Published online Apr 16, 2022. doi: 10.12998/wjcc.v10.i11.3485
Peer-review started: July 25, 2021
First decision: October 25, 2021
Revised: November 4, 2021
Accepted: February 27, 2022
Article in press: February 27, 2022
Published online: April 16, 2022
Processing time: 257 Days and 1.4 Hours
Glomus tumors are rare neoplasms, usually found on the fingers or toes. Glomus tumours that occur in the lower leg are even rarer and is likely to be misdiagnosed or underdiagnosed. This article will document the diagnosis, treatment, and follow-up of a rare glomus tumor of the lower leg, which had been misdiagnosed for up to 15 years.
The patient was a A 36-year-old woman who had suffered from localized pain in her left lower leg for 15 years. After a complete physical examination, a glomus tumor on her lower leg was considered and removed surgically. The specimen was pathologically diagnosed as a glomus tumor. There was no relapse at a 4-year follow-up.
Correct diagnosis and complete removal of the glomus tumor is important.
Core Tip: A 36-year-old woman who had suffered from localized pain in her left lower leg had been misdiagnosed for up to 15 years. She was eventually diagnosed with glomus tumor and underwent surgical treatment. The patient recovered well with no recurrence observed at a 4-year follow-up.
- Citation: Wang HY, Duan P, Chen H, Pan ZY. Unusual glomus tumor of the lower leg: A case report. World J Clin Cases 2022; 10(11): 3485-3489
- URL: https://www.wjgnet.com/2307-8960/full/v10/i11/3485.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i11.3485
Glomus tumor (GT), a rare neoplasm caused by degenerated smooth muscle cells in a neuro-arterial adenoma, regulates body temperature through arteriovenous shunting of blood[1,2]. Most GTs are benign, with few malignant cases reported[3,4]. The characteristic clinical manifestations of GT are spontaneous lancinating pain, extreme pain with the slightest touch, and intolerance to temperature changes[5]. It usually presents as a well-defined, blue or red nodule, often located on the fingers or toes, especially in the nail bed, and uncommon elsewhere[6]. Individual literatures have reported GTs occurring in rare sites such as sinonasal location, but more evidences are needed to verify this[7]. We reviewed the literature and found that GT was infrequently reported in the lower leg, thus, it is likely to be misdiagnosed or underdiagnosed. In this article, we report the diagnosis, treatment and follow-up of a rare case of GT of the lower leg, which was misdiagnosed for up to 15 years because of its small number of favored sites and size. The tumor was removed surgically and the patient had complete remission after surgery. This case can enhance our understanding of the rare location of GTs to decrease misdiagnosis and missed diagnosis.
A 36-year-old Asian woman was admitted to our hospital on April 25, 2016 with localized pain in the left anterior tibial region for 15 years.
The patient had visited several hospitals in the past 15 years but was diagnosed with venous thrombosis, which did not improve with conservative treatment such as analgetics. Over the past three years, the patient's pain had progressively worsened, and was exacerbated by touch, temperature changes and mood swings. In addition, the patient often had a poor sleep at night because of the pain.
No special history of past illness.
There was no personal history of GT or any other family medical history.
Physical examination revealed mildly localized swelling on the on left leg along with tenderness in a 50 mm × 30 mm area of skin on the anterior medial aspect of her left lower extremity, with no ulceration or warmth.
No obvious abnormality was found in laboratory examination.
After careful consideration of the patient's medical history and physical examination findings, including spontaneous tingling, minimal tenderness and intolerance to temperature changes, we made a tentative diagnosis of GT.
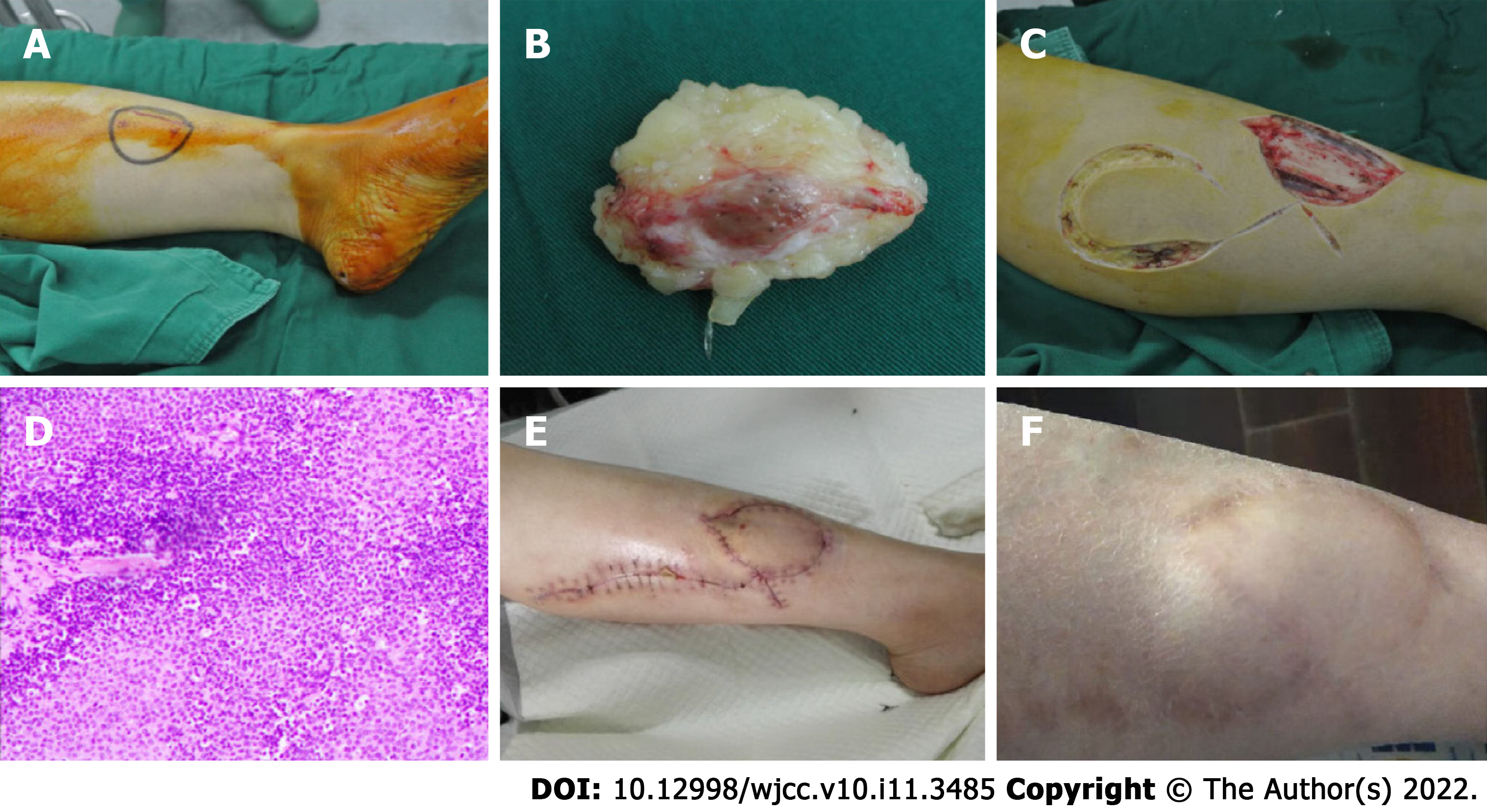
After a thorough preoperative examination and confirming no surgical contraindications, the patient underwent soft tissue lesion resection, biopsy and flap transposition on April 27, 2016 (Figure 1A). Intra-operative examination showed an oval tumor with a light red colour, firm texture, intact envelope and clear contours under the skin of her lower leg.
We completely removed the tumor and the surrounding normal soft tissue, which was approximately 10 mm in thickness and 50 mm × 30 mm in size, for pathological diagnosis (Figure 1B). Because of the skin and soft-tissue defect, we designed a lateral gastrocnemius nutrition flap of the left lower limb to cover it (Figure 1C).
The pathological examination at our hospital showed a spindle cell tumor (Figure 1D). The results of immunohistochemistry were as follows: Ki-67 (3%, partially up to 10%), Caldesmon(+), CK(-), P63(-), S-100(-), SMA(part+), VIMENTIN(+), GFAP(-), CD31(-), CD34(-), HMB45(-). The examination results at two other tertiary hospitals confirmed it to be a GT. Suturing was performed two weeks after surgery. The wound healed well, and the survival of the skin flap was satisfactory (Figure 1E). There was no abnormality in blood flow, sensation and movement of her left lower limb. At the one-month follow up, the wound was well healed and patient was pain free. No recurrence of pain was observed during a 4-year follow-up (Figure 1F).
GTs were firstly reported by Wood in 1812 as "painful subcutaneous tubercle"[8]. It was not until 1924 that Masson et al named it GT after pathological analysis[5]. GTs are most commonly encountered on the fingers[9]. It has been reported to be very rare, accounting for 1% to 2% of all soft tissue tumors, most of which are benign[3,4,10]. The characteristic clinical manifestations of GTs are subcutaneous blue or red nodules, firm and smooth, usually no more than 10 mm in diameter. Pain is the most obvious symptom of the disease, usually presenting as spontaneous tingling, extreme pain with the slightest touch, and intolerance to temperature changes[5,11]. In addition to these obvious symptoms, uncommon presentations such as tumor-induced osteomalacia were also reported, but more evidences are needed to support this discovery[12]. The disease diagnosis depends on clinical tests such as the Love test (point tenderness) and Hildreth's sign (decreased pain on exsanguination of the limb and application of a tourniquet)[13]. In addition to qualitative diagnosis, characteristic pain can also be used to localize the lesion. Magnetic resonance imaging (MRI) is occasionally helpful, and hyperenhanced lesions on T2 weighted and short time inversion recovery sequence imaging may illustrate the vascular appearance of GT. Other imaging examinations may include plain radiography, computed tomography and colour Doppler ultrasonography. However, all of the above may be negative and exploration of the painful location should be considered if a GT is suspected even if the MRI findings are negative[14].
In the present case, the tumor was located in the left anterior tibial region, which is relatively rare, so it had been misdiagnosed as venous thrombosis or sciatica resulting in chronic pain for up to 15 years. On the one hand, the initial symptom was pain, which would be easily confused with skin disease, thrombotic diseases, etc., when the disease is located in the lower leg. On the other hand, the huge size of this tumor is extremely rare in this disease. A study of 138 cases suggested that the median size of superficial GT was 8 mm, with none exceeding 45 mm[1], while the size of the tumor in our case was up to 50 mm in size.
Once diagnosed, surgical resection is an effective method for the treatment of GT. It should still be noted that recurrence may occur due to incomplete resection. We should therefore remove the tumor completely during surgery via avoiding residuals and expanding the resection area when conditions permit[15]. In previous case reports, a simple excisional approach has generally been used. In our case, we used an innovative combination of extended tumor resection and flap transposition due to the large volume of the tumor to avoid soft tissue defects while resecting the tumor completely. The patient recovered well after the surgery with no recurrence observed during the 4 years of follow-up. The patient was satisfied with the surgery and recovered well.
The patient with glomus tumor had visited many specialists and underwent numerous examinations before receiving a correct diagnosis. Correct diagnosis and surgical treatment eventually healed her. Remaining alert to rare diseases can be an effective way to avoid them.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Peripheral vascular disease
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghannam WM, Egypt; Raj R, United States S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Mravic M, LaChaud G, Nguyen A, Scott MA, Dry SM, James AW. Clinical and histopathological diagnosis of glomus tumor: an institutional experience of 138 cases. Int J Surg Pathol. 2015;23:181-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 108] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 2. | Singh D, Garg RS, Vikas, Garg Y, Arora V. Glomus Tumor - A Rarity; M.R.I- A big help in early Diagnosis. J Orthop Case Rep. 2016;6:38-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 3. | McDermott EM, Weiss AP. Glomus tumors. J Hand Surg Am. 2006;31:1397-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 406] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 5. | Abou Jaoude JF, Roula Farah A, Sargi Z, Khairallah S, Fakih C. Glomus tumors: report on eleven cases and a review of the literature. Chir Main. 2000;19:243-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Gombos Z, Zhang PJ. Glomus tumor. Arch Pathol Lab Med. 2008;132:1448-1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 173] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 7. | Raj R, Hasanzadeh S, Dashtizadeh M, Kalantarhormozi M, Vahdat K, Dabbaghmanesh MH, Nabipour I, Ravanbod M, Assadi M, Hashemi B, Asadipooya K. Oncogenic osteomalacia secondary to glomus tumor. Endocrinol Diabetes Metab Case Rep. 2021;2021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Gombos Z, Fogt F, Zhang PJ. Intraosseous glomus tumor of the great toe: a case report with review of the literature. J Foot Ankle Surg. 2008;47:299-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Takase K. Intraosseous glomus tumour in the distal phalanx of the index finger. J Hand Surg Eur Vol. 2011;36:74-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Tuncali D, Yilmaz AC, Terzioglu A, Aslan G. Multiple occurrences of different histologic types of the glomus tumor. J Hand Surg Am. 2005;30:161-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Heys SD, Brittenden J, Atkinson P, Eremin O. Glomus tumour: an analysis of 43 patients and review of the literature. Br J Surg. 1992;79:345-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Dehghani M, Dabbaghmanesh MH, Khalafi-Nezhad A, Riazmontazer N, Dehghanian A, Vojdani R, Sasani M. Glomus tumor as a cause of oncogenic osteomalacia. Clin Cases Miner Bone Metab. 2017;14:359-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Giele H. Hildreth's test is a reliable clinical sign for the diagnosis of glomus tumours. J Hand Surg Br. 2002;27:157-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Al-Qattan MM, Al-Namla A, Al-Thunayan A, Al-Subhi F, El-Shayeb AF. Magnetic resonance imaging in the diagnosis of glomus tumours of the hand. J Hand Surg Br. 2005;30:535-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 92] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 15. | Giugale JM, Fowler JR. Glomus Tumors: A Review of Preoperative Magnetic Resonance Imaging to Detect Satellite Lesions. Orthopedics. 2015;38:e888-e890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |