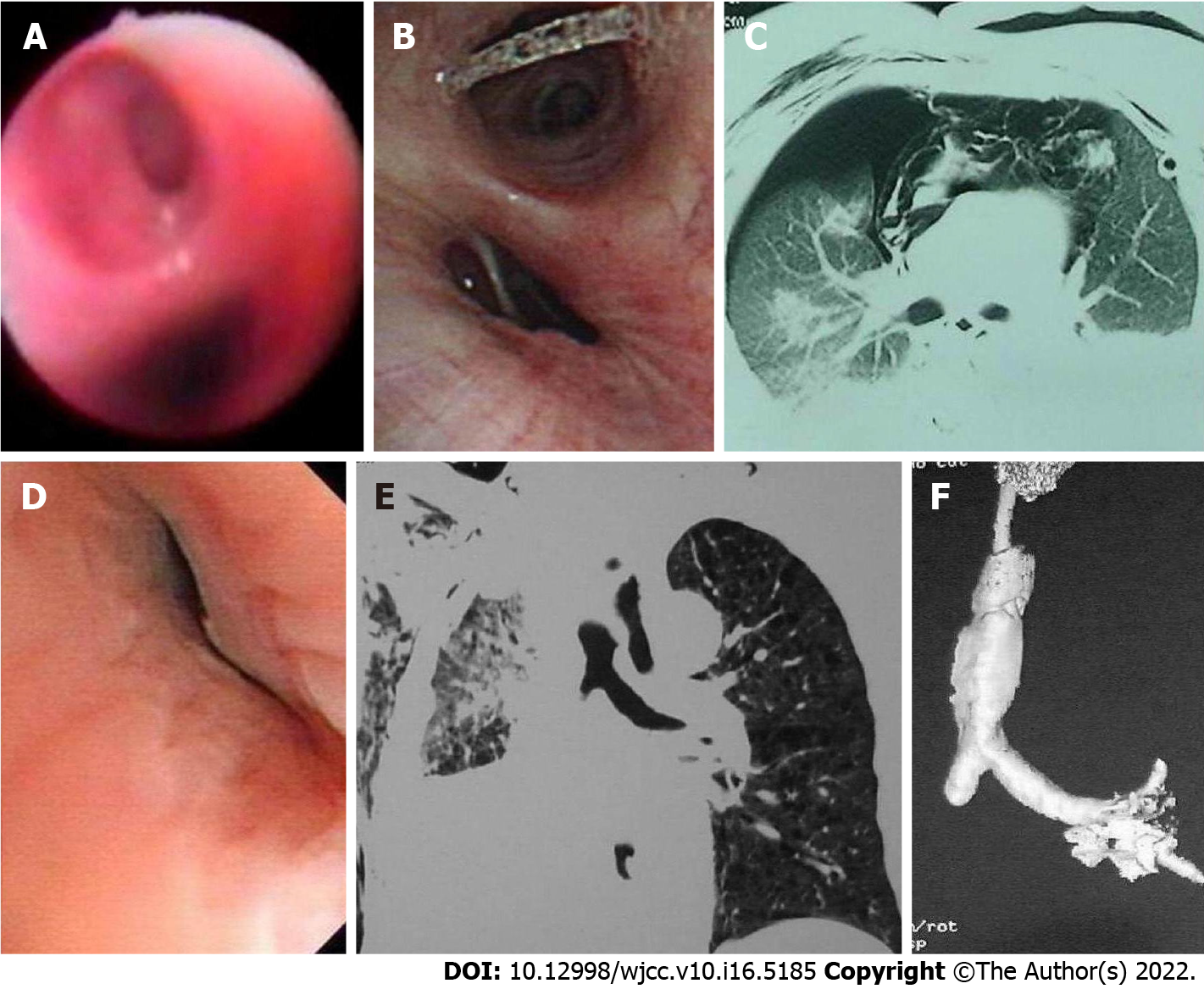
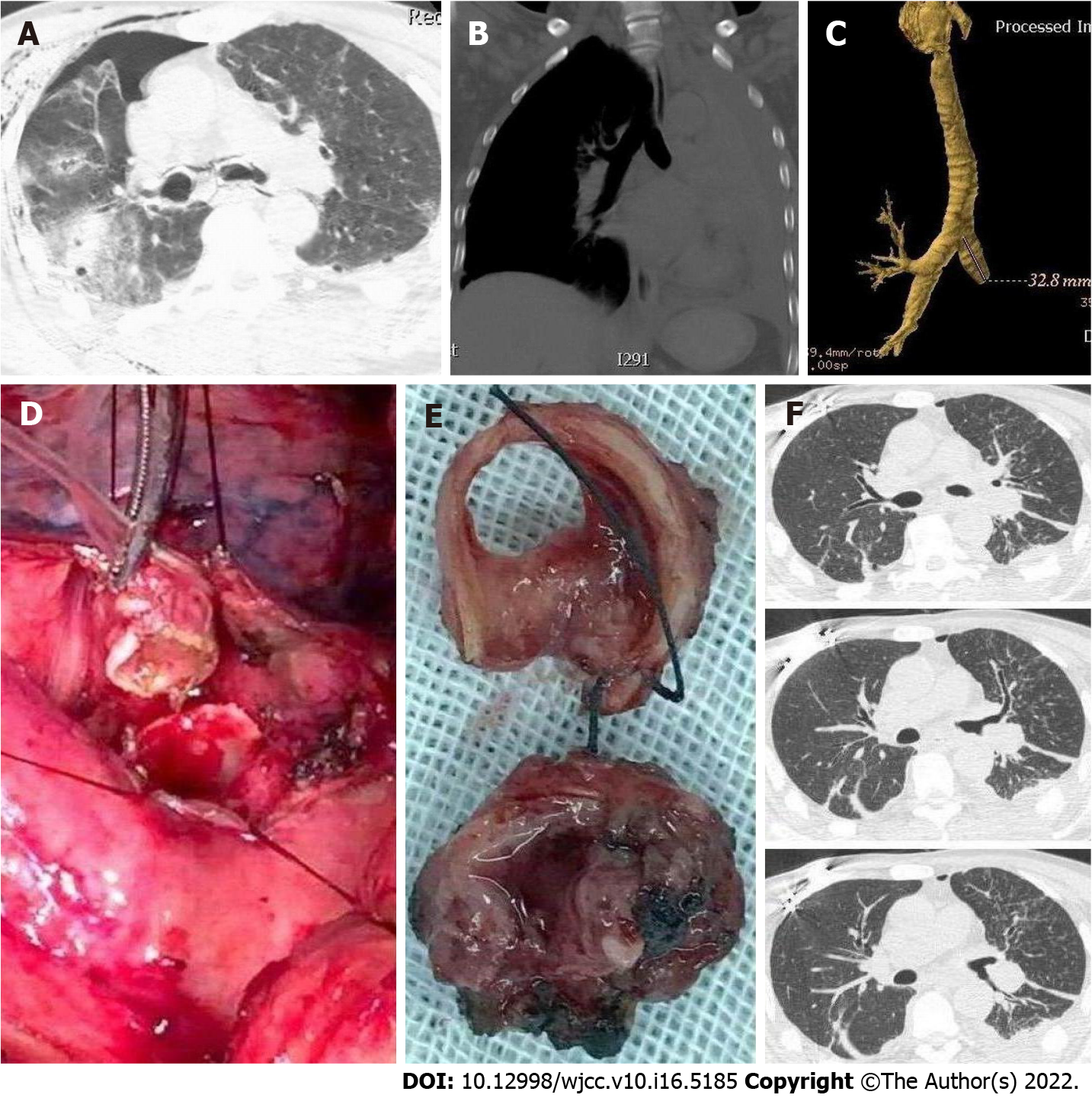
All 38 patients in the BBT group had dyspnea, and among them, 13 presented with hemoptysis. All patients received a chest X-ray (n = 6) or CT scan (n = 29), but three had to undergo EDT due to worsening tension pneumothorax. Positive signs included pneumothorax in 32 (27 tension and 9 hemopneumothorax), subcutaneous emphysema in 29, pneumomediastinum in 15 (8 tension and 1 associated with pneumoperitoneum), total or lobar atelectasis in 28, “fallen lung sign”[3] in 5, pulmonary contusion in 28, rib fracture in 25, clavicle fracture in 9, and sternal fracture in 7. Most patients had both dyspnea and hemoptysis at the same time. Among them, 19 patients with pneumothorax developed delayed atelectasis 5-10 d after injury. Furthermore, clear proof of BT was observed by 3D-spiral CT in 76% (22/29) of patients undergoing this examination. In all 35 patients without EDT, BT was confirmed by FB (Figures 1-5). The median time of definite diagnosis was 68 h (0.5 h to 52 d) after injury, and the diagnosis was delayed over 48 h in 21 (55.3%) patients. All 38 patients underwent emergency or delayed thoracotomy.
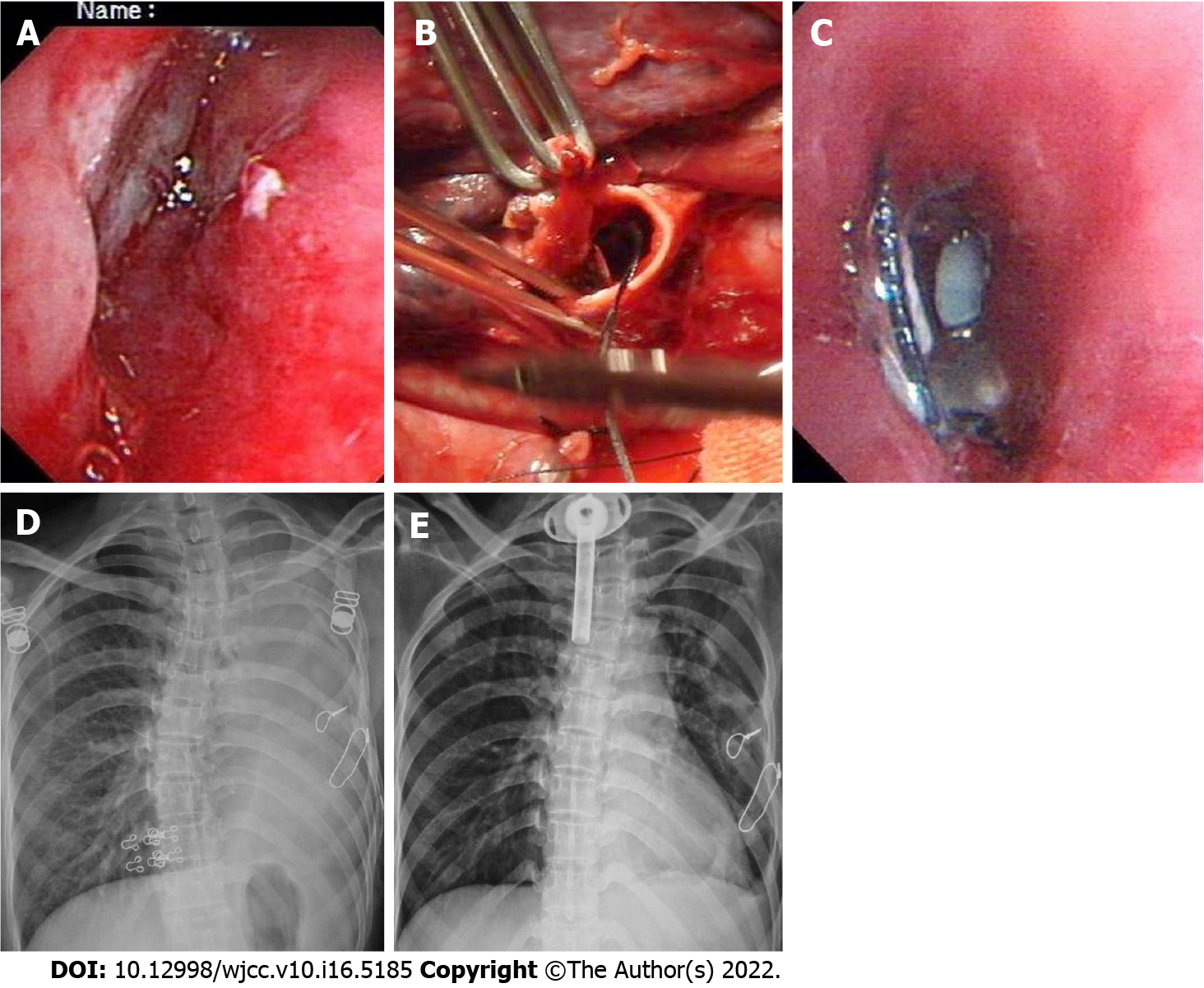
Among the 35 patients in the PBT group, 31 presented with hemothorax with shock, and of them, 12 exhibited hemoptysis. Emergency thoracotomy was performed soon after admission, and the average time from admission to operation was 1.22 ± 0.35 h (0.5 to 6 h). In the remaining four patients without shock, thoracotomy was performed within 12 h after admission because of ongoing hemothorax. Of these 35 patients, eight had preoperative chest X-rays, and seven had CT scans. All images showed hemothorax with no direct evidence of BT. During the operation, BT was found. The surgical methods and outcomes of the 73 patients are shown in Table 1.
| Surgical procedure | No. of patients | No. of survivors |
| BBT group (n = 38) | ||
| Debridement and end-to-end anastomosis of the main bronchus | 121,2 | 12 |
| Simple suture of the main bronchus | 3 | 3 |
| EDT for clamping of proximal end of main bronchus | 1 | 0 |
| Emergency explorative thoracotomy in operating room | 1 | 0 |
| Pneumonectomy of left lung | 1 | 0 |
| Simple suture of lobar bronchus | 5 | 5 |
| Lobectomy | 73 | 7 |
| Irregular segmentectomy | 8 | 8 |
| PBT group (n = 35) | ||
| Repair of main bronchus | 21 | 2 |
| Simple suture of lobar bronchus | 4 | 4 |
| Lobectomy | 6 | 6 |
| Emergency explorative thoracotomy in operating room | 1 | 0 |
| Pulmonary tractotomy for ligation of vessels and bronchi | 22 | 21 |
In this series, the overall mortality rate was 6.9% (5/73), and it was 7.9% (3/38) in the BBT group and 5.7% (2/35) in the PBT group. Among the three deaths in the BBT group, one died of severe ventilation disturbance caused by bilateral large bronchus injury, one was due to prolonged total atelectasis with pneumonia due to a missed diagnosis of main bronchus injury 48 d later, and another was due to pulmonary hypertension and right heart failure 1 year after pneumonectomy. The causes of two deaths in the PBT group were exsanguination from the hilum during the operation and sepsis after the operation.
In the BBT group, postoperative complications included atelectasis (n = 8), five cases of which were due to stenosis. Therapy included respiratory physiotherapy and diathermy or cryotherapy of granulation via FB. Mechanical ventilation was administered cautiously after surgery in three patients. Three cases required reoperation (Table 1). In the PBT group, no significant complications were observed.
All 68 survivors were followed for 6 to 42 (23 ± 6.4) mo to observe their clinical manifestations, and they underwent CT, FB, and pulmonary function examinations. All surviving patients exhibited normal lung function and healthy conditions, but three required reoperation, as described above. Comparisons between the two groups are shown in Table 2.
| Variable | Blunt (n = 38) | Penetrating (n = 35) | P value |
| Mean ISS | 38.22 ± 8.13 | 21.33 ± 6.12 | < 0.001 |
| Incidence of polytrauma | 31/38 (81.6%) | 8/35 (22.9%) | < 0.001 |
| Incidence of BT | 38/1911 (2.0%) | 35/1107 (3.2%) | < 0.05 |
| Injured right side | 22/38 (57.9%) | 10/35 (28.6%) | < 0.001 |
| Time of definite diagnosis after injury > 48 h | 21/38 (55.3%) | 0/35 (0.0%) | < 0.001 |
| Preoperative imaging | 35/38 (92.1%) | 12/35 (34.3%) | < 0.001 |
| Incidence of partial resection of lung | 16/38 (42.1%) | 6/35 (17.1%) | < 0.025 |
| Percentage of segmental bronchus injury | 8/38 (21.1%) | 22/35 (62.9%) | < 0.001 |
| Shock rate | 12/38 (31.6%) | 31/35 (88.6%) | < 0.001 |
| Morbidity | 8/38 (21.1%) | 0/35 (0%) | < 0.001 |
| Mortality | 3/38 (7.9%) | 2/35 (5.7%) | > 0.05 |
The number of BT patients has increased due to improvements in prehospital care, as well as CT and FB. Failure to diagnose BT early can lead to catastrophic outcomes, such as lethal tension pneumothorax and stubborn atelectasis with pneumonia due to stenosis (Figures 2A, 2E, 3A-D, 4B, and 5D). Early diagnosis and treatment clearly decrease morbidity and mortality. Unfortunately, the diagnosis of BBT is often delayed until refractory atelectasis with pneumonia occurs, and many cases are diagnosed by FB only weeks after the injury[11-14]. In the BBT group of this series, 55.3% of patients were diagnosed more than 48 h after the injury. In victims of high-energy blunt thoracic trauma, BT should be strongly considered to detect the associated injuries. Common presenting signs include dyspnea, subcutaneous emphysema, and hemoptysis. X-ray or CT findings are most commonly pneumothorax, pneumomediastinum, atelectasis, pulmonary contusion, and rib fractures. There was one case of tension pneumomediastinum with pneumoperitoneum in this series. This rare phenomenon is considered pneumoperitoneum caused by air passing through the aortic and esophageal hiatus[15,16]. Among the abovementioned conditions, pneumothorax (or pneumomediastinum) and atelectasis are the most important. The former appears immediately after injury, while the latter can be in the early or late stage or from early pneumothorax to late atelectasis.
There are two main causes of atelectasis after blunt chest trauma: Pulmonary contusion and BT. In the first condition, atelectasis is caused by a decrease in pulmonary compliance due to edema, effusion, bleeding, and obstruction of the bronchial lumen due to clotting and secretions. In BT patients, atelectasis can be caused by obstruction of the lumen due to clots or the dislocation of injured cartilage in the acute phase and by bronchial stenosis with granulation in the delayed phase. Therefore, differential diagnosis is required when posttraumatic atelectasis exists. The most important diagnostic methods are 3D-spiral CT and FB, especially FB, which is recognized as the gold standard for diagnosis[14,15,17-19].
The first task of emergency treatment is to relieve ventilatory dysfunction, including rapid decompression and drainage of the tension pneumothorax and pneumomediastinum. However, Mattox[11] indicated that when bronchial transection exists, chest tube drainage can result in evacuation of the total tidal volume. In this series, one victim was sent to the emergency department 15 min after injury, and thoracic drainage was immediately placed for bilateral tension pneumothorax. However, her breathing stopped suddenly during the process. EDT showed that the right main and left lobar bronchi were transected, and the total amount of bilateral chest blood was < 500 mL. The patient died of severe ventilation disturbance half an hour after the injury (Table 1). Therefore, when addressing tension pneumothorax resulting from bronchial rupture, thoracic drainage alone is not sufficient. In this case, single lumen intubation should be performed immediately to reach the contralateral main bronchus to ensure ventilation of the contralateral lung. This is also a damage control surgery measure; if there is another injury requiring priority surgery, it can be performed. We do not advocate for double-lumen intubation because it may aggravate bronchial injury. Shemmeri and Vallières[3] have the same opinion. Another alternative is clamping the proximal end of the main bronchus by EDT. When BT is suspected, mechanical ventilation should not be blindly used because it can aggravate the injury or worsen the condition[5,20].
Once BT is confirmed or highly suspected, thoracotomy should be performed immediately. The surgical method primarily depends on the location and degree of injury. If the tear is less than 1/3 of the circumference of the tube or is longitudinal, a simple suture can be placed in the main or lobar bronchus; otherwise, different procedures should be performed according to the bronchial grade. When the disruption is in the lobar or segmental bronchus, lobectomy or segmental resection can be performed. In this condition, trying to repair the damage is unlikely to succeed because of stenosis after the operation. However, if the damage involves the main bronchus, bronchorrhaphy, end-to-end anastomosis, and sleeve resection are the correct procedures. When accompanied by vascular injury, it should be repaired simultaneously. Many authors have indicated that pneumonectomy should be avoided if possible[7,10,14,20]. Pneumonectomy inevitably leads to pulmonary hypertension and right heart failure. One patient in this group suffered such an outcome (Table 1). Debridement should be performed before anastomosis; otherwise, the rate of failure or complications, such as leakage and stenosis due to granulation, will increase[2,3,14,17]. If the lung can be expanded, anastomosis can be performed. BT that causes total atelectasis can be repaired with a return of pulmonary function for many years after the injury[19]. In this group, one patient underwent reoperation for scar resection and anastomosis with a satisfactory return of pulmonary function 3 years after the injury (Figures 5D and 5E, Table 1). Of course, these issues should be addressed early. After the operation, if pulmonary compliance is poor, mechanical ventilation is needed to maintain lung expansion. The pressure should not be too high, and close observation is needed. There were three such cases in this group, and no leakage was induced.
Long-term delayed diagnosis of main bronchial injury leading to atelectasis with severe pneumonia is life-threatening. One patient was admitted to a local hospital after injury and underwent thoracotomy. Unfortunately, BT was missed during the operation. She was subsequently transferred to our hospital 45 d after the injury, and left main BT was confirmed by FB. However, she developed serious pneumonia due to long-term atelectasis and died 3 d later.
Penetrating BT is different from blunt BT in many aspects and is perhaps much simpler (Table 2). In fact, it is primarily based on two differences: (1) Although there are many explanations for the mechanism of blunt BT, the main explanation is the shearing force. The accompanying vessels are seldom damaged at the same time due to their toughness, so most patients do not have massive hemothorax and shock. In contrast, penetrating BT often involves blood vessels as well, causing massive hemothorax and shock; and (2) Blunt trauma is characterized by extensive injury, including pulmonary parenchyma and extrathoracic injuries. However, penetrating injuries are limited; when PBT occurs, there are fewer pulmonary and extrathoracic injuries. For the above reasons, in penetrating BT, emergency thoracotomy is often required to stop the bleeding, and it is difficult to miss the diagnosis. Preoperative imaging is often absent, and there are fewer postoperative complications. Among the 35 patients in the PBT group, 31 underwent emergency thoracotomy soon after admission, and 4 underwent emergency thoracotomy within 12 h after admission.
After opening the chest cavity, the control method for turbulent bleeding involves temporary clamping of the pulmonary hilum. This maneuver yields the following four benefits: (1) It controls massive hemorrhage and exposes the operative field; (2) When the main bronchus is ruptured, contralateral ventilation is ensured; (3) It prevents the blood from the injured side from flowing into the healthy side of the lung and causing asphyxia; and (4) If the pulmonary vein is injured, coronary artery air embolism can be prevented.
Unnecessary pneumonectomy should especially be avoided because there is less lung tissue damage in PBT. Since the 1980s, we have treated deep lung lacerations, including hilar injury, by opening the wound tract, ligating the injured blood vessels and bronchioles, and then suturing the lung laceration without postoperative necrosis or infection of lung tissue. Wall et al[21] reported a similar treatment protocol.
In this series, there were more BBTs on the right side, which is similar to most reports[1,3,6,8,22]. However, most of the PBTs were on the left side, and most of them were segmental branch injuries. The reason for this is that most assailants use their right hand, corresponding to the injury being in the left middle and lower part of the chest. Another reason for the fewer penetrating main bronchus injuries is that a hilar penetrating injury is often complicated with massive hemorrhage, which is difficult to survive, even in the hospital.
In summary, the difference between blunt and penetrating BTs is obvious. In BBT, patients generally have no vessel injury, and the diagnosis and treatment are easily delayed and missed. The main cause of death is ventilation disturbance due to tension pneumothorax early and refractory atelectasis with pneumonia late. However, in PBT, most patients require emergency thoracotomy because of simultaneous vessel trauma and massive hemothorax; a delayed diagnosis is infrequent. The leading cause of death is hemorrhagic shock. BT focuses on blunt injury. In patients with blunt chest injury, we must be vigilant, perform CT and FB in time to make a clear diagnosis, and strive for early treatment to reduce morbidity and mortality.
The number of patients with bronchial trauma (BT) who survived to the hospital has increased with the improvement of prehospital care; early diagnosis and treatment should be considered, especially among blunt trauma patients whose diagnosis is frequently delayed.
Treatment of the injury is not the difficult part, but timely diagnosis of bronchial injury does. In this paper, we try to analyze the characteristics of blunt and penetrating bronchial injuries and clarify the difference between them.
In this study, we reviewed and analyzed the data of blunt and penetrating bronchial injuries cases that we had dealt with to describe the early recognition and surgical management considerations of the two types of bronchial injuries.
Data from all patients with chest trauma treated at the Chongqing Emergency Medical Center from July 2005 to June 2020 were reviewed, and BT data were screened for retrospective analysis regarding sex, age, injury mechanism, diagnostic and therapeutic methods, and outcome. Patients were divided into two groups according to the injury mechanism: Blunt BT (BBT) and penetrating BT (PBT).
A total of 73 patients with BT were admitted during the study period. The proportion of BTs in the entire cohort of chest trauma was 2.4% (73/3018). All 73 underwent thoracotomy. Polytrauma patients accounted for 81.6% in the BBT group and 22.9% in the PBT group; the mean Injury Severity Score was 38.22 ± 8.13 and 21.33 ± 6.12, respectively. Preoperative three-dimensional spiral computed tomography (CT) and/or fiberoptic bronchoscopy (FB) were performed in 92.1% of cases in the BBT group (n = 38) and 34.3% in the PBT group (n = 35). In the BBT group, delayed diagnosis over 48 h occurred in 55.3% of cases. In the PBT group, 31 patients underwent emergency thoracotomy for massive hemothorax, and BT was confirmed during the operation. Among them, 22 underwent pulmo-tractotomy for hemostasis, avoiding partial pneumonectomy. In this series, the overall mortality rate was 6.9% (5/73), and it was 7.9% (3/38) in the BBT group and 5.7 % (2/35) in the PBT group (P > 0.05). All 68 survivors were followed for 6 to 42 (23 ± 6.4) mo, and CT, FB, and pulmonary function examinations were performed as planned. All patients exhibited normal lung function and healthy conditions except three who required reoperations.
The difference between blunt and penetrating BT is obvious. In BBT, patients generally have no vessel injury, and the diagnosis and treatment are easily delayed and missed. The main cause of death is ventilation disturbance due to tension pneumothorax early and refractory atelectasis with pneumonia late. However, in PBT, most patients require emergency thoracotomy because of simultaneous vessel trauma and massive hemothorax; a delayed diagnosis is infrequent. The leading cause of death is hemorrhagic shock.
Treatment of bronchial injuries should focus more on early diagnosis and timely management.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Batyrbekov K, Kazakhstan; Deshwal H, United States S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Madani A, Pecorelli N, Razek T, Spicer J, Ferri LE, Mulder DS. Civilian Airway Trauma: A Single-Institution Experience. World J Surg. 2016;40:2658-2666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Welter S, Essaleh W. Management of tracheobronchial injuries. J Thorac Dis. 2020;12:6143-6151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Shemmeri E, Vallières E. Blunt Tracheobronchial Trauma. Thorac Surg Clin. 2018;28:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Madden BP. Evolutional trends in the management of tracheal and bronchial injuries. J Thorac Dis. 2017;9:E67-E70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Bagga B, Kumar A, Chahal A, Gamanagatti S, Kumar S. Traumatic Airway Injuries: Role of Imaging. Curr Probl Diagn Radiol. 2020;49:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | van Roozendaal LM, van Gool MH, Sprooten RTM, Maesen BAE, Poeze M, Hulsewé KWE, Vissers YLJ, de Loos ER. Surgical treatment of bronchial rupture in blunt chest trauma: a review of literature. J Thorac Dis. 2018;10:5576-5583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Prokakis C, Koletsis EN, Dedeilias P, Fligou F, Filos K, Dougenis D. Airway trauma: a review on epidemiology, mechanisms of injury, diagnosis and treatment. J Cardiothorac Surg. 2014;9:117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 8. | Rieth A, Varga E, Kovács T, Ottlakán A, Németh T, Furák J. Contemporary management strategies of blunt tracheobronchial injuries. Injury. 2021;52 Suppl 1:S7-S14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Díaz C, Carvajal DF, Morales EI, Sangiovanni S, Fernández-Trujillo L. Right main bronchus rupture associated with blunt chest trauma: a case report. Int J Emerg Med. 2019;12:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Alassal MA, Ibrahim BM, Elsadeck N. Traumatic intrathoracic tracheobronchial injuries: a study of 78 cases. Asian Cardiovasc Thorac Ann. 2014;22:816-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Mattox KL. Thoracic injury requiring surgery. World J Surg. 1983;7:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Demondion P, Fabre D, Herve P, Dartevelle P. Posttraumatic main left bronchial rupture. Ann Thorac Surg. 2014;97:e25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Maskey N, Sapkota R, Thapa B. Bronchial injuries: a tale of differing presentations. Indian J Thorac Cardiovasc Surg. 2019;35:245-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Li Y, Wang G, Wu C, Pan Z, Li H, Wang Q, Wang Y, Dai J. Experience of diagnosis and treatment of traumatic bronchial rupture in children in a single clinical center. Pediatr Surg Int. 2020;36:1019-1025. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Grewal HS, Dangayach NS, Ahmad U, Ghosh S, Gildea T, Mehta AC. Treatment of Tracheobronchial Injuries: A Contemporary Review. Chest. 2019;155:595-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 83] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 16. | Hong SB, Lee JY, Lee J, Choi KB, Suh JH. Right Main Bronchus Rupture Presenting with Pneumoperitoneum. Korean J Thorac Cardiovasc Surg. 2018;51:216-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Saleh ME, Beshir H, Mohammed WH, Sanad M. Tracheobronchial injuries: tertiary center experience. Asian Cardiovasc Thorac Ann. 2020;28:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Lin WT, Su SY, Hsieh CF, Lai CC, Chao CM. Traumatic Thoracic Burst Fracture Associated with Bronchial Rupture. J Emerg Med. 2017;53:260-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Carretta A, Melloni G, Bandiera A, Negri G, Voci C, Zannini P. Conservative and surgical treatment of acute posttraumatic tracheobronchial injuries. World J Surg. 2011;35:2568-2574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Hsu WC, Schweiger C, Hart CK, Smith M, Varela P, Gutierrez C, Ormaechea M, Cohen AP, Rutter MJ. Management of the Disrupted Airway in Children. Laryngoscope. 2021;131:921-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Wall MJ Jr, Hirshberg A, Mattox KL. Pulmonary tractotomy with selective vascular ligation for penetrating injuries to the lung. Am J Surg. 1994;168:665-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Chowdhury S, Griniatsos J. Right main bronchus rupture due to blunt chest trauma. Clin Case Rep. 2019;7:242-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |