Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4684
Peer-review started: December 8, 2021
First decision: January 26, 2022
Revised: January 30, 2022
Accepted: March 16, 2022
Article in press: March 16, 2022
Published online: May 16, 2022
Processing time: 156 Days and 0.1 Hours
Maisonneuve fracture is a special type of ankle fracture that consists of proximal fibular fracture, a lesion of the inferior tibiofibular syndesmotic complex (interosseous ligament, anterior inferior tibiofibular ligament and posterior inferior tibiofibular ligament), and injury of the medial structure of the ankle (deltoid ligament tear or medial malleolar fracture). The accepted mechanism of Maisonneuve fracture is pronation external rotation according to the Lauge-Hansen classification. In this paper, we report a rare pattern of Maisonneuve fracture, which has the characteristics of both pronation external rotation ankle fracture and supination adduction ankle fracture.
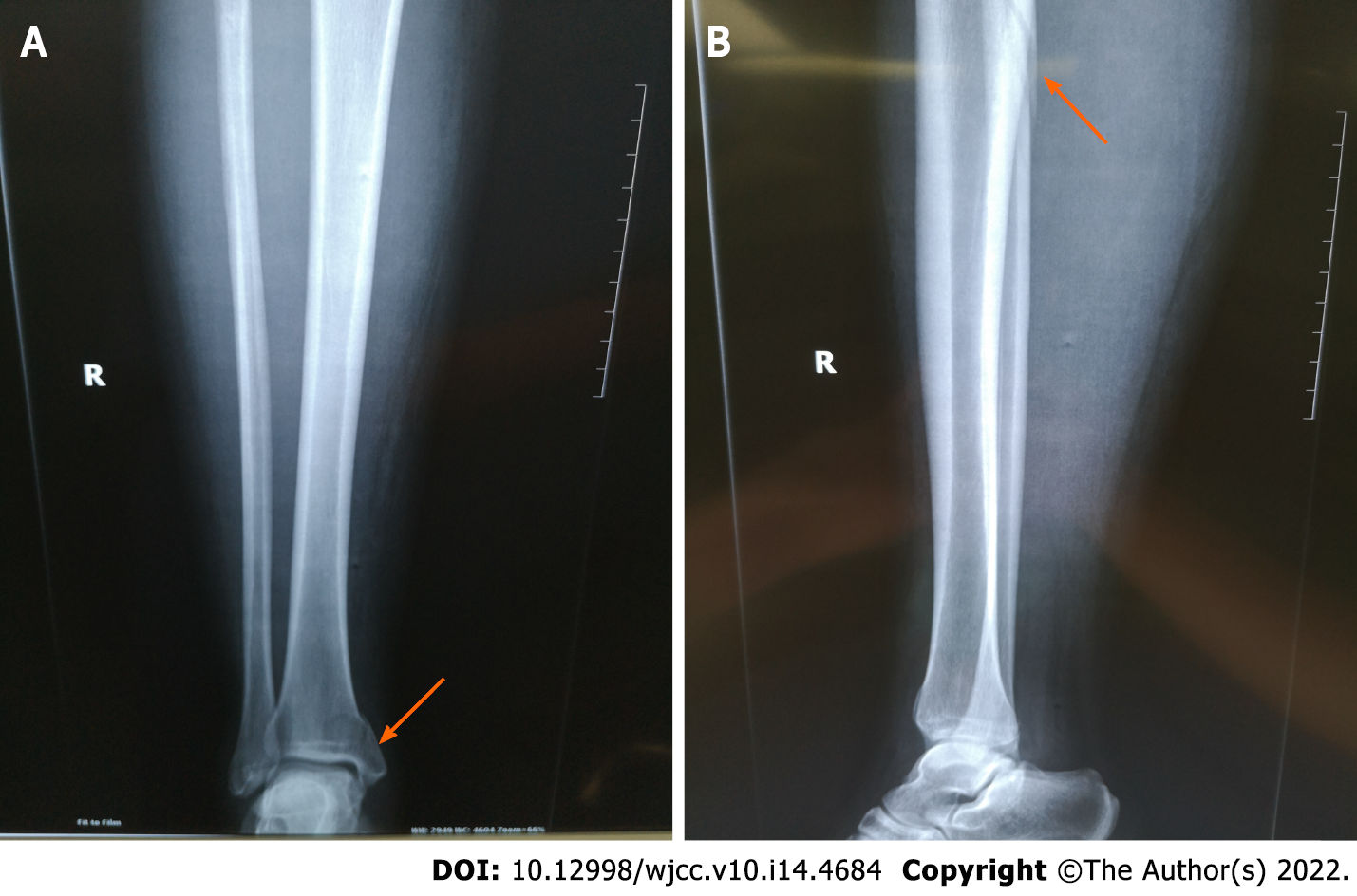
A 31-year-old female patient accidentally sprained her right ankle while walking 5 d before hospitalization in our hospital. The patient was initially missed in other hospitals and later rediagnosed in our outpatient department. Full-length radi
To our knowledge, this rare pattern of Maisonneuve fracture has not been previously described. The possible mechanism of injury is supination adduction combined with pronation external rotation. Careful analysis of the injury mechanism of Maisonneuve fracture is of great clinical significance and can better guide clinical treatment.
Core Tip: We report a rare pattern of Maisonneuve fracture, which has the characteristics of both pronation external rotation and supination adduction. The patient was initially missed in other hospital and later rediagnosed in our hospital. The patient underwent open reduction and internal fixation. A 6-mo postoperative follow-up confirmed a good clinical outcome. To our knowledge, this rare pattern of Maisonneuve fracture has not been previously described. The possible mechanism of injury is supination adduction combined with pronation external rotation. Careful analysis of the injury mechanism of Maisonneuve fracture is of great clinical significance and can better guide clinical treatment.
- Citation: Zhao B, Li N, Cao HB, Wang GX, He JQ. Rare pattern of Maisonneuve fracture: A case report. World J Clin Cases 2022; 10(14): 4684-4690
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4684.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4684
Maisonneuve fracture is a special type of ankle fracture that consists of proximal fibular fracture, a lesion of the inferior tibiofibular syndesmotic complex (interosseous ligament, anterior inferior tibiofibular ligament and posterior inferior tibiofibular ligament), and injury of the medial structure of the ankle (deltoid ligament tear or medial malleolar fracture)[1,2]. Understanding the injury mechanism of ankle fractures can better guide their treatment[3]. The accepted mechanism of Maisonneuve fracture is pronation external rotation according to the Lauge-Hansen classification[4].
In this paper, we report a rare pattern of Maisonneuve fracture, which has the characteristics of both pronation external rotation ankle fracture and supination adduction ankle fracture. To our knowledge, this is the first time that this rare pattern of Maisonneuve fracture has been reported, and there are no similar cases in the English literature.
A 31-year-old female patient accidentally sprained her right ankle while walking 5 d before hospitalization in our hospital.
She felt pain and gradual swelling in her right ankle and could not stand or walk normally. No significant relief was found after rest. The patient was admitted to the emergency department of another hospital for X-ray examination, which indicated a fracture of the right medial malleolus. The patient received manual reduction and external fixation with braces. Two days before hospitalization, the patient was reviewed in the outpatient department of our hospital. The patient complained of extensive pain around the ankle joint. The patient was admitted to our hospital for further examination and treatment.
She had no other history of past illnesses.
She had no genetic or familial disease history.
Physical examination revealed a closed ankle injury with extreme tenderness, swelling and subcutaneous ecchymoses around the ankle joint. There was also tenderness and subcutaneous ecchymoses at the proximal fibula. Neurological examination showed no obvious abnormalities. The dorsalis pedis pulse and posterior tibial artery pulse were palpable.
Laboratory examinations revealed no obvious abnormality.
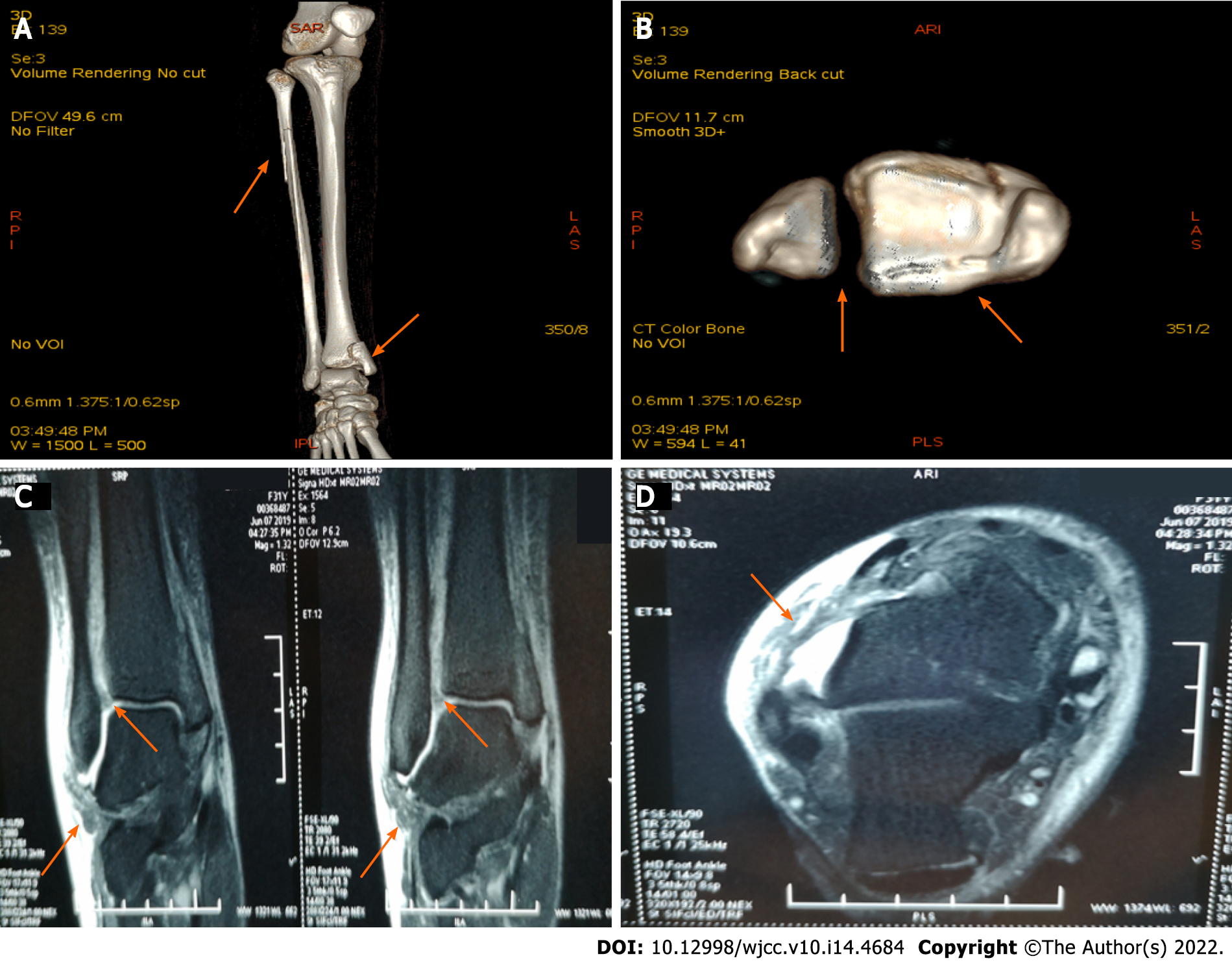
Full-length radiographs of the lower leg revealed proximal fibula fracture, inferior tibiofibular joint separation, and medial malleolar fracture involving the posterior malleolus (Figure 1), which was also revealed on computed tomography (CT) scans (Figure 2A and B). The proximal fibula fracture was located approximately 7 cm from the distal end of the fibula head, and the fracture line was long and oblique, which is similar to a Maisonneuve fracture and belongs to pronation external rotation fracture according to the Lauge-Hansen classification. The medial malleolar fracture was a vertical fracture, which is similar to supination adduction fracture according to the Lauge-Hansen classification. Magnetic resonance imaging revealed rupture of the anterior inferior tibiofibular ligament and anterior talofibular ligament, surrounded by areas of high signal representing edema and hemorrhage (Figure 2C and D).
We diagnosed a rare pattern of Maisonneuve fracture with proximal fibular fracture, inferior tibiofibular joint separation, medial malleolar fracture and ruptures of the anterior inferior tibiofibular ligament and anterior talofibular ligament.
On the second day after admission, we performed open reduction and internal fixation of the right ankle fracture in the operating room. Meanwhile, ligament exploration and repair were performed. Epidural anesthesia was used. After successful anesthesia, the patient was placed in the supine position. Routine disinfection, dressing, and tourniquet were performed.
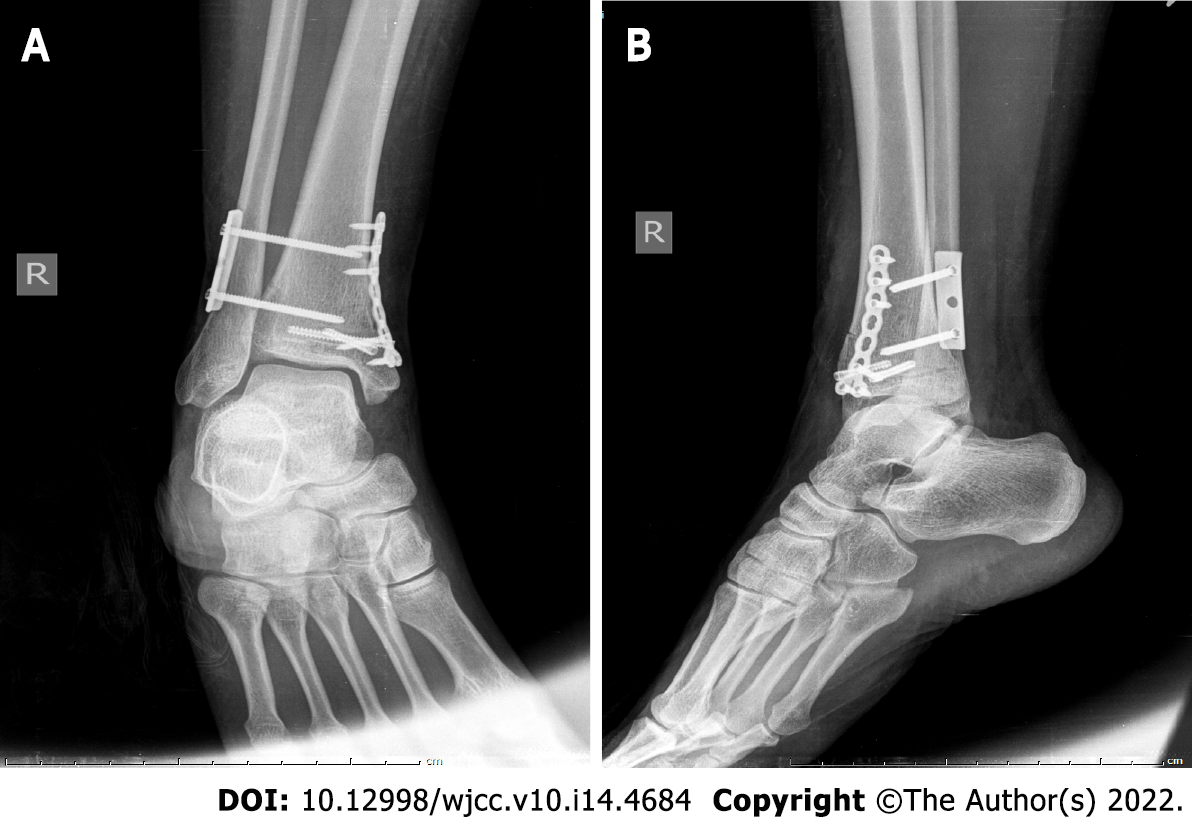
First, the inferior tibiofibular syndesmosis was explored by a lateral approach. The inferior tibiofibular syndesmosis was separated, and the anterior inferior tibiofibular ligament was ruptured. The length of the fibula was restored, and the inferior tibiofibular syndesmosis was reduced. Kirschner wire was used for temporary fixation. After satisfactory anatomical reduction by fluoroscopy, the syndesmosis was fixed with locking plate screws. The screw placement direction was oriented 30° from posterior to anterior with slight dorsiflexion of the ankle. Next, the medial malleolar fracture was reduced by an arc-shaped incision along the posterolateral side of the medial malleolus and fixed by two 3.5-mm partially threaded cannulated screws (Figure 3). The fracture was still fretting and was supplementally fixed with microplate screws. Finally, the anterior talofibular ligament was repaired with absorbable sutures at the lateral incision. Intraoperative stress radiographs showed that the fracture was in good alignment and that the tibiofibular syndesmosis was stable.
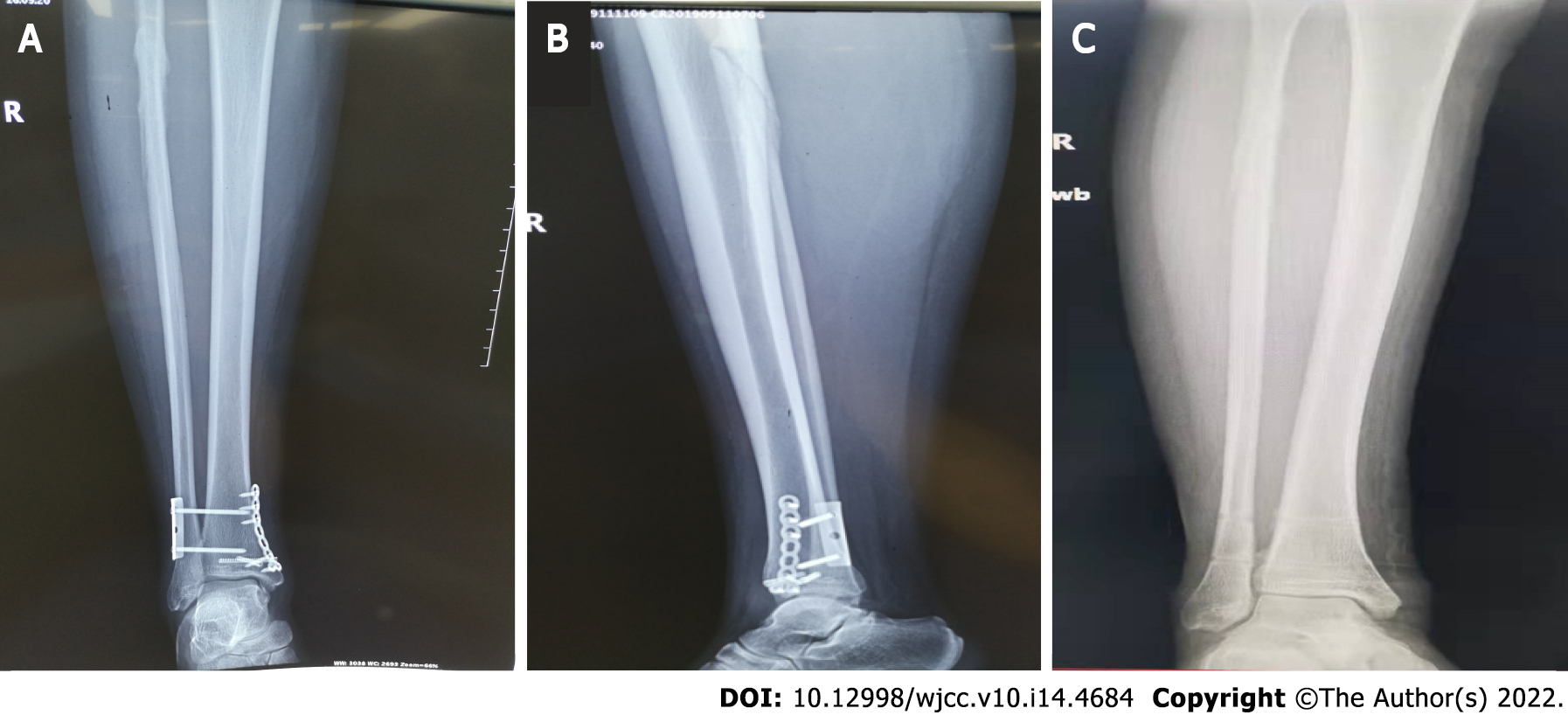
Postoperatively, the ankle was immobilized in a short-leg cast for two weeks, and then active and passive non-weight bearing exercise of the ankle was started. Three months after the operation, reexamination of the radiographs showed that the fracture line of the medial malleolus disappeared, the fibula fracture line was blurred, and extensive callus formed around the broken end of the fibula fracture (Figure 4A and B). Then, the plate and all screws were removed (Figure 4C). Subsequently, the patient gradually performed weight-bearing, functional exercises. At 6 mo postoperative, the patient's ankle range of motion was fully restored to her preinjury level. The patient’s American Orthopedic Foot and Ankle Society hindfoot-ankle scale[5] score was 100 points.
Maisonneuve fracture was first named in 1840 by the French surgeon Maisonneuve[6]. According to the literature, Maisonneuve fractures account for approximately 7% of ankle fractures[7]. Maisonneuve fracture is often missed because most patients complain of ankle pain rather than proximal fibula pain[8]. In this case, the patient was initially admitted to an outside hospital. Since the patient only complained of pain in the ankle, only an ankle radiograph was performed. The results suggested medial malleolar fracture with slight separation of the inferior tibiofibular syndesmosis. The patient was treated conservatively. Three days after the injury, the patient was re-examined in our outpatient department due to ankle pain. Maisonneuve fracture was confirmed by careful physical examination and full-length radiographs of the lower leg. These results suggest that Maisonneuve fracture should be highly suspected in patients with simple medial malleolar fracture. Careful examination of the entire lower leg should be performed in all patients with ankle fractures. For patients with suspected Maisonneuve fracture, full-length leg radiographs or even stress-position radiographs should be taken.
Understanding the mechanism of injury is very important for the treatment of ankle fracture[9]. For either closed reduction or open reduction, the physician can reduce the fracture according to the opposite direction of the injury mechanism[10,11]. The Lauge-Hansen classification provides a sequential mechanism of injury that considers soft tissue as well as osseous structures in the development of ankle fractures[12]. According to the Lauge-Hansen classification, ankle fractures can be divided into four types: Supination external rotation, supination adduction, pronation external rotation and pronation abduction[13,14].
Most scholars classify Maisonneuve fractures as pronation external rotation ankle fractures according to the Lauge-Hansen classification[15,16]. Once injured, the medial structure is damaged first, including rupture of the deltoid ligament or fracture of the medial malleolus, followed by rupture of the anterior inferior tibiofibular ligament or avulsion fracture of the attachment, rupture of the interosseous ligament, rupture of the interosseous membrane, and proximal fibula fracture. If violence persists, rupture of the posterior inferior tibiofibular ligament or avulsion fracture of the posterior tibial tubercle may occur[17-19].
The case presented here is a rare pattern of Maisonneuve fracture, which has the characteristics of both pronation external rotation ankle fracture and supination adduction ankle fracture. In this case, the fibula fracture was long and oblique, and the fracture line was proximal to the fibula. There was also inferior tibiofibular separation. These characteristics are similar to a typical Maisonneuve fracture, which is a pronation external rotation ankle fracture. However, the medial malleolus of the typical pronation external rotation ankle fracture usually presents an oblique fracture or rupture of the deltoid ligament, without rupture of the anterior talofibular ligament or calcaneofibular ligament[20]. In this case, the medial malleolar fracture was vertical, and there was rupture of the anterior talofibular ligament, which is consistent with supination adduction ankle fracture.
The separate fracture configurations raise questions regarding the injury mechanism of the presented case. Inferior tibiofibular separation and proximal fibula fracture are clearly prone to external rotation patterns. However, the fracture morphology of the medial malleolus and rupture of the anterior talofibular ligament display the characteristics of a supination adduction pattern. We hypothesized that the mechanism of this injury may be that the foot starts in supination and suddenly experiences an adduction type injury, resulting in rupture of the anterior talofibular ligament and vertical fracture of the medial malleolus. The original position of the foot was changed to pronation when the patient tried to stand, which was followed by an external rotation injury resulting in inferior tibiofibular separation and proximal fibula fracture.
In summary, Maisonneuve fracture is an uncommon fracture that is often overlooked in patients with ankle injuries. An accurate and thorough physical examination, appropriate radiological examinations and intraoperative stress fluoroscopy are necessary. Careful analysis of the injury mechanism of Maisonneuve fracture is of great clinical significance and can better guide clinical treatment.
We would like to thank the nursing term of the Department of Foot and Ankle Surgery Ⅰ, Tianjin Hospital, for the support, and our patient for participating in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Liu J, United States; Liu J, United States; Moshref L, Saudi Arabia S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Kalyani BS, Roberts CS, Giannoudis PV. The Maisonneuve injury: a comprehensive review. Orthopedics. 2010;33:196-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Pankovich AM. Maisonneuve fracture of the fibula. J Bone Joint Surg Am. 1976;58:337-342. [PubMed] |
| 3. | Sproule JA, Khalid M, O'Sullivan M, McCabe JP. Outcome after surgery for Maisonneuve fracture of the fibula. Injury. 2004;35:791-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | He JQ, Ma XL, Xin JY, Cao HB, Li N, Sun ZH, Wang GX, Fu X, Zhao B, Hu FK. Pathoanatomy and Injury Mechanism of Typical Maisonneuve Fracture. Orthop Surg. 2020;12:1644-1651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3199] [Cited by in RCA: 3117] [Article Influence: 100.5] [Reference Citation Analysis (0)] |
| 6. | Maisonneuve JG. Recherches sur la fracture du perone. Arch Gen Med. 1840;7:165-187, 433. |
| 7. | Liu GP, Li JG, Gong X, Li JM. Maisonneuve injury with no fibula fracture: A case report. World J Clin Cases. 2021;9:3733-3740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Taweel NR, Raikin SM, Karanjia HN, Ahmad J. The proximal fibula should be examined in all patients with ankle injury: a case series of missed maisonneuve fractures. J Emerg Med. 2013;44:e251-e255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Hinds RM, Tran WH, Lorich DG. Maisonneuve-hyperplantarflexion variant ankle fracture. Orthopedics. 2014;37:e1040-e1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Bartoníček J, Rammelt S, Kašper Š, Malík J, Tuček M. Pathoanatomy of Maisonneuve fracture based on radiologic and CT examination. Arch Orthop Trauma Surg. 2019;139:497-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Charopoulos I, Kokoroghiannis C, Karagiannis S, Lyritis GP, Papaioannou N. Maisonneuve fracture without deltoid ligament disruption: a rare pattern of injury. J Foot Ankle Surg. 2010;49:86.e11-86.e17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Duchesneau S, Fallat LM. The Maisonneuve fracture. J Foot Ankle Surg. 1995;34:422-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Shariff SS, Nathwani DK. Lauge-Hansen classification--a literature review. Injury. 2006;37:888-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Ramos LS, Gonçalves HM, Freitas A, Oliveira MP, Lima DMS, Carmargo WS. Evaluation of the Reproducibility of Lauge-Hansen, Danis-Weber, and AO Classifications for Ankle Fractures. Rev Bras Ortop (Sao Paulo). 2021;56:372-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Stufkens SA, van den Bekerom MP, Doornberg JN, van Dijk CN, Kloen P. Evidence-based treatment of maisonneuve fractures. J Foot Ankle Surg. 2011;50:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 16. | Hensel KS, Harpstrite JK. Maisonneuve fracture associated with a bimalleolar ankle fracture-dislocation: a case report. J Orthop Trauma. 2002;16:525-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Richmond RR, Henebry AD. A Maisonneuve Fracture in an Active Duty Sailor: A Case Report. Mil Med. 2018;183:e278-e280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Smeeing DPJ, Houwert RM, Kruyt MC, Hietbrink F. The isolated posterior malleolar fracture and syndesmotic instability: A case report and review of the literature. Int J Surg Case Rep. 2017;41:360-365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Mansur H, Lima T, Goncalves C, Castro I. Adult Tillaux Fracture in Association with Volkmann and Maisonneuve Fratures: A Case Report. J Am Podiatr Med Assoc. 2019;109:477-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Ebraheim NA, Weston JT, Ludwig T, Moral MZ, Carroll T, Liu J. The association between medial malleolar fracture geometry, injury mechanism, and syndesmotic disruption. Foot Ankle Surg. 2014;20:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (1)] |