Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4563
Peer-review started: September 9, 2021
First decision: October 22, 2021
Revised: November 1, 2021
Accepted: March 25, 2022
Article in press: March 25, 2022
Published online: May 16, 2022
Processing time: 246 Days and 1.6 Hours
In recent years, people have paid more attention to oral health with the development of stomatology. Due to the various physiological changes during pregnancy, such as changing hormone levels and immune functions, oral diseases have a high incidence during pregnancy, and the prevention and treatment of oral diseases have also received the attention of both dentists and obstetricians. However, the anesthetic management of pregnant patients with oral disease, especially severe maxillofacial infections, and patients who need surgical treatment or have obstetric emergencies and need to terminate their pregnancy is not clear.
This article describes a parturient patient with a severe masseteric space infection who had an emergency cesarean section.
This case report aims to discuss the important anesthetic considerations for these patients.
Core Tip: The anesthetic management of pregnant patients with oral disease, especially severe maxillofacial infections, and patients who need surgical treatment or have obstetric emergencies and need to terminate their pregnancy is not clear. This article describes a parturient patient with a severe masseteric space infection who had an emergency cesarean section, and this case report aims to discuss the important anesthetic considerations for these patients.
- Citation: Ren YL, Ma YS. Anesthesia management for cesarean section in a pregnant woman with odontogenic infection: A case report. World J Clin Cases 2022; 10(14): 4563-4568
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4563.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4563
There are many changes occurring in the hormone levels and diet customs during pregnancy that make the formation of dental plaque more likely, and dental plaque contains a large number of bacteria that irritate the gum and cause local inflammation, swelling, bleeding, and pain[1]. The oral and maxillofacial region is connected to several spaces, such as the submandibular space, para-pharyngeal space, retropharyngeal space, submental space, pre-tracheal space, and epidural space. The infection can spread along these spaces and can cause serious complications, including upper airway obstruction, descending mediastinitis, septic shock, disseminated intravascular coagulopathy, and pericarditis[2]. Due to the influence of the fetus, there is a reduced function of the maternal immune system, and the response to infection is reduced. Therefore, the infection is more likely to spread and be aggressive. However, in the early stages of infection, patients’ symptoms are easily overlooked, or patients are worried about the effects of drugs on the fetus. Both of these often lead to delays in diagnosis and treatment. In this case, the mother had a serious maxillofacial space infection due to delay in treatment, which brought great challenges to both anesthesia and delivery.
A 25-year-old G1P0 woman at 38+6 wk of pregnancy, who had a left wisdom tooth pericoronitis that was present for more than 4 mo and was exacerbated for 1 mo, was admitted to the hospital.
Four months prior to presentation, the patient went to a dental hospital for a gradual progressive swelling of the left maxillofacial region and was diagnosed with a left wisdom tooth pericoronitis, which was suspected to be concurrent with a masseter space infection. Then, she received cefuroxime sodium for 1 wk, but there was no significant improvement. She did not receive any further treatment afterward. One month prior to presentation, she again went to the hospital for a worsened swelling with throbbing pain which was radiating to her ear. Additionally, her mouth opening was obviously restricted. She was diagnosed with left mandible chronic osteomyelitis associated with infection, and advised to undergo incision and drainage after delivery.
The patient was healthy previously.
The patient denied any family history.
On admission, the patient’s body temperature was 37.8 °C, her heart rate was 73-91 beats/min, and her respiratory rate was 18-20 breaths/min. Fetal monitoring showed that contractions occurred every 5-6 min for 20-30 s, and the fetus was assessed as normal.
Routine blood tests showed a white blood cell (WBC) count of 14.0 x 109/L and a C-reactive protein level of 36.1 mg/L.
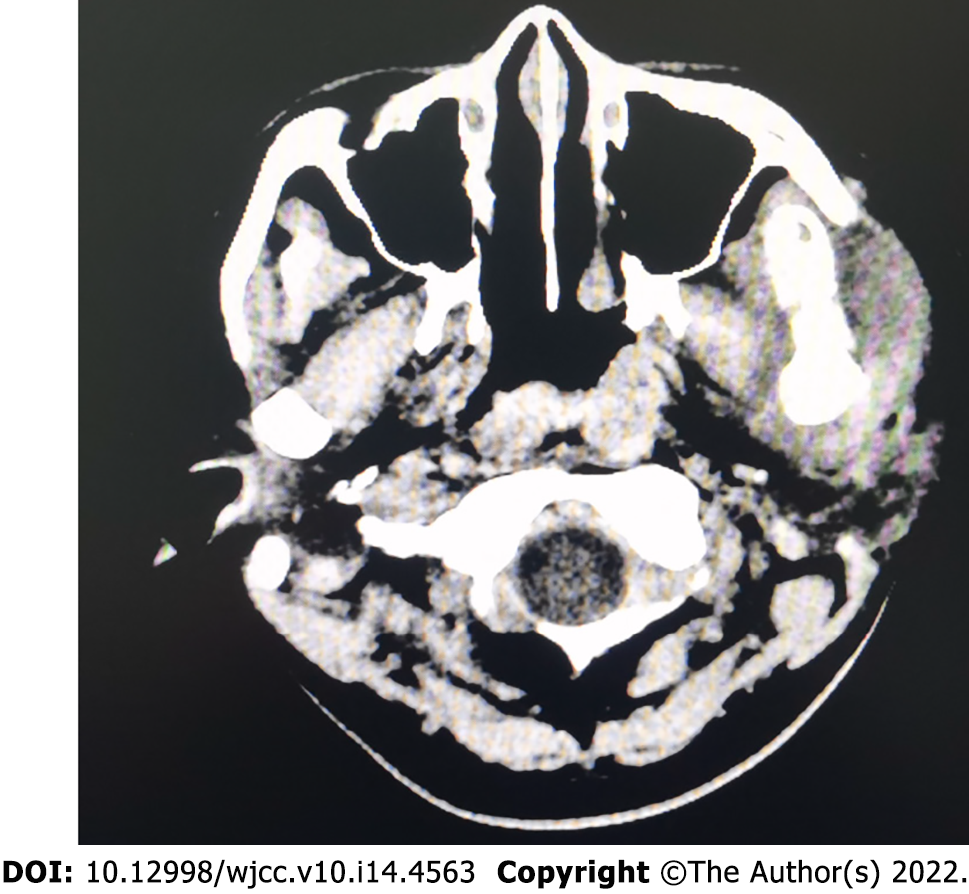
A plain computed tomography (CT) scan image of the neck is shown in Figure 1.
After consultation with the stomatology department, a local aspiration was performed, a small amount of dead bone-like material was removed, but no obvious pus was removed. The anesthesia consultation showed that the patient’s left maxillofacial and submandibular area was swollen and had obvious tenderness, her skin temperature was warm, her mouth opening was only one finger wide, and her neck movement was acceptable. There were no symptoms or signs of airway obstruction.
The patient received a diagnosis of left mandibular chronic osteomyelitis with an infection present.
Piperacillin sodium and tazobactum sodium were given to actively resist infection. The patient and her family expressed that considering increased infection and sepsis during delivery process may endanger mother and fetus’ life, they refused to try vaginal delivery and prepared for emergency cesarean section at any time.
A day later, the patient was scheduled to undergo an emergency cesarean section to terminate the pregnancy. After anti-infective treatment, the patient’s temperature was 37 °C and she had no contraindications for intraspinal anesthesia. The planned anesthesia method was combined spinal-epidural block. However, considering the possibility of the failure of the intraspinal anesthesia, the possibility of needing general tracheal intubation due to other emergencies during the operation, and the high risk of having a difficult airway, we prepared a fiberoptic bronchoscope to guide the nasotracheal intubation before the operation, and we were ready for tracheotomy. We located the tracheostomy puncture point using ultrasound guidance to prepare for a tracheotomy (Figure 2) after the patient entered the operating room. She could not lie on her left side due to the pain in her left cheek, so we performed combined spinal-epidural anesthesia on the right lateral decubitus at L2-3 using the needle-through-needle technique (A 25G pencil point spinal needle and a 16G epidural needle), after a failed puncture at L3-4. In order to ensure the effect of intraspinal anesthesia, 3 mL of 0.5% bupivacaine was administered, and the anesthesia reached the level of T4. Her vital signs were stable during the operation, and the fetus was removed routinely with Apgar scores of 10 at 1, 5, and 10 min. After the operation, she continued to undergo anti-infective treatments. Three days later, she was safely discharged and transferred to a dental hospital for further treatment.
Oral diseases during pregnancy not only affect the mother, but also affect the fetus and pregnancy outcomes. Several studies have found that periodontal disease is a risk factor for adverse pregnancy outcomes such as a preterm birth, fetal growth restriction, the development of preeclampsia, and a low birth weight[3], and the active treatment of periodontal disease during pregnancy can reduce the incidences of premature births and low body weight infants[4]. There is no clear conclusion regarding the specific mechanism of how oral diseases affect pregnancy outcomes. At present, researchers have mainly proposed two possible mechanisms: First, oral pathogens transmit and colonize the placenta through the bloodstream, which has been verified after finding oral bacterial DNA in the placentas of high-risk mothers[5]; second, inflammatory mediators produced from periodontal disease act on uterine smooth muscle, which could cause muscle contraction and promote a preterm birth, which can affect the blood supply of the placenta and influence fetal growth. These speculations have only been verified in animal models[6], and further research is still needed to prove these hypotheses. In short, pregnant women with periodontal infections not only face the risk of treatment difficulties but also face a high risk of obstetric emergencies.
Intraspinal anesthesia: For patients with severe local infections, the possibility of systemic infection needs to be considered before the infection is treated. To date, there are no definite guidelines for using intraspinal anesthesia in patients with infection or sepsis. However, many studies have shown that sepsis is not an absolute contraindication for intraspinal anesthesia. Among patients with or possibly suffering from bacteremia, the incidence of central nervous system infection after intraspinal puncture is 0.007%-0.6%[7]. Some researchers have also proposed that spinal anesthesia could be used for patients whose generalized infection is controlled by appropriate antibiotics or if the patient shows indications that they are responding to treatment, such as a decrease in body temperature. However, whether an epidural catheter can be placed safely is still controversial[7]. In the case presented here, the patient had symptoms of generalized infection, including a high temperature of 38.1 °C, a WBC count of 14.0 x 109/L, and a C-reactive protein level of 36.1 mg/L. She received broad-spectrum antibiotics after admission to the hospital. On the day of the operation, her body temperature decreased, so we performed spinal and epidural anesthesia.
General anesthesia: General anesthesia should be considered when such patients have generalized infections or other contraindications and if intraspinal anesthesia has failed. Relevant studies and guidelines point out that airway assessment, such as using direct laryngoscopy or visual laryngoscopy to check the airway under topical anesthesia, should be performed during the second trimester of pregnancy or when the disease progresses to prepare for an elective cesarean[8]. After laryngoscopy, pregnant women with acceptable intubation conditions and no difficulty in facemask ventilation can choose rapid sequential induction. However, most of these patients have predictably difficult airways, and it is generally accepted that awake tracheal intubation is a safe airway management method[9]. Furthermore, nasal tracheal intubation using flexible bronchoscopy may be easier for patients with a limited mouse opening or if patients have oral sinus or purulent secretions[10], but the risk of nasal mucosal hemorrhage is higher due to the edema of the upper airway during pregnancy. Topical anesthesia with tetracaine or lidocaine in the nasal cavity and pharyngeal cavity, as well as the injection of local anesthetics through a cricothyrocentesis or a posterior superior nerve block under ultrasound guidance, can reduce airway stress. However, it should be noted that the risk of systemic toxicity of local anesthetics in pregnant women is higher and should be used with caution. The combination of lidocaine and phenylephrine is recommended[11]. Awake tracheal intubation guidelines for difficult airways in 2019 pointed out that sedative drugs, such as dexmedetomidine and remifentanil, are available for awake intubation for obstetric procedures and are less toxic to fetuses[11]. Before that, high-flow nasal oxygen can be considered for preoxygenation[12]. In addition, preparations should be made in cases of failure of intubation, such as in patient positioning, the preparation for cricothyrocentesis using ultrasound guidance, and the preparation of personnel and materials for tracheotomy.
It is obviously not appropriate to spend 5-10 min or even longer to perform awake tracheal intubation for general anesthesia or intraspinal anesthesia if placental abruption or fetal distress occurs, because these conditions warrant an emergent cesarean section during labor. Even with laryngoscopy or fiberoptic bronchoscopy and other equipment to visualize the anatomy, some patients may still fail to have intubation performed. In these cases, tracheostomy should be considered. Considering that the spread of inflammation may invade the surrounding tissues around the trachea and may compress the trachea and cause displacement, the location of the cricothyroid under ultrasound guidance can be determined before surgery. At the same time, the otolaryngologist should be notified to be present in the preparation of an emergency tracheotomy.
Difficult airway assessment: Most of these patients have difficult airways. Regardless of which anesthesia method is selected, airway management is important. The preoperative evaluation of difficult airways is necessary. Song et al[13] showed that in patients with oral and maxillofacial space infections, the laryngopharynx is prone to displacement due to the lack of a bony structural support, and its volume and average cross-sectional area at this level are associated with difficult airway. At present, a variety of techniques for three-dimensional airway reconstruction and assessment of difficult airways based on imaging such as CT, magnetic resonance imaging (MRI), and ultrasound, have been proposed, which allows anesthesiologists to more intuitively observe the anatomical changes of the patient's throat. Jain et al[14] summarized that by using CT high-resolution scanning, providers can complete the scan with the patients holding their breath. Compared to MRI, CT has fewer artifacts affected by breathing, and it scans the bony structures more accurately. MRI is more advantageous in soft tissue and inflammatory changes, and the effects of radiation can be ignored. In addition, there was no significant difference between ultrasound and CT in the measurement of airway structures[15]. Using imaging results to calculate and construct a three-dimensional model can intuitively measure the airway structure, which helps anesthesiologists evaluate difficult airways and prepare for airway management.
Above all, this is the first case report of anesthesia management of cesarean section in pregnant women with odontogenic infection. Our deficiency is that sufficient amount of bupivacaine should not be given to ensure anesthetic effect, which may affect her breath caused by high level of anesthesia. Fortunately, this did not happen, and we have made full preparations.
During pregnancy, oral infections may progress rapidly. The spread of inflammation not only endangers mothers’ lives but could also cause premature deliveries and threaten labor. Therefore, an adequate preoperative multidisciplinary evaluation should be performed, and selective termination of pregnancy should be chosen as much as possible to avoid the need for emergency airway management[12]. However, obstetrician support is necessary to ensure the safety of the mother and fetus if surgical intervention is needed to treat oral and maxillofacial infections.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta A, India; Karna ST, India S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Turner M, Aziz SR. Management of the pregnant oral and maxillofacial surgery patient. J Oral Maxillofac Surg. 2002;60:1479-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Lee JK, Kim HD, Lim SC. Predisposing factors of complicated deep neck infection: an analysis of 158 cases. Yonsei Med J. 2007;48:55-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | Komine-Aizawa S, Aizawa S, Hayakawa S. Periodontal diseases and adverse pregnancy outcomes. J Obstet Gynaecol Res. 2019;45:5-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 4. | López NJ, Smith PC, Gutierrez J. Periodontal therapy may reduce the risk of preterm low birth weight in women with periodontal disease: a randomized controlled trial. J Periodontol. 2002;73:911-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 334] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 5. | Aagaard K, Ma J, Antony KM, Ganu R, Petrosino J, Versalovic J. The placenta harbors a unique microbiome. Sci Transl Med. 2014;6:237ra65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1218] [Cited by in RCA: 1372] [Article Influence: 124.7] [Reference Citation Analysis (0)] |
| 6. | Kunnen A, van Pampus MG, Aarnoudse JG, van der Schans CP, Abbas F, Faas MM. The effect of Porphyromonas gingivalis lipopolysaccharide on pregnancy in the rat. Oral Dis. 2014;20:591-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Gimeno AM, Errando CL. Neuraxial Regional Anaesthesia in Patients with Active Infection and Sepsis: A Clinical Narrative Review. Turk J Anaesthesiol Reanim. 2018;46:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Mushambi MC, Athanassoglou V, Kinsella SM. Anticipated difficult airway during obstetric general anaesthesia: narrative literature review and management recommendations. Anaesthesia. 2020;75:945-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 9. | Xue FS, Lie YY, Li HX. Selection and analysis of algorithms for difficult airway management. Int J Anesthesiol Resusc. 2017;38:961-966. [DOI] [Full Text] |
| 10. | Zhao L, Liu L. Perioperative airway management strategy in patients with maxillofacial space infection. Zhongguo Dangdai Yixue. 2020;27:165-167+174. [DOI] [Full Text] |
| 11. | Ahmad I, El-Boghdadly K, Bhagrath R, Hodzovic I, McNarry AF, Mir F, O'Sullivan EP, Patel A, Stacey M, Vaughan D. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020;75:509-528. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 135] [Cited by in RCA: 259] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 12. | Mushambi MC, Kinsella SM, Popat M, Swales H, Ramaswamy KK, Winton AL, Quinn AC; Obstetric Anaesthetists' Association; Difficult Airway Society. Obstetric Anaesthetists' Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia. 2015;70:1286-1306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 296] [Cited by in RCA: 328] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 13. | Song Q, Yan J, Zhou R, Zhang L, Jiang H. Application of 3D-CT reconstruction technology to predicting difficult airway in patients with odontogenic infections. Shanghai Jiaotong Daxue Xuebao. 2020;40:1263-1269. [DOI] [Full Text] |
| 14. | Jain K, Gupta N, Yadav M, Thulkar S, Bhatnagar S. Radiological evaluation of airway - What an anaesthesiologist needs to know! Indian J Anaesth. 2019;63:257-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Prasad A, Yu E, Wong DT, Karkhanis R, Gullane P, Chan VW. Comparison of sonography and computed tomography as imaging tools for assessment of airway structures. J Ultrasound Med. 2011;30:965-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (1)] |