Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.4776
Peer-review started: December 5, 2021
First decision: December 27, 2021
Revised: January 7, 2022
Accepted: March 26, 2022
Article in press: March 26, 2022
Published online: May 26, 2022
Processing time: 170 Days and 4.7 Hours
Cervical degenerative disc (CDD) disease is a common type of spondylosis. Although anterior cervical discectomy and fusion (ACDF) is the preferred treatment for CDD disease, internal fixation with a titanium plate may cause various complications. The invention of the ACDF with a self-locking fusion cage (ROI-C) has effectively decreased the incidence of postoperative complications.
To observe the outcomes of CDD disease treated by ACDF with a ROI-C.
Ninety patients with CDD disease treated at our hospital from March 2019 to March 2021 were included. They were divided into two groups (control group and observation group, n = 45 in each) using a random number table. Patients in the control group received ACDF plus internal fixation with a titanium plate. Those in the observation group received ACDF + ROI-C placement. The two groups of patients were compared in terms of surgical parameters, pain, cervical spine function, range of motion, and complications.
The two groups of patients showed no significant differences in surgical time, blood loss, drainage volume, and length of hospital stay (P > 0.05). No significant differences in the visual analogue scale (VAS), Japanese Orthopedic Association (JOA), and neck disability index (NDI) scores were observed between the two groups before surgery (P > 0.05). The VAS and NDI scores in the observation group were considerably lower than those in the control group after surgery; however, the JOA scores in the observation group were significantly higher than those in the control group (P < 0.05). No significant differences were observed in cervical disc height and the range of motion of the superior or inferior adjacent vertebrae between the two groups before surgery (P > 0.05). The disc height in the observation group was larger than that in the control group after surgery. The range of motion of both the superior and inferior adjacent vertebrae was significantly smaller in the observation group than in the control group (P < 0.05). The incidence of complications was only 2.22% in the observation group compared to 15.56% in the control group, and the difference was statistically significant (P < 0.05).
Cervical spine function restoration was better with ROI-C with internal fixation in ACDF than with conventional titanium plates in ACDF for CDD disease.
Core Tip: Self-locking fusion cage (ROI-C) with internal fixation showed similar efficacy to conventional titanium plates in anterior cervical discectomy and fusion (ACDF) for cervical degenerative disc disease. However, cervical spine function restoration was better with the former than with the latter. The ROI-C featuring VerteBRIDGE plates is worthy of clinical application. The pain and complications were less common using ROI-C compared with conventional titanium plates in ACDF. The range of motion of the cervical spine was not increased significantly after using ROI-C.
- Citation: Zhang B, Jiang YZ, Song QP, An Y. Outcomes of cervical degenerative disc disease treated by anterior cervical discectomy and fusion with self-locking fusion cage. World J Clin Cases 2022; 10(15): 4776-4784
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/4776.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.4776
The incidence of spondylosis has been increasing in recent years as people experience more stress in a rapidly developing society. In addition, spondylosis has become more common in younger populations. Cervical degenerative disc (CDD) disease is a common type of spondylosis. At present, anterior cervical discectomy and fusion (ACDF) is the preferred treatment for CDD disease and is widely accepted as the gold standard treatment. A titanium plate is generally used in ACDF for internal fixation[1,2]. Although ACDF is extensively performed, it has been noted that internal fixation with a titanium plate may cause various postoperative complications, such as pseudarthrosis, loosening of the internally fixed plates, and dysphagia. These disorders may seriously affect the life quality and prognosis of patients[3,4].
In recent years, we have witnessed a growing demand for healthcare. The conventional ACDF + internal fixation using a titanium plate is no longer adequate. Reducing postoperative complications and improving the therapeutic effect have long been topics of interest[5,6]. The invention of the ACDF with a self-locking fusion cage (ROI-C) has effectively decreased the incidence of postoperative complications and has drawn increasing attention[7,8]. In the present study, we further investigated the efficacy of ACDF using ROI-C for internal fixation in CDD disease. Patients with CDD disease treated at our hospital received the conventional ACDF using either a titanium plate or ROI-C for internal fixation. The effect of this technique on patient prognosis was analyzed. The findings offer theoretical clues for the treatment of CDD disease.
Ninety patients with CDD disease treated at our hospital from March 2019 to March 2021 were retrospectively analyzed. The present study was approved by the hospital ethics committee. The patients were divided into two groups (control group and observation group, n = 45 in each) using a random number table. The control group consisted of 25 males and 20 females aged 26-75 years (average 42.3 ± 5.2 years). With regard to the vertebrae affected, one segment was affected in 38 patients, and two affected in 7 patients. As to the type of spondylosis, 25 patients were affected at the nerve roots, 12 patients in the spinal cord, and 8 patients were of mixed type. The observation group consisted of 26 males and 19 females aged 28-79 years (average 43.4 ± 5.3 years). With regard to the vertebrae affected, one segment was affected in 36 patients, and two affected in 9 patients. As to the type of spondylosis, 24 patients were affected at the nerve roots, 14 patients in the spinal cord, and 7 patients were of mixed type. There were no significant differences in terms of gender, age, number of segments affected, and type of spondylosis between the two groups (P > 0.05).
Inclusion criteria were: (1) Conformed to the diagnostic criteria for CDD disease according to examinations and clinical signs[9]; (2) voluntarily engaged in the present study and signed an informed consent; (3) unresponsive to conservative treatment; and (4) indicated for cervical spine surgery via the anterior approach.
Exclusion criteria were: (1) Cervical deformity; (2) combined with osteoporosis; (3) history of cervical spine surgery; (4) combined with severe diseases that might influence the results of the present study, such as malignancies; and (5) participating in other studies during the same period.
Patients in the control group received ACDF plus a titanium plate for internal fixation. The patients were placed in the supine position. General anesthesia was performed after tracheal intubation. The head was immobilized in a neutral position, and the neck was slightly moved backward. A transverse incision of approximately 6 cm was made in the right anterior cervical region. The skin was cut open, and the platysma muscle was transected. The muscle flap was pulled down. Blunt dissection was performed at the intermuscular space between the sternocleidomastoid muscle and sternothyroid. The omohyoid muscle was exposed and then dissociated, ligated, and severed. The esophagus and trachea were pushed to the left. External traction was applied to the sternocleidomastoid muscle and carotid sheath to expose the prevertebral fascia. The relevant segment was located by a C-arm X-ray. A longitudinal incision was made in the prevertebral fascia to peel it up and down slowly. The range of peeling did not exceed the medial margin of the longus colli muscle by 3 mm. Two distraction screws were inserted into the middle of the superior and inferior vertebrae adjacent to the lesioned segment, respectively. The distractor was mounted on the screws to separate the vertebral bodies. The anterior longitudinal ligament was cut open and peeled off to the two sides. The fibrous ring was exposed and cut open using a long-handled scalpel. Blunt dissection was performed up and down to remove the intervertebral disc. Autologous bone was placed into the intervertebral space. A titanium anterior cervical plate of an appropriate length was inserted for internal fixation. The implant position was confirmed again by C-arm X-ray, and locking screws were inserted for internal fixation. A drainage tube was placed after surgery, and the incision was closed.
Patients in the observation group received ACDF + ROI-C placement for internal fixation. The first few steps were the same as those in the control group until the intervertebral disc was removed. Then trialing began to select an implant of the appropriate size. After filling with autologous bone, the implant was inserted into the intervertebral space. The implant position was confirmed by C-arm X-ray. Subsequently, two ROI-C VerteBRIDGE plates were tapped in for immobilization. A drainage tube was placed after surgery, and the incision was closed. The autologous bone from the resected osteophytes and decompression were used for intraoperative bone grafting in the two groups.
The two groups of patients were compared in terms of the following surgical parameters: Surgical time, blood loss, drainage volume, and length of hospital stay, in addition to pain, cervical spine function, range of motion, and complications. The visual analogue scale (VAS) was used to assess pain, and the patients were scored on a 0-10 scale. The higher the VAS score, the more severe the pain[10]. Cervical spine function was assessed using the Japanese Orthopedic Association (JOA) score[11] and the neck disability index (NDI)[12]. The total JOA score ranged from 0 to 29. The lower the score, the more severe the dysfunction. NDI is a 10-item questionnaire, and each item is scored from 0 to 5. The total index = [total score/(number of items responded by patients × 5)] 100%. The higher the NDI, the more severe the dysfunction. The cervical range of motion covered cervical disc height and the range of motion of inferior and superior adjacent vertebrae.
Statistical analysis was performed using the SPSS 18.0 software (Chicago, IL, United States). Measurements were expressed as mean ± SD, and t test was used for intergroup comparison of measurement data. Counts were expressed as percentages (%), and the χ2test was used for intergroup comparison of count data. P < 0.05 indicated a significant difference.
Surgical time, blood loss, drainage volume, and length of hospital stay were not significantly different between the two groups of patients (P > 0.05, Table 1).
| Group | Surgical time (min) | Blood loss (mL) | Drainage volume (mL) | Length of hospital stay (d) |
| Control group | 86.25 ± 13.46 | 46.03 ± 8.72 | 15.12 ± 2.67 | 14.69 ± 2.85 |
| Observation group | 88.17 ± 14.24 | 46.94 ± 8.83 | 16.03 ± 2.84 | 14.37 ± 2.74 |
| t | 0.657 | 0.492 | 1.566 | 0.543 |
| P value | > 0.05 | > 0.05 | > 0.05 | > 0.05 |
No significant differences in the VAS, JOA, and NDI scores were observed between the two groups before surgery (P > 0.05). The VAS and NDI scores in the observation group were considerably lower than those in the control group after surgery; however, the JOA scores in the observation group were significantly higher than those in the control group (P < 0.05, Table 2).
| Group | VAS score | JOA score | NDI (%) | |||
| Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | |
| Control group | 5.42 ± 1.06 | 1.95 ± 0.48 | 8.94 ± 2.18 | 13.26 ± 3.35 | 33.82 ± 6.43 | 14.56 ± 2.84 |
| Observation group | 5.38 ± 1.05 | 1.03 ± 0.29 | 9.03 ± 2.19 | 18.71 ± 3.62 | 33.79 ± 6.36 | 8.92 ± 2.33 |
| t | 0.180 | 11.005 | 0.195 | 7.412 | 0.022 | 10.299 |
| P value | > 0.05 | < 0.05 | > 0.05 | < 0.05 | > 0.05 | > 0.05 |
No significant differences were observed in cervical disc height and the range of motion of the superior and inferior adjacent vertebrae between the two groups before surgery (P > 0.05). The cervical disc height in the observation group was larger than that in the control group after surgery. The range of motion of both the superior and inferior adjacent vertebrae was significantly smaller in the observation group than in the control group (P < 0.05, Table 3).
| Group | Disc height (mm) | Range of motion of the superior adjacent vertebra (°) | Range of motion of the inferior adjacent vertebra (°) | |||
| Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | |
| Control group | 5.26 ± 0.72 | 7.24 ± 0.78 | 10.32 ± 2.64 | 15.28 ± 4.43 | 10.29 ± 2.56 | 15.37 ± 4.21 |
| Observation group | 5.31 ± 0.75 | 7.68 ± 0.85 | 10.38 ± 2.65 | 11.74 ± 2.96 | 10.33 ± 2.62 | 12.18 ± 3.15 |
| t | 0.323 | 2.559 | 0.108 | 4.457 | 0.073 | 4.070 |
| P value | > 0.05 | < 0.05 | > 0.05 | < 0.05 | > 0.05 | < 0.05 |
Complications in the two groups included dysphagia, loosening of the internally fixed implant, and infection. The incidence of these complications was only 2.22% in the observation group compared to 15.56% in the control group, and the difference was statistically significant (P < 0.05, Table 4).
| Group | Dysphagia | Loosening of the internally fixed implant | Infection | Incidence, n (%) |
| Control group | 3 | 3 | 1 | 7 (15.56) |
| Observation group | 0 | 1 | 0 | 1 (2.22) |
| χ2 | - | - | - | 4.939 |
| P value | - | - | - | < 0.05 |
The pathogenesis of CDD disease has not yet been fully clarified. Some scholars attribute this disease to the natural degeneration of intervertebral discs[13,14]. Others propose that it is associated with biomechanical changes in the adjacent vertebrae after surgery[15,16]. ACDF is a common treatment for cervical disc disorders. Several procedures have been proposed for ACDF. For example, ACDF with autologous bone grafting, allogenic bone grafting, anterior steel plate placement, or an intervertebral fusion cage has been widely used. No significant difference in the fusion rate has been reported with different ACDF procedures. However, differences have been observed in the incidence of complications and postoperative recovery[17-19].
ACDF with internal fixation using a steel plate is one of the most common choices. Although the steel plate improves cervical stability and promotes bone fusion, the anterior placement of a steel plate requires a larger surgical field. Therefore, the esophagus, trachea, and nerves are more likely to be damaged, leading to postoperative complications[20]. In addition, screw insertion may damage the spinal cord and vertebral artery, leading to long-term complications, such as screw loosening and steel plate dislocation[21]. How to improve the therapeutic effect of ACDF and reduce complications has been a long-standing concern. In recent years, an increasing number of reports have emerged concerning the use of an intervertebral fusion cage in ACDF, and the outcome is generally good[22-24].
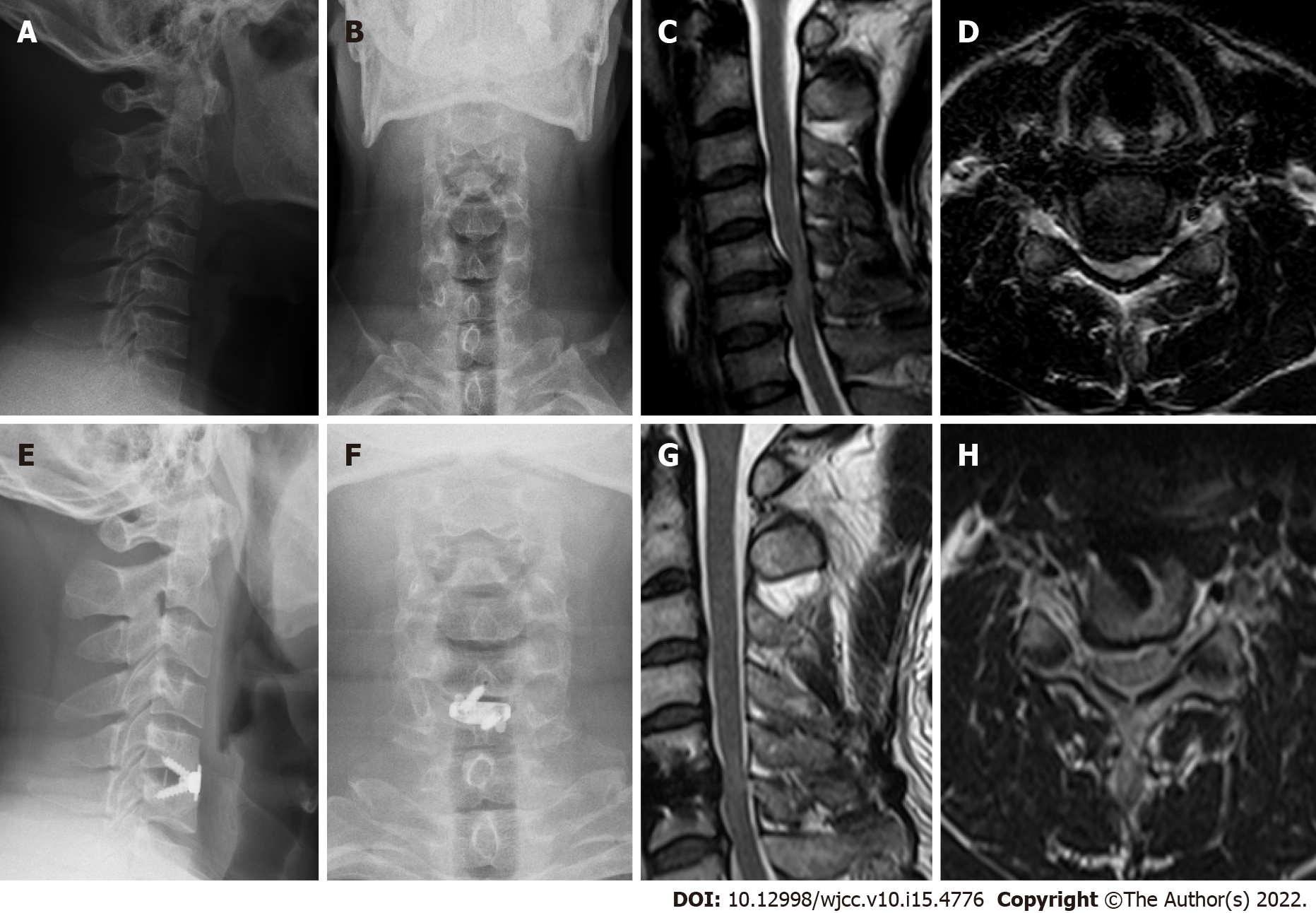
We recruited patients with CDD disease treated at our hospital by ACDF using either a conventional titanium plate or ROI-C for internal fixation. The results showed that surgical time, blood loss, drainage volume, and length of hospital stay were not significantly different between the two groups of patients. This was because the first few steps of the surgical procedures were similar between the two groups (Figure 1) and the steps following removal of the intervertebral disc were different. In the control group, the patients received internal fixation using a titanium plate after autologous bone grafting. In the observation group, autologous bone was first placed into the implant, which was then inserted into the intervertebral space. Both procedures were easy. There were no significant differences in surgical time, blood loss, postoperative drainage volume, and length of hospital stay between the two groups. Pain and cervical spine function were assessed in the two groups. The VAS scores and NDI were lower in the observation group than in the control group, while the JOA scores were higher in the former than in the latter. These results indicated that pain was relieved more after surgery in the observation group, hence the cervical spine function was better. The cervical range of motion in the two groups was examined, and it was found that the cervical disc height was larger in the observation group than in the control group. The range of motion of both the superior and inferior adjacent vertebrae was significantly smaller in the observation group than in the control group. These results indicated that the cervical disc height was improved considerably in the observation group after surgery, with the range of motion in adjacent vertebrae mildly affected.
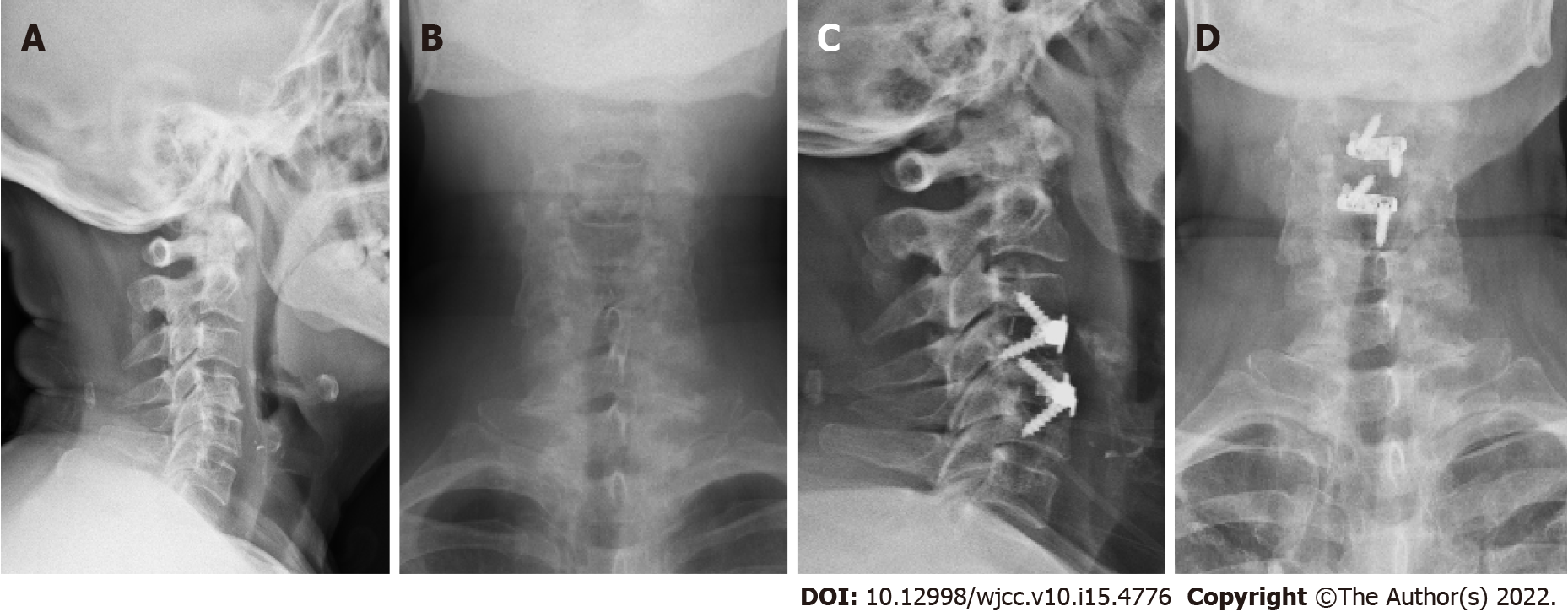
The intervertebral fusion cage can maintain lordosis and a normal range of motion and prevent kyphosis. Thus, the intervertebral fusion cage plays an important role in relieving postoperative pain and improving cervical spine functions[25,26]. The intervertebral fusion cage involves slight peeling of the anterior longitudinal ligament, with only exposure of the intervertebral space in the segment to be operated. The screws were inserted at an oblique angle into the endplate through the intervertebral space (Figure 2). In this way, the adverse influence on the adjacent vertebrae is minimized, especially the range of motion of adjacent vertebrae[27,28]. The vertebral bodies are separated using a distractor before inserting the intervertebral fusion cage, which is conducive to restoring the vertebral height. An intervertebral fusion cage insertion reduces height loss of the vertebral body, relieves nerve root compression, and avoids degeneration of adjacent vertebrae[29,30].
In the present study, it was also found that the incidence of postoperative complications was significantly lower in the observation group than in the control group. This was because two VerteBRIDGE plates were used with ROI-C. These self-locking plates were inserted into the superior and inferior vertebrae, respectively, to immobilize the implant more effectively. As the implant is more firmly immobilized by the VerteBRIDGE plates, postoperative complications are generally reduced.
Taken together, ROI-C with internal fixation showed similar efficacy to conventional titanium plates in ACDF for CDD disease. However, cervical spine function restoration was better with the former than with the latter. The range of motion of the cervical spine was not increased significantly after using ROI-C. Nevertheless, pain and complications were less common using ROI-C. Given the above advantages, the ROI-C featuring VerteBRIDGE plates is worthy of clinical popularization.
The conventional anterior cervical discectomy and fusion (ACDF) + internal fixation using a titanium plate is no longer adequate. The invention of the ACDF with a self-locking fusion cage (ROI-C) has effectively decreased the incidence of postoperative complications after ACDF and has drawn increasing attention.
To evaluate the efficacy of ROI-C.
To observe the outcomes of cervical degenerative disc (CDD) disease treated by ACDF with ROI-C.
Ninety patients with CDD disease treated at our hospital from March 2019 to March 2021 were included. They were divided into two groups (n = 45 in each) using a random number table. Patients in the control group received ACDF plus internal fixation with a titanium plate. Those in the observation group received ACDF + ROI-C placement. The two groups of patients were compared in terms of surgical parameters, pain, cervical spine function, range of motion, and complications.
The two groups of patients showed no significant differences in surgical time, blood loss, drainage volume, and length of hospital stay (P > 0.05). No significant differences in the visual analogue scale (VAS), Japanese Orthopaedic Association (JOA), and neck disability index (NDI) scores were observed between the two groups before surgery (P > 0.05). The JOA scores in the observation group were significantly higher than those in the control group (P < 0.05). No significant differences were observed in cervical disc height and the range of motion of the superior or inferior adjacent vertebrae between the two groups before surgery (P > 0.05). The range of motion of both the superior and inferior adjacent vertebrae was significantly smaller in the observation group than in the control group (P < 0.05). The incidence of complications was only 2.22% in the observation group compared to 15.56% in the control group, and the difference was statistically significant (P < 0.05).
The use of ROI-C with internal fixation in ACDF had similar efficacy to the use of conventional titanium plates in ACDF for CDD disease. However, cervical spine function restoration after using ROI-C was better than the control. The range of motion of the cervical spine was not increased significantly after using ROI-C, but pain and complications were less common. The ROI-C featuring the VerteBRIDGE plate is worthy of clinical popularization.
The long-term efficacy of ROI-C still needs to be evaluated.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kwon YM, United States; Maer T, United States S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL
| 1. | Chai YW, Yu XG, Shen GR. Efficacy of anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion (ACCF). Zhongguo Laonianxue Zazhi. 2021;41 (2):284-287. |
| 2. | Li N, Zhou Y, Liu M, Liu YT, Huang D, Xin B. Comparison of zero-profile anchored spacer ROI-C and traditional fusion cage combined with titanium plate in ACDF. Xuzhou Yike Daxue Xuebao. 2021;41 (1):45-50. |
| 3. | Coric D, Guyer RD, Nunley PD, Musante D, Carmody C, Gordon C, Lauryssen C, Boltes MO, Ohnmeiss DD. Prospective, randomized multicenter study of cervical arthroplasty versus anterior cervical discectomy and fusion: 5-year results with a metal-on-metal artificial disc. J Neurosurg Spine. 2018;28:252-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 4. | He JB, Liu H, Wu YK, Wang BN, Hong Y, Rong X. Biomechanical analysis of anterior cervical discectomy and fusion versus cervical disc arthroplasty for skip-level cervical disc herniation: a finite element study. Jizhu Waike Zazhi. 2021;19 (1):38-45. |
| 5. | Su QH, Chen T, Zhang Y, Zhang JB, Tan J, Guo S. Radiological changes of postoperative cervical disc height and overall curvature after single-level anterior cervical discectomy and fusion. Tongji Daxue Xuebao (Yixueban). 41 (1):100-106. |
| 6. | Hirvonen T, Siironen J, Marjamaa J, Niemelä M, Koski-Palkén A. Anterior cervical discectomy and fusion in young adults leads to favorable outcome in long-term follow-up. Spine J. 2020;20:1073-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Bai XF, Li L, He GL, Yin XH. The study on the short- and long-term efficacy of anterior cervical discectomy and fusion in patients with cervicalspondylotic radiculopathy aged below 35. Shanxi Yiyao Zazhi. 2019;48 (23):2870-2872. |
| 8. | Wang XP, Gai L, Jia W, Zhang K, Qiu YJ. Comparison of intraoperative preservation versus resection of the uncovertebral joint in anterior cervical discectomy and fusion. Zhongguo Gu Yu Guanjie Sunshang Zazhi. 2020;35 (1):32-34. |
| 9. | Peng JC, Tang YC, Zhang SC, Yang ZD, Zhou TP, Luo PJ, Wen GW, Xu YR, Ma YH. Comparison of postoperative degeneration of adjacent vertebrae after internal fixation and fusion using zero-profile fusion cage versus conventional titanium plate following anterior cervical decompression. Zhongguo Jisui Jizhu Zazhi. 2020;30 (5):417-426. |
| 10. | Liu B, Liu X, Chen Y, Wang G, Shen X, Liu H, Liao X. Clinical effect observation of intravenous application of zoledronic acid in patients with cervical spondylosis and osteoporosis after anterior cervical discectomy and fusion: A randomized controlled study. J Orthop Surg (Hong Kong). 2019;27:2309499019847028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | He S, Feng H, Lan Z, Lai J, Sun Z, Wang Y, Wang J, Ren Z, Huang F, Xu F. A Randomized Trial Comparing Clinical Outcomes Between Zero-Profile and Traditional Multilevel Anterior Cervical Discectomy and Fusion Surgery for Cervical Myelopathy. Spine (Phila Pa 1976). 2018;43:E259-E266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | Li YW, Wang HJ, Cui W, Li C, Zhou P, Xiao W, Wen Y, Hu BT, Li F, Zhao SX. Comparison of the efficacy of ACDF in the treatment of cervical spondylotic myelopathy using 3D printed intervertebral fusion cage and polyether-ether-ketone (PEEK) intervertebral fusion cage. Zhongguo Jisui Jizhu Zazhi. 2021;31 (1):16-24. |
| 13. | Zhao CM, Chen Q, Zhang Y, Huang AB, Ding WY, Zhang W. Anterior cervical discectomy and fusion versus hybrid surgery in multilevel cervical spondylotic myelopathy: A meta-analysis. Medicine (Baltimore). 2018;97:e11973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Chen JX, Zhang ZC, Shi W. Treatment of multilevel cervical spondylotic myelopathy with modified single-segment anterior cervical corpectomy and fusion and anterior cervical discectomy and fusion. Jizhu Waike Zazhi. 2021;19 (2):94-99. |
| 15. | Lim S, Haider S, Zakaria H, Chang V. Comparison of 30-day outcome following anterior cervical discectomy and fusion with or without instrumentation for cervical spondylosis: A review of 2352 elective cases. Surg Neurol Int. 2019;10:246. [PubMed] |
| 16. | Burkhardt BW, Kerolus MG, Witiw CD, David BT, Traynelis VC, Fessler RG. Comparison of radiographic parameters after anterior cervical discectomy and fusion with semiconstrained translational versus rotational plate systems. Clin Neurol Neurosurg. 2019;183:105379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | YU WJ, Wang GH. Advance in finite element analysis on the effects of cervical and lumbar disc degeneration and spinal fusion and fixation on spinal biomechanics. Yixue Linchuang Yanjiu. 2021;38 (7):961-965. |
| 18. | Cui W, Wang L, Ma S, Liu BY. Surgical treatment of degenerative rigid cervical kyphosis by anterior trans-intervertebral osteotomy. Shoudu Yike Daxue Xuebao. 2019;40 (4):497-502. |
| 19. | Jiang HC, Wang JX, Yang XD, Lai Z, Wu JQ, Liu ZX. Long-term outcomes of adjacent segment intervertebral disc degeneration after degenerative lumbar spondylolisthesis fusion. Jing Yaotong Zazhi. 2021;42 (4):512-515. |
| 20. | Song LL, Meng YY, Guo EP. Clinical outcomes of single segment ProDisc-CACDR and ACDF in the treatment of cervical spondylosis. Clinical comparison of single segment ProDisc cacdr and ACDF in the treatment of cervical spondylosis. Jing Yaotong Zazhi. 2019;40 (3):420-421. |
| 21. | Wu DR, Guo T. The current research and advance of bone graft fusion after anterior cervical decompression. Anhui Med Pharm J. 2019;23 (9):1701-1705. |
| 22. | Wang R, Liang BR, Li H. Outcomes of anterior single segment cage and zero-P assisted decompression and fusion in the treatment of cervical degenerative diseases. Chin J Bone Joint Surg. 2019;12 (11):848-853. |
| 23. | Shao W, Zhong HY, Lin T. Compensatory changes of cervical sagittal parameters in patients with degenerative lumbar scoliosis after orthopedic surgery. Jing Yaotong Zazhi. 2020;41 (1):1-4. |
| 24. | Li Q, Yu HQ, Yang Y, Wang X. Clinical outcomes of rhBMP-2 on cervical fusion in patients with cervical degenerative diseases. Chuanbei Yixueyuan Xuebao. 2019;34 (5):532-535. |
| 25. | Qiu F, Zhang X, Li XJ. Application of Carmen synchronous stable cervical fusion system in reoperation of adjacent segment degenerative diseases after cervical fusion. Zhongguo Jizhu Jisui Zazhi. 2019;29 (5):471-474. |
| 26. | Yang Y, Liu H, Meng Y. History and current situation of cervical fusion cage. Shengwu Guke Cailiao Yu Linchuang Yanjiu. 2020;17 (3):62-65. |
| 27. | Huang CZ, Lin Q, Lin JZ. The current research and advance of posterior cervical single door laminoplasty in the treatment of cervical spinal stenosis. Shengwu Guke Cailiao Yu Linchuang Yanjiu. 2019;16 (2):67-71. |
| 28. | Guan HS, Shi J, Li CG. Incidence and related factors of early dysphagia after anterior cervical decompression and fusion. Zhongguo Yaowu Yu Linchuang. 2019;19 (13):2262-2265. |
| 29. | Shen SF, Hu Y, Wu JD, Chu ZT. Population characteristics of young patients with cervical spondylosis and their correlation with cervical disc degeneration. Zhongguo Jisui Jizhu Zazhi. 2021;31 (7):613-618. |
| 30. | Li XF. Prevention and treatment of adjacent segment degeneration after anterior cervical fusion. Jizhu Waike Zazhi. 2021;19 (3):198-202. |