Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4535
Peer-review started: August 22, 2021
First decision: October 22, 2021
Revised: November 3, 2021
Accepted: March 25, 2022
Article in press: March 25, 2022
Published online: May 16, 2022
Processing time: 263 Days and 16.8 Hours
Regular abdominal massage can be used to treat digestive symptoms such as bloating and constipation and is reported to reduce abdominal discomfort, improve digestive function, and increase the quality of life, without serious adverse effects. Isolated pancreatic injury is rare, and most often occurs during severe trauma such as steering wheel impact injury. To our knowledge, pancreatic injury caused by massage has not yet been reported in the literature.
A 57-year-old woman was referred to our hospital for acute abdominal pain and transient syncope. On examination, she had low hemoglobin concentration and a high white blood cell count and neutrophil percentage. Plain computed tomography of the abdomen revealed a substantial hemorrhage in the abdominal cavity. A large amount of exudate in the pancreatic area was considered a hematoma. Preoperative diagnosis was difficult. Her hemoglobin and blood pressure did not rise even after blood. We suspected progressive bleeding in the abdominal cavity and urgently performed exploratory laparotomy. During the operation, the pancreas was confirmed to be ruptured; hence, spleen-preserving pancreatic body and tail resection were performed. A pancreatic fistula was found on the 15th d after the operation, and the patient was discharged with a drainage tube on the 24th d after active treatment. Subsequently, it was discovered that the patient had undergone a vigorous abdominal massage the day before the abdominal pain began. To our knowledge, this is the first report of isolated pancreatic injury and massive abdominal hemorrhage caused by abdominal massage.
Our findings indicate that any action that increases intra-abdominal pressure may cause internal organ damage. We also review similar cases reported in the literature.
Core Tip: Abdominal massage is considered a reliable treatment method to relieve abdominal distension and constipation, but when asked by doctors about trauma history, it is sometimes ignored. Pancreas rupture is more common in severe steering wheel impact injuries, but it is rarely associated with abdominal massage. Therefore, we must be alert to the increase in intra-abdominal pressure caused by massage, which may further damage the pancreas or other abdominal organs.
- Citation: Sun BL, Zhang LL, Yu WM, Tuo HF. Isolated pancreatic injury caused by abdominal massage: A case report. World J Clin Cases 2022; 10(14): 4535-4540
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4535.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4535
Because of the deep anatomical location of the pancreas, traumatic pancreatic rupture is relatively rare. The pancreas lies adjacent to the stomach, liver, duodenum, small intestine, colon, and other important organs, as well as large blood vessels in the abdominal cavity; therefore, pancreatic injury is typically associated with damage to other organs and blood vessels, with isolated harm to the pancreas accounting for only 14% of all pancreatic injuries[1]. Isolated pancreatic injury most often occurs during severe upper abdominal trauma. There have been no reports of isolated pancreatic injury caused by abdominal massage. In this report, we describe a very rare case of pancreatic injury following abdominal massage, which caused massive abdominal hemorrhage.
A 57-year-old woman had acute abdominal pain for 1 d, which worsened in the last 12 h.
The patient had developed persistent severe upper abdominal pain 1 d previously, which could be relieved by rest. The upper abdominal pain worsened in the last 12 h, accompanied by nausea, vomiting, and transient syncope, prior to her presentation at the emergency center of a tertiary hospital.
She had hypertension and denied a history of surgery and/or trauma.
The personal and family history of patients are unremarkable.
When she arrived at the hospital, she was conscious but unwell and her face was pale. Her body temperature was 35.5 ℃, blood pressure was 13.2/10.2 kPa, heart rate was 105 beats/min, breathing rate was 26 beats/min, and blood oxygen saturation was 99%. There was no ecchymosis in the abdomen, obvious tenderness in the umbilical area and upper abdomen, and no rebound pain or muscle tension. Abdominal percussion was dull, and no bowel sounds were heard.
Preoperative blood test showed that white blood cell count was 11.76 × 109/L, neutrophil percentage was 85.8%, hemoglobin was 77.00 g/L, and the D-dimer quantification was 1.54 mg/L.
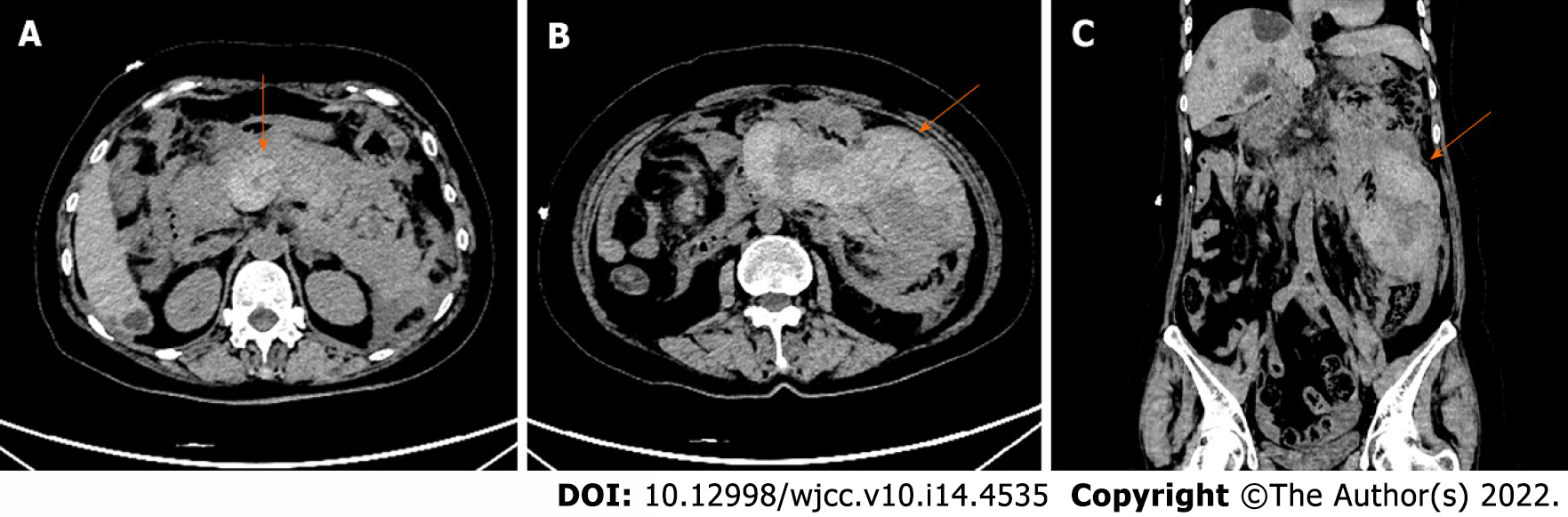
Abdominal computed tomography (CT) showed no abnormalities in the soft tissue and bone structure of the abdominal wall. There was a large amount of fluid in the abdominal cavity, and some of it had a slightly higher density. Multiple round-like density shadows with clear borders could be seen in the liver parenchyma, and the larger ones were about 39 mm in diameter; the intrahepatic bile ducts were not dilated. The pancreas was not clearly displayed, large-scale exudation could be seen in and around the pancreas (Figure 1A), the surrounding fat gap was blurred, and multiple clusters of high- and slightly low-density shadows could be seen around the pancreas, the larger of which was about 8.8 cm × 6.4 cm in size (Figures 1B and 1C). The adjacent peritoneum and bilateral prerenal fascia showed thickening. Pelvic CT showed a small amount of effusion in the pelvic cavity, and there was no obvious abnormality in the uterus and appendages. Chest CT showed mild emphysema in both lungs, and no pleural effusion was seen on either side.
The patient was diagnosed with massive abdominal hemorrhage secondary to pancreatic rupture.
In the emergency center, we quickly established intravenous access and infused 4U O-type red blood cells, 400 mL plasma, and 4U cryoprecipitated clotting factor. Blood pressure was 12.5/9.7 kPa, heart rate was 106 beats/min, and hemoglobin was retested as 63 g/L after transfusion. To determine the cause of the bleeding, we performed exploratory laparotomy. Surgery revealed extensive old hemorrhage in the abdominal cavity, hematoma in the omental sac, retroperitoneal hematoma, injury to the pancreatic body, and hemorrhage from blood vessels on the back of the pancreatic body. After suturing and hemostasis, exploration showed that approximately three quarters of the transverse diameter of the pancreas was damaged, and there were hematomas behind the pancreas, colon, and mesentery root. As the pancreatic injury was too large to be repaired, a pancreatic body and tail resection was performed. The pancreas was transected from the ruptured area, and the proximal end was sutured to arrest the bleeding. We used a disposable endoscopic wire-cutting stapler with a length of a 2.5-mm nail to remove the vessels near the tail of the pancreas and part of the splenic hilum. The lateral width of the distal pancreas tissue was about 4 cm. As the vital signs of the patient were stable during the operation, we retained the spleen. The wound stopped bleeding and two abdominal drainage tubes were properly placed. The operation was completed uneventfully.
After the operation, the patient was transferred to the intensive care unit for treatment. After sedatives were discontinued on the first postoperative day, she gradually became conscious and could complete simple commands. However, her hemodynamics remained unstable, volume expansion was required, and norepinephrine administered via a syringe pump. She gradually recovered after comprehensive treatment, including somatostatin, ulinastatin, antibiotics, blood transfusion, and nutritional support. The patient developed a pancreatic fistula 15 d after the operation, and the abdominal pain was significantly reduced after continuous negative pressure drainage through the spiral negative pressure drainage tube. The drainage fluid gradually reduced from 100 to 20 mL per 24 h by the 21st d after surgery. The abdominal drainage tube placed in the right abdomen was then removed. The patient recovered well after the operation and was discharged on the 24th d after surgery. The patient attended our clinic for reexamination one month after the operation. The abdominal drainage tube on the left abdomen had no drainage in the past 4 d, and the blood-related examinations and amylase were normal. We considered the patient’s pancreatic fistula to be cured, and the abdominal drainage tube was hence pulled out.
When the patient was admitted to the hospital, she denied any history of trauma or surgery, and no evidence of trauma was detected on physical examination. CT could objectively reveal abdominal cavity damage, and the time required for examination is relatively short. Hence, this technique has an important role in routine diagnosis and treatment of acute abdominal pain[2]. Therefore, we chose to conduct a CT examination, which clearly showed the intra-abdominal hemorrhage. There was a large-scale exudation in the pancreatic area, accompanied by a variety of high-density and low-density shadows, considering the possibility of hematoma. There were also multiple cystic lesions in the liver. Because the patient was anemic, we first considered intra-abdominal hemorrhage of unknown etiology or pancreatic disease to exclude abdominal trauma. Sudden severe abdominal pain accompanied by hemorrhagic shock is similar to the symptoms of abdominal aortic aneurysm rupture, and combined with the patient’s history of hypertension, this possibility could not be ruled out[3].
Faced with unexplained abdominal bleeding, it is sometimes difficult to make accurate judgments, and emergency laparotomy can be used to determine the cause and save lives. Exploration of the abdominal cavity revealed old bloody fluid, with hematoma in the lesser omental sac, and paraduodenal hematoma beyond the retroperitoneum, all of which suggested pancreatic injury. Intraoperative exploration confirmed that the pancreas was damaged and bleeding. According to the American Association for Traumatic Surgery pancreatic injury grading standard (Table 1), the patient was confirmed to have grade III injury[4]. According to relevant research instructions, grade I and II injuries should be treated conservatively when the hemodynamics are stable and there are no other abdominal cavity injuries that urgently require surgery; whereas, grade III, IV, and V injuries usually require surgical treatment, with distal pancreatectomy being the first choice for grade III pancreatic injury[5]. As far as possible, distal pancreatectomy aims to ligate the pancreatic duct alone. Stapler suture alone after distal pancreatectomy is a fast and safe suture method, which is not inferior to other suture techniques, and does not increase the possibility of pancreatic fistula or other abdominal complications[6]. For patients with stable hemodynamics, the spleen should be preserved, which can effectively reduce the risk of dangerous infection complications and thromboembolism after surgery[7,8]. Although the patient’s condition was complex and critical, and the slow emergence of the clinical signs of pancreatic injury delayed diagnosis and treatment, fortunately, timely surgical treatment controlled the dangerous abdominal bleeding and saved her life.
| Grade | Injury description |
| I | Minor contusion or superficial laceration without duct injury |
| II | Minor contusion or laceration without duct injury or tissue loss |
| III | Distal transaction or parenchymal injury with duct injury |
| IV | Proximal (right or superior mesenteric artery) transection or parenchymal injury |
In conversation following the operation, the patient told us that she had undergone abdominal massage the day before the abdominal pain occurred. At the time, she felt the massage had been very powerful and painful. On detailed questioning, she had no other injuries. Because the pancreas is a retroperitoneal organ and is protected by the abdominal wall, stomach, and colon, injury is not likely. Pancreatic injury occurs in only 0.2% of patients who endure blunt abdominal injury[9]. Closed pancreatic injuries are most often traffic injuries. The soft pancreas can be squeezed by external forces, such as a steering wheel or bicycle handlebars, and collides with the hard spine behind, causing local pancreatic injury or even rupture. It is not difficult to imagine that any high-intensity external force acting on the abdomen may cause varying degrees of pancreatic damage. Although there is no direct evidence, we consider that abdominal massage caused the pancreatic injury in our patient, based on her medical history. Recent studies have shown[10,11] that abdominal massage can reduce gastric residual volume and the incidence of abdominal distension by mechanically stimulating intestinal movement, as well as increasing the frequency of defecation, with no obvious adverse effects detected. In a previous report, an elderly man was admitted to the hospital with sudden abdominal pain; he had received a vigorous massage the day before its onset and was found to have isolated mesenteric injury during surgery, which had caused severe abdominal hemorrhage[12]. Similar to the pancreas, isolated mesenteric injury after blunt abdominal trauma is also very rare, as external force needs to be directly transmitted to the mesentery to cause it to tear. The medical history of our patient was very similar to this previous report, providing strong evidence that vigorous abdominal massage can be a cause for pancreatic injury. Therefore, deep and powerful abdominal massage should be avoided.
To our knowledge, this is the first case report of a pancreatic rupture caused by abdominal massage. Appropriate abdominal massage is beneficial to relieve abdominal distension and constipation; however, vigorous abdominal massage should be avoided, as it can cause life-threatening damage to the internal organs and tissues of the abdomen.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghannam WM, Egypt; Tenreiro N, Portugal S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Biffl WL, Moore EE, Croce M, Davis JW, Coimbra R, Karmy-Jones R, McIntyre RC Jr, Moore FA, Sperry J, Malhotra A, Feliciano D. Western Trauma Association critical decisions in trauma: management of pancreatic injuries. J Trauma Acute Care Surg. 2013;75:941-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Heiken JP, Katz DS, Menu Y. Emergency Radiology of the Abdomen and Pelvis: Imaging of the Non-traumatic and Traumatic Acute Abdomen. 2018 Mar 21. In: Diseases of the Abdomen and Pelvis 2018-2021: Diagnostic Imaging - IDKD Book [Internet]. Cham (CH): Springer; 2018–. [PubMed] |
| 3. | Barrionuevo P, Malas MB, Nejim B, Haddad A, Morrow A, Ponce O, Hasan B, Seisa M, Chaer R, Murad MH. A systematic review and meta-analysis of the management of visceral artery aneurysms. J Vasc Surg. 2020;72:40S-45S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 4. | Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, Gennarelli TA, McAninch JW, Pachter HL, Shackford SR, Trafton PG. Organ injury scaling, II: Pancreas, duodenum, small bowel, colon, and rectum. J Trauma. 1990;30:1427-1429. [PubMed] |
| 5. | Ho VP, Patel NJ, Bokhari F, Madbak FG, Hambley JE, Yon JR, Robinson BR, Nagy K, Armen SB, Kingsley S, Gupta S, Starr FL, Moore HR 3rd, Oliphant UJ, Haut ER, Como JJ. Management of adult pancreatic injuries: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017;82:185-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 107] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 6. | Peck GL, Blitzer DN, Bulauitan CS, Huntress LA, Truche P, Feliciano DV, Dente CJ. Outcomes after Distal Pancreatectomy for Trauma in the Modern Era. Am Surg. 2016;82:526-532. [PubMed] |
| 7. | Nikfarjam M, Rosen M, Ponsky T. Early management of traumatic pancreatic transection by spleen-preserving laparoscopic distal pancreatectomy. J Pediatr Surg. 2009;44:455-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Pommerening MJ, Rahbar E, Minei K, Holcomb JB, Wade CE, Schreiber MA, Cohen MJ, Underwood SJ, Nelson M, Cotton BA. Splenectomy is associated with hypercoagulable thrombelastography values and increased risk of thromboembolism. Surgery. 2015;158:618-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Iacono C, Zicari M, Conci S, Valdegamberi A, De Angelis M, Pedrazzani C, Ruzzenente A, Guglielmi A. Management of pancreatic trauma: A pancreatic surgeon's point of view. Pancreatology. 2016;16:302-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Dehghan M, Malakoutikhah A, Ghaedi Heidari F, Zakeri MA. The Effect of Abdominal Massage on Gastrointestinal Functions: a Systematic Review. Complement Ther Med. 2020;54:102553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Çetinkaya O, Ovayolu Ö, Ovayolu N. The Effect of Abdominal Massage on Enteral Complications in Geriatric Patients. SAGE Open Nurs. 2020;6:2377960820963772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Mori S, Ai T, Otomo Y. Laceration of the transverse mesocolon in an old man with a habit of abdominal massage for constipation: a case report. Surg Case Rep. 2020;6:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |