Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.4942
Peer-review started: September 30, 2021
First decision: January 11, 2022
Revised: January 20, 2022
Accepted: April 3, 2022
Article in press: April 3, 2022
Published online: May 26, 2022
Processing time: 236 Days and 0.7 Hours
Ewing’s sarcoma (ES) is a highly aggressive bone malignancy. Extraskeletal ES (EES) originating in the spinal canal is extremely rare. Herein, we report on a rare case of EES with a primary lumbar spinal nerve root including the complete diagnosis and treatment.
A young female patient presented with a complaint of right lower limb pain for 1 mo. Magnetic resonance imaging (MRI) revealed an 11 mm × 14 mm × 31 mm mass in the lumbar epidural region extending at the fifth lumbar spine (L5) level toward the right L5 neural foramen. Our initial diagnosis was an epidural schwannoma. The patient underwent total laminectomy, tumor resection and pedicle screw internal fixation and the L5 root tumor was found to have been completely removed intraoperatively. Histopathological examination of the lesion showed a typical ES with a large number of small, round cells. Immunohistochemistry analysis indicated positive CD99 and S100. After surgery, the patient received chemotherapy and radiotherapy with a 1 year of follow-up and no recurrent tumors or new lesions were found upon spine MRI and positron emission tomography/computed tomography reexamination.
Clinically, ES outside the bone should be considered when nerve root tumors are encountered inside and outside the spinal canal and the diagnosis should be determined by pathological biopsy. After surgical resection, chemotherapy and radiotherapy should be performed. After treatment, active follow-up and regular review should be completed.
Core Tip: Ewing’s sarcoma (ES) is a very aggressive primary bone malignancy. Extraskeletal ES (EES) itself is rare, and primary intraspinal EES is even rarer, accounting for only 5% of all ES cases. Within the spine, these malignancies are typically located in the paravertebral and epidural spaces. Both domestically and internationally, most reported cases of EES have been found in the spinal canal. Primary nerve root EES is rare with only a few cases reported. Involvement of the lumbar nerve roots in EES has not been previously reported. Herein, we report a case of EES with primary intramedullary lumbar 5 nerve root including complete diagnosis and treatment.
- Citation: Lei LH, Li F, Wu T. Primary extraskeletal Ewing’s sarcoma of the lumbar nerve root: A case report. World J Clin Cases 2022; 10(15): 4942-4948
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/4942.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.4942
Ewing’s sarcoma (ES) is a very aggressive primary bone malignancy. Extraskeletal ES (EES) in itself is rare, and primary intraspinal EES is even rarer, accounting for only 5% of all ES cases[1]. Within the spine, these malignancies are typically located in the paravertebral and epidural spaces. Both domestically and internationally, most reported cases of EES have been found in the spinal canal[2-4]. Primary nerve root EES is rare with only a few cases reported[4,5]. Involvement of lumbar nerve roots in EES has not been reported previously. Herein, we report on a case of EES with a primary intramedullary lumbar 5 nerve root location including complete diagnosis and treatment.
A young female patient (23-years-old) complained of pain in the right buttocks, posterolateral thigh and lateral leg over the previous month. She presented with protopathic pain, intolerance and difficulty in sleeping and walking. She reported no symptoms of perineal numbness, urinary incontinence or fecal incontinence.
The patient has no relevant medical history.
The patient has no history of past illness.
The patient has no history of personal and family illness.
Physical examination indicated that the right straight leg high test was positive 40° and the strengthening test was positive; the right tibial anterior muscle, hallux extensor muscle and fibula long muscle strengths were grade 4; sensation in the right lower limb was normal; the right Achilles tendon reflex was weakened; no pathological signs were observed. Visual analogue scale (VAS): 9 points.
Laboratory examinations were normal.
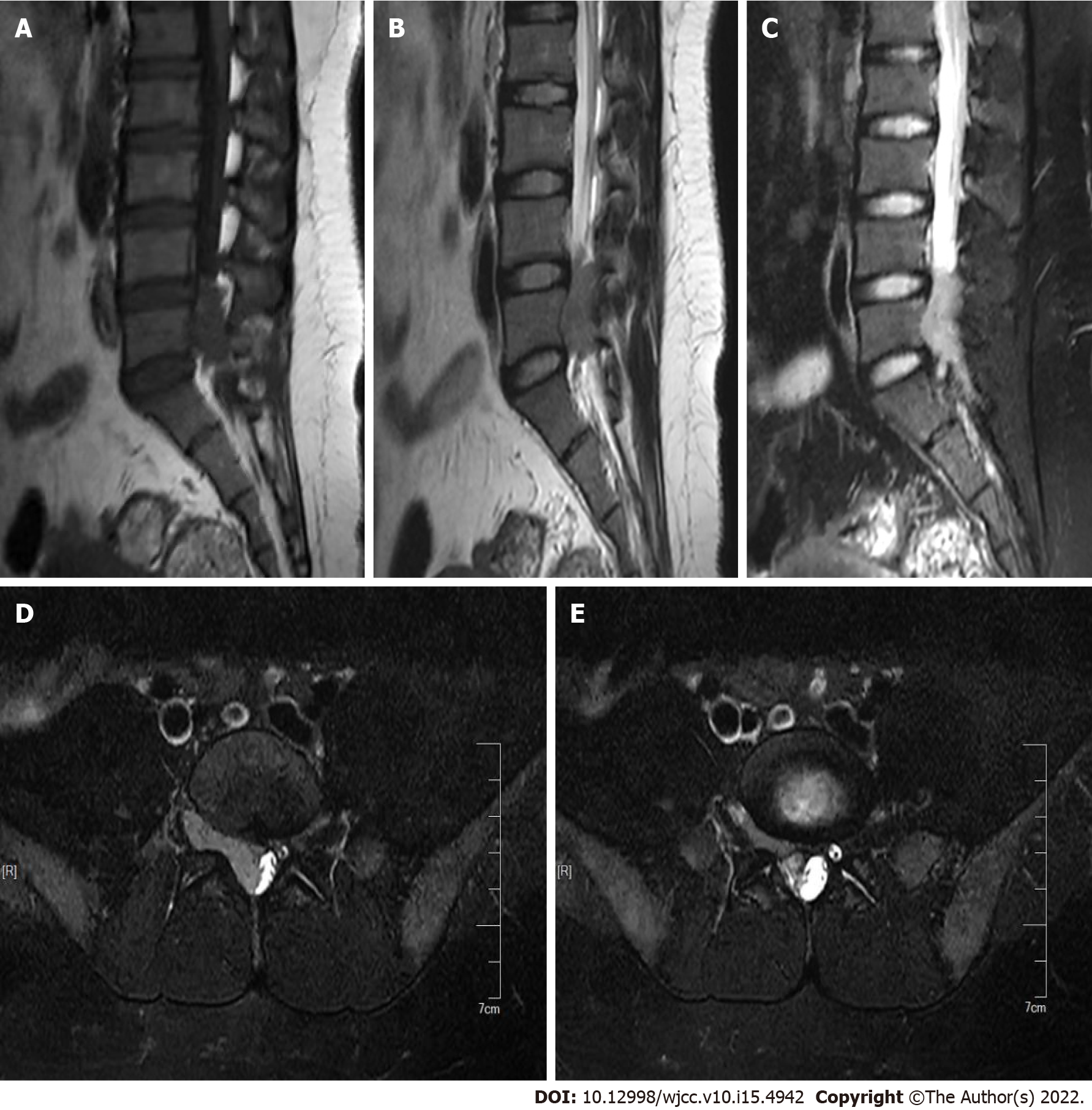
Preoperative X-ray, computed tomography (CT) and 3D reconstruction of the lumbar spine revealed no obvious abnormalities. Magnetic resonance imaging (MRI) examination showed normal signal in the lumbar body and intervertebral disc. At the level of the L4-5 vertebral body, there were abnormal lump-like signals in the vertebral canal, about 11 mm × 14 mm × 31 mm in size, extending to the right foraminal area. T1W1 showed low signal, T2W1 showed both slightly higher and lower signals with a few small nodular high signals, and short inversion time inversion-recovery (STIR) showed high signal. The subarachnoid space was compressed and narrowed in the corresponding plane and the adjacent dural sac and cauda equina terminus were compressed and deformed. The signal was normal and the diagnosis of schwannoma was considered (Figure 1).
The patient was diagnosed with schwannoma.
The patient was later diagnosed with EES.
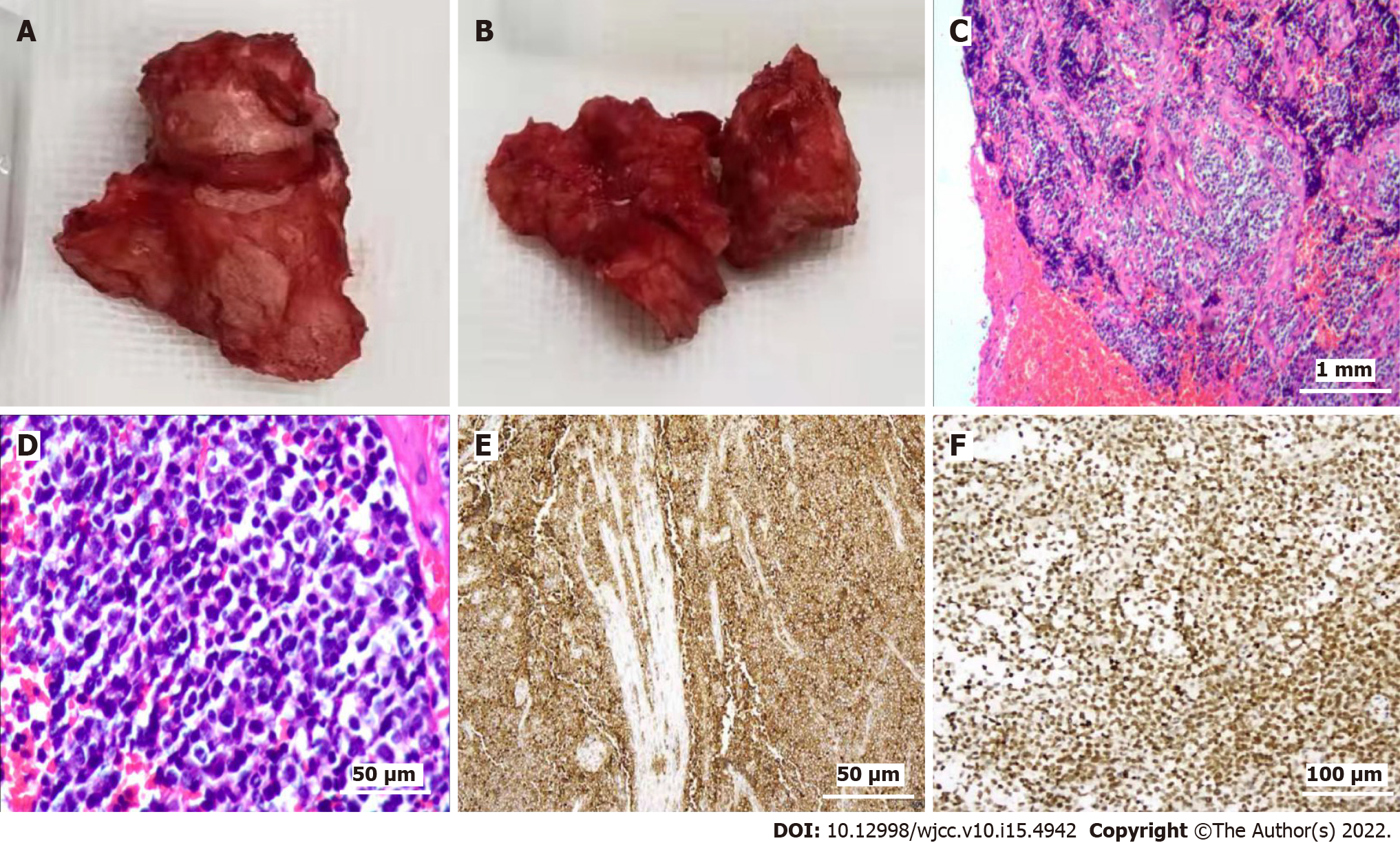
Based on departmental discussion, enhanced MRI examination was recommended to confirm the diagnosis. After communication with the patient, surgical treatment and disease diagnosis were performed. The patient underwent total laminectomy, tumor resection and pedicle screw internal fixation under general anesthesia. During the operation, a dark red, fish-like extradural mass was observed with clear boundaries ranging from the lower part of the lumbar 4-5 disc to the lumbar 5-sacral 1 intervertebral foramen with lateral recess outside and internal pressure on the dural sac. The right fifth lumbar spine (L5) nerve root was surrounded by a mass and the nerve root fibers were scattered, lacked obvious shape or boundary and could not be separated. Therefore, we determined that the tumor was primary to the L5 nerve root. On the right side, the L5 nerve root was ligated from the dural sac. The nerve root was excised, the distal end of the mass was separated and the distal nerve root was excised. The mass was completely resected and its size was determined to be approximately 3 cm × 1.5 cm × 0.6 cm (Figure 2A and B). Postoperatively, the pain in the patient’s right lower limb disappeared and muscle strength was not significantly weakened compared to pre-surgery levels. Skin tactile sensation was decreased in the lateral side of the right leg and the dorsal foot. Patient was not incontinent of urine or feces. Tissue diagnosis indicated a small round cell malignancy (Figure 2C-F). Immunohistochemistry results were as follows: CK-PAN (-); EMA (-); NSE (-); CD99 (+); CD57 (-); HMB-45 (-); Wt-1 (-); Melan A (-); Vimentin; Ki-67 (5%-10%); Desmin (-); MyoD1 (-); Myogenin (-); Syn (-); CgA (-); S100 (+); LCA (-); Msa (-). Combined with the results of examination and immunohistochemistry, the final diagnosis was EES. Further molecular biology analysis has not been done yet. Postoperative positron emission tomography/CT (PET/CT) examination showed changes to the vertebral body and surrounding soft tissues accompanied by an uneven increase in glucose metabolism. Based on postoperative changes, no metastatic lesions were observed. After discussion with the department of oncology, a chemotherapy scheme of isophoramide + etoposide was selected for administration. The patient-underwent six courses of chemotherapy and one course of radiotherapy (36 Gy) for the lumbosacral primary site and lymph drainage area.
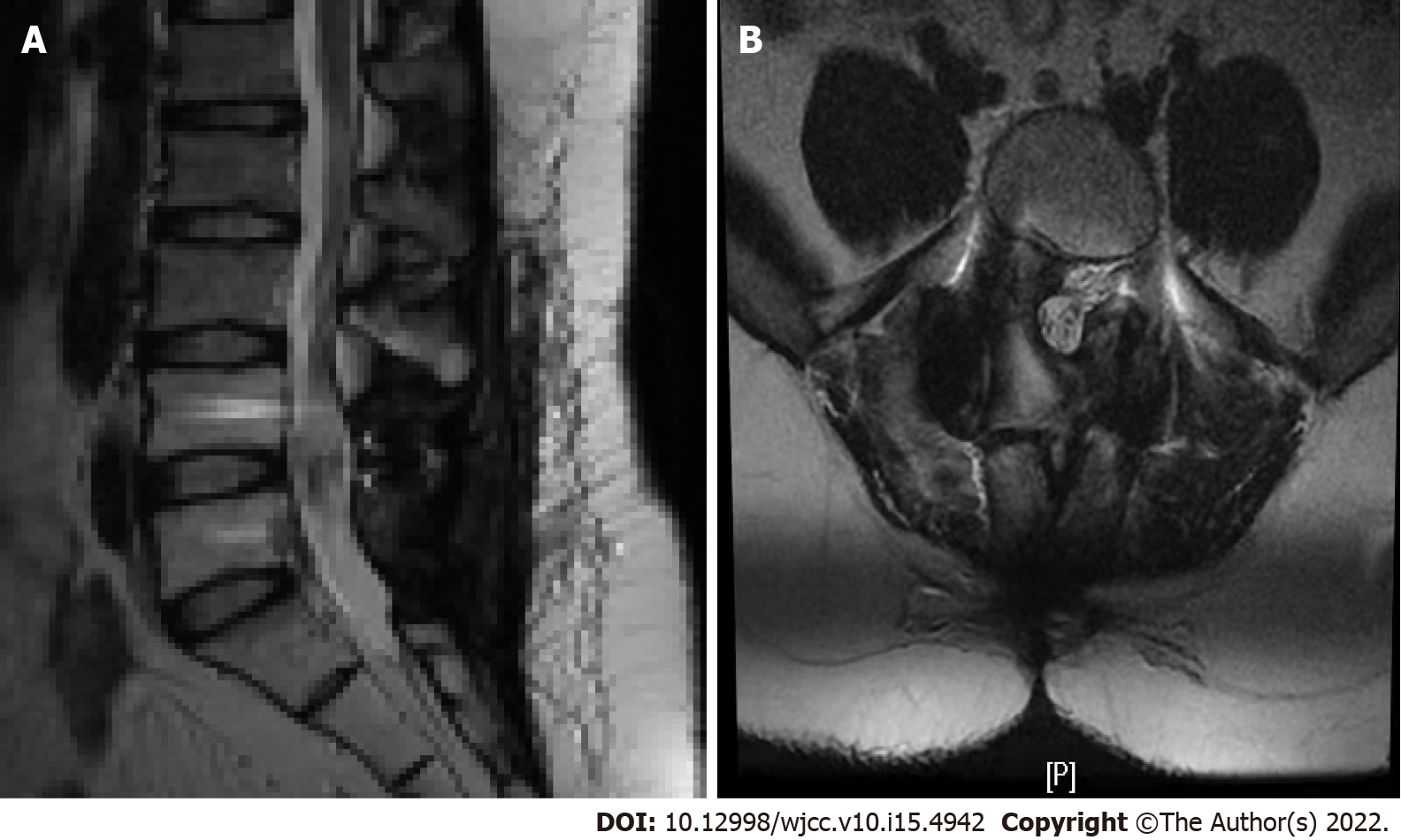
After 1 year and 3 mo of follow-up, the VAS score was 1 point. Reexamination by PET/CT showed no significant recurrent metabolic signs anywhere in the body. MRI examination showed that the space occupying the spinal canal at the L4-5 level had been removed and no obvious metabolic signs of recurrence were observed (Figure 3).
ES is a highly aggressive malignant tumor characterized by rapid growth, poor prognosis and a high recurrence rate. It often has no obvious early symptoms and late diagnosis is often based on feelings of soft tissue pain or swelling as lesions close to the nervous system usually compress the corresponding nerves and cause neurological dysfunction. Here, we report on a case of primary L5 EES of the nerve root. The patient’s disease progressed rapidly and presented with intolerable nerve root pain. ES has no obvious specific imaging signs but instead manifests differently based on the disease site, leading to a high misdiagnosis rate. According to reports in the literature, MRI of the seventh cervical vertebra (C7)-the second thoracic vertebra (T2) intraspinal extradural ES showed clear boundaries, T1 showed equivalent signal, and T2 showed slightly higher and uneven signal, with necrosis in the lesion and uneven enhancement capacity after enhancement[6]. MRI of L3-the first sacral vertebra (S1) intraspinal extradural ES showed a long strip of abnormal signal. ES in the spinal canal is rare and often presents as an extramedullary mass on MRI typically showing equal signal on T1W1 and equal or slightly higher signal on T2WI which can be significantly enhanced. If there is necrosis or cystic degeneration in the tumor, enhancement is uneven and adjacent bone can be invaded and destroyed. Soft tissue masses in the spinal canal may have exogenous tendencies. In this case, T1W1 presented low signal, T2W1 presented both slightly high and low signals, with a few small nodular high signals, and STIR presented high signal leading to a preoperative misdiagnosis as schwannoma. The diagnosis of ES is based on pathology. The staining revealed a large number of primitive small round cells with uneven morphology, reduced cytoplasm, hyperchromatic nuclei and atypical Homer-Wright structures around blood vessels. This case was pathologically diagnosed as a small round cell malignancy with the diagnosis refined to EES in combination with immunohistochemistry. With the progress of modern molecular biology technologies, genetic testing has become an important tool for identifying and clarifying suspicious cases[7,8]. The incidence of ES in the spinal canal is low and there is a lack of clinical case studies so no unified treatment exists at present. For clinical recommendations of “surgery combined with chemoradiotherapy” programs or chemotherapy programs, EES chemotherapy is currently recommended as the initial treatment program for skeletal ES. The malignant degree of this disease is high and the prognosis is very poor, with an approximate 2-year survival rate < 40% and approximate three-year survival rates < 10%. Key prognostic factors include pathological type, surgical resection range and tumor metastasis[9]. New treatment methods such as targeted therapies and hematopoietic stem cell transplantation require further investigation[10,11]. In recent years, in-depth research into the molecular mechanisms of Pnet/EWS and efficacy of immunotherapy has allowed the replication of tumor cells to be well-inhibited and the long-term survival rate of patients to be significantly improved[12]. In this case, following surgical resection combined with postoperative radiotherapy and chemotherapy, no obvious discomfort was reported during the 1-year follow-up with the exception of residual numbness on the lateral side of the right leg and a good curative effect was achieved. Due to the short follow-up time, however, we do not believe that the patient has been cured and the long-term efficacy of this treatment remains to be clarified.
Primary intraspinal EES of the lumbar nerve root is rarely reported. By comprehensively presenting the diagnosis and treatment process, this case report provides a general reference for improving clinicians’ understanding of EES, increasing preoperative diagnosis rates, preventing misdiagnosis, promoting early diagnosis and treatment and improving patient prognosis.
Clinically, when encountering nerve root tumors inside and outside the spinal canal, ES outside the bone should be considered and this diagnosis should be determined by pathological biopsy. After surgical resection, chemotherapy and radiotherapy should be performed. After treatment, active follow-up and regular review should be carried out.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Machado I, Spain; Nambi G, Saudi Arabia S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL
| 1. | Gong HS, Huang QS, Liu GJ, Chen FH, Zhao HB. Cervical Primary Ewing's Sarcoma in Intradural and Extramedullary Location and Skip Metastasis to Cauda Equina. Turk Neurosurg. 2015;25:943-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Karikari IO, Mehta AI, Nimjee S, Hodges TR, Tibaleka J, Montgomery C, Simpson L, Cummings TJ, Bagley CA. Primary intradural extraosseous Ewing sarcoma of the spine: case report and literature review. Neurosurgery. 2011;69:E995-E999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Benesch M, Sperl D, von Bueren AO, Schmid I, von Hoff K, Warmuth-Metz M, Ferrari R, Lassay L, Kortmann RD, Pietsch T, Rutkowski S. Primary central nervous system primitive neuroectodermal tumors (CNS-PNETs) of the spinal cord in children: four cases from the German HIT database with a critical review of the literature. J Neurooncol. 2011;104:279-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Scantland JT, Gondim MJ, Koivuniemi AS, Fulkerson DH, Shih CS. Primary Spinal Intradural Extraosseous Ewing Sarcoma in a Pediatric Patient: Case Report and Review of the Literature. Pediatr Neurosurg. 2018;53:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Kim JW, Lee J, Kim JH. Extraskeletal Ewing’s Sarcoma of the Thoracic Nerve Root: A Case Report. J Korean Soc Radiol. 2019;80 (3):568-573. [DOI] [Full Text] |
| 6. | Tan XL, Xu YK, Peng H. Imaging analys is of Ewing’s sarcoma. Chin Clin Med Imaging. 2012;23 (1):59-62. |
| 7. | Allegretti M, Casini B, Mandoj C, Benini S, Alberti L, Novello M, Melucci E, Conti L, Covello R, Pescarmona E, Milano GM, Annovazzi A, Anelli V, Ferraresi V, Biagini R, Giacomini P. Precision diagnostics of Ewing's sarcoma by liquid biopsy: circulating EWS-FLI1 fusion transcripts. Ther Adv Med Oncol. 2018;10:1758835918774337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Bashir MR, Pervez S, Hashmi AA, Irfan M. Frequency of Translocation t(11;22)(q24;q12) Using Fluorescence In Situ Hybridization (FISH) in Histologically and Immunohistochemically Diagnosed Cases of Ewing's Sarcoma. Cureus. 2020;12:e9885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Virani MJ, Jain S. Primary intraspinal primitive neuroectodermal tumor (PNET): a rare occurrence. Neurol India. 2002;50:75-80. [PubMed] |
| 10. | Stewart E, Goshorn R, Bradley C, Griffiths LM, Benavente C, Twarog NR, Miller GM, Caufield W, Freeman BB 3rd, Bahrami A, Pappo A, Wu J, Loh A, Karlström Å, Calabrese C, Gordon B, Tsurkan L, Hatfield MJ, Potter PM, Snyder SE, Thiagarajan S, Shirinifard A, Sablauer A, Shelat AA, Dyer MA. Targeting the DNA repair pathway in Ewing sarcoma. Cell Rep. 2014;9:829-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 141] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 11. | Gaspar N, Rey A, Bérard PM, Michon J, Gentet JC, Tabone MD, Roché H, Defachelles AS, Lejars O, Plouvier E, Schmitt C, Bui B, Boutard P, Taque S, Munzer M, Vannier JP, Plantaz D, Entz-Werle N, Oberlin O. Risk adapted chemotherapy for localised Ewing's sarcoma of bone: the French EW93 study. Eur J Cancer. 2012;48:1376-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Meng XT, He SS. Primitive neuroectodermal tumor in the spinal canal: A case report. Oncol Lett. 2015;9:1934-1936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |