Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4550
Peer-review started: September 21, 2021
First decision: October 22, 2021
Revised: November 3, 2021
Accepted: March 25, 2021
Article in press: March 25, 2021
Published online: May 16, 2022
Processing time: 234 Days and 2.1 Hours
Treating periodontally hopeless teeth with advanced bone resorption and severe tooth mobility is a great challenge for both orthodontists and periodontists. Biofilm-induced periodontal inflammation and occlusal trauma-related inflammation may synergistically aggravate tooth mobility. This case report illustrates that even periodontally hopeless teeth can be saved and have long-term stability with comprehensive periodontal treatment to control periodontal inflammation and promote periodontal bone regeneration and intricate orthodontic mechanical control to correct cross bite and occlusal trauma.
A 27-year-old female patient whose chief complaint was severe tooth mobility and discomfort of the maxillary incisor was diagnosed with severe aggressive periodontitis by clinical and radiographic examinations. To reduce tooth mobility and establish stable occlusion, we combined orthodontic treatment with periodontal therapy to preserve the tooth. Orthodontic treatment was performed after basic periodontal therapy and periodontal surgery. The loosened upper right central incisor was successfully retained, and the periodontal tissue remained stable during follow-up.
Teeth with severe mobility and bone loss can be saved through interdisciplinary treatment when periodontal inflammation is strictly controlled.
Core Tip: Traditionally severe tooth mobility may affect the prognosis after orthodontic tooth movement, since orthodontic treatment has been reported to increase tooth mobility. However, whether orthodontic tooth movement can be conducted in “periodontally hopeless teeth” with Class III mobility has never been reported. In this case report, we described periodontal-orthodontic interdisciplinary treatment of a case with a “periodontally hopeless” upper central incisor with Class III mobility.
- Citation: Jiang K, Jiang LS, Li HX, Lei L. Periodontal-orthodontic interdisciplinary management of a “periodontally hopeless” maxillary central incisor with severe mobility: A case report and review of literature. World J Clin Cases 2022; 10(14): 4550-4562
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4550.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4550
Periodontitis, an inflammatory response to invading periodontal pathogens, may lead to the destruction of periodontal supporting tissues[1]. Tooth mobility, a common symptom of advanced periodontitis, is a major reason patients seek dental consultation and a main factor of clinical decision-making by dentists[2]. Loss of supportive periodontal tissue height and widening of the periodontal ligament are the underlying mechanisms of increased tooth mobility[3]. Occlusal trauma-induced tooth mobility, a result of periodontal membrane widening rather than inadequate bone support, can be caused by acute periapical periodontitis, orthodontic treatment, or prosthesis implantation[4]. Malocclusion-associated occlusal trauma is well recognized in patients with a deep impinging overbite or anterior dental crossbite[5,6].
Teeth with significant supportive periodontal tissue loss are especially prone to occlusal trauma, which has been defined as secondary occlusal trauma[7,8]. Primary occlusal trauma mainly refers to occlusal trauma occurring before the presence of periodontal disease and is regarded as a synergistic factor of periodontal disease. Despite consensus on the definitions of primary and secondary occlusal trauma, specific criteria of reduced periodontal support that leads to a clinical diagnosis of secondary occlusal trauma have not been identified clearly. Since both periodontal inflammation and occlusal trauma can result in an increase in the tooth mobility, any clinical decision should be made only after periodontal inflammation is well controlled and occlusal trauma is clearly alleviated[9]. Clinical diagnosis that occlusal trauma has occurred or is occurring may include progressive tooth mobility, fremitus, occlusal discrepancies, tooth migration, root resorption, etc. Once alveolar bone absorption exceeds 70% of total bone support, secondary occlusal trauma and severe tooth mobility may ensue, leading to a possible diagnosis of “periodontally hopeless teeth”[10].
Orthodontic treatment after the careful periodontal treatment of periodontally compromised teeth with pathological tooth migration has been reported in some cases[11-13], and the prerequisites for orthodontic intervention are controlled periodontal inflammation and reduced mobility after strict periodontal treatment[14]. Occlusal adjustment and periodontal splinting have been advocated to stabilize periodontally questionable and hopeless teeth[15,16]. Traditionally, severe tooth mobility may affect the prognosis after orthodontic tooth movement[14], since orthodontic treatment has been reported to increase tooth mobility[17]. However, there is no consensus concerning whether orthodontic tooth movement can be conducted for “periodontally hopeless teeth” with class III mobility.
Extraction of teeth with severe attachment loss has been a common practice in the past because it is expensive to preserve such teeth and the prognosis is usually poor. In addition, in the absence of periodontal treatment, the retention of "hopeless" teeth has a destructive effect on the periodontium of adjacent teeth[18,19]. Although orthodontic treatment in subjects with aggressive periodontitis have been reported[14,20], orthodontic-periodontal interdisciplinary treatment in periodontally hopeless teeth has seldom been reported. In this case report, we describe the periodontal-orthodontic interdisciplinary treatment of a “periodontally hopeless” upper central incisor with class III mobility with a good prognosis over a follow-up period of 3 years.
A 27-year-old female had a chief complaint of severe tooth mobility and discomfort of the maxillary incisor.
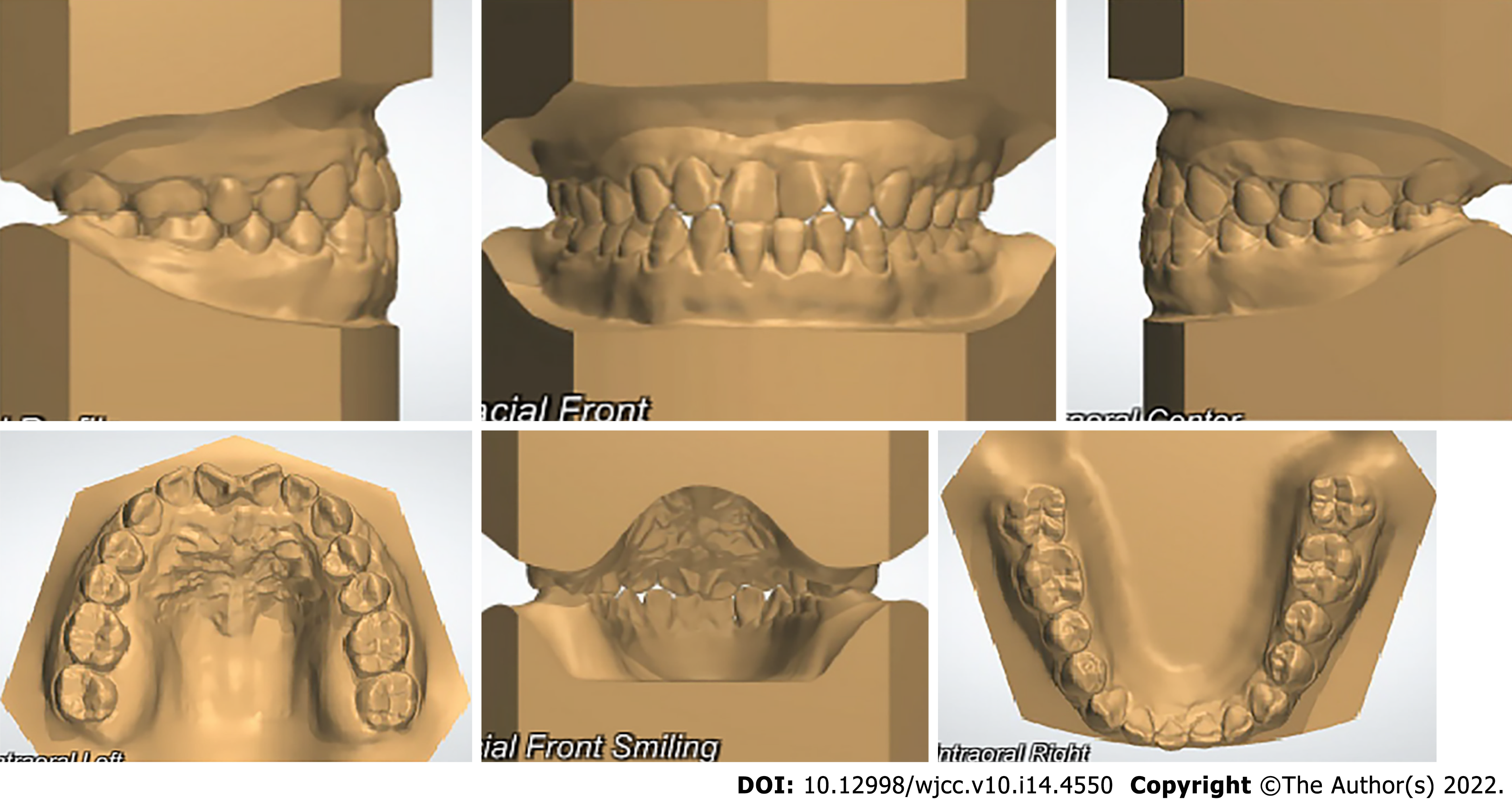
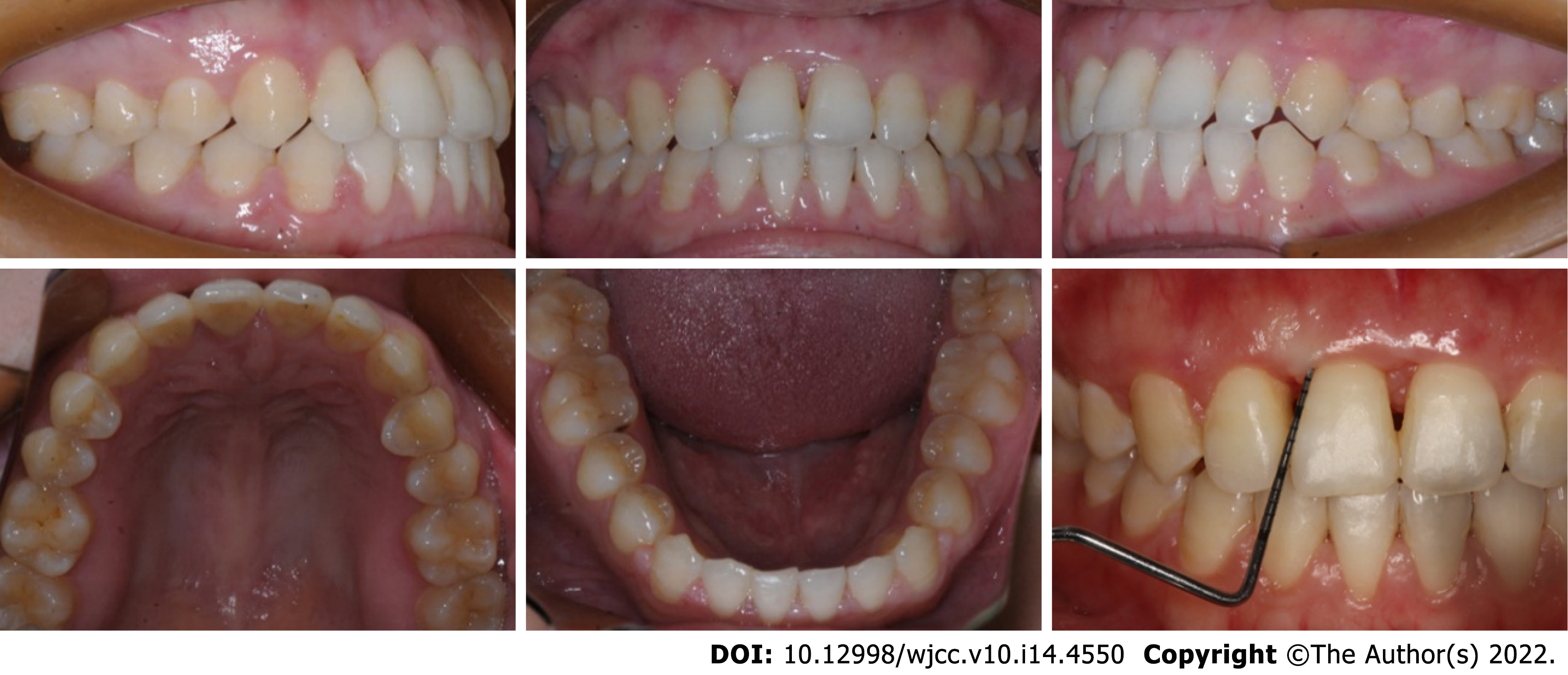
The patient was referred by the periodontist for orthodontic advice. Despite strict periodontal maintenance for half a year, periodontal treatment failed to reduce tooth mobility. The patient had a site of edge-to-edge occlusion with a tendency for a crossbite in the incisor region. Angle class I molar relationships were observed on both sides. Her maxillary central incisors were rotated, especially the upper right central incisor (Figures 1 and 2). The upper right central incisor displayed class III mobility.
She did not have any history of systemic illness.
The patient had a non-contributory personal and family history.
Her oral hygiene was good and all permanent teeth were present. The upper right central incisor displayed class III mobility.
The patient's blood test results were all normal.
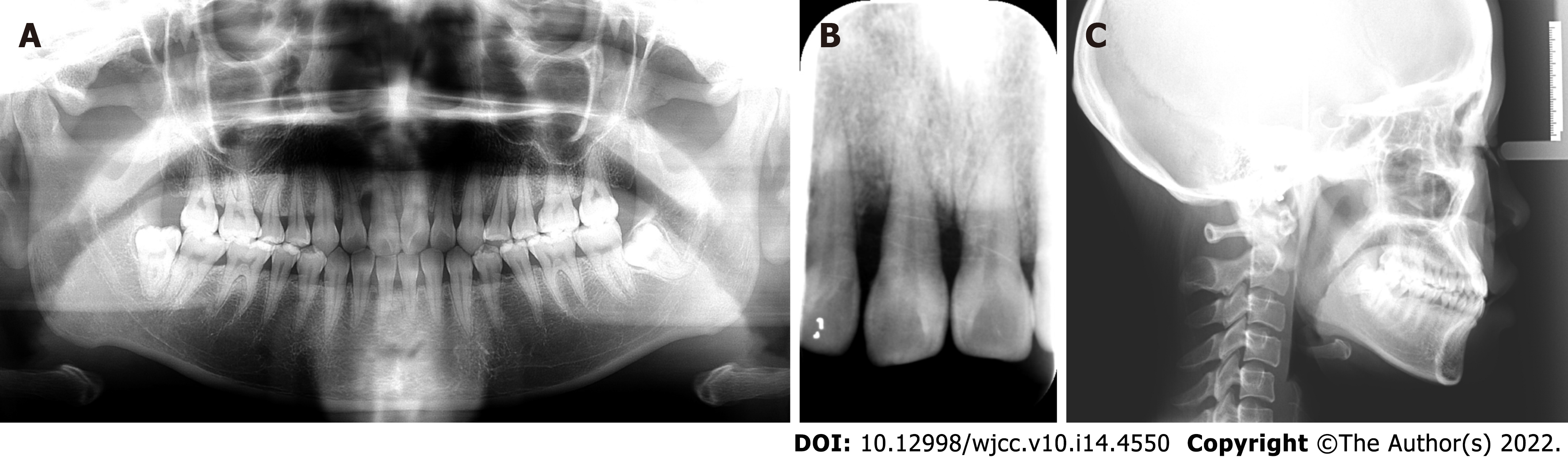
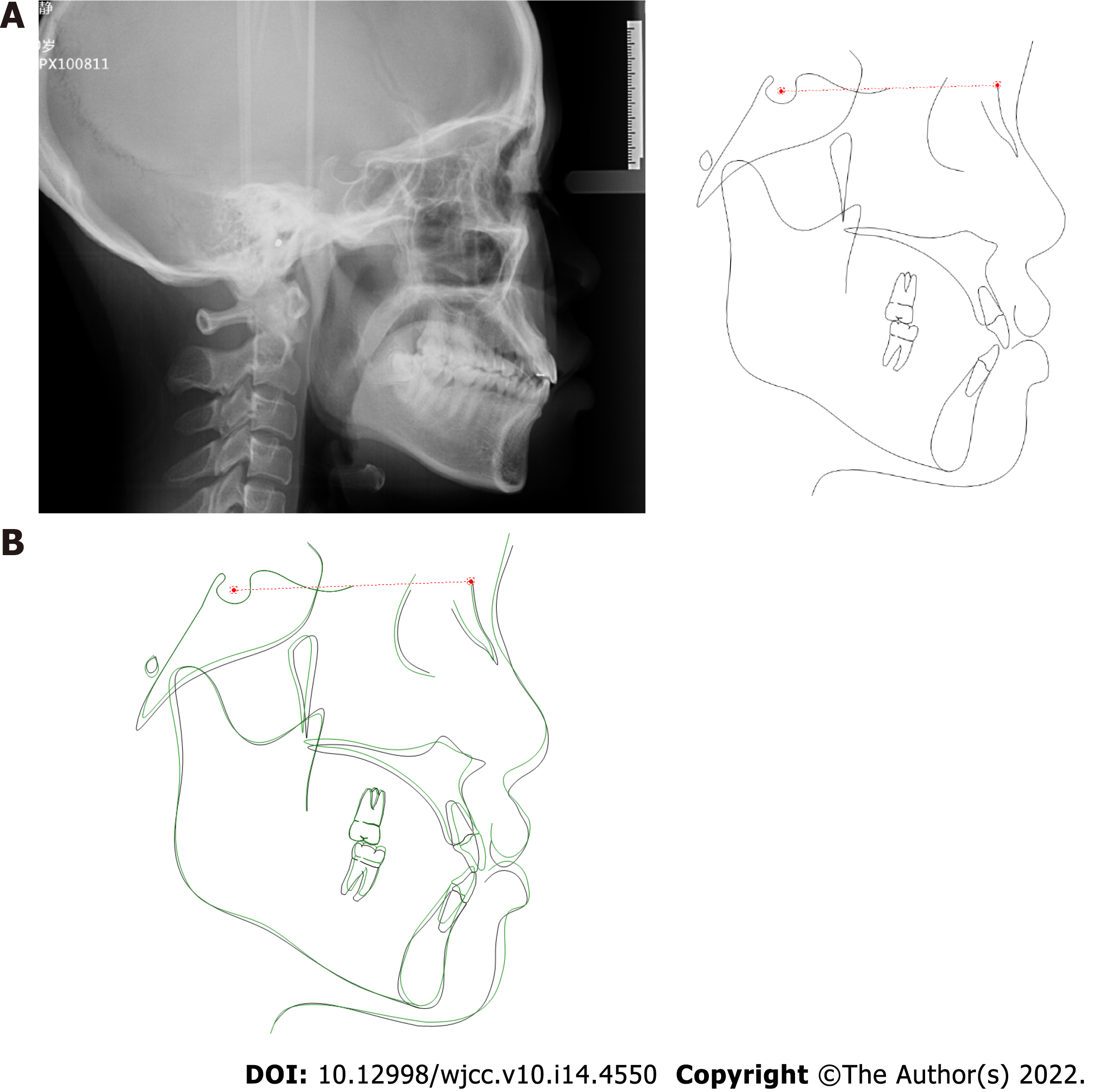
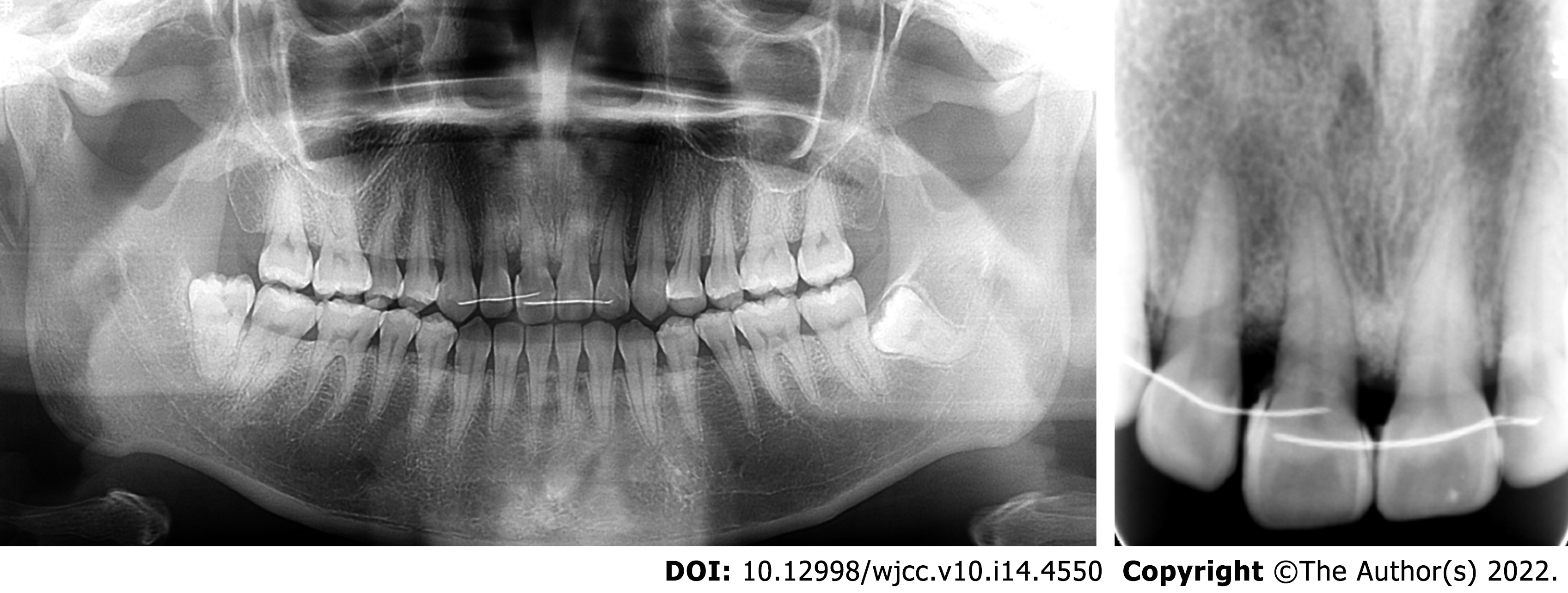
In the region of the maxillary right central incisor on the apical radiograph, less than 25% of remaining alveolar bone was observed, and extensive but relatively mild alveolar bone resorption could be seen on the panoramic radiograph in other regions (Figure 3). The upper right central incisor displayed class III mobility. Cephalometric analysis showed that the patient showed a skeletal class III tendency and an average angle with proclined upper incisors and retroclined lower incisors (Table 1).
| Measurement | norm ± SD | Pretreatment | Posttreatment |
| Maxilla to cranial base | |||
| SNA (°) | 82.8 ± 4.0 | 85.0 | 85.1 |
| Mandible to cranial base | |||
| SNB (°) | 80.1 ± 3.9 | 83.7 | 83.8 |
| SN-MP (°) | 32.5 ± 5.2 | 26.6 | 26.3 |
| FMA (MP-FH) (°) | 31.3 ± 5.0 | 23.1 | 22.2 |
| Maxillomandibular | |||
| ANB (°) | 2.7 ± 2.0 | 1.3 | 1.3 |
| Maxillary dentition | |||
| U1-NA (mm) | 5.1 ± 2.4 | 4.6 | 6.9 |
| U1-SN (°) | 101.3 ± 5.7 | 107.3 | 110.2 |
| Mandibular dentition | |||
| L1-NB (mm) | 6.7 ± 2.1 | 6.3 | 6.1 |
| L1-MP (°) | 93.0 ± 5.8 | 95.2 | 91.7 |
| Soft tissue | |||
| Lower lip to E-plane (mm) | -1.0 ± 1.0 | 4.1 | 3.0 |
| Upper lip to E-plane (mm) | 1.0 ± 2.0 | -0.1 | -0.2 |
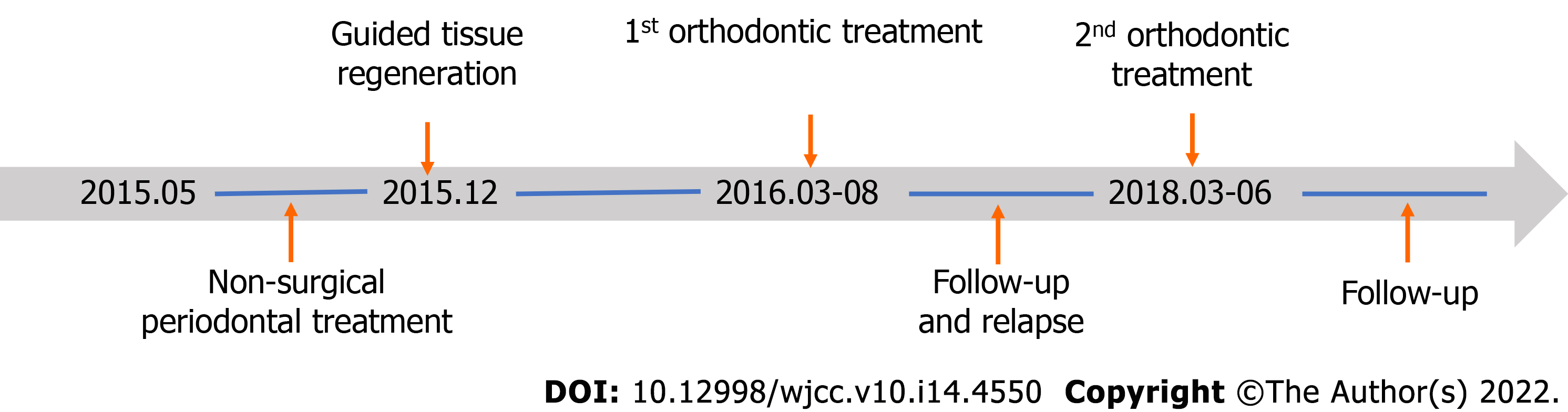
Based on the information, the patient was diagnosed with skeletal class I malocclusion and anterior crossbite. When the patient first visited the periodontal department, she was diagnosed with severe aggressive periodontitis (classification 2018: stage IV grade C). The primary aim of periodontal and orthodontic treatment was to reduce tooth mobility and preserve the upper right central incisor. The long-term goal was to establish stable occlusion and maintain periodontal tissue health to prevent tooth extraction. The treatment plan was as follows: (1) Initial periodontal treatment (full-mouth scaling and root planning, tooth brushing instruction); (2) Periodontal surgery (guided tissue regeneration, GTR); (3) Orthodontic treatment; and (4) Supportive periodontal therapy.
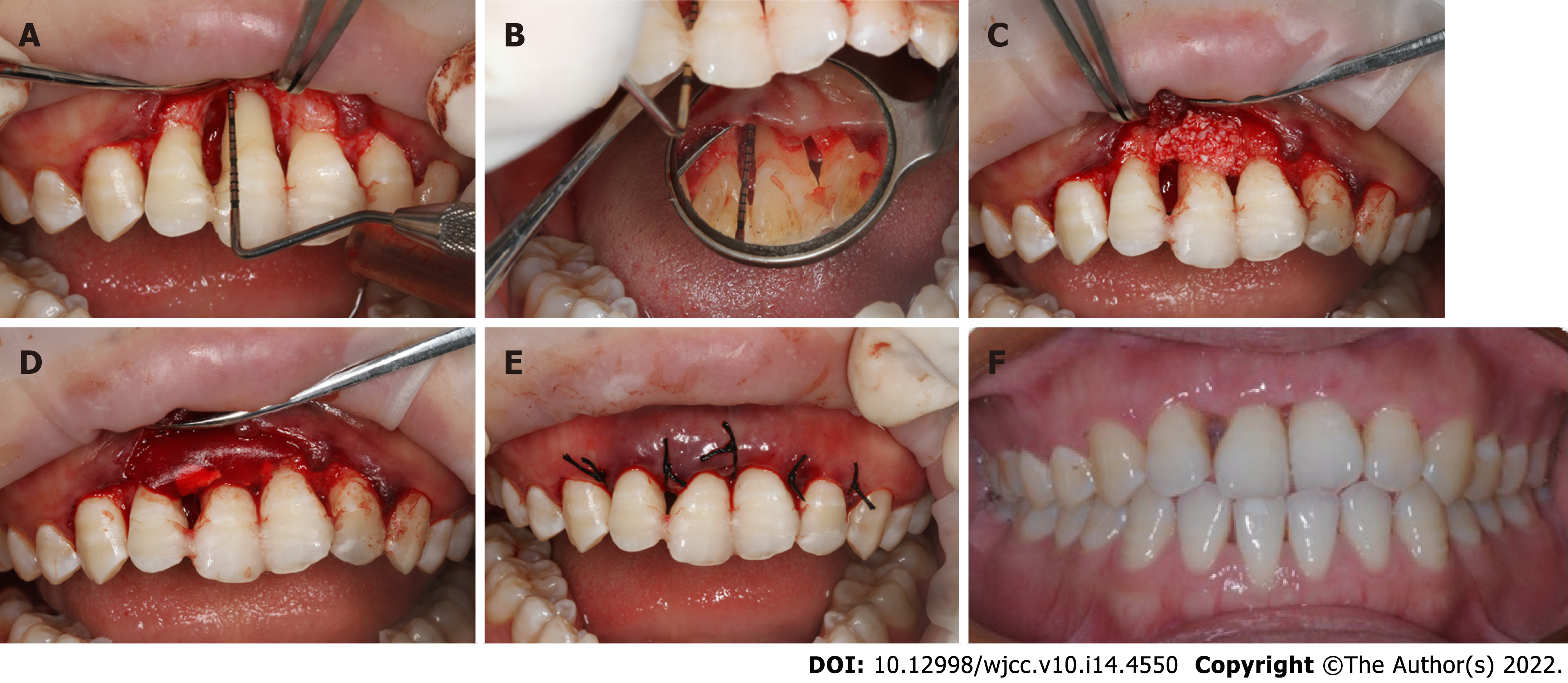
The overall treatment process is shown in Figure 4. After initial periodontal therapy, a splint was placed on the maxillary front teeth to avoid further occlusal trauma and facilitate periodontal repair. Periodontal surgery (guided tissue regeneration) was performed to augment the alveolar bone and soft tissue. Significant bone loss up to the apical third was observed on both the buccal and lingual sides during the surgery. After complete curettage and debriding, bovine-derived xenograft Bio-Oss® was placed in the bony defect area, and then the bone particulates were covered with an absorbable collagen membrane to prevent early epithelial cell attachment onto the root surface and provide anatomical space for periodontal regeneration (Figure 5).
Two months later, an acceptable periodontal health condition was observed; however, the upper right central incisor still displayed class III tooth mobility, and gingival recession was observed at both the mesial and distal papilla after removal of the resin splint (Figure 5F). A conventional 0.022-in × 0.028-in straight-wire appliance with a McLaughlin-Bennet prescription was placed. A 0.012-inch nickel-titanium arch wire was inserted in both the maxillary and mandibular arches to align the teeth; meanwhile, a bite turbo was placed on the mandibular molars to relieve the occlusal interference. Unexpectedly, the mobility of the upper right central incisor was reduced to class I mobility after preliminary alignment. Further alignment with 0.012-in NiTi wires in the maxillary arch and 0.018-in NiTi wires in the mandibular arch was performed at month 2. A 0.018-in Australian arch wire was inserted in the mandibular arch to close the space at month 3 with power chain. To further increase the overjet and reduce the premature contact, we performed an interproximal reduction (IPR) of 1.0 mm to gain further space for lower incisor retraction at month 4. In the last mouth of the treatment, we used 0.018-in Australian arch wires for finishing and detailing in the mandibular and maxillary arch (Figure 6).
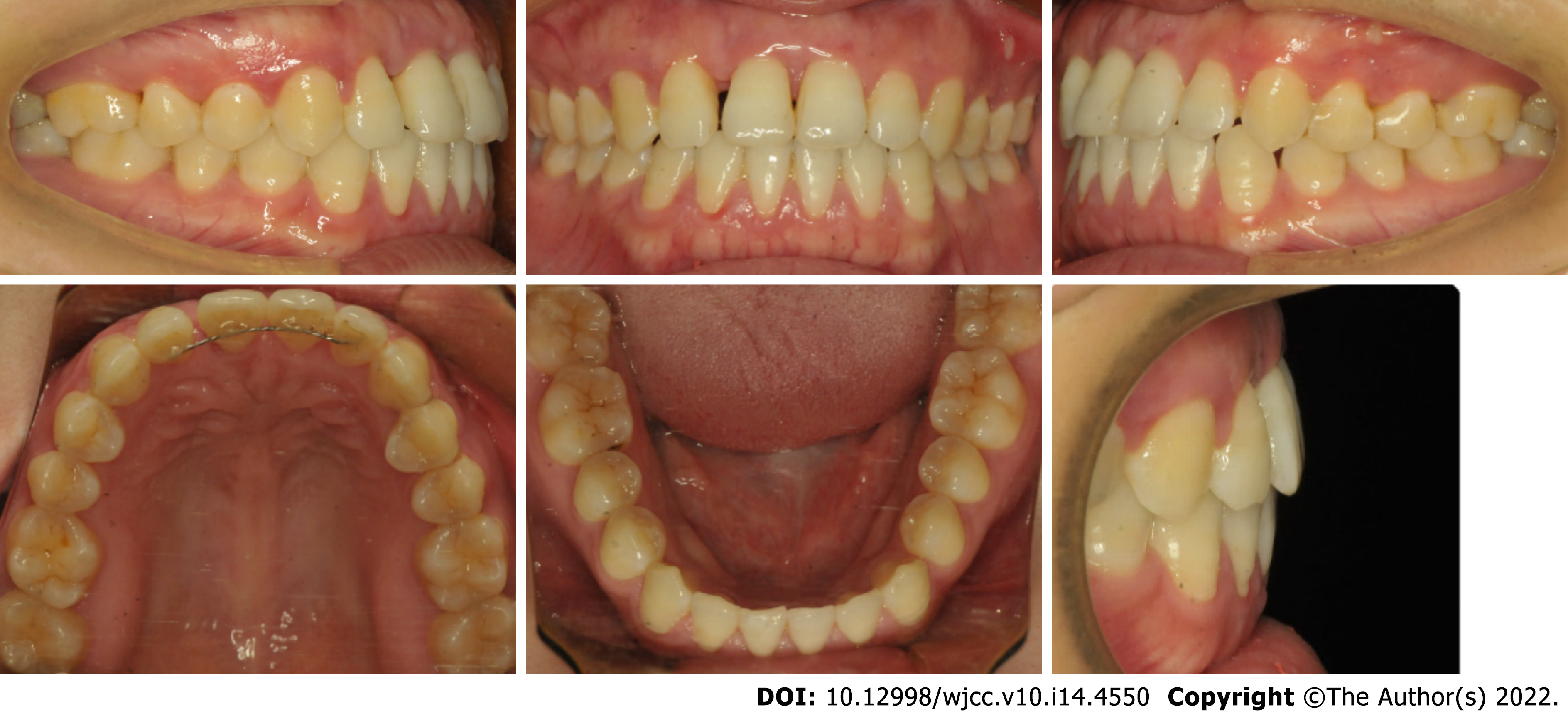
After 5 mo of active orthodontic treatment, the crossbite was corrected. At the end of orthodontic treatment, the mobility of the upper right central incisor was improved to class I, while the periodontal tissue was in good condition, with no deep periodontal pockets (Figure 7). A fixed retainer was placed to prevent relapse of rotation and stabilize the dentition.
The patient was recalled after 15 mo. Unexpectedly, a space of 1 mm was observed between the upper right lateral incisor and the upper right central incisor, although the fixed retainer was stable and not broken (Figure 8), indicating the presence of occlusal trauma. At this stage, minor premature contact was still observed.
Two treatment alternatives were proposed for the patient this time. The first option was comprehensive orthodontic treatment of both the upper and lower arches. Further IPR of 2 mm was needed to close the space in the upper arch and relieve the premature contact. Since the lower incisors were already lingually inclined, such IPR may lead to relapse in the lower arch, potentially followed by occlusal trauma. The second option was orthodontic treatment of only the maxillary arch. A space of 2 mm would be placed on the distal side of the upper right canine, and the space could be restored by the resin composite. The black triangle, space, and premature contact between the front teeth could all be resolved, and a high probability of posttreatment stability could be expected. The patient finally chose option 1.
The second orthodontic treatment was conducted for three months. A NiTi super-elastic coil was utilized to open space between the canine and the premolar, then the space was finally placed on the distal side of the upper right canine. We use composite resin materials to restore the space and improve the black triangle. A lingual bonded retainer from the canine to the incisor in the upper arch was placed to stabilize the occlusion of the upper arch (Figure 9).
The mobile tooth was stabilized, and periodontal inflammation was well controlled. Owing to the establishment of normal incisal guidance in the anterior region without occlusal interference, the occlusal trauma disappeared, as demonstrated by the cephalometric measurement (Figure 10 and Table 1). The angle of U1-SN was increased from 107.3° to 110.2°, while the angle of L1-MP was decreased from 95.2° to 91.7°. The improved inter-incisal relationship contributed to correction of early contact and removal of occlusal trauma. Both the posttreatment panoramic radiograph and apical radiographs showed that the resorption of alveolar bone was under control and that newly formed trabecular bone was present in the region with severe resorption. Apart from this, there was no marked root resorption. The panoramic radiograph (43 mo after periodontal surgery and 2 mo after the second orthodontic treatment) showed that the alveolar ridge height remained relatively stable, and even newly formed trabecular bone could be seen in the region with severe resorption (Figure 11). The occlusion remained stable over a further follow-up period of 1 years (Figure 12). The patient was very satisfied with the final treatment result. A recent follow-up visit (70 mo after periodontal surgery and 39 mo after the second orthodontic treatment) showed that the tooth remained stable, functionally and aesthetically. The maxillary central incisor has no obvious looseness and deep periodontal pocket. Compared with the previous apical radiograph, the alveolar bone had no obvious absorption (Figure 13).
Biofilm-induced periodontal infection, occlusal trauma-associated sterile inflammation, and orthodontic tooth movement-related inflammation can all contribute to periodontal membrane widening and tooth mobility[4]. Our present case report demonstrates that despite class III tooth mobility and vertical bone absorption to the apex, a “periodontally hopeless tooth” can be retained after comprehensive periodontal treatment and precise orthodontic treatment.
Without plaque-induced inflammation, occlusal trauma did not cause irreversible bone loss or attachment loss in some animal studies[21-23]. Occlusal trauma models in mice, rats, dogs, and monkeys are mostly established by an elevation of occlusion[23-25]; therefore, such hyperocclusion may differ from the occlusal forces in the lateral excursion and various forms of malocclusion. Periodontal pathogenic bacteria, the host immune reaction, the familial gene background, and behavioral factors can aggravate alveolar bone resorption in periodontitis patients. In this case, the rotated upper right central incisor bore traumatic force from several incisors of the lower arch, leading to bone loss to the apex, while inadequate correction of occlusal trauma in the first phase led to the presence of a space between the lateral incisor and canine. This case clearly demonstrates that long-term occlusal trauma can induce severe periodontal bone loss.
Two treatment options have been proposed in the first stage. The first was orthodontic treatment to establish a fine and stable occlusion after the periodontal treatment. The corrected occlusion might be beneficial to the long-term periodontal health. The disadvantage was the further periodontal destruction as well as an economical burden of orthodontic treatment. The second option was to place an implant after incisor extraction. Such plan can greatly shorten the time of total treatment. However, insufficient bone mass, lack of soft tissue and poor occlusal condition may pose a great challenge for the long-term survival of the implant. Since tooth mobility may improve after correction of the malocclusion, we finally chose the conservative option to try orthodontic correction. The patient understood and accepted the risks that may occur during orthodontic treatment.
Orthodontic treatment is a double-edged sword for patients with severe periodontitis. On the one hand, orthodontic treatment can help improve the dentition arrangement and change the occlusal relationship[14,26]. On the other hand, clinical and experimental studies have shown that when inflammation is not fully controlled orthodontic treatment may trigger inflammatory processes and accelerate the progression of periodontal destruction leading to further loss of attachment, even in patients with sound oral hygiene[27]. There is also a great risk of additional attachment loss and bone loss if the orthodontic force used is improper[14]. Orthodontic force may induce bone absorption on the side under compression and bone deposition on the side under tension; therefore, proper orthodontic diagnosis should be performed and treatment plans should be prepared to minimize further bone loss during orthodontic tooth movement[28]. In addition, although orthodontic force does not induce changes in the alveolar bone level[11,29], it may induce apical root resorption in teeth affected by periodontitis, especially in teeth with intrusion, since periodontal ligament loss may expose the periodontal tissue to greater force[30]. The long-term outcomes of orthodontic on the periodontal health have been controversial. A recent systematic review demonstrated that orthodontic therapy was associated with 0.03 mm of gingival recession, 0.13 mm of alveolar bone loss, and 0.23 mm of increased pocket depth when compared with no treatment[31]. In the present case, labial tipping of the upper incisors may have further decreased the buccal bone support; therefore, we performed gene replacement therapy to reduce further alveolar bone loss.
Bone regeneration was still a challenge in the horizontal alveolar bone defect. To improve the thin periodontal phenotype and maintain soft tissue stability, we used Bio-Oss bone particulates, which have a slower degradation rate and maintain the three-dimensional gingiva contour in a long term. Traditional guided tissue or bone regeneration is mainly used in the treatment of vertical bone resorption or molar root bifurcation lesions. It promotes periodontal regeneration through bone filling materials and barrier membranes to form new periodontal attachments. Periodontally accelerated osteogenic orthodontics is a clinical procedure that combines selective alveolar corticotomy, particulate bone grafting and the application of orthodontic forces[32], majorly conducted in patients with healthy periodontal status. Regional acceleratory phenomena (RAP) induced by corticotomy promotes alveolar bone remodeling and accelerate toot movement, while the alveolar augmentation expands bone boundaries and benefits periodontal conditions[33].
The timing and type of periodontal intervention are also controversial in the interdisciplinary treatment of periodontally compromised teeth. Previously, full healing of periodontal tissues for 6 mo was advocated before any orthodontic tooth movement. Later, orthodontic tooth movement was initiated as early as 7–10 d after periodontal surgery[28,29,34]. The biological philosophy underlying early treatment is the RAP, by which the inflammatory response after an injury may promote tissue health[24]; therefore, the inflammatory response during periodontal tissue healing after periodontal surgery may promote orthodontic tooth movement. The cytokine-mediated acceleration of orthodontic tooth movement has been utilized in various biology-based techniques, including micro-osteoperforation, bone corticotomy and piezocision[25]. In the present case, although we did not conduct orthodontic treatment early after GTR, the periodontal inflammation from occlusal trauma still promoted quick alignment and crossbite correction.
Our understanding of the nature of periodontal health and inflammation has greatly changed our perspectives regarding orthodontic tooth movement, alveolar bone remodeling and periodontal inflammation. In the most recent periodontal classifications of both the American Academy of Periodontology and European Federation of Periodontology, clinical gingival health on a reduced periodontium in a patient with stable periodontitis is defined as periodontal health and gingival health. Therefore, based on strict biofilm and periodontal risk screening, orthodontic treatment can be performed on a periodontally healthy patient[14].
The clinical decision of fixed appliances or removable clear aligners is important for the prognosis of periodontally hopeless teeth[35]. Despite its convenience of oral hygiene, clear aligners may produce large instantaneous stress on the periodontal tissue during repeated removal and wear[36]. Considering the extreme tooth mobility in this case, mechanic force during wearing aligners may aggravate periodontal status. Therefore, fixed appliance is a better choice for teeth with severe tooth mobility.
The clinical decision to treat or extract “periodontally hopeless teeth” should take into consideration several factors, including clinical parameters, assessed risk, financial aspects, and individual motivation. The survival rate of hopeless teeth in patients with aggressive periodontitis varied from 38% over 10 years to 59.5% over 15 years[10]. Despite reports regarding orthodontic treatment in patients with aggressive periodontitis[14], chronic periodontitis[28], and pathological tooth migration[37], there are very few reports about the prognosis of orthodontically treated hopeless teeth. In the present case, advanced bone loss and severe tooth mobility posed a great challenge in diagnosis and treatment. The long-term synergistic effects of occlusal force and periodontal inflammation led to severe bone loss. We observed improved tooth mobility after unlocking the bite by bite turbo in the molar region, indicating that occlusal trauma contributed to the severe tooth mobility. Therefore, occlusal trauma should be considered during the diagnosis of “periodontally hopeless teeth”; moreover, the indications for and contraindications to the orthodontic treatment of periodontally compromised teeth should take into consideration not only periodontal bone loss but also underlying occlusal trauma.
Despite stable periodontal and orthodontic treatment outcomes in teeth with class III mobility, risks during the orthodontic treatment of teeth with advanced periodontitis should never be ignored. The changes in the biomechanical characteristics of a severely reduced periodontal membrane may lead to an apical shift of the center of resistance; therefore, orthodontic mechanical force may further strain the periodontal ligament of the hypermobile tooth[38], and the inflammatory response during orthodontic tooth movement may accelerate periodontal bone absorption[4].
In this case, the loosened upper right central incisor was successfully retained, and the periodontal tissue remained stable during the follow-up period. This result proves that teeth with severe mobility and bone loss can be saved through interdisciplinary treatment when periodontal inflammation is strictly controlled. Malocclusion-associated or occlusal trauma-related tooth mobility should be an important consideration in diagnosing and planning treatment for periodontally compromised teeth.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ozturk T, Turkey; Zhang Y, China S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Van Dyke TE, Sima C. Understanding resolution of inflammation in periodontal diseases: Is chronic inflammatory periodontitis a failure to resolve? Periodontol 2000. 2020;82:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 93] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 2. | Aminoshariae A, Mackey SA, Palomo L, Kulild JC. Declassifying Mobility Classification. J Endod. 2020;46:1539-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Jin LJ, Cao CF. Clinical diagnosis of trauma from occlusion and its relation with severity of periodontitis. J Clin Periodontol. 1992;19:92-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 62] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Iwata M, Saito A, Kuroda Y, Shinohara T, Tanaka E. Interdisciplinary therapy for severe periodontitis with Angle Class II Division 1 malocclusion: A case report with 7-year follow-up. J Am Dent Assoc. 2019;150:960-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Zimmer B, Seifi-Shirvandeh N. Changes in gingival recession related to orthodontic treatment of traumatic deep bites in adults. J Orofac Orthop. 2007;68:232-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Shulman JD, Peterson J. The association between incisor trauma and occlusal characteristics in individuals 8-50 years of age. Dent Traumatol. 2004;20:67-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Greenstein G, Cavallaro J, Scharf D, Tarnow D. Differential diagnosis and management of flared maxillary anterior teeth. J Am Dent Assoc. 2008;139:715-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Branschofsky M, Beikler T, Schäfer R, Flemming TF, Lang H. Secondary trauma from occlusion and periodontitis. Quintessence Int. 2011;42:515-522. [PubMed] |
| 9. | Fan J, Caton JG. Occlusal trauma and excessive occlusal forces: Narrative review, case definitions, and diagnostic considerations. J Periodontol. 2018;89 Suppl 1:S214-S222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 10. | Graetz C, Dörfer CE, Kahl M, Kocher T, Fawzy El-Sayed K, Wiebe JF, Gomer K, Rühling A. Retention of questionable and hopeless teeth in compliant patients treated for aggressive periodontitis. J Clin Periodontol. 2011;38:707-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Aimetti M, Garbo D, Ercoli E, Grigorie MM, Citterio F, Romano F. Long-Term Prognosis of Severely Compromised Teeth Following Combined Periodontal and Orthodontic Treatment: A Retrospective Study. Int J Periodontics Restorative Dent. 2020;40:95-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Xie Y, Zhao Q, Tan Z, Yang S. Orthodontic treatment in a periodontal patient with pathologic migration of anterior teeth. Am J Orthod Dentofacial Orthop. 2014;145:685-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Morikawa T, Ishii T, Goto H, Motegi E, Nishii Y. A Case of Orthodontic Treatment for Generalized Aggressive Periodontitis. Bull Tokyo Dent Coll. 2021;62:181-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Carvalho CV, Saraiva L, Bauer FPF, Kimura RY, Souto MLS, Bernardo CC, Pannuti CM, Romito GA, Pustiglioni FE. Orthodontic treatment in patients with aggressive periodontitis. Am J Orthod Dentofacial Orthop. 2018;153:550-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Foz AM, Artese HP, Horliana AC, Pannuti CM, Romito GA. Occlusal adjustment associated with periodontal therapy--a systematic review. J Dent. 2012;40:1025-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Graetz C, Ostermann F, Woeste S, Sälzer S, Dörfer CE, Schwendicke F. Long-term survival and maintenance efforts of splinted teeth in periodontitis patients. J Dent. 2019;80:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Konermann A, Al-Malat R, Skupin J, Keilig L, Dirk C, Karanis R, Bourauel C, Jäger A. In vivo determination of tooth mobility after fixed orthodontic appliance therapy with a novel intraoral measurement device. Clin Oral Investig. 2017;21:1283-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Machtei EE, Zubrey Y, Ben Yehuda A, Soskolne WA. Proximal bone loss adjacent to periodontally "hopeless" teeth with and without extraction. J Periodontol. 1989;60:512-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Machtei EE, Hirsch I. Retention of hopeless teeth: the effect on the adjacent proximal bone following periodontal surgery. J Periodontol. 2007;78:2246-2252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Kurem I, Topsakal U, Ozturk T. Evaluation of Multidisciplinary Treatment Relationship between Orthodontics and Periodontology Departments by Examining Inter-Departmental Consultation Notes. Niger J Clin Pract. 2021;24:1234-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Polson AM. Trauma and progression of marginal periodontitis in squirrel monkeys. II. Co-destructive factors of periodontitis and mechanically-produced injury. J Periodontal Res. 1974;9:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 36] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Campiño JI, Ríos CC, Rodriguez-Medina C, Botero JE. Association between traumatic occlusal forces and periodontitis: A systematic review. J Int Acad Periodontol. 2019;21:148-158. [PubMed] |
| 23. | Arita Y, Yoshinaga Y, Kaneko T, Kawahara Y, Nakamura K, Ohgi K, Arita S, Ryu T, Takase M, Sakagami R. Glyburide inhibits the bone resorption induced by traumatic occlusion in rats. J Periodontal Res. 2020;55:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Tsuzuki T, Kajiya H, T-Goto K, Tsutsumi T, Nemoto T, Okabe K, Takahashi Y. Hyperocclusion stimulates the expression of collagen type XII in periodontal ligament. Arch Oral Biol. 2016;66:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 25. | Passanezi E, Sant'Ana ACP. Role of occlusion in periodontal disease. Periodontol 2000. 2019;79:129-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 26. | Gkantidis N, Christou P, Topouzelis N. The orthodontic-periodontic interrelationship in integrated treatment challenges: a systematic review. J Oral Rehabil. 2010;37:377-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 123] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 27. | Artun J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofacial Orthop. 1988;93:143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 93] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Zasčiurinskienė E, Lund H, Lindsten R, Jansson H, Bjerklin K. Outcome of periodontal-orthodontic treatment in subjects with periodontal disease. Part II: a CBCT study of alveolar bone level changes. Eur J Orthod. 2019;41:565-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Re S, Corrente G, Abundo R, Cardaropoli D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int J Periodontics Restorative Dent. 2000;20:31-39. [PubMed] |
| 30. | Feller L, Khammissa RA, Thomadakis G, Fourie J, Lemmer J. Apical External Root Resorption and Repair in Orthodontic Tooth Movement: Biological Events. Biomed Res Int. 2016;2016:4864195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 31. | Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. J Am Dent Assoc. 2008;139:413-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 183] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 32. | Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21:9-19. [PubMed] |
| 33. | Xu M, Sun XY, Xu JG. Periodontally accelerated osteogenic orthodontics with platelet-rich fibrin in an adult patient with periodontal disease: A case report and review of literature. World J Clin Cases. 2021;9:1367-1378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 34. | Re S, Cardaropoli D, Abundo R, Corrente G. Reduction of gingival recession following orthodontic intrusion in periodontally compromised patients. Orthod Craniofac Res. 2004;7:35-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Miethke RR, Brauner K. A Comparison of the periodontal health of patients during treatment with the Invisalign system and with fixed lingual appliances. J Orofac Orthop. 2007;68:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 36. | Lu H, Tang H, Zhou T, Kang N. Assessment of the periodontal health status in patients undergoing orthodontic treatment with fixed appliances and Invisalign system: A meta-analysis. Medicine (Baltimore). 2018;97:e0248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 37. | Kumar N, Jhingta P, Negi KS, Bhardwaj VK, Sharma D, Thakur AS. Combined Periodontal-Orthodontic Treatment of Pathologic Tooth Migration: A Case Study with 10-Year Follow-Up. Contemp Clin Dent. 2018;9:S377-S381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Baghdadi D, Reimann S, Keilig L, Reichert C, Jäger A, Bourauel C. Biomechanical analysis of initial incisor crowding alignment in the periodontally reduced mandible using the finite element method. J Orofac Orthop. 2019;80:184-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |