Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.5036
Peer-review started: December 13, 2021
First decision: February 14, 2022
Revised: February 25, 2022
Accepted: March 26, 2022
Article in press: March 26, 2022
Published online: May 26, 2022
Processing time: 162 Days and 2.7 Hours
Secondary thyroid malignancies are rarely reported, especially thyroid metastasis after resection of hepatocellular carcinoma (HCC). We report a patient with thyroid metastasis after resection of HCC.
A 42-year-old female underwent partial hepatectomy for HCC three years ago. She attended hospital because of neck discomfort. After various examinations, she was diagnosed with metastatic HCC. She survived after surgical resection of the affected side of the thyroid.
Although secondary malignant tumor of the thyroid is classified as distant metastasis, surgical resection is still necessary according to the patient's condition.
Core Tip: Thyroid metastasis after resection of hepatocellular carcinoma (HCC) is rare. We report a patient with isolated thyroid metastasis 3 years after surgery for HCC, and describe our clinical experience in its diagnosis and treatment. Based on this report and literature review, we suggest that surgical resection of the affected thyroid should be performed according to the patient’s condition.
- Citation: Zhong HC, Sun ZW, Cao GH, Zhao W, Ma K, Zhang BY, Feng YJ. Metastasis of liver cancer to the thyroid after surgery: A case report. World J Clin Cases 2022; 10(15): 5036-5041
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/5036.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.5036
There are a few reports of metastases to the thyroid gland[1,2]. Thyroid metastases from breast, melanoma, kidney, colorectal cancer and primary lung tumors have been reported, but there are few reports of metastasis from gastrointestinal malignancies[3-5]. Hepatocellular carcinoma (HCC) metastatic to the thyroid gland is particularly rare.
We report a case of liver cancer metastasis to the thyroid gland 3 years after partial hepatectomy, and review the literature regarding liver cancer metastases to the thyroid gland.
The patient complained of neck pain at admission.
The patient was a 42-year-old female who underwent surgical resection for liver cancer three years ago. She was hospitalized due to neck pain during sneezing.
The patient underwent left lateral hepatectomy for HCC three years ago. The postoperative pathology was HCC, pT2, N0, M0, stage II. No targeted drug treatment was administered after surgery.
No special personal history, no familial genetic disease.
A solid and painless 3 cm × 2 cm mass was palpable on the left thyroid lobe.
Thyroid function test showed that serum thyroid stimulating hormone, thyroglobulin antibody and hydroxyperoxidase antibody were higher than normal. Alpha fetoprotein (AFP) was 7016 ng/mL. Carcinoembryonic antigen, carbohydrate antigen 19-9, cancer antigen (CA) 242, CA50 and CA125 were all in the normal range.
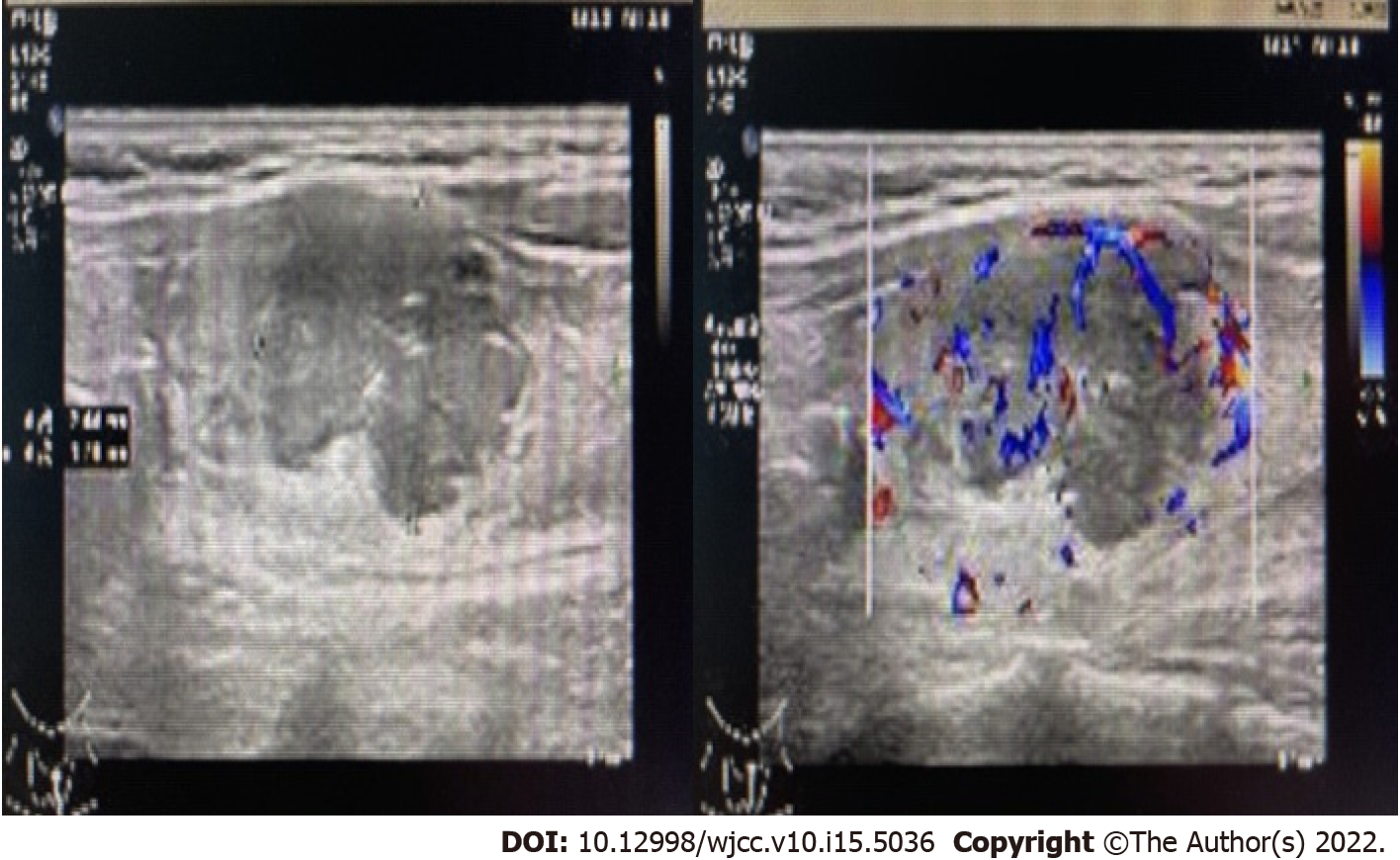
Thyroid color Doppler ultrasound showed hypoechoic nodules in the left lobe of the thyroid (TI-RADS 4b) and enlarged lymph nodes in the central area of the left neck (Figure 1). Fine needle biopsy (FNAB) of the thyroid gland was performed. The pathological results suggested a malignant tumor, and metastasis could not be ruled out. Positron emission tomography computed tomography (PET-CT) showed low-density nodules and increased metabolism in the left lobe of the thyroid. The maximum standardized uptake value was 4.0. Metastasis was considered No lymph node hypermetabolism was observed. At the same time, PET-CT showed changes in the left lateral lobe of the liver after operation, and no metabolic abnormalities were found.
HCC metastasis to the thyroid.
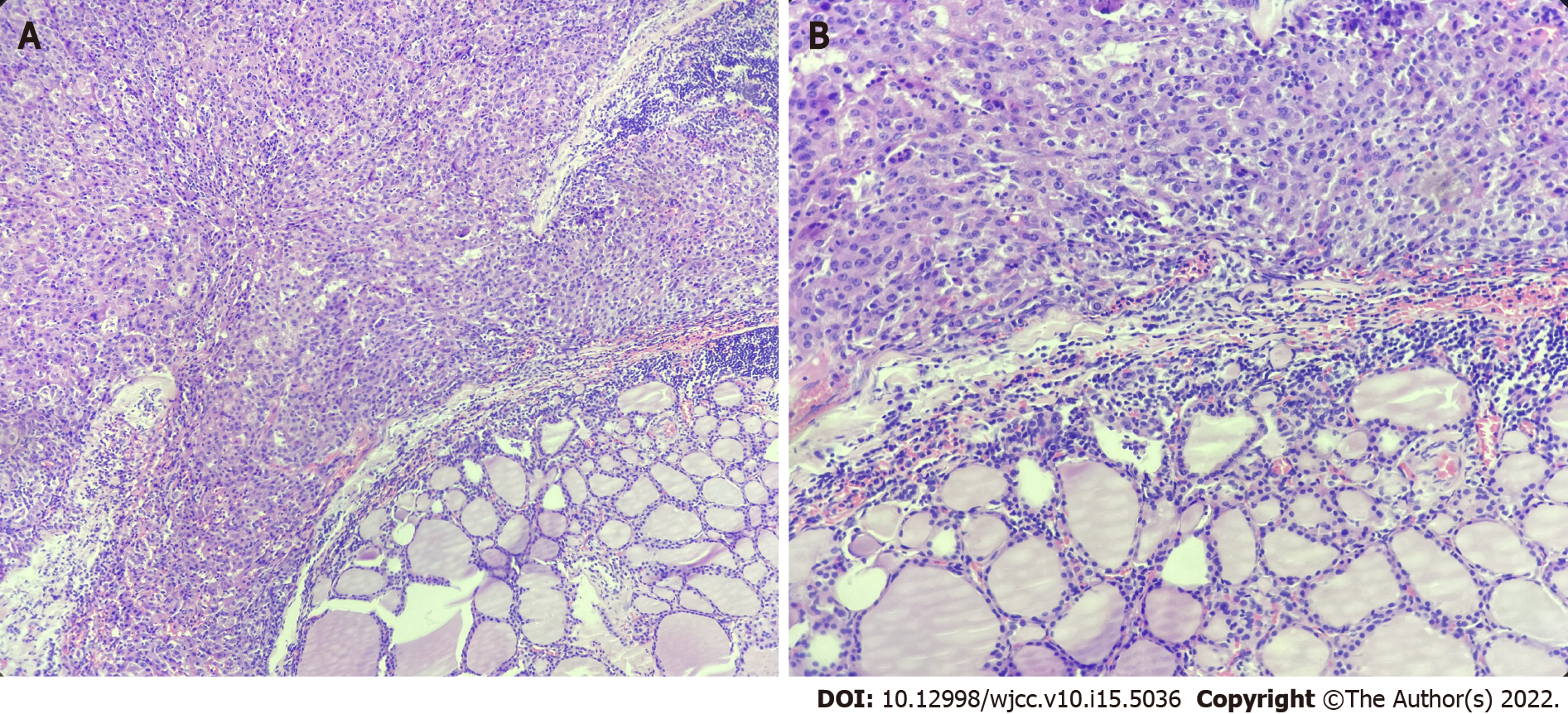
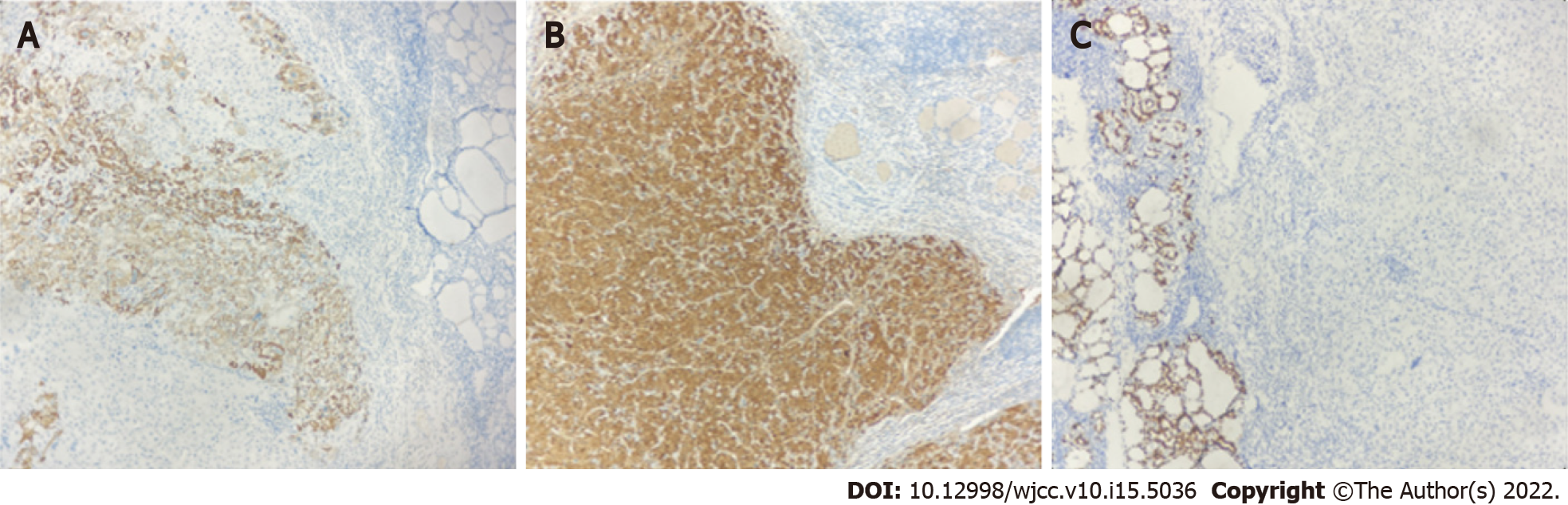
Left lobe thyroidectomy and central lymph node dissection were performed (Figure 2). Postoperative pathology showed metastatic HCC (Figure 3) and Hashimoto's thyroiditis in the surrounding thyroid, and a metastatic lymph node is around the tumor. Immunohistochemical examination was positive for hepatocytes and arginase-1, and negative for thyroid transcription factor-1 (Figure 4).
Both surgical and pathological findings confirmed HCC metastasis to the thyroid. No targeted therapy was given, and no recurrence was found 6 mo after thyroid gland resection.
Metastases to the thyroid gland are uncommon[4]. A case of metastatic urothelial carcinoma to the thyroid with bone metastasis was reported[3] in a 45-year-old female who underwent a rectal cancer resection five years ago. PET-CT showed thyroid lesions and lung metastasis. After partial pneumonectomy, the patient underwent partial thyroidectomy. Pathology and immunohistochemistry showed that the lesions originated from previous rectal cancer. The patient experienced no recurrence two years after thyroid surgery.
The presence of metastatic lesions to the thyroid usually indicates a poor prognosis, and most patients die shortly after diagnosis[6,7]. At the time of diagnosis of thyroid metastasis, 35% to 80% of patients with thyroid metastasis have metastatic diseases in other parts[1,8,9]. In such instances, treatment decisions should be individualized, as the effect of thyroidectomy on patients' overall prognosis is limited[10,11].
Mistelou et al[12] reviewed the autopsy records and pathological features of 36 cases of secondary thyroid tumors. Most of them were epithelial cancers. Lung was the most common primary tumor site (33.3%), followed by breast (8.33%) and kidney (8.33%). The most common non-epithelial malignancy was lymphoma, followed by leukemia (25%)[12].
Isolated thyroid metastasis has rarely been reported. Thomson reported two patients with solitary thyroid nodules, which were metastases from kidney and colon, respectively. One patient had a disease-free survival of more than 5 years after resection of solitary metastases[13].
It should be noted that active surgery for solitary thyroid metastases may improve the prognosis.
We report a patient with liver cancer diagnosed with thyroid metastasis 3 years after partial hepatectomy. Her thyroid was examined using ultrasound as neck discomfort was the first symptom. After thyroid biopsy, HCC was diagnosed. This is the first report of postoperative solitary metastasis of liver cancer to the thyroid gland.
Thyroid metastases are uncommon but can be detected with routine use of FNAB. They usually occur when there are metastases elsewhere, sometimes many years after the diagnosis of the primary tumor and generally have a poor prognosis[14].
In the differential diagnosis of these lesions, the patient's clinical history is the most important part. It should be emphasized that thyroid nodules found in patients with known cancer should be regarded as metastasis unless otherwise proved[15].
The recurrence and metastasis of liver cancer can be inferred according to an abnormality of AFP. PET-CT can be used to exclude other distant metastases and assist clinicians in determining the treatment plan.
Although distant metastasis is usually a marker of poor prognosis, thyroid metastasis does not seem to lead to worse results than metastasis to other sites[9]. Life expectancy mainly depends on the prognosis of primary tumors[9]. Solitary metastatic thyroid nodules may indicate a good clinical prognosis. Timely surgical resection may be beneficial to patients[16,17].
In our case, six months after surgery, the patient had not relapsed and is being followed up.
Although a secondary malignant tumor of the thyroid is classified as distant metastasis, some patients are accompanied by multiple metastases in the body, and the overall survival rate is low. However, surgical resection of the affected thyroid should be performed according to the patient's condition. The primary lesions and other metastases can be determined according to the medical history and auxiliary examinations (such as PET-CT, puncture biopsy, etc.). Thus, patients with thyroid nodules with a history of malignant tumors require a clear diagnosis to distinguish between primary thyroid cancer and metastasis. Solitary thyroid metastasis after liver cancer surgery is rare, but surgical resection after diagnosis may not affect the prognosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Casella C, Italy; Corrales FJ, Spain; Sudhamshu KC, Nepal; Ker CG, Taiwan S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Chung AY, Tran TB, Brumund KT, Weisman RA, Bouvet M. Metastases to the thyroid: a review of the literature from the last decade. Thyroid. 2012;22:258-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 182] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 2. | Watanabe I, Tsuchiya A. Secondary carcinoma of the thyroid gland. Jpn J Surg. 1980;10:130-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Mori K, Koinuma K, Nishino H, Horie H, Lefor AK, Sata N. Rectal cancer with a metastasis to the thyroid gland: A case report. Int J Surg Case Rep. 2020;66:39-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Tuncer M, Faydaci G, Altin G, Erdogan BA, Kibar S, Sanli A, Bilgici D. Metastasis of non-muscle-invasive bladder cancer into the thyroid gland: a literature review accompanied by a rare case. Korean J Urol. 2014;55:222-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Yamauchi M, Kai K, Shibamiya N, Shimazu R, Monji M, Suzuki K, Kakinoki H, Tobu S, Kuratomi Y. Didactic surgical experience of thyroid metastasis from renal cell carcinoma: A case report. World J Clin Cases. 2018;6:1018-1023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 6. | Aron M, Kapila K, Verma K. Role of fine-needle aspiration cytology in the diagnosis of secondary tumors of the thyroid--twenty years' experience. Diagn Cytopathol. 2006;34:240-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Pastorello RG, Saieg MA. Metastases to the Thyroid: Potential Cytologic Mimics of Primary Thyroid Neoplasms. Arch Pathol Lab Med. 2019;143:394-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Iesalnieks I, Winter H, Bareck E, Sotiropoulos GC, Goretzki PE, Klinkhammer-Schalke M, Bröckner S, Trupka A, Anthuber M, Rupprecht H, Raab M, Meyer W, Reichmann F, Kästel M, Mayr M, Braun W, Schlitt HJ, Agha A. Thyroid metastases of renal cell carcinoma: clinical course in 45 patients undergoing surgery. Assessment of factors affecting patients' survival. Thyroid. 2008;18:615-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Papi G, Fadda G, Corsello SM, Corrado S, Rossi ED, Radighieri E, Miraglia A, Carani C, Pontecorvi A. Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol (Oxf). 2007;66:565-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Montero PH, Ibrahimpasic T, Nixon IJ, Shaha AR. Thyroid metastasectomy. J Surg Oncol. 2014;109:36-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Wood K, Vini L, Harmer C. Metastases to the thyroid gland: the Royal Marsden experience. Eur J Surg Oncol. 2004;30:583-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 131] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 12. | Mistelou A, Papadatos SS, Kousi C, Lampri E, Mitsis M, Vougiouklakis T, Galani V. Thyroid Gland as a Target of Secondary Malignancies - an Autopsy Study and Review Data. Folia Med (Plovdiv). 2019;61:277-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Thomson JA, Kennedy JS, Browne MK, Hutchison J. Secondary carcinoma of the thyroid gland. Br J Surg. 1975;62:692-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Kim TY, Kim WB, Gong G, Hong SJ, Shong YK. Metastasis to the thyroid diagnosed by fine-needle aspiration biopsy. Clin Endocrinol (Oxf). 2005;62:236-241. [PubMed] |
| 15. | Schröder S, Wodzynski A, Padberg B. [Cytokeratin expression of benign and malignant epithelial thyroid gland tumors. An immunohistologic study of 154 neoplasms using 8 different monoclonal cytokeratin antibodies]. Pathologe. 1996;17:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Chen H, Nicol TL, Udelsman R. Clinically significant, isolated metastatic disease to the thyroid gland. World J Surg. 1999;23:177-80; discussion 181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 115] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Lin JD, Weng HF, Ho YS. Clinical and pathological characteristics of secondary thyroid cancer. Thyroid. 1998;8:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 77] [Article Influence: 2.9] [Reference Citation Analysis (0)] |