Published online Apr 16, 2022. doi: 10.12998/wjcc.v10.i11.3533
Peer-review started: September 18, 2021
First decision: December 10, 2021
Revised: December 18, 2021
Accepted: February 27, 2022
Article in press: February 27, 2022
Published online: April 16, 2022
Processing time: 202 Days and 10.9 Hours
Andersson lesion (AL) is an uncommon complication in ankylosing spondylitis (AS), which is characterized by nonneoplastic bone destruction and often appears as bone destruction and sclerosis in the vertebral body and/or the area involving the intervertebral disc. According to the literature, Andersson lesion commonly occur in the thoracic and lumbar spine and rarely in the cervical spine.
This case involved a 78-year-old man with a long history of AS who developed AL in the cervical spine (C5/6 and C6/7). One-stage anterior-posterior approach surgery was successfully performed. At the 6-month follow-up, the pain was significantly reduced, and the limb function was gradually improved.
AL uncharacteristically appears in the cervical spine and tends to be misdiagnosed as vertebral metastases or spinal tuberculosis. Posterior combined with anterior surgery achieves solid biological stabilization in the treatment of AL bone destruction.
Core Tip: This case involved an Andersson lesion in the cervical spine that occurred in an ankylosing spondylitis patient and was very rare. The Andersson lesion was diagnosed based on orthopaedist clinical experience, imaging examinations and final pathology results. This case report provides a reference for the clinical diagnosis of such cases.
- Citation: Peng YJ, Zhou Z, Wang QL, Liu XF, Yan J. Ankylosing spondylitis complicated with andersson lesion in the lower cervical spine: A case report. World J Clin Cases 2022; 10(11): 3533-3540
- URL: https://www.wjgnet.com/2307-8960/full/v10/i11/3533.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i11.3533
Andersson lesion (AL) are characterized by nonneoplastic bone destruction, which is an uncommon phenomenon in late-stage ankylosing spondylitis (AS) and often appears as erosive focal changes with sclerosis widely distributed in the region of the vertebral end plate[1,2]. The prevalence of AL-complicating AS ranges from 1.5% to > 28%[3,4]. With the development of AL, these pathological and destructive changes of the spine may lead to progressive, localized and pain-intolerable kyphosis deformities and even neurological defects, which must be treated in severe cases[5,6]. AS is a chronic active nonunion state with unstable posterior column fractures or unfused facet joints associated with vertebral lesion[7]. Since nonspecific inflammation is the main pathological manifestation, Andersson lesion commonly occur in the region of the thoracic and lumbar spine but rarely in the cervical spine[8]. We successfully treated a patient with nonneoplastic and noninfectious bone destruction of the C6 vertebral body, who had a history of ankylosing spondylitis for decades, which resulted in nonunion involving the middle and posterior columns, characteristics of an Andersson lesion. To the best of our knowledge, this is the first report of unstable fractures of AS with C6 aggressive bone destruction and accumulation of three columns of the cervical spine.
A 78-year-old male farmer was admitted to our hospital with neck pain, worsened numbness and increased disability due to an accidental fall a month prior. He had neck pain and a limited range of motions, but he had no symptoms of fever, night sweats or increased nocturnal pain.
This patient had a history of AS and mobility impairments for decades. He had progressive symptoms of neck pain for 3 mo complicated with left upper limb pain and numbness without obvious cause.
He had no history of diabetes, tuberculosis or tumour. He had undergone thoracolumbar fracture surgery more than ten years ago.
The patient denied family history.
Physical examination revealed a restricted cervical range of motion. The muscle power of the left upper limbs was grade IV with slightly decreased sensation. The Hoffman signs of both upper limbs were negative, and bilateral Babinski signs were negative in the lower extremities.
Routine blood analysis revealed a slight increase in the neutrophil ratio (77.4%) with normal haematocrit and leukocyte counts. Prothrombin and partial thromboplastin times were almost normal, and d-dimers were increased at 1.56 μg/mL. Serum C-reactive protein was increased at 55.6 mg/dL (normal range < 10 mg/dL). The blood serum tumour marker analysis showed that ferroprotein increased at 516 ng/mL (normal range 30-400 ng/mL), and prostate-specific antigen marginally increased to 8.53 ng/mL (normal range < 4 ng/mL).
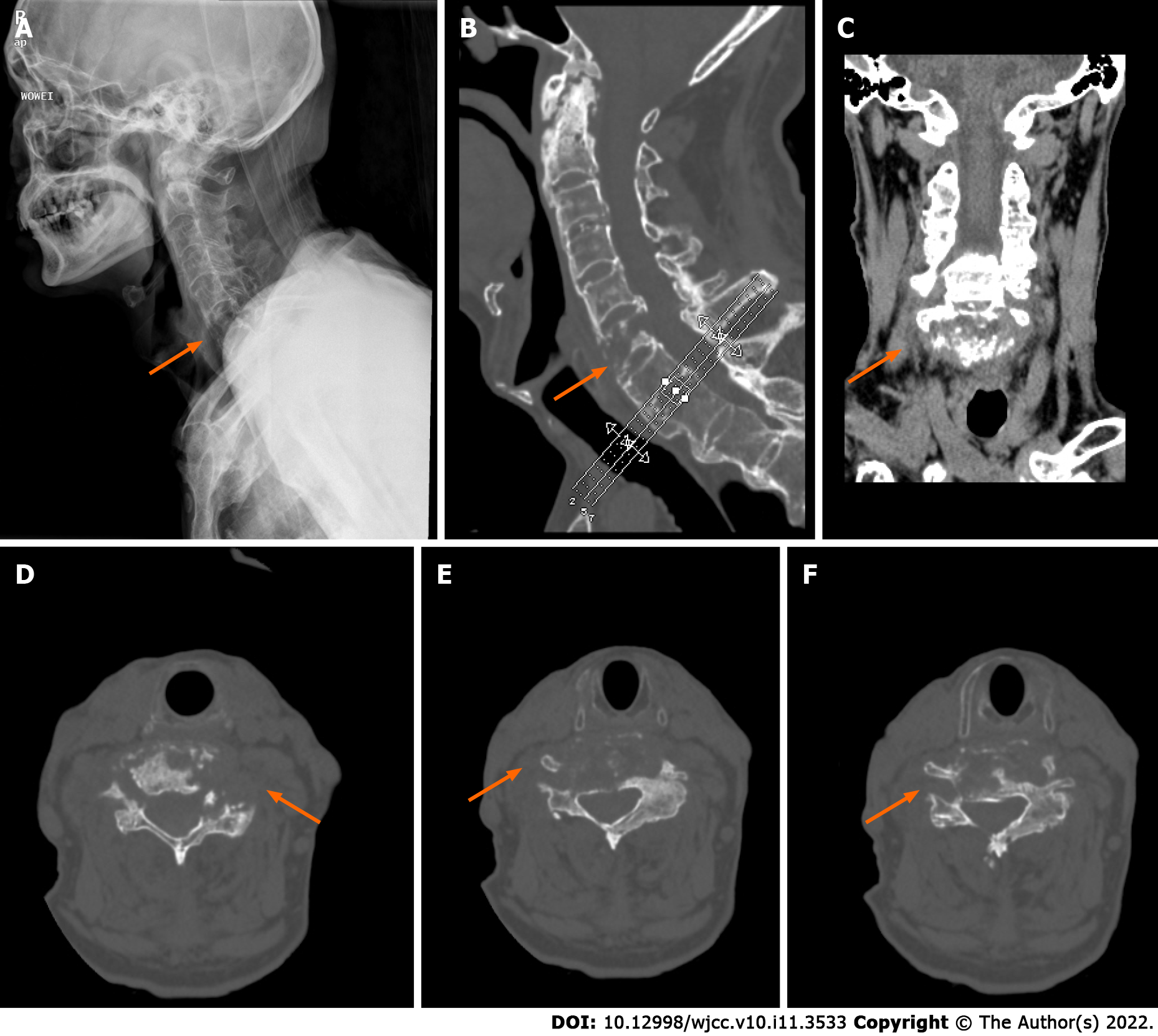
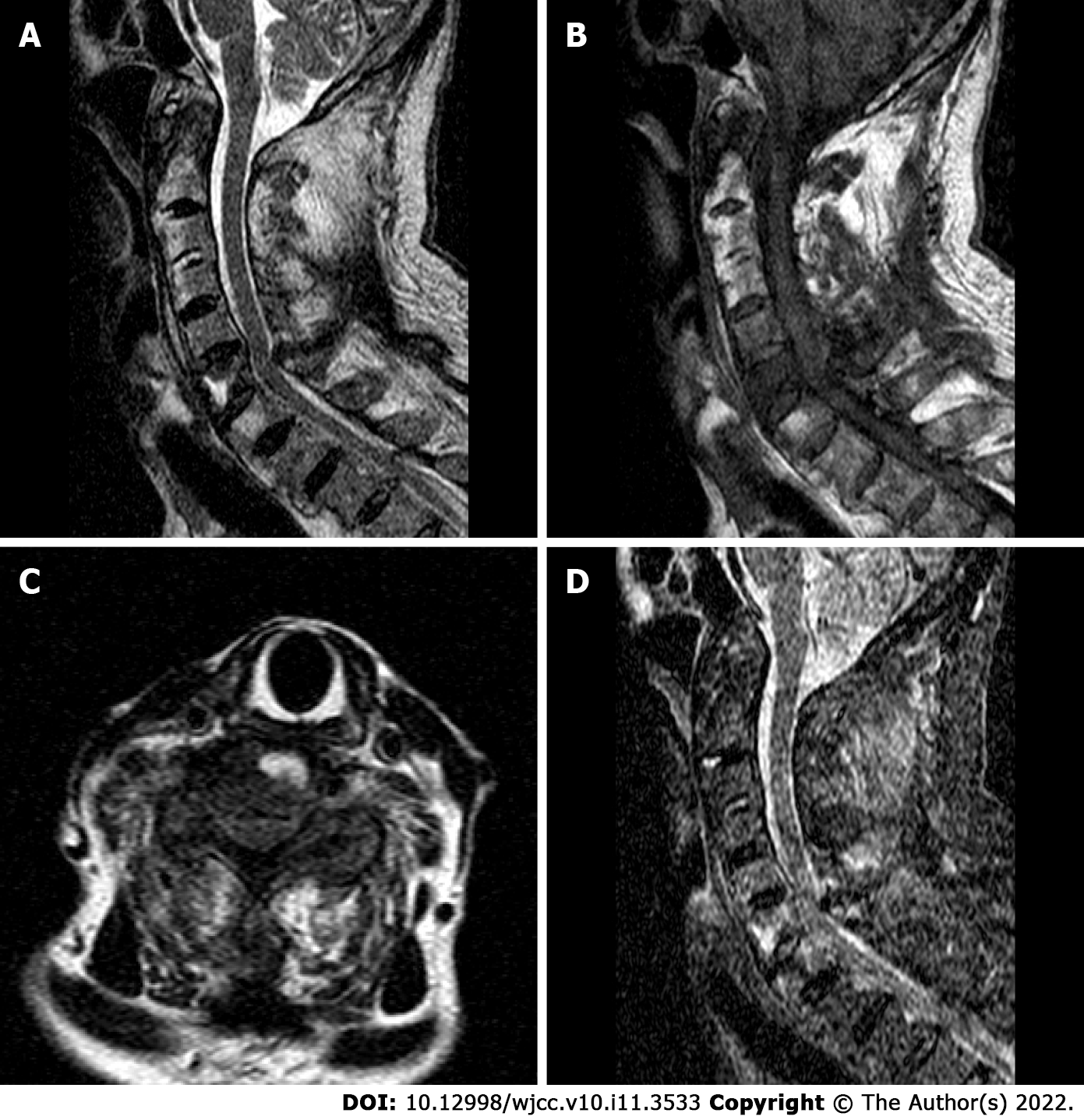
Radiography and computed tomography (CT) scans revealed typical ankylosing spondylitis in the entire spine, i.e., bamboo-like changes; a pathological fracture changed from the C6 vertebra and accumulated at the upper and lower endplates to spinous processes (Figure 1). Magnetic resonance imaging (MRI) showed C6 new-onset vertebral compression fractures and oedema spread from the anterior region of the C6 spinal centrum to the spinous process and supraspinous ligaments, which were complicated by the degenerative cervical instability and compression of the spinal cord due to the injured cervical spinal stenosis (Figure 2).
The final diagnosis of the presented case was Andersson lesion in the lower cervical spine.
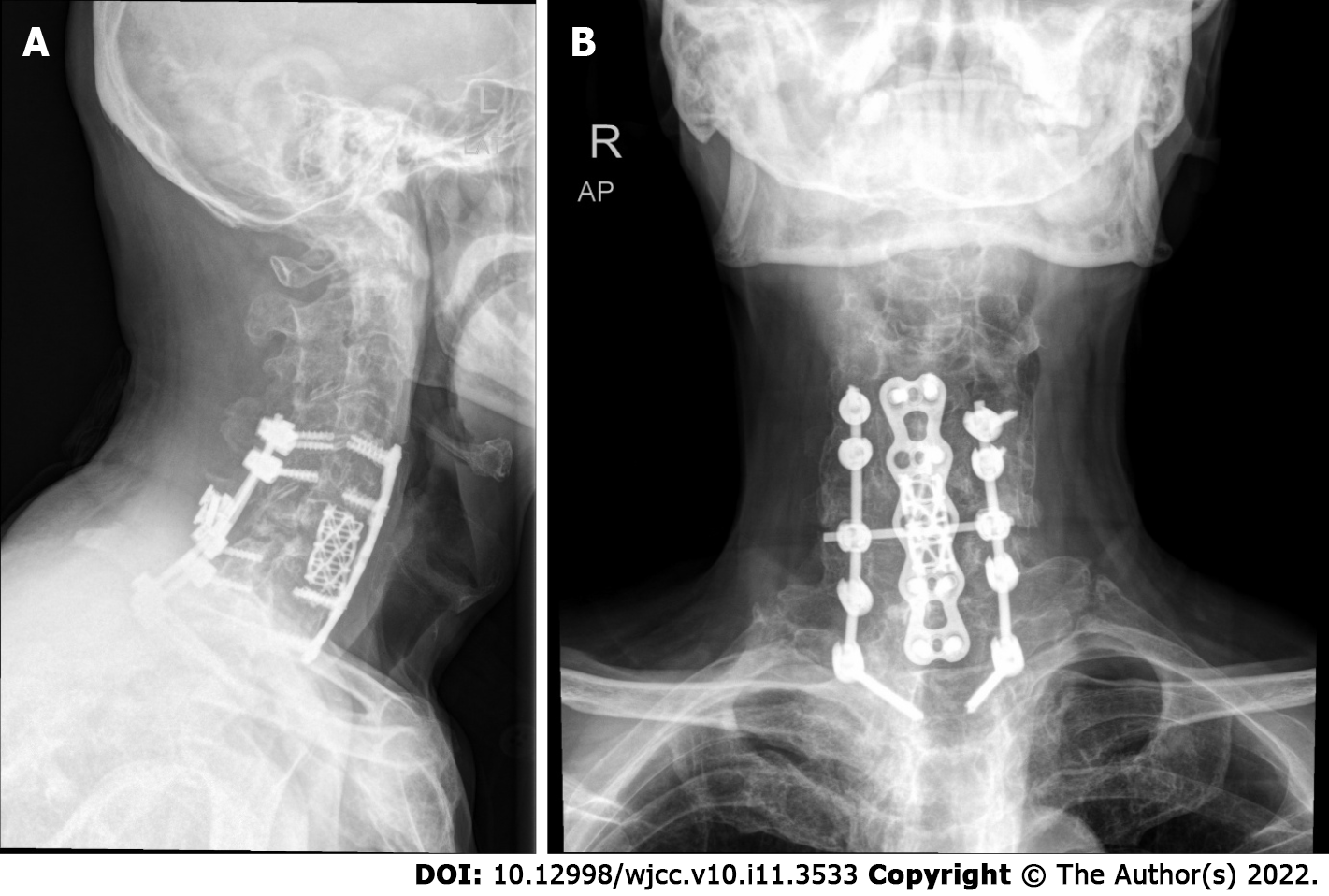
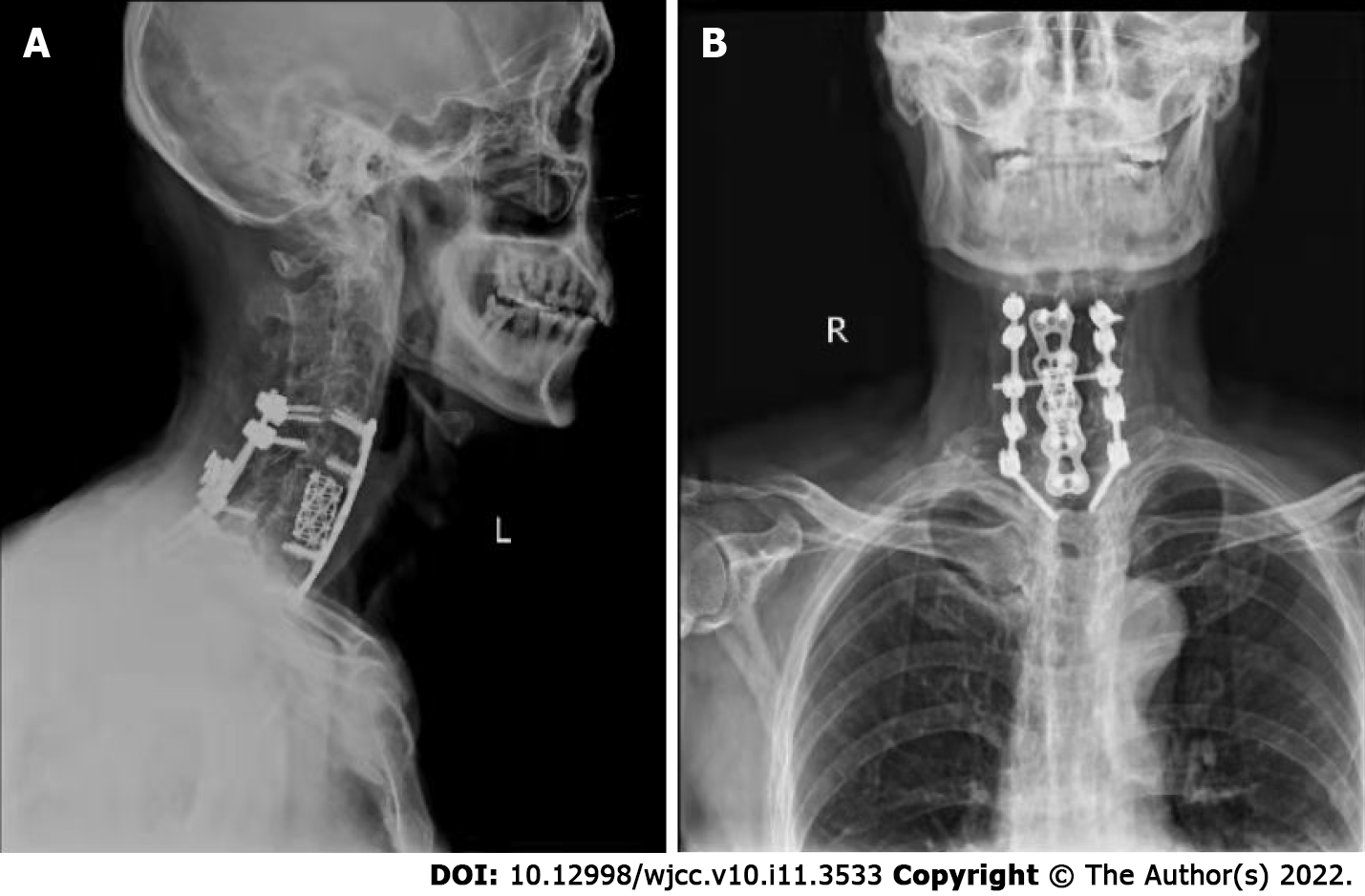
The patient underwent surgery for instrumented stabilization through anterior combined posterior approaches. First, the patient's body temperature was normal throughout the examination. Second, he was convinced that he had no history of tuberculosis or malignant visceral tumours, and all tuberculosis-related laboratory tests or tumour markers were negative. To restore cervical stability, we performed a combined posterior and anterior fixation approach with pedicle screws under a C-arm perspective (Figure 3). In brief, after exposure of C4-T2 with a posterior midline incision, part of the C5 and C6 Laminae were removed using an ultrasonic osteotome; the structure in the spinal canal was exposed, and posterior spinal canal decompression was completed. Under the guidance of C-arm fluoroscopy, the lateral mass or pedicle screws (8 in total, brand: Medtronic) were placed after positioning, drilling and sounding on the side mass of C4, C5 and C7 and the pedicle of T2; a connecting rod (Brand: Medtronic) was used to connect the fixing screws. Next, anterior surgery in the supine position was performed to expose the C6 vertebral body. Under the microscope, the C6 vertebral body and the upper and lower endplates were scraped with a curette. Then, we removed the granulation tissue for pathological examination and bacterial culture, and a short titanium mesh (Brand: Medtronic) was used to support and fix between the C5 Lower endplate and the C6 residual vertebral body. Anterior cervical plates and screws (Brand: Medtronic) were placed in front of C4-T1. To prevent screw loosening caused by osteoporosis, we used bone cement to strengthen the nail channels.
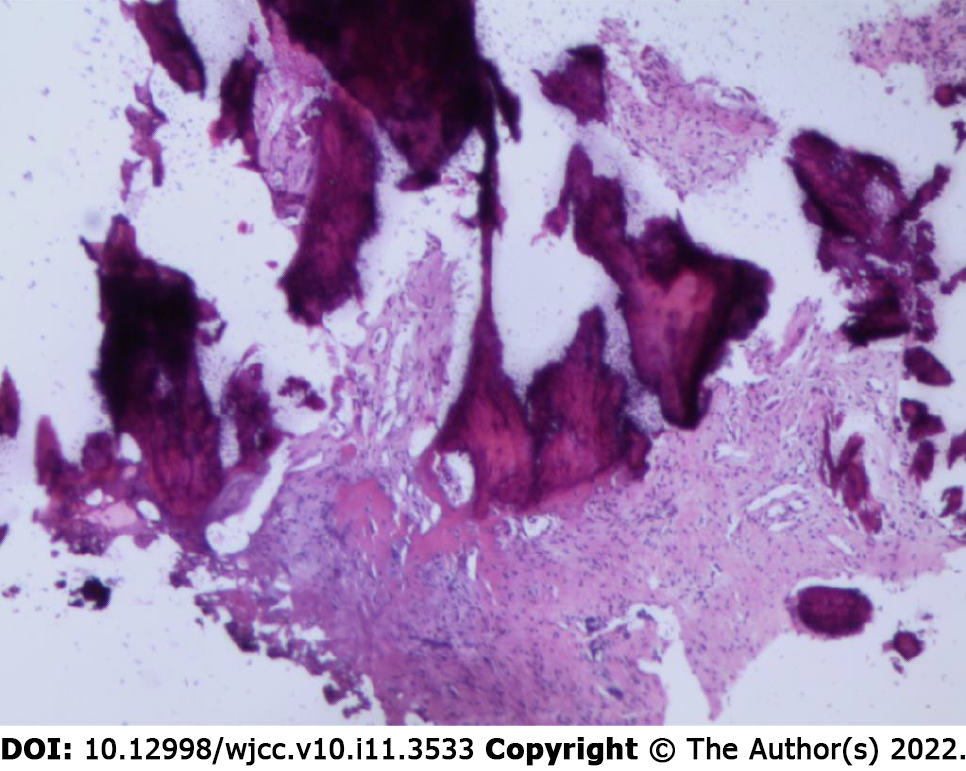
The operation was very successful, and the pathology indicated hyperplastic and fibrous bone tissue with dead bone reaction with no indications of tumour cells and negative bacterial culture results (Figure 4). A postoperative double-check CT scan revealed that the internal fixation device was firm and reliable, and the stability of the cervical spine recovered well. Six months after the operation, the patient reported that the symptoms of pain and numbness were notably relieved and almost returned to normal. The follow-up X-ray images of the cervical spine AL showed that the balance of the coronal plane and sagittal plane recovered well (Figure 5).
Andersson first described the characteristics of destructive lesion of the vertebral body and/or intervertebral disc in patients with ankylosing spondylitis in 1937[8]. Since then, they have been known as Andersson lesion, spondylodiscitis, spinal pseudarthroses and destructive spondylopathy[9,10]. This uncertainty in the naming of AL is mainly due to the lack of consistency in the ethology and pathology of the characteristics of these lesions. To date, two mainstream possible mechanisms have been reported. First, these lesions are considered to have a chronic nonspecific inflammatory nature and are attributed to the disease characteristics of ankylosing spondylitis. The other explanation is that they originate from traumatic injury and are characterized by constitute mechanical stress fracture, spinal nonunion or pseudarthroses after trauma[11-13]. Generally, the entire spine of patients with ankylosing spondylitis is susceptible. However, clinically, the most common site of this lesion is the thoracic and lumbar spine, especially the thoracolumbar transition area, i.e., T10-L2, possibly since this area is defined as the transition area of high stress in anatomy and biomechanics[14-16].
Previous reports on AL mainly involved the thoracic vertebrae and lumbar vertebrae regions, but there were almost no reports of AL in the cervical vertebrae. This is the first study to show nonneoplastic destructive lesion in the lower cervical vertebrae and the induction of cervical trauma injury.
This patient had a recent history of trauma, and the destructive lesion in the C6 vertebra was almost consistent with the characteristics of imaging, pathology and biomechanics of the Andersson lesion (bone destruction caused by chronic compression). Thus, we suspected that these unstable lower cervical spine fractures resulted from trauma with Andersson lesion, although the location was different from that previously reported (mainly in the thoracic and lumbar vertebrae). Most AL patients have been middle-aged and elderly men with or without AS symptoms for decades. The common clinical manifestations are local intolerable and progressive pain of the thoracolumbar spine and local severe pain after mild trauma with dysfunction[12].
When combined with spinal cord nerve injury, some patients have serious symptoms such as numbness, muscle weakness, incomplete paralysis or even paraplegia. X-ray examination can preliminarily detect the degree of erosive bone destruction. Computed tomography is more accurate and stereoscopic than X-ray in displaying bone lesion, especially in assessing the location of spinal cord compression, the involvement of the spinal canal, the severity of vertebral destruction and the injury mechanism. In addition, MRI can provide information about the involvement of soft tissue around the spine, and the state of the spinal cord and nerve is clearer.
Based on the imaging findings for this patient, AL might be easily misdiagnosed for spinal tuberculosis or spinal metastasis because these conditions are mostly identified by bone destruction. In addition, both AL and spinal tuberculosis may be characterized by the narrowed intervertebral space, hyperosteogeny and late sclerosis[13]. Unlike AL, most patients with spinal tuberculosis have low fever, night sweats and other systemic symptoms in the early stage, and the anti-tuberculosis treatment is effective. Similarly, patients with spinal metastases often have symptoms in primary organs, such as gastrointestinal tumours and prostate cancer. Spinal metastases are common in the thoracolumbar spine, and cervical metastases are rarely reported. With detailed physical examination and previous AS disease history, laboratory markers, X-ray, CT and magnetic resonance examination are vitally important for the diagnosis of AL.
To the best of our knowledge, there are no exact and consistent guidelines on how to systematically treat AL[17]. Conservative treatment, including NSAIDs and anti-TNF-α therapy, is often initially suggested, and some researchers have confirmed that conservative treatment is safe and effective[8]. Nevertheless, there is still no recognized evidence that these drugs can help the treatment of symptomatic AL, although they have been proven to be effective in patients with ankylosing spondylitis. Therefore, surgical treatment is recommended to reduce unbearable pain, kyphosis deformity, biomechanical instability or neurological deficits caused by trauma[18-21]. Our patient had a mild traumatic fracture involving three columns of the cervical spine secondary to Andersson lesion. To reconstruct the stability of the cervical spine and fully decompress the spinal canal, we chose the posterior with the anterior approach for surgery. According to our experience, successful interbody fusion through surgery (one-stage internal fixation) is the safest and most effective choice to treat AL.
In summary, AL constitutes a relatively infrequent nonneoplastic bone destruction in patients with AS. Our report provides a meaningful reference for the diagnosis, differential diagnosis, treatment and prognosis of AL. Surgery is a more reasonable choice to treat AL with unstable cervical fracture, especially for patients with kyphosis and dysfunction caused by nerve compression. Fusion is critical, and complete decompression is fundamental in the treatment of Andersson lesion.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cure E, Turkey; Hui Yang, China S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Wu M, Yan F, Ping A, Lei J. Effects of Andersson lesion treatment in ankylosing spondylitis: A medical record review study focused on medium- to long-term outcomes. Int J Rheum Dis. 2020;23:753-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Ji X, Su M, Chen J, Wang X, Cai X. A novel method for plastic particle sizing in suspension based on acoustic impedance spectrum. Ultrasonics. 2017;77:224-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Shao J, Gao YZ, Gao K, Yu ZH. Ankylosing Spondylitis Complicated with Atlantoaxial Dislocation and Destruction of the Dens and Lateral Atlantoaxial Joint: A Case Report. JBJS Case Connect. 2019;9:e0216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Fu X, Zhang Y, Jiang W, Monnot AD, Bates CA, Zheng W. Regulation of copper transport crossing brain barrier systems by Cu-ATPases: effect of manganese exposure. Toxicol Sci. 2014;139:432-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Zhang X, Wang Y, Wu B, Hu W, Zhang Z. Treatment of Andersson lesion-complicating ankylosing spondylitis via transpedicular subtraction and disc resection osteotomy, a retrospective study. Eur Spine J. 2016;25:2587-2595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Barman A, Sinha MK, Rao PB. Discovertebral (Andersson) lesion of the Ankylosing Spondylitis, a cause of autonomic dysreflexia in spinal cord injury. Spinal Cord Ser Cases. 2016;2:16008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 7. | Liang Y, Tang X, Zhao Y, Wang Z. Posterior wedge osteotomy and debridement for Andersson lesion with severe kyphosis in ankylosing spondylitis. J Orthop Surg Res. 2017;12:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Wang HF, Bi C, Chen ZQ. [Research progress on Andersson lesion in ankylosing spondylitis]. Zhonghua Wai Ke Za Zhi. 2017;55:798-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Van Royen BJ, Kastelijns RC, Noske DP, Oner FC, Smit TH. Transpedicular wedge resection osteotomy for the treatment of a kyphotic Andersson lesion-complicating ankylosing spondylitis. Eur Spine J. 2006;15:246-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Obradov M, Schönfeld DH, Franssen MJ, de Rooy DJ. Andersson lesion in ankylosing spondylitis. JBR-BTR. 2001;84:71. [PubMed] |
| 11. | Queiro R, Tejón P, Alonso S, Alperi M, Ballina J. Erosive discovertebral lesion (Andersson lesion) as the first sign of disease in axial psoriatic arthritis. Scand J Rheumatol. 2013;42:220-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Dhakad U, Das SK. Andersson lesion in ankylosing spondylitis. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Park YS, Kim JH, Ryu JA, Kim TH. The Andersson lesion in ankylosing spondylitis: distinguishing between the inflammatory and traumatic subtypes. J Bone Joint Surg Br. 2011;93:961-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Wang G, Zhuo N, Tian F, Wen Z, Li J. Andersson lesion in the lumbar spine of SAPHO syndrome. Rheumatology (Oxford). 2022;61:877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Qin W, Yang P, Zhou F, Mao H, Yang H. Andersson Lesion Occurring in the Lumbosacral Segment of a Young Man: A Case Report and Literature Review. World Neurosurg. 2020;143:419-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Hu X, Kong Y, Li B. Andersson Lesion in the Thoracic Spine. J Clin Rheumatol. 2021;27:e258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Yang F, Yang L, Ren E, Yang Y, Wang J, Kang X. Surgical Treatment of Ankylosing Spondylitis with Andersson Lesion. J Coll Physicians Surg Pak. 2019;29:S135-S137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Dave BR, Kulkarni M, Patidar V, Devanand D, Mayi S, Reddy C, Singh M, Rai RR, Krishnan A. Results of in situ fixation of Andersson lesion by posterior approach in 35 cases. Musculoskelet Surg. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Ding K, Zhu J, Chen H, Tian Y, Hao D. [Debridement and interbody fusion via posterior pedicle lateral approach for ankylosing spondylitis with thoracolumbar Andersson lesion]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33:1474-1479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Shaik I, Bhojraj SY, Prasad G, Nagad PB, Patel PM, Kashikar AD, Kumar N. Management of Andersson Lesion in Ankylosing Spondylitis Using the Posterior-Only Approach: A Case Series of 18 Patients. Asian Spine J. 2018;12:1017-1027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Rajoli SR, Kanna RM, Aiyer SN, Shetty AP, Rajasekaran S. Circumferential Fusion through All-Posterior Approach in Andersson Lesion. Asian Spine J. 2017;11:444-453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |