Published online May 6, 2022. doi: 10.12998/wjcc.v10.i13.4196
Peer-review started: September 14, 2021
First decision: January 22, 2022
Revised: January 28, 2022
Accepted: March 14, 2022
Article in press: March 14, 2022
Published online: May 6, 2022
Processing time: 227 Days and 16.3 Hours
Primary pulmonary meningioma (PPM) is a rare disease that is usually benign. The most common presentation of PPM is isolated pulmonary nodules or masses, so the disease can mimic any other lung tumor on imaging, especially lung cancer or metastasis.
A 47-year-old asymptomatic woman presented with a well-defined, lobulated pulmonary mass with calcification in the left lower lobe. The mass measured 69 mm × 57 mm × 61 mm and was found during a chest computed tomography (CT) performed for physical examination. Contrast-enhanced CT and positron emission tomography (PET)/CT revealed mild enhancement of the mass, with accumulation of 18-fluoro-2-deoxy-D-glucose (18F-FDG). Transbronchial biopsy suggested a provisional diagnosis of low-grade neuroendocrine tumor. Subse
PPM should be considered in the differential diagnosis of isolated pulmonary masses found incidentally on CT and should be diagnosed based on a combination of radiological and histological features. Surgical resection is currently the main treatment strategy. No recurrence of benign PPMs has been reported after complete resection.
Core Tip: Primary pulmonary meningioma (PPM) is a rare tumour that usually presents as an asymptomatic solitary pulmonary mass. Limited knowledge of the disease can make diagnosis difficult. Here, we present the case of a 47-year-old woman with PPM.
- Citation: Zhang DB, Chen T. Primary pulmonary meningioma: A case report and review of the literature. World J Clin Cases 2022; 10(13): 4196-4206
- URL: https://www.wjgnet.com/2307-8960/full/v10/i13/4196.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i13.4196
Primary ectopic meningiomas are rare tumors that occur in the head, neck, skin, peripheral nerves, bone, retroperitoneum, and lungs. They account for approximately 2% of meningiomas[1,2]. Primary pulmonary meningiomas (PPMs) are rare. Since the first case report in 1982 by Kemnitz et al[3], only 67 cases of PPMs have been reported domestically in the medical literature. Among these cases, only five were malignant meningiomas, and PPMs were more likely to be benign.
PPMs usually appear as isolated pulmonary nodules that are accidentally detected on chest radiographs or computed tomography (CT). Despite advancements in radiological examination such as enhanced CT and positron emission tomography (PET), it remains difficult to assess indeterminate isolated pulmonary nodules or masses, and many benign PPMs are misdiagnosed. The present paper reports a rare case of PPM. We also summarized the clinical imaging characteristics of PPMs in the literature to provide a reference for PPM diagnosis.
A 47-year-old woman had a pulmonary mass on physical examination 1 mo ago.
The patient was hospitalized due to chest CT findings of a pulmonary mass in the left lower lobe of the lung upon physical examination 1 mo prior.
The patient had a free previous medical history.
The patient had no personal and family history.
Physical examination revealed no obvious positive signs.
All tumor marker results were within the normal range.
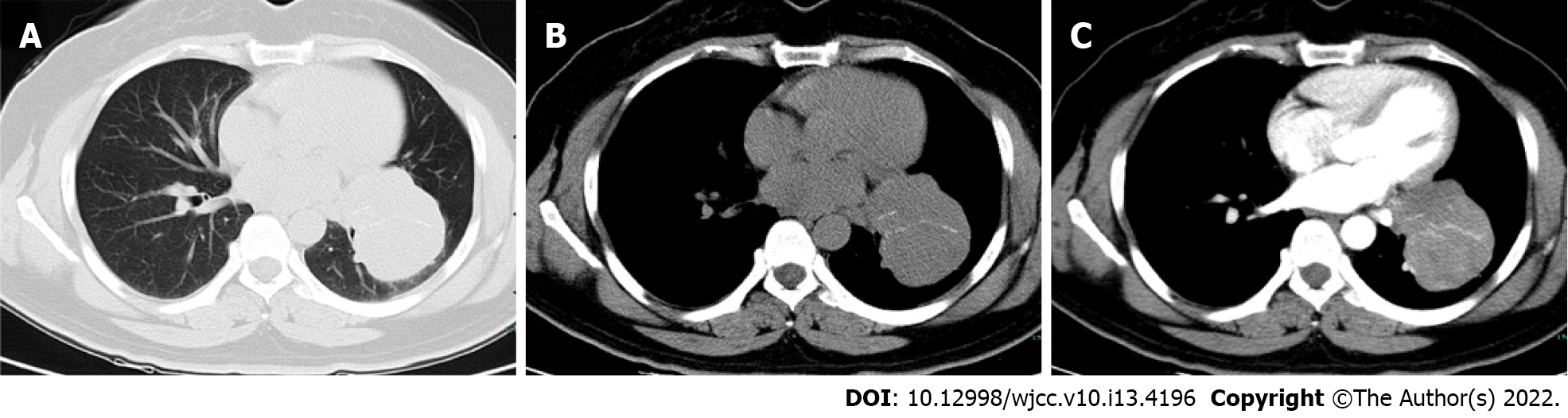
Contrast-enhanced chest CT revealed a 6.9 cm diameter mass with a well-circumscribed margin in the left lower lobe of the lung. The adjacent left lower lobar bronchus and lingual segment of the left upper lobar bronchus were compressed by the mass. The lesion was confined to the lung parenchyma and showed striated calcification. After contrast enhancement, the mass showed mild homogeneous enhancement, from a pre-contrast attenuation of 40 HU to a postcontrast attenuation of 60 HU (Figure 1).
On 18-fluoro-2-deoxy-D-glucose (FDG) PET imaging, the standardized uptake value (SUV) of the mass increased unevenly, with a maximum value of 4.4, which suggested malignant lesion (Figure 2). No other lesions were detected on PET/CT. Moreover, enhanced magnetic resonance imaging (MRI) of the brain showed no evidence of intracranial tumors or metastases. Bronchoscopy revealed partial obstruction of the lower left lobe by the mass and narrowing of the lingual opening in the upper left lobe. A subsequent transbronchial biopsy result suggested a low-grade neuroendocrine tumor (Figure 3).
The final diagnosis of the presented case was PPM.
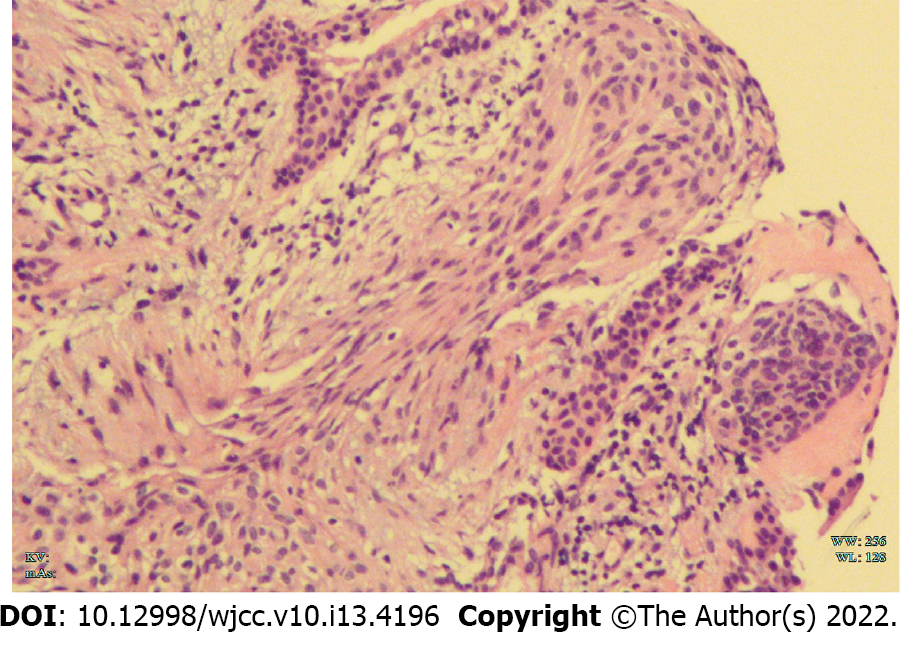
Considering the CT and PET features of the mass and the results of transbronchial biopsy, an open cuff resection of the left lower lobe and wedge resection of the lingual segment were performed. Gross examination revealed a 6.5 cm, off-white, tenacious texture mass. Microscopic examination revealed a tumor with focal bronchial cartilage involvement, no pleural involvement, and fusiform nests of cells arranged in fascicles or whorls. Immunohistochemistry showed positivity for epithelial membrane antigen (EMA), progesterone receptor (PR), somatostatin receptor 2 (SSTR2), D2-40, and CD34, and negativity for S-100, cytokeratin (CK), glial fibrillary acidic protein, CgA, SOX10, and SMA; the Ki-67 index was about 5%-10% positive (Figure 4). These morphological and immunohistochemical features were suggestive of a PPM. Preoperative contrast-enhanced chest CT, contrast-enhanced brain MRI, and PET-CT did not reveal evidence of intracranial or spinal meningioma.
The patient was disease-free after 3 mo of follow-up.
A total of 68 patients diagnosed with PPM were reported in the English literature from 1982 to 2021. All of these patients received histological assessment confirming PPM. Eighteen cases were excluded because (1) They underwent no radiological examination; or (2) They received no radiological evaluation of the CNS negative for meningioma. Ultimately, 50 patients (including the case reported above) were included in the analysis.
The study group comprised 50 patients: 19 men and 31 women. The age range was 18–108 years (median age: 58.0 years). Thirty-five patients were asymptomatic and only occasionally showed pulmonary nodules or masses on chest CT or X-ray. Thirteen patients had respiratory symptoms, including chest pain, chest tightness, hemoptysis, cough, and sputum). In addition, two patients had non-specific symptoms[3,4]. There were nine patients with a history of malignancy: two had suffered lung adenocarcinoma[5,6], two colorectal cancer[7,8], two breast cancer[9,10], one buccal cancer[11], one papillary thyroid carcinoma[12], and one thymoma and kidney cancer[13] (Table 1)[14-47].
| No. | Ref. | Age (Gender) | Symptom | Size (cm) | Histology | Follow-up |
| 1 | Kemnitz et al[3] | 59 (F) | Weakness, loss ofappetite, weight loss | 4.0 | B | 30 |
| 2 | Chumas et al[14] | 58 (F) | None | 4.0 | B | 12 |
| 3 | Zhang et al[15] | 58 (F) | None | 2.5 | B | 18 |
| 4 | Kodama et al[16] | 53 (M) | None | 2.6 | B | 84 |
| 5 | Drlicek et al[17] | 41 (M) | None | 2.5 | B | 72 |
| 6 | 62 (F) | None | 6.0 | B | 72 | |
| 7 | Flynn et al[18] | 63 (F) | Coughing | 3.0 | B | 44 |
| 8 | 74 (F) | None | 1.7 | B | 37 | |
| 9 | Maiorana et al[19] | 68 (M) | None | 1.8 | B | 24 |
| 10 | Kaleem et al[20] | 45 (F) | None | 1.2 | B | 10 |
| 11 | Lockett et al[21] | 65 (M) | None | 0.8 | B | 5 |
| 12 | Ueno et al[22] | 61 (F) | None | 0.4-1.5 | B | 36 |
| 13 | de Perrot et al[5] | 57 (F) | None | 0.9 | B | 30 |
| 14 | Prayson et al[23] | 51 (M) | None | 6.5 | M | 10 |
| 15 | Spinelli et al[24] | 71 (F) | Bronchitis | 1.5 | B | 96 |
| 16 | Falleni et al[7] | 59 (M) | None | 2.5 | B | 30 |
| 17 | Cesario et al[25] | 56 (M) | None | 2.0 | B | 72 |
| 18 | CURA et al[26] | 58 (F) | None | 2.0 | B | N |
| 19 | Comin et al[27] | 33 (M) | Hemoptysis and thoracic pain | 2.0 | B | 47 |
| 20 | Rowsell et al[28] | 51 (M) | None | 4.0 | B | 8 |
| 21 | Picquet et al[9] | 54 (F) | None | 1.4 | B | 6 |
| 22 | Kaneda et al[29] | 59 (F) | None | 1.4 | B | 14 |
| 23 | van der Meij et al[30] | 40 (F) | Dyspnea, coughing dysphagia | 5.0 | M | 40 |
| 24 | Meirelles et al[31] | 48 (M) | None | 1.5 | B | N |
| 25 | Incarbone et al[32] | 24 (M) | Hemoptysis | 2.4 | B | 42 |
| 26 | Izumi et al[33] | 18 (F) | Hemoptysis on exertion | 3.3 | B | 15 |
| 27 | Weber et al[4] | 108 (F) | Asthenia, lack of appetite, loss of weight and anxiety | 15.0 | M | N |
| 28 | Lepanto et al[10] | 60 (F) | None | 1.6 | B | 12 |
| 29 | Kim et al[34] | 61 (F) | Chest pain | 2.5 | B | 84 |
| 30 | Jiang et al[35] | 63 (F) | None | 3.5 | B | N |
| 31 | Juan et al[11] | 55 (M) | None | 4.5 | B | 6 |
| 32 | Oide et al[36] | 44 (M) | None | 2.0 | B | N |
| 33 | Huang et al[37] | 44 (F) | Chest pain | 2.5 | B | 6 |
| 34 | Žulpaitė et al[38] | 43 (F) | None | 4.5 | M | 24 |
| 35 | Hong et al[39] | 54 (M) | Cough and sputum | 1.6 | B | 24 |
| 36 | Luo et al[40] | 65 (F) | Cough | 3.5 | B | N |
| 37 | Xu et al[41] | 65 (F) | Chest pain and tightness | 0.7 | B | N |
| 38 | Ohashi et al[42] | 60 (F) | None | 2.0 | B | 36 |
| 39 | Bae et al[43] | 43 (F) | None | 1.9 | B | 26 |
| 40 | Cimini et al[13] | 80 (M) | None | 1.4 | B | N |
| 41 | 80 (M) | None | 1.2 | M | N | |
| 42 | Wang et al[44] | 64 (F) | None | 3.4 (cystic nodules 0.8-2) | B | N |
| 43 | Fujikawa et al[12] | 62 (F) | None | 0.8 | B | 20 |
| 45 | Han et al[6] | 64 (F) | None | 0.6 | B | 28 |
| 44 | 75 (F) | None | 0.6 | B | 2 | |
| 46 | Gürçay et al[45] | 55 (F) | Cough | 2.0 | B | N |
| 47 | Jiang et al[8] | 70 (M) | None | 1.5 | B | N |
| 48 | Bas et al[46] | 57 (M) | Cough | 1.0 | B | N |
| 49 | Oh et al[47] | 54 (M) | None | 0.5-1.3 | B | 24 |
| 50 | Present report | 46 (F) | None | 6.9 | B | 3 |
Most PPMs were benign, and only five cases were malignant[4,13,23,30,38]. Benign PPMs were generally well-circumscribed on radiological studies, with diameters ranging from 0.4 to 6 cm (median: 2 cm). The five malignant PPMs ranged in diameter from 1.5 to 15 cm (median: 6.4 cm). On chest CT scan, benign PPMs usually appear as isolated, rounded, solid, well-defined nodules or masses, with or without lobulation. Five cases were lobulated[24,31,32,37,40], two manifested as ground glass density[11,45], and two showed burrs on the edges[6]. In addition, one recent study reported that the PPM showed multiple cystic lesions with a solid component[44]. The CT features of the lesions were not described in the remaining eight cases (Table 2)[14-47].
| No. | Ref. | Location | CT feature | Enhancement feature | PET/CT |
| 1 | Kemnitz et al[3] | RL-P | Well-circumscribed | N | N |
| 2 | Chumas et al[14] | RL-P | Well-circumscribed | N | N |
| 3 | Zhang et al[15] | LU-P | Well-circumscribed | N | N |
| 4 | Kodama et al[16] | LU-P | N | N | N |
| 5 | Drlicek et al[17] | LL-N | Well-circumscribed | N | N |
| 6 | LL-N | N | N | N | |
| 7 | Flynn et al[18] | LU-C | Well-circumscribed | N | N |
| 8 | LL-P | Well-circumscribed | N | N | |
| 9 | Maiorana et al[19] | N-P | Well-circumscribed | N | N |
| 10 | Kaleem et al[20] | LL-P | Well-circumscribed | N | N |
| 11 | Lockett et al[21] | LL-P | Well-circumscribed | N | N |
| 12 | Ueno et al[22] | Bil-N | N | N | N |
| 13 | de Perrot et al[5] | RL-P | Well-circumscribed | N | N |
| 14 | Prayson et al[23] | RU-P | Smooth margins and focal necrosis | N | N |
| 15 | Spinelli et al[24] | N-P | Lobulated margins | N | N |
| 16 | Falleni et al[7] | LU-P | Well-circumscribed | N | N |
| 17 | Cesario et al[25] | LU-P | Well-circumscribed | N | N |
| 18 | CURA et al[26] | RU-C | Well-circumscribed | Enhancement | High uptake (no value) |
| 19 | Comin et al[27] | LU-P | N | N | N |
| 20 | Rowsell et al[28] | RL-C | N | N | N |
| 21 | Picquet et al[9] | LL-P | Well-circumscribed | N | N |
| 22 | Kaneda et al[29] | N-P | Well-circumscribed | N | N |
| 23 | van der Meij et al[30] | RH-C | N | N | N |
| 24 | Meirelles et al[31] | RL-C | Lobulated margins | N | High uptake (12.9) |
| 25 | Incarbone et al[32] | RU-P | Lobulated margins | N | High uptake (10.14) |
| 26 | Izumi et al[33] | LU-C | Well-circumscribed | N | N |
| 27 | Weber et al[4] | RL-C | N | N | N |
| 28 | Lepanto et al[10] | LL-P | N | N | Low uptake (1.2) |
| 29 | Kim et al[34] | RU-P | Well-circumscribed | Homogeneous enhancement enhancement | N |
| 30 | Jiang et al[35] | LU-P | Well-circumscribed | N | N |
| 31 | Juan et al[11] | LU-P | Ground-glass opacity | N | N |
| 32 | Oide et al[36] | LU-P | Well-circumscribed | N | N |
| 33 | Huang et al[37] | RL-P | Calcifications, mild peripheral lobulation | Mild enhancement | N |
| 34 | Žulpaitė et al[38] | LU-P | N | Homogeneous enhancement | N |
| 35 | Hong et al[39] | LU-P | Well-circumscribed | Heterogeneous enhancement | N |
| 36 | Luo et al[40] | RL-P | Heterogeneous lobulated | N | N |
| 37 | Xu et al[41] | RL-P | Well-circumscribed | N | N |
| 38 | Ohashi et al[42] | RL-P | N | N | N |
| 39 | Bae et al[43] | RL-C | Oval-shaped | Well-enhancement | Mildly high uptake (2.48) |
| 40 | Cimini et al[13] | RU-P | N | No significant enhancement | High uptake (4.63) |
| 41 | LU-N | N | Enhancement | Mildly high uptake (2.46) | |
| 42 | Wang et al[44] | RL-N | Multiple thin-, smooth-walled cysts or cystic nodules with solid component | Mild enhancement | N |
| 43 | Fujikawa et al[12] | LL-P | Well-circumscribed | N | N |
| 45 | Han et al[6] | RL-P | Burrs on the edges | N | N |
| 44 | RL-P | Burrs on the edges | N | N | |
| 46 | Gürçay et al[45] | RU-P | Peripheral ground-glass | N | Low uptake (1.89) |
| 47 | Jiang et al[8] | RL-P | Well-circumscribed | Mild centripetal enhancement | Low uptake (0.6) |
| 48 | Bas et al[46] | LL-P | Well-circumscribed | N | Low uptake (no value) |
| 49 | Oh et al[47] | scattered | Well-circumscribed | N | Mildly high uptake (3.1) |
| 50 | Present report | LL-C | Well-circumscribed | Mild homogeneous enhancement | High uptake (4.4) |
The CT enhancement patterns were described in 11 patients: six cases showed homogeneous enhancement, one showed heterogeneous enhancement[39], two showed mild enhancement[37,44], one showed mild concentric enhancement[8], and one showed no significant enhancement[13].
18F-fluorodeoxyglucose-PET was performed in 12 patients, including our reported case. The PET scans of four patients showed no accumulation of 18F-FDG in lung lesions[8,10,45,46]. Seven patients showed metabolically active lesions suspicious for malignancy, with a reported SUV range from 2.46 to 12.9 in seven cases. No other extra-pulmonary sites with increased FDG uptake were detected in any of the patients.
The prognosis of benign PPM resection is good, with almost no recurrence or metastasis. Follow-up was reported in 35 benign cases, ranging from 2 to 96 mo (median: 24 mo). However, two malignant PPMs relapsed[23,30]. The above summary is presented in Table 3.
| Variables | Number | Ratio (%) | |
| Gender (n = 50) | Female | 31 | 62.0 |
| Male | 19 | 38.0 | |
| Age (n = 50) | ≤ 40 yr | 4 | 8.0 |
| 40–60 yr | 26 | 52.0 | |
| ≥ 60 yr | 20 | 40.0 | |
| Symptoms (n = 50) | No | 35 | 70.0 |
| Yes | 15 | 30.0 | |
| Size (n = 50) | ≤ 3 cm | 37 | 74.0 |
| > 3 cm | 13 | 26.0 | |
| Histology (n = 50) | Benign | 45 | 90.0 |
| Malignant | 5 | 10.0 | |
| Site (n = 47) | RL | 15 | 31.9 |
| RU | 6 | 12.8 | |
| LL | 10 | 21.3 | |
| LU | 13 | 27.7 | |
| Other | 3 | 6.4 | |
| Location (n = 45) | Peripheral | 36 | 80.0 |
| Centrilobar | 9 | 20.0 | |
| Main CT features (n = 38) | Well-circumscribed | 27 | 71.1 |
| Lobulated | 5 | 13.2 | |
| Burrs | 2 | 5.3 | |
| Ground-glass density | 2 | 5.3 | |
| Calcification | 2 | 5.3 | |
| PET/CT (n = 12) | High uptake | 8 | 66.7 |
| Low uptake | 4 | 33.3 |
Primary ectopic pulmonary meningiomas are very rare, and only 67 cases (including our report) of PPM have been reported in the English language medical literature. The present study reported a case with very complete clinical procedure and imaging data, including preoperative enhanced CT examination, PET-CT examination, bronchoscopy biopsy, and postoperative pathological results. There were rare signs of calcification on CT, false positives on PET-CT and errors in our biopsy results. This suggests that we need to be cautious when excluding PPM only through auxiliary examination or even needle biopsy in clinical work.
The pathogenesis of PPMs remains unclear. One hypothesis is that the tumors develop from multipotent mesenchymal cells. Another states that PPMs originate from minute pulmonary meningothelial nodules that are occasionally found in approximately 1% of autopsies and excised lung specimens[48]. However, the incidence of meningiomas is much lower than that of meningeal epithelial nodules. Moreover, previous genotypic comparisons have failed to demonstrate pulmonary meningeal epithelial nodules or intracranial meningiomas, further supporting the hypothesis[49].
To date, approximately 90% of PPMs reported in the literature have been benign, while five have been malignant[4,13,23,30,38]. Most patients with PPM have no obvious symptoms, while some have respiratory or non-specific symptoms. Clinical symptoms may be related to the lesion location. As previously reported, benign PPMs are usually located in the peripheral pulmonary region, with no involvement of the bronchi, blood vessels, or pleura. Some PPM patients have a known history of malignancy[8], so a comprehensive and careful evaluation of pulmonary lesions must be carried out to avoid the misdiagnosis of metastasis.
Radiologically, PPMs usually appear as isolated, solid, and well-defined parenchymal coin-like lesions, ranging in size from 0.4 to 6.5 cm. Approximately 74.0% of PPMs are less than 3 cm in diameter. The lesions may present with burrs, lobulation, ground-glass density, or calcification, but these features are uncommon. Furthermore, one study reported a PPM presenting as multiple cystic lesions[44]. PPMs have diverse enhancement CT manifestations. They usually show different degrees of enhancement, or even no significant enhancement. Hence, the pattern of lesion enhancement may not help to determine whether the lesion is benign or malignant. On 18F-FDG PET, most PPMs exhibit high or mildly high metabolic activity, as in in our reported case. Only four PPMs showed low uptake of 18F-FDG[8,10,45,46]. However, one recent study reported a patient with both benign and malignant PPMs, both characterized by increased glucose uptake[13]. This suggests that the malignancy of PPMs may not be related to 18F-FDG uptake.
Pathological identification is necessary to allow PPM diagnosis; however, diagnosis can sometimes be difficult using needle biopsy alone[32]. False positives are sometimes reported, in addition to negative reports. For instance, in the case reported by Žulpaitė et al[38], a false positive diagnosis of paraganglioma was given based on preoperative transthoracic needle biopsy. The present patient was misdiagnosed as having low-grade neuroendocrine tumor based on preoperative bronchoscopic biopsy.
In conclusion, the accurate diagnosis of PPM is challenging because the tumors are rare and show variable radiological manifestations. A single 18F FDG PET or contrast-enhanced CT examination may not be sufficient to evaluate patients with PPM. Surgical resection is the main treatment strategy, and no relapse has been reported in benign cases after complete resection. In clinical practice, attention should be paid to common isolated pulmonary nodule or mass, especially in asymptomatic patients. PPM should be considered in the differential diagnosis of lung diseases.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Soriano-Ursúa MA, Mexico; Sultana N, Bangladesh S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Kershisnik M, Callender DL, Batsakis JG. Extracranial, extraspinal meningiomas of the head and neck. Ann Otol Rhinol Laryngol. 1993;102:967-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Muzumdar DP, Vengsarkar US, Bhatjiwale MG, Goel A. Diffuse calvarial meningioma: a case report. J Postgrad Med. 2001;47:116-118. [PubMed] |
| 3. | Kemnitz P, Spormann H, Heinrich P. Meningioma of lung: first report with light and electron microscopic findings. Ultrastruct Pathol. 1982;3:359-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Weber C, Pautex S, Zulian GB, Pusztaszeri M, Lobrinus JA. Primary pulmonary malignant meningioma with lymph node and liver metastasis in a centenary woman, an autopsy case. Virchows Arch. 2013;462:481-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | de Perrot M, Kurt AM, Robert J, Spiliopoulos A. Primary pulmonary meningioma presenting as lung metastasis. Scand Cardiovasc J. 1999;33:121-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Han D, Deng H, Liu Y. Primary pulmonary meningiomas: report of two cases and review of the literature. Pathol Res Pract. 2020;216:153232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Falleni M, Roz E, Dessy E, Del Curto B, Braidotti P, Gianelli U, Pietra GG. Primary intrathoracic meningioma: histopathological, immunohistochemical and ultrastructural study of two cases. Virchows Arch. 2001;439:196-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Jiang M, Chen P, Huang R, Zhang J, Zheng J. A case report of primary pulmonary meningioma masquerading as lung metastasis in a patient with rectal carcinoma: role of 18F-FDG PET/CT. J Cardiothorac Surg. 2021;16:153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Picquet J, Valo I, Jousset Y, Enon B. Primary pulmonary meningioma first suspected of being a lung metastasis. Ann Thorac Surg. 2005;79:1407-1409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Lepanto D, Maffini F, Petrella F, Colandrea M, Putzu C, Barberis M, Paganelli G, Viale G. Atypical primary pulmonary meningioma: a report of a case suspected of being a lung metastasis. Ecancermedicalscience. 2014;8:414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Juan CM, Chen ML, Ho SY, Huang YC. Primary Pulmonary Meningioma Simulating a Pulmonary Metastasis. Case Rep Pulmonol. 2016;2016:8248749. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Fujikawa R, Arai Y, Otsuki Y, Nakamura T. A case of a primary pulmonary meningioma mimicking a metastasis from a papillary thyroid carcinoma due to a size reduction after radioactive iodine therapy. Surg Case Rep. 2020;6:57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Cimini A, Ricci F, Pugliese L, Chiaravalloti A, Schillaci O, Floris R. A Patient with a Benign and a Malignant Primary Pulmonary Meningioma: An Evaluation with 18F Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography and Computed Tomography with Iodinated Contrast. Indian J Nucl Med. 2019;34:45-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Chumas JC, Lorelle CA. Pulmonary meningioma. A light- and electron-microscopic study. Am J Surg Pathol. 1982;6:795-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Zhang FL, Cheng XR, Zhang YS, Ding JA. Lung ectopic meningioma. A case report. Chin Med J (Engl). 1983;96:309-311. [PubMed] |
| 16. | Kodama K, Doi O, Higashiyama M, Horai T, Tateishi R, Nakagawa H. Primary and metastatic pulmonary meningioma. Cancer. 1991;67:1412-1417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Drlicek M, Grisold W, Lorber J, Hackl H, Wuketich S, Jellinger K. Pulmonary meningioma. Immunohistochemical and ultrastructural features. Am J Surg Pathol. 1991;15:455-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Flynn SD, Yousem SA. Pulmonary meningiomas: a report of two cases. Hum Pathol. 1991;22:469-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Maiorana A, Ficarra G, Fano RA, Spagna G. Primary solitary meningioma of the lung. Pathologica. 1996;88:457-462. [PubMed] |
| 20. | Kaleem Z, Fitzpatrick MM, Ritter JH. Primary pulmonary meningioma. Report of a case and review of the literature. Arch Pathol Lab Med. 1997;121:631-636. [PubMed] |
| 21. | Lockett L, Chiang V, Scully N. Primary pulmonary meningioma: report of a case and review of the literature. Am J Surg Pathol. 1997;21:453-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Ueno M, Fujiyama J, Yamazaki I, Uchiyama T, Ishikawa Y, Satoh Y. Cytology of primary pulmonary meningioma. Report of the first multiple case. Acta Cytol. 1998;42:1424-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Prayson RA, Farver CF. Primary pulmonary malignant meningioma. Am J Surg Pathol. 1999;23:722-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Spinelli M, Claren R, Colombi R, Sironi M. Primary pulmonary meningioma may arise from meningothelial-like nodules. Adv Clin Path. 2000;4:35-39. [PubMed] |
| 25. | Cesario A, Galetta D, Margaritora S, Granone P. Unsuspected primary pulmonary meningioma. Eur J Cardiothorac Surg. 2002;21:553-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Cura M, Smoak W, Dala R. Pulmonary meningioma: false-positive positron emission tomography for malignant pulmonary nodules. Clin Nucl Med. 2002;27:701-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Comin CE, Caldarella A, Novelli L, Janni A. Primary pulmonary meningioma: report of a case and review of the literature. Tumori. 2003;89:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Rowsell C, Sirbovan J, Rosenblum MK, Perez-Ordoñez B. Primary chordoid meningioma of lung. Virchows Arch. 2005;446:333-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Kaneda Y, Miyoshi T, Hiratsuka M, Yamamoto S, Kato F, Maki K, Hayashi H, Shiraishi T, Iwasaki A, Iwasaki H, Nabeshima K, Shirakusa T. [Primary pulmonary meningioma; report of a case]. Kyobu Geka. 2005;58:512-515. [PubMed] |
| 30. | van der Meij JJ, Boomars KA, van den Bosch JM, van Boven WJ, de Bruin PC, Seldenrijk CA. Primary pulmonary malignant meningioma. Ann Thorac Surg. 2005;80:1523-1525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Meirelles GS, Ravizzini G, Moreira AL, Akhurst T. Primary pulmonary meningioma manifesting as a solitary pulmonary nodule with a false-positive PET scan. J Thorac Imaging. 2006;21:225-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Incarbone M, Ceresoli GL, Di Tommaso L, Cappuzzo F, Inzirillo F, Infante M, Alloisio M. Primary pulmonary meningioma: report of a case and review of the literature. Lung Cancer. 2008;62:401-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 33. | Izumi N, Nishiyama N, Iwata T, Nagano K, Tsukioka T, Hanada S, Suehiro S. Primary pulmonary meningioma presenting with hemoptysis on exertion. Ann Thorac Surg. 2009;88:647-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Kim YY, Hong YK, Kie JH, Ryu SJ. Primary pulmonary meningioma: an unusual cause of a nodule with strong and homogeneous enhancement. Clin Imaging. 2016;40:170-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 35. | Jiang GY, Zhang Y, Yu JH, Lin XY, Fan CF, Sun CL, Xu HT, Wang EH. Primary pulmonary meningioma: a case report and a review of the literature. J Clin Exp Pathol. 2016;9:4467-4472. |
| 36. | Oide T, Hiroshima K, Shibuya K, Nakatani Y. Primary Pulmonary Meningioma Presenting as a Coin Lesion. Intern Med. 2017;56:2073-2074. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Huang S, Chen L, Mao Y, Tong H. Primary pulmonary meningioma: A case report. Medicine (Baltimore). 2017;96:e6474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Žulpaitė R, Jagelavičius Ž, Mickys U, Janilionis R. Primary Pulmonary Meningioma With Rhabdoid Features. Int J Surg Pathol. 2019;27:457-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 39. | Hong S, Jiang J, Zhou F, Liu J. Computed tomography findings of primary pulmonary meningioma: A case report. Medicine (Baltimore). 2018;97:e9651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Luo JZ, Zhan C, Ni X, Shi Y, Wang Q. Primary pulmonary meningioma mimicking lung metastatic tumor: a case report. J Cardiothorac Surg. 2018;13:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 41. | Xu KK, Tian F, Cui Y. Primary pulmonary meningioma presenting as a micro solid nodule: A rare case report. Thorac Cancer. 2018;9:874-876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 42. | Ohashi-Nakatani K, Shibuki Y, Fujima M, Watanabe R, Yoshida A, Yoshida H, Matsumoto Y, Tsuchida T, Watanabe SI, Motoi N. Primary pulmonary meningioma: A rare case report of aspiration cytological features and immunohistochemical assessment. Diagn Cytopathol. 2019;47:330-333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 43. | Bae SY, Kim HS, Jang HJ, Chung WS, Kim H, Kim YH, Lee JH, Bang SS. Primary Pulmonary Chordoid Meningioma. Korean J Thorac Cardiovasc Surg. 2018;51:410-414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 44. | Wang X, Li P, Zhou P, Fu Y, Lai Y, Che G. Intrapulmonary metastasis from primary pulmonary meningioma presenting as multiple cystic lesions: a case report. BMC Pulm Med. 2019;19:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 45. | Gürçay N, Öztürk A, Demirağ F, İncekara F. Primary pulmonary meningioma mimicking pulmonary metastasis: A rare case report. Turk Gogus Kalp Damar Cerrahisi Derg. 2020;28:699-701. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 46. | Bas A, Valiyev E, Ozkan ND, Tombul I, Yonat S, Sayan M, Kurul IC. A Rare Entity: Primary Pulmonary Meningioma. Turk Patoloji Derg. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | Oh JH, Cho HS, Hwang HS, Ji W. Primary pulmonary meningioma presenting as multiple lung nodules: A case report. Thorac Cancer. 2022;13:141-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 48. | Gaffey MJ, Mills SE, Askin FB. Minute pulmonary meningothelial-like nodules. A clinicopathologic study of so-called minute pulmonary chemodectoma. Am J Surg Pathol. 1988;12:167-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 68] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 49. | Ionescu DN, Sasatomi E, Aldeeb D, Omalu BI, Finkelstein SD, Swalsky PA, Yousem SA. Pulmonary meningothelial-like nodules: a genotypic comparison with meningiomas. Am J Surg Pathol. 2004;28:207-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |