Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4569
Peer-review started: September 23, 2021
First decision: November 11, 2021
Revised: November 23, 2021
Accepted: March 25, 2022
Article in press: March 25, 2022
Published online: May 16, 2022
Processing time: 231 Days and 19.9 Hours
Convulsive-like movements are rare in basilar artery occlusive cerebral infarction (BAOCI). These manifestations may easily be mistaken for epileptic seizures caused by compromised anterior circulation or by cortical lesions. Delayed diagnosis of this condition affects its subsequent treatment and prognosis. Therefore, it is critical to recognize this type of phenomenon in the early stage.
A 55-year-old male patient presented with unconsciousness, rigidity, and a paroxysmal twitch in both lower limbs. These conditions lasted for nearly 2 h and resembled status epilepticus. After the initial conditions subsided, hemiplegia occurred and then subsided rapidly. The family refused thrombolytic therapy because the symptoms were similar to Todd paralysis after epilepsy. However, magnetic resonance imaging showed left pontine infarction. No abnormality was observed in a video electroencephalogram during the interictal period. Digital subtraction angiography revealed that the basilar artery was occluded and that the posterior communicating arteries were patent. Fortunately, the patient received a good prognosis after antiplatelet therapy, lipid regulation, balloon dilatation of the basilar artery, and rehabilitation.
Convulsive-like movements may be an early sign of basilar artery occlusive brainstem infarction. It is important to identify this phenomenon in a timely manner.
Core Tip: It is rare for convulsive-like movements to occur as the first symptom of basilar artery occlusive cerebral infarction (BAOCI). When they do occur, however, these movements can serve as an early warning sign of BAOCI. The early diagnosis of basilar artery occlusion can influence patients’ treatment and prognosis.
- Citation: Wang TL, Wu G, Liu SZ. Convulsive-like movements as the first symptom of basilar artery occlusive brainstem infarction: A case report. World J Clin Cases 2022; 10(14): 4569-4573
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4569.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4569
Basilar artery occlusive cerebral infarction (BAOCI) is a rare ischaemic cerebrovascular disease that accounts for approximately 1%–4% of all ischaemic stroke[1]. BAOCI carries high morbidity and mortality. For clinical reference, we report a rare case of basilar artery occlusive pontine infarction with convulsive-like movements at the onset.
A 55-year-old male patient was sent to our hospital because of unconsciousness and limb convulsion for 1 h.
The patient's wife found him vocalizing in his sleep. He was unconscious and presented with a foaming mouth, limb rigidity and urinary incontinence. Paroxysmal convulsions of both lower limbs were observed. Thirty minutes after admission, the patient regained consciousness but remained unable to speak. His right limb was hemiplegic, and he had paroxysmal involuntary twitches of both lower limbs, with no limb ankylosis. An hour after admission, the patient was able to answer some questions and raise his right limbs. The lower limbs were no longer twitching.
The patient had a history of right pontine infarction 3 years prior. The clinical manifestation at that time was mild weakness of the left limbs, and there were no sequelae after treatment.
The patient had no personal or family history of epilepsy. Additionally, he had no risk factors for cerebral infarction, such as hypertension, diabetes, smoking, drinking, atrial fibrillation or valvular heart disease.
The patient did not cooperate with the eye movement examination, and no gaze was observed. Physical examination showed vague speech, bilateral symmetry of the nasolabial grooves, grade IV muscle strength in the right limbs, normal limb muscle tension, and positive bilateral pathological signs.
Routine blood tests, liver function, kidney function, electrolytes, glucose levels and coagulation function were normal.
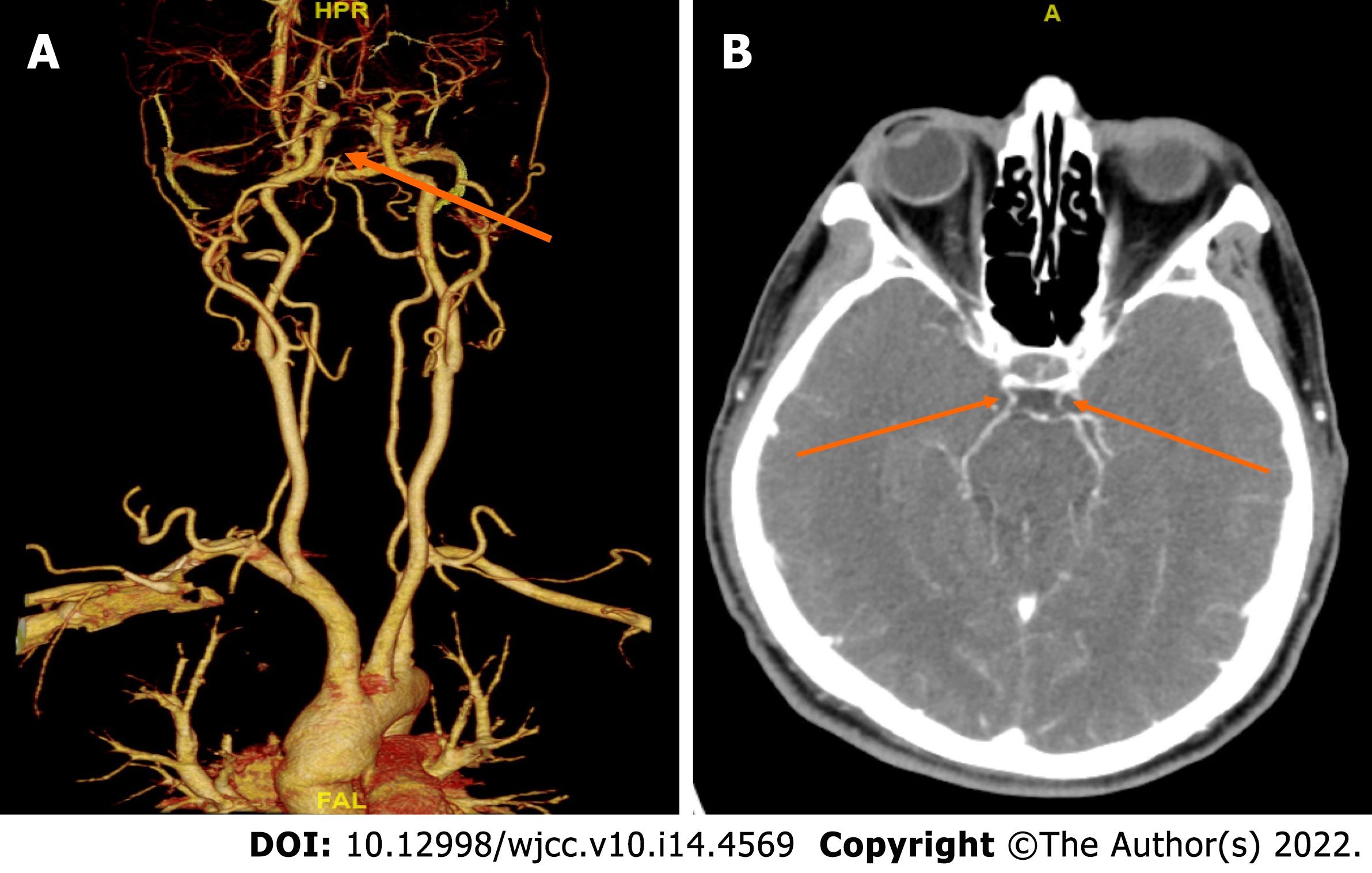
Head computed tomography showed no abnormality. No hypoperfused area was found via computed tomography perfusion imaging of the anterior circulation. Computed tomography angiography showed that the basilar artery was occluded and that the posterior communicating artery was patent (Figures 1 and 2). There was no abnormality on video electroencephalogram (EEG) examination during the interictal period. Additionally, 24-h Holter monitoring showed no abnormality.
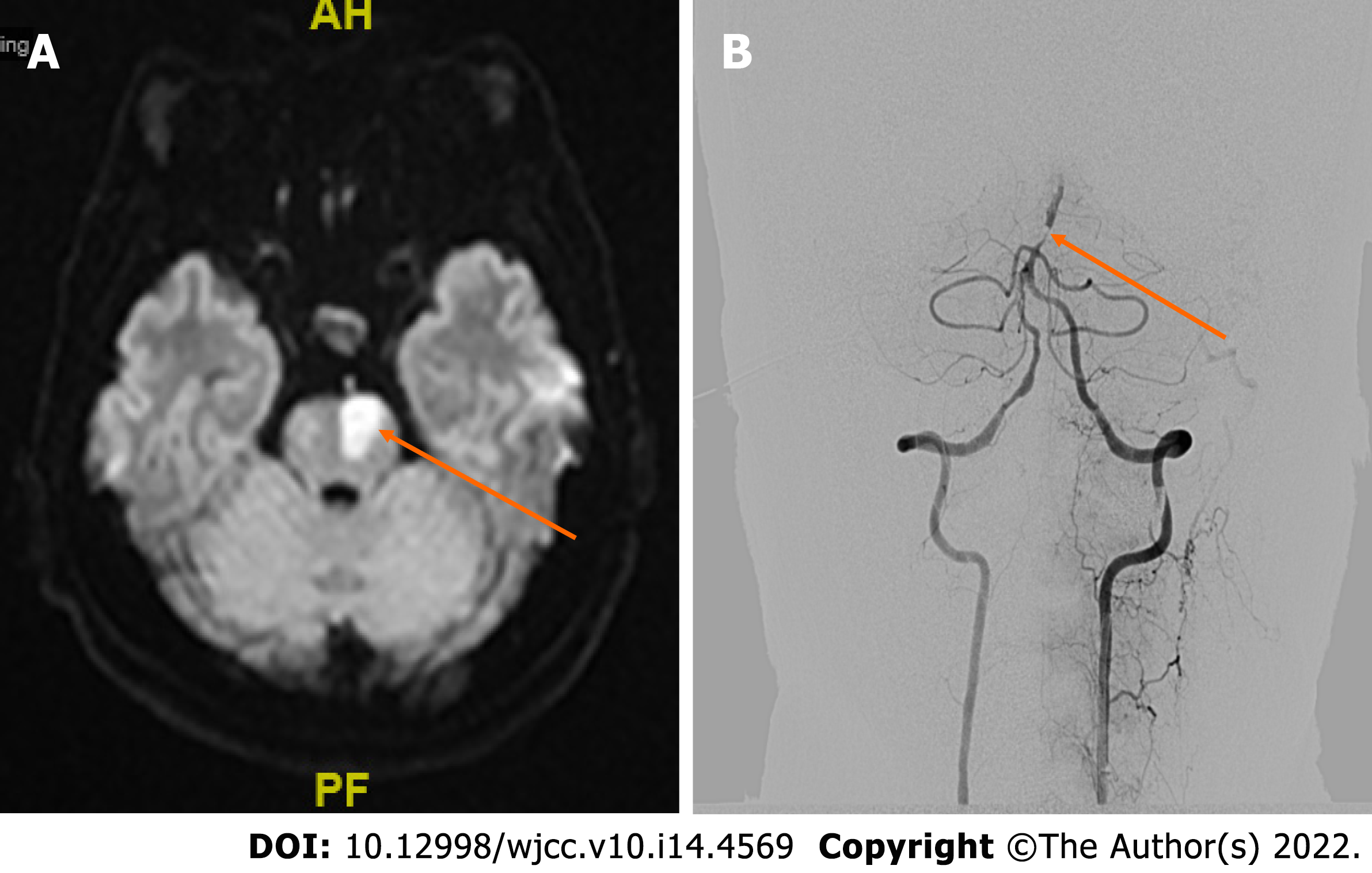
Magnetic resonance imaging revealed left pontine infarction (Figure 2A). Digital subtraction angiography showed that the lower segment of the basilar artery was severely stenosed, the upper segment was occluded, and the bilateral posterior communicating arteries were patent (Figure 2B).
The final diagnosis of the presented case was left pontine infarction and basilar artery occlusion.
The patient's right limb weakness worsened on the 3rd day after admission. Physical examination showed that the proximal muscle strength of the right upper limb was grade III, the distal muscle strength was grade 0, and the muscle strength of the right lower limb was grade III. The patient received antiplatelet therapy, lipid regulation, basilar artery balloon dilatation and rehabilitation.
The patient’s muscle strength recovered to grade V. The prognosis was good.
BAOCI is a rare ischaemic stroke that is life threatening in severe cases. Early diagnosis and treatment can lead to an improved prognosis and an increased survival rate. Therefore, the early diagnosis of basilar artery occlusion (BAO) is very important. However, convulsive movement or epilepsy rarely occurs as the first symptom of BAOCI. A large meta-analysis revealed that the incidence of epilepsy in the early stage of ischaemic stroke was only 3.3%[2]. Studies have shown that cerebral infarction with epilepsy onset mostly occurs in the anterior circulation and cerebral cortex, accounting for approximately three-quarters (75%) of cases. The incidence of posterior circulation infarction is approximately one-quarter (25%)[3].
Convulsive-like movements may be the first symptom of BAO. As early as 1868, there was a description of convulsive movement in brainstem diseases[4]. This phenomenon was often described as epileptic seizure by eyewitnesses, and it was believed to be related to the decerebrate rigidity caused by ischaemia and hypoxia after stroke. Ropper et al[5] described 8 patients with convulsive-like movements after BAO. They presented with limb rigidity and small-amplitude convulsions. Some patients had limb flexion and large-amplitude convulsions. However, EEG examination during tic-like seizures was not performed. Therefore, it is difficult to judge whether the symptom is an epileptic seizure. Edward et al[6] reported a case of middle cerebral infarction with BAO. There was no EEG evidence of epileptiform discharge during the patient’s whole-limb twitch and lower-limb twitch. The authors suggested that convulsive-like movements might not be epileptic seizures. However, recently, Bhatt et al[7] reported a BAO patient with disturbance of consciousness and left limb tonic movement. They found epileptic activity on EEG and recorded the spastic seizure movements of the limb. Therefore, they considered convulsive-like movements to be status epilepticus caused by basilar artery thrombosis.
The mechanism of convulsive-like movements caused by BAO is unclear. Penfield proposed the hypothesis of a centrencephalic system, suggesting that the brainstem was the causative centre of epileptic seizures[8]. It may directly participate in the control of the epileptic threshold through a wide range of forebrain projections. Animal experiments have shown that stimulation of the midbrain, pons or medulla may lead to tonic seizures[4]. Saposnik et al[4] described a pontine infarction patient with BAO. The patient presented with unconsciousness and convulsions of both upper limbs. However, an EEG showed no cortical discharge. This study suggested that the convulsions may be related to ischaemia of the corticospinal tracts rather than brainstem-originated seizures. Alvarez et al[9] reported a case of bilateral pontine infarction with ankylosing movement. They held the same opinions as Saposnik et al. In our case, we could not distinguish whether the convulsive-like movements were secondary to ischemic stroke or caused by epileptic seizures. The patient had no epileptic pathogeny or risk factors for epileptic seizures, such as trauma, tumour, poisoning, infection, metabolic abnormality, or family history of epilepsy. Furthermore, the patient did not undergo EEG examination upon presenting with convulsive-like movements, and no abnormality was observed on EEG during the follow-up treatment. Therefore, we cannot judge whether the phenomenon is epilepsy. However, the patient had basilar artery occlusion, a risk factor for ischemic stroke. We are inclined to believe that the convulsive-like movements were secondary to ischemic stroke.
In our case, the patient presented with epileptic-like symptoms and rapid recovery of limb weakness. The presentation was similar to Todd’s paralysis after seizures. Additionally, the patient seemed to have no other risk factors for cerebral infarction, such as hypertension, diabetes, smoking, or alcohol consumption. Thus, his family members refused thrombolytic therapy. Anterior circulation computed tomography perfusion examination was selected because epilepsy after cerebral infarction is most common in the cortex and anterior circulation. As a result, we failed to identify the cerebral perfusion of the posterior circulation in time. The patient did not receive thrombolysis and thrombectomy. Therefore, when observing convulsive-like movements, clinicians should take the possibility of BAOCI into account.
Studies have shown that the prognosis of BAOCI is related to the location, aetiology, vascular anatomy and collateral circulation[10]. The good prognosis of this patient may be due to the patent status of the posterior communicating artery. Because of severe stenosis of the lower basilar artery, the thrombus moved forward to the upper segment, blocking the opening of the paracentral branch. As a result, an infarction occurred on one side of the pons. Due to the patent status of the posterior communicating artery, the blood supply of the midbrain, cerebellum and other posterior circulation areas was guaranteed. The patient’s prognosis was good.
When it is difficult to distinguish Todd’s paralysis from ischaemic stroke in the early stage, both anterior- and posterior-circulation computed tomography perfusion and vascular examination should be performed as early as possible. More active treatment strategies should be adopted, including thrombolysis and mechanical thrombectomy when necessary.
BAOCI is a rare type of ischaemic stroke with high morbidity and mortality. Brainstem infarction with convulsive-like movements as the first symptom is uncommon. When the phenomenon of convulsive-like movements is observed, we should consider the possibility of BAOCI. Early recognition of this phenomenon may reduce the misdiagnosis of BAO and improve the prognosis through early thrombolysis and interventional therapy. If possible, we suggest that an EEG should be performed in time to detect the essential features of the phenomenon.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Neurosciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chen Y, China; Ciarambino T, Italy; Ennab RM, Jordan S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Algahtani H, Shirah B, Abdelghaffar N, Alqahtani AJ, Alshehri M. Unusual presentation of basilar artery thrombosis. J Cerebrovasc Endovasc Neurosurg. 2020;22:282-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Wang JZ, Vyas MV, Saposnik G, Burneo JG. Incidence and management of seizures after ischemic stroke: Systematic review and meta-analysis. Neurology. 2017;89:1220-1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 3. | Cheng JH, Zhang Z, Ye Q, Ye ZS, Xia NG. Characteristics of the ischemic stroke patients whose seizures occur at stroke presentation at a single institution in Eastern China. J Neurol Sci. 2018;387:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Saposnik G, Caplan LR. Convulsive-like movements in brainstem stroke. Arch Neurol. 2001;58:654-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Ropper AH. 'Convulsions' in basilar artery occlusion. Neurology. 1988;38:1500-1501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 6. | Mader EC Jr, Losada V, Baity JC, McKinnies EM, Branch LA. Stroke-Onset Seizures During Midbrain Infarction in a Patient With Top of the Basilar Syndrome. J Investig Med High Impact Case Rep. 2020;8:2324709620940497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Bhatt SK, Dawit S, Okazaki EM, Noe KH. Refractory Left Focal Motor Status Epilepticus as Initial Clinical Presentation of Acute Basilar Artery Thrombosis. Mayo Clin Proc Innov Qual Outcomes. 2021;5:511-515. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Matsuo K, Fujii C, Fuse I, Nakajima M, Takada M, Miyata K. Top of the basilar syndrome in a young adult initially presenting with a convulsive seizure. Intern Med. 2011;50:1425-1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Alvarez V, Morier J, Hirt L. An episode mimicking a versive seizure in acute bilateral pontine stroke. J Clin Neurosci. 2011;18:1141-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Kwak HS, Park JS. Mechanical Thrombectomy in Basilar Artery Occlusion: Clinical Outcomes Related to Posterior Circulation Collateral Score. Stroke. 2020;51:2045-2050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |