Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.5072
Peer-review started: December 16, 2021
First decision: February 8, 2022
Revised: February 15, 2022
Accepted: March 26, 2022
Article in press: March 26, 2022
Published online: May 26, 2022
Processing time: 159 Days and 0.8 Hours
Thymic carcinoma is a rare, aggressive tumor arising from the thymus. In less than 7% of patients with thymic carcinoma, extrathoracic metastases occur in the extrathoracic lymph nodes, liver, and bone. Isolated splenic metastasis can occur but is very uncommon. To date, only 2 cases of splenic metastases from thymic carcinoma have been reported.
A 45-year-old man presented with chronic cough, dyspnea, persistent hoarseness and unintentional weight loss 17 kgs in 6 mo. Neck magnetic resonance imaging revealed a large, lobulated, soft-tissue mass measuring 5.4 cm × 6.6 cm × 3.8 cm which involved the left superior mediastinum and supraclavicular fossa. Chest computed tomography (CT) revealed a confluent and lobulated soft tissue mass encased the right brachiocephalic artery, right and left carotid arteries, and left subclavian artery in the mediastinum. A fluorodeoxyglucose-positron emission tomography was arranged for malignancy survey. The image revealed intense fluorodeoxyglucose avidity in a soft tissue lobulated mass occupying the superior mediastinum, over the cystic lesion in the spleen and in few enlarged nodules over the left supraclavicular fossa. CT-guided biopsy of the thymic mass and the ultrasound-guided biopsy of the splenic lesion were consistent with a thymic carcinoma with splenic metastasis. The patient was diagnosed of thymic carcinoma, cT2N2M1b, stage IVb.
A fluorodeoxyglucose (FDG)-positron emission tomography (PET) scan can provide a useful diagnostic value in conjunction with pathological result in evaluating tumor staging. Our case emphasizes the utility of FDG-PET for metastasis detection in thymic carcinoma.
Core Tip: Isolated splenic metastasis from thymic carcinoma is very rare. Nevertheless, splenic metastasis should be taken into consideration, although it is often asymptomatic. Our case emphasizes the utility of fluorodeoxyglucose -positron emission tomography for metastasis detection in thymic carcinoma.
- Citation: Tsai YH, Lin KH, Huang TW. Rare solitary splenic metastasis from a thymic carcinoma detected on fluorodeoxyglucose-positron emission tomography: A case report. World J Clin Cases 2022; 10(15): 5072-5076
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/5072.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.5072
Thymic carcinoma is a rare, aggressive tumor arising from the thymus. The anterosuperior mediastinum is where most thymic carcinomas are found. In less than 7% patients, extrathoracic metastases are present in extrathoracic lymph nodes, the liver, and bones[1]. Isolated splenic metastases are exceptionally rare. Patients with solitary splenic metastasis are often diagnosed without symptoms or raised tumor marker levels. This case study presents our experience with an unusual case of solitary splenic metastasis from a thymic carcinoma.
A 45-year-old man visited outpatient department presented with chronic cough, dyspnea and persistent hoarseness.
The patient started to have persistent cough with chest tightness since 10 mo ago. Unintentional weight loss for 17 kgs in 6 mo was also mentioned.
The patient denied any history of past illness.
The patient denied any family history or allergic history to food or medicines.
No specific finding on physical examinations was identified.
Routine blood test results were unremarkable, with normal levels of carcinoembryonic antigen, carbohydrate antigen 19-9 and squamous cell carcinoma antigen.
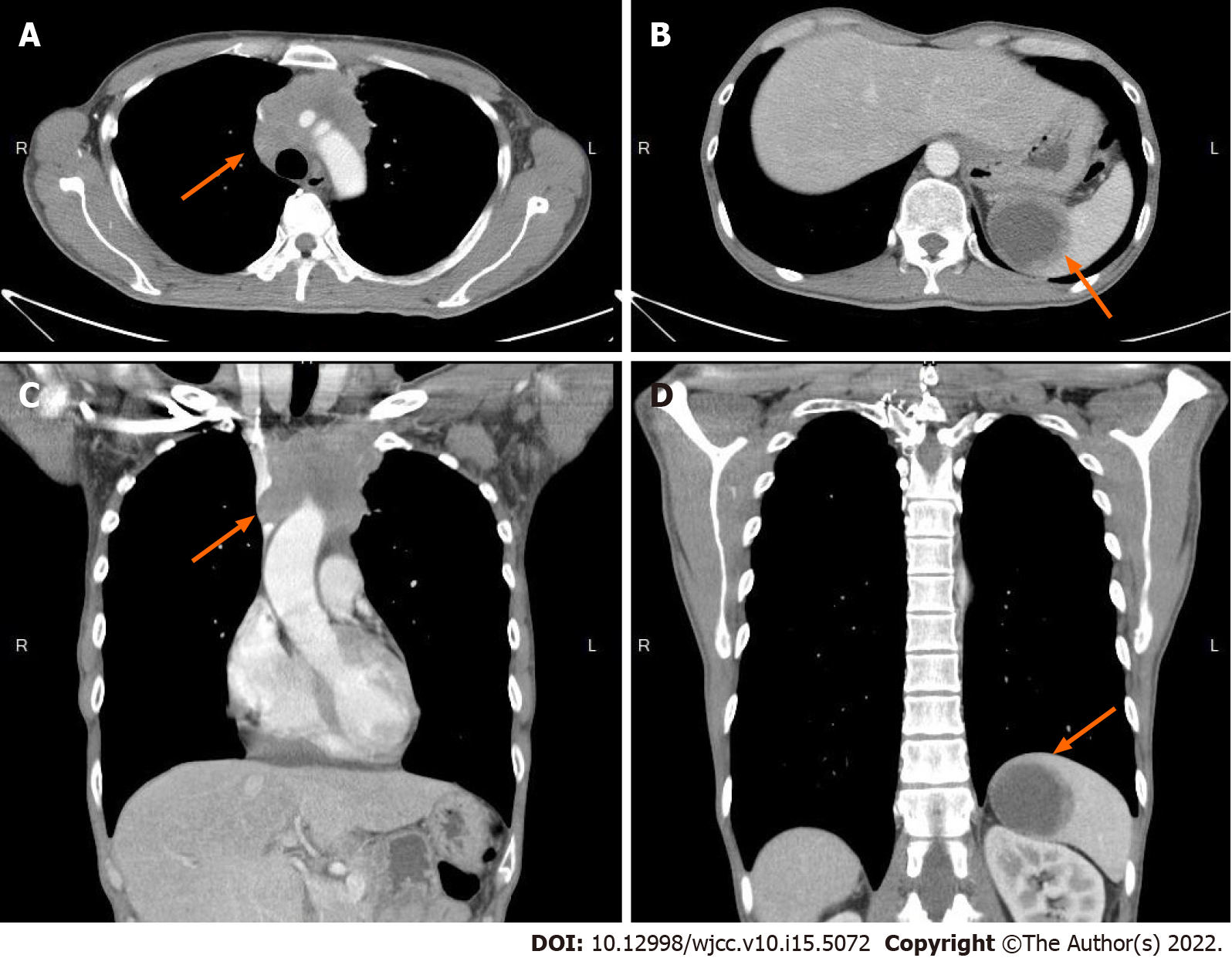
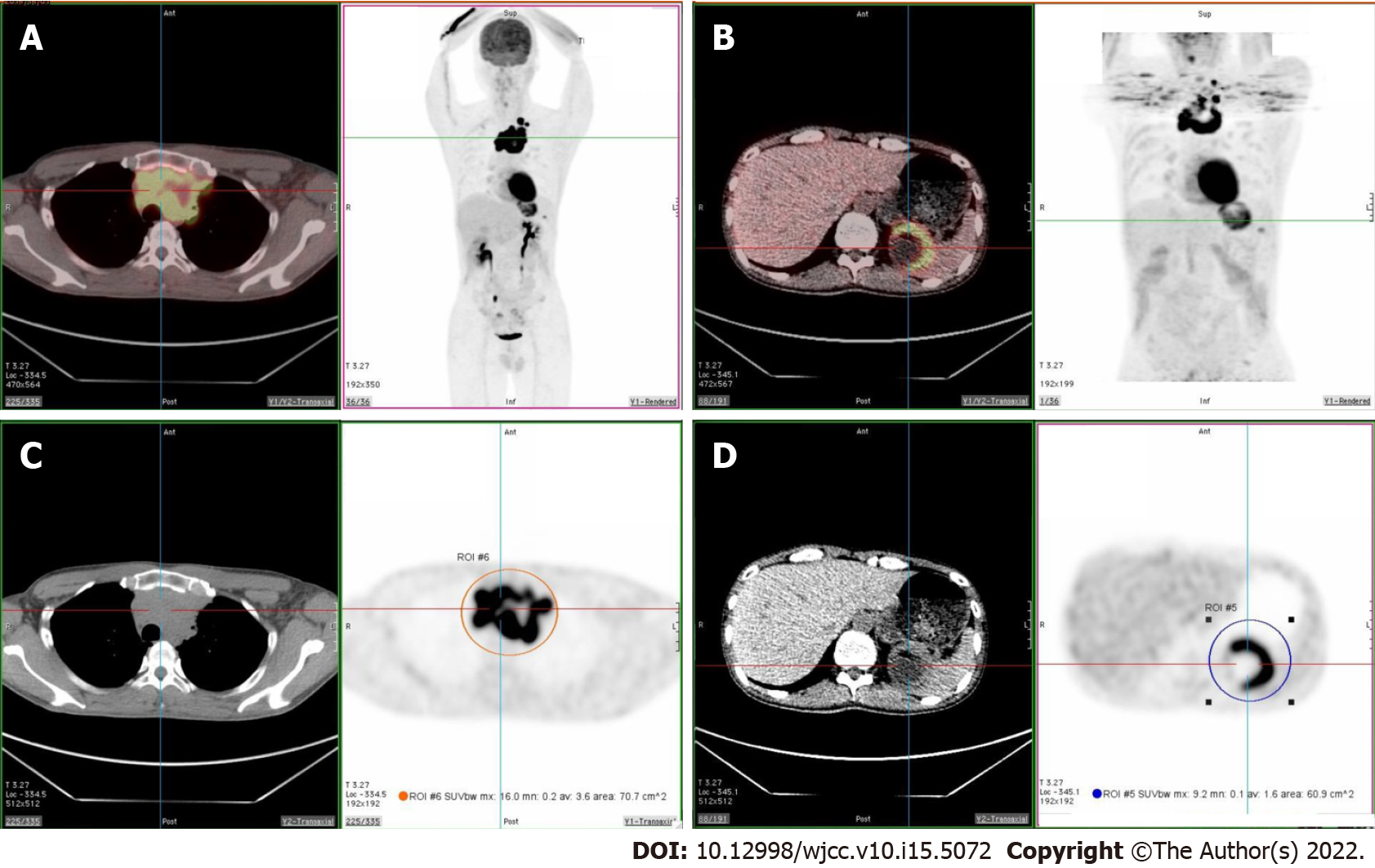
The chest X-ray did not show any significant abnormalities. No significant abnormal findings on the abdominal sonography. Abdomen computed tomography (CT) discovered a 3.8 cm cystic lesion with mild irregular wall in the spleen was noted, which regular follow up was suggested. The patient was transferred to otorhinolaryngology department owing to persistent hoarseness and left shoulder pain. He underwent microlaryngeal surgery after left sided vocal cord palsy with a protruding lesion on the postcricoid region was revealed by stroboscopy. Neck magnetic resonance imaging (MRI) and bone scan were arranged after surgery. A large, lobulated, soft-tissue mass measuring 5.4 cm x 6.6 cm x 3.8 cm which involved the left superior mediastinum and supraclavicular fossa was discovered accidentally on MRI. Chest CT (Figure 1) revealed a confluent and lobulated soft tissue mass encased the right brachiocephalic artery, right and left carotid arteries, and left subclavian artery in the mediastinum. With enlarged nodes (maximal size: 1.6 cm) in the left supraclavicular region. In addition, the chest CT scan disclosed a cystic mass in the spleen that increased from 3.8 cm to 5.1 cm in diameter in one month (Figure 1). A fluorodeoxyglucose (FDG)-positron emission tomography (PET) was arranged two months later for malignancy survey. The image revealed intense FDG-avidity in a soft tissue lobulated mass occupying the superior mediastinum (standard uptake value (SUV) max = 16.0, size > 9.0 cm), over the cystic lesion in the spleen (SUV max = 9.2, size = 6.1 cm) and in few enlarged nodules over the left supraclavicular fossa (SUV max. up to 17.5, size = 2.1 cm) (Figure 2).
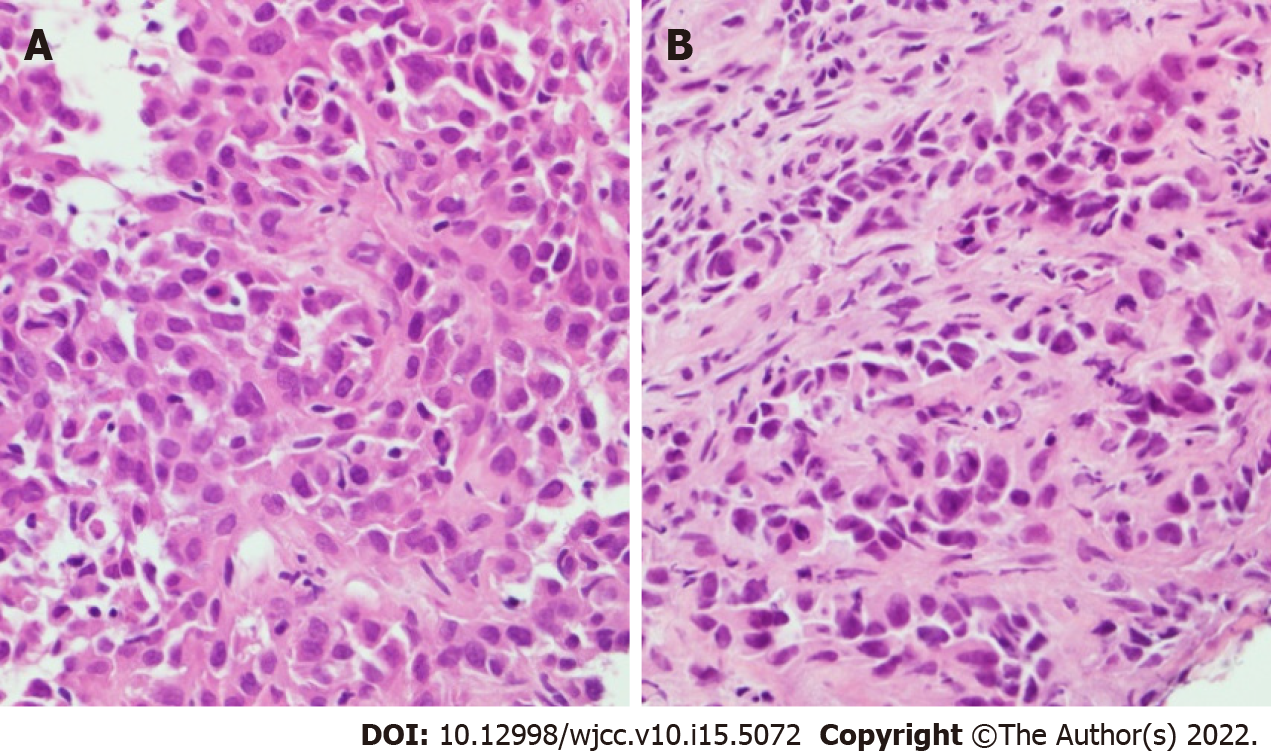
The pathology result of the postcricoid lesion was benign. The CT-guided biopsy of the thymic mass was positive for cluster of differentiation 5, negative for thyroid transcription factor-1. Microscopically, Hematoxylin-Eosin staining of the thymic mass showed polygonal and spindle shaped tumor cells accompanied by giant cells with bizarre and multilobulated nuclei, suggesting poorly differentiated carcinoma of the mediastinum (Figure 3). The ultrasound-guided biopsy of the splenic lesion was made, which was consistent with a metastasis from the thymic carcinoma (Figure 3).
A thymic malignancy with regional nodal and splenic metastases, cT2N2M1b was suggested by the results of the PET scan. Correlated to the pathology results of thymic and splenic lesion, the patient was diagnosed of thymic carcinoma, cT2N2M1b, stage IVb according to eighth edition of TNM staging system.
The patient underwent biopsies of the thymic and splenic masses. Nevertheless, the patient refused to take further treatment after the diagnosis of thymic carcinoma with solitary splenic metastasis was confirmed.
After two months of follow up at outpatient department. Unfortunately, we lost follow up of the patient after then.
Comparing with thymoma, thymic carcinoma is more aggressive. Survival rates for thymic carcinomas vary depending on the stage (stages I-II: 91%; stages III-IV: 31%) and resectability[2]. Surgery is the gold standard treatment for early stage thymic carcinoma. Platinum-based chemotherapy is the standard choice for patients with locally invasive and metastatic disease[3]. It is important to evaluate staging thoroughly to make proper therapeutic plan.
Isolated splenic metastasis from a thymic carcinoma is very rare. To date, only 2 cases have been reported[4,5]. However, spleen biopsy was not performed in the case presented by Chen et al[5]. Extrathoracic metastasis could also be neglected by abdomen sonography, which was operator dependent in the first study[4]. In our study, pathological evidence and PET scan results completed a more definite diagnosis of thymic carcinoma with isolated splenic metastasis, cT2N2M1b, stage IVb.
It’s extremely rare to find isolated splenic metastasis in a patient with thymic carcinoma. Nevertheless, splenic metastasis should be taken into consideration, while splenic metastases are often asymptomatic. To help determine the appropriate management for thymic carcinoma, FDG-PET scan is suggested. FDG-PET scan can provide a useful diagnostic value in conjunction with pathological result in evaluating tumor staging. Our case emphasizes the utility of FDG-PET for metastasis detection in thymic carcinoma.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koizumi T, Japan; Liu YC, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Lewis JE, Wick MR, Scheithauer BW, Bernatz PE, Taylor WF. Thymoma. A clinicopathologic review. Cancer. 1987;60:2727-2743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Litvak AM, Woo K, Hayes S, Huang J, Rimner A, Sima CS, Moreira AL, Tsukazan M, Riely GJ. Clinical characteristics and outcomes for patients with thymic carcinoma: evaluation of Masaoka staging. J Thorac Oncol. 2014;9:1810-1815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Yang Y, Fan XW, Wang HB, Xu Y, Li DD, Wu KL. Stage IVb thymic carcinoma: patients with lymph node metastases have better prognoses than those with hematogenous metastases. BMC Cancer. 2017;17:217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Kao HW, Lin WC, Peng YJ, Chen CY. Unusual isolated splenic metastasis secondary to thymic carcinoma. Zhonghua Fangshexue Zazhi. 2005;4. |
| 5. | Chen D, Meng X, Zhao Y, Wu S. Isolated splenic metastasis from a thymic carcinoma: A case report. Cancer Biol Ther. 2016;17:911-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |