Published online Apr 16, 2022. doi: 10.12998/wjcc.v10.i11.3426
Peer-review started: August 20, 2021
First decision: November 11, 2021
Revised: November 12, 2021
Accepted: February 27, 2022
Article in press: February 27, 2022
Published online: April 16, 2022
Processing time: 230 Days and 20.8 Hours
The purpose of enhanced recovery after surgery (ERAS) was to reduce surgical pressure and accelerate postoperative functional recovery. Although the application of biologics in treating inflammatory bowel disease (IBD) has changed treatment strategies, most patients with IBD still require surgery.
To evaluate the advantage of ERAS in IBD surgery.
The PubMed, EMBASE and Cochrane Library databases were searched from inception to March 21, 2021 to find eligible studies. The primary outcome was postoperative complications, and the secondary outcomes included operation time, time to first flatus, time to bowel movement, postoperative hospital stay and readmission. The PROSPERO registration ID of this meta-analysis is CRD42021238052.
A total of eight studies involving 1939 patients were included in this meta-analysis. There were no differences in baseline information between the ERAS group and the non-ERAS group. After pooling up all of the data, no significant difference was found between the ERAS group and the non-ERAS group in terms of postoperative overall complications [odds ratio = 0.82, 95% confidence interval (CI) = 0.66 to 1.02, P = 0.08]. The ERAS group had a lower prevalence of anastomotic fistula (odds ratio = 0.36, 95%CI = 0.13 to 0.95, P = 0.04), less time to first flatus [mean difference (MD) = -2.03, 95%CI = -3.89 to -0.17, P = 0.03], less time to bowel movement (MD = -1.08, 95%CI = -1.60 to -0.57, P < 0.01) and shorter postoperative hospital stays (MD = -1.99, 95%CI = -3.27 to -0.71, P < 0.01) than the non-ERAS group.
ERAS was effective for the quicker recovery in IBD surgery and did not lead to increased complications.
Core Tip: The purpose of this meta-analysis was to evaluate the safety and efficacy of enhanced recovery after surgery in inflammatory bowel disease surgery. In conclusion, enhanced recovery after surgery was effective for the quicker recovery in inflammatory bowel disease surgery and did not lead to increased complications.
- Citation: Peng D, Cheng YX, Tao W, Tang H, Ji GY. Effect of enhanced recovery after surgery on inflammatory bowel disease surgery: A meta-analysis. World J Clin Cases 2022; 10(11): 3426-3435
- URL: https://www.wjgnet.com/2307-8960/full/v10/i11/3426.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i11.3426
Enhanced recovery after surgery (ERAS) or fast-track surgery programs were first proposed by Kehlet[1], and the purpose of ERAS was to reduce surgical pressure and accelerate postoperative functional recovery[2]. The ERAS protocol involves a series of interventions during the perioperative period, including preoperative short fasting, intraoperative epidural anesthesia, minimally invasive surgery, postoperative pain management and nutritional care[3-5]. Due to its significant advantages and safety, ERAS has developed rapidly over the past decade[6]. In recent years, ERAS has been applied to various surgical fields, including gastrectomy[7], cardiac surgery[8], esophageal cancer surgery and colorectal surgery[9,10].
Although the application of biologics in treating inflammatory bowel disease has changed treatment strategies, most patients with inflammatory bowel disease (IBD) still require surgery[11,12]. IBD patients are often malnourished and immunosuppressed, which increases the risk of postoperative complications and prolongs the postoperative hospital stay[13]. In addition, reoperation was required in a large population of IBD patients, which might not be suitable for minimally invasive surgery[14]. Furthermore, patients with IBD might experience prolonged postoperative intestinal obstruction due to chronic inflammation of the intestinal wall[15]. Therefore, the application of ERAS in IBD surgery might be limited in these high-risk situations.
A few studies suggest the feasibility of ERAS for IBD patients[16]; however, work comparing the efficiency of ERAS in IBD and non-IBD patients is scant[17]. Therefore, the purpose of this meta-analysis was to evaluate the safety and efficacy of ERAS in IBD surgery.
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement[18]. The PROSPERO registration ID is CRD42021238052, and the link is as follows: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021238052.
The PubMed, EMBASE and Cochrane Library databases were searched by two authors independently. The literature search was conducted on March 21, 2021. The search strategy focused on two key words: ERAS and IBD. The search strategy for ERAS was as follows: "enhanced recovery protocol" OR "enhanced recovery after surgery" OR "enhanced recovery" OR "fast track surgery" OR "fast track rehabilitation" OR "fast track" OR "FTS" OR "ERAS". The search strategy for IBD was as follows: "inflammatory bowel disease" OR "Crohn’s" OR "Crohn disease" OR "Crohn’s disease" OR "ulcerative colitis" OR "colitis" OR "IBD" OR "CD" OR "UC". Then, we used “AND” to combine these two search strategies, and the publication language was restricted to English in this search.
The inclusion criteria were as follows: 1, patients who underwent surgery for CD or UC; 2, the ERAS and non-ERAS protocols were both reported; and 3, reported at least one of the surgical outcomes, including operation time, complications, time to first flatus, time to bowel movement, postoperative hospital stay and readmission. The exclusion criteria were as follows: 1, reviews, letters, case reports, comments or conferences; and 2, publications with insufficient data that could not be extracted. For studies with overlapping patient groups, the most recent study or the study with the larger sample size were included. Disagreement regarding inclusion and exclusion were resolved by discussion between the two authors.
The databases were searched by the two authors. First, the titles and abstracts were screened for relevant studies. Second, the full texts were evaluated based on the inclusion and exclusion criteria. Disagreements were discussed, and a final judgment was made by a third author if disagreement occurred.
The data were extracted and cross-checked by two authors. The extracted data included first author, study date, study design, country, publishing year, patients’ baseline information, sample size, operation time, complications, time to first flatus, time to bowel movement, postoperative hospital stay and readmission.
The primary outcome of the current meta-analysis was postoperative complications, which were graded based on the Clavien-Dindo classification[19]. Secondary outcomes included operation time, time to first flatus, time to bowel movement, postoperative hospital stays and readmission.
The Newcastle-Ottawa Scale was used to evaluate the quality of the included studies[20]. High-quality studies are indicated by a score of 9 points, medium-quality studies have scores from 7-8 points, and low-quality studies have scores less than 7 points[21].
In the current meta-analysis, continuous variables are presented as the mean ± standard deviation, and categorical variables are presented as proportions. For dichotomous and continuous variables, odds ratios (ORs) and mean differences (MDs) were calculated, and 95% confidence intervals (CIs) were calculated. The I2 value and the results of the chi-squared test were used to assess the statistical heterogeneity[22,23]. High heterogeneity was considered when I2 > 50%; in such cases, the random effects model was used, and P < 0.1 was considered statistically significant. The fixed effects model was used when I2 ≤ 50%, and P < 0.05 was considered statistically significant. This meta-analysis was performed with RevMan 5.3 (The Cochrane Collaboration, London, United Kingdom).
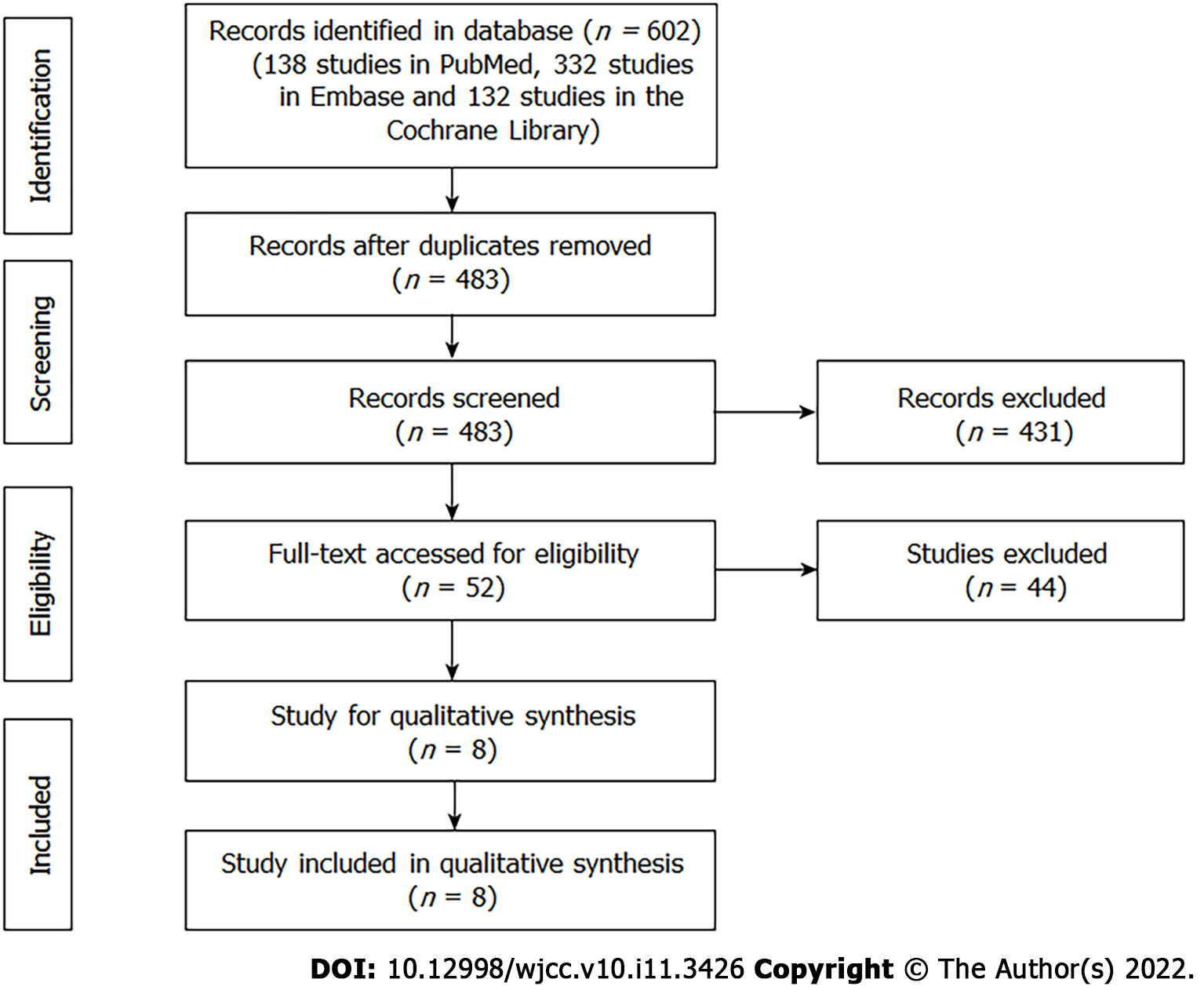
A total of 602 studies (138 studies in PubMed, 332 studies in EMBASE and 132 studies in the Cochrane Library) were retrieved in the initial search, and 483 studies were screened after excluding duplicated records. The titles and abstracts were screened, and then, 52 studies were left for full-text assessment. Finally, a total of eight studies[16,24-30] that compared the surgical outcomes of IBD patients between ERAS and non-ERAS protocols were included (Figure 1).
A total of eight studies including 1939 patients were included in this meta-analysis. The publication years ranged from 2012- 2021, and the study dates ranged from 2000-2019. There were six retrospective studies, one observational study and one randomized controlled trial (RCT). Three studies were conducted in United States, two studies were conducted in Italy, one study was conducted in China, one study was conducted in France and one study was conducted in the United Kingdom. The sample size and the scores of the Newcastle-Ottawa Scale of each study are shown in Table 1.
| Ref. | Year | Study date | Study design | Single/Multi center | Disease type | Country | Sample size | NOS |
| Spinelli et al[24] | 2012 | January 2008 to September 2011 | Retrospective | Multi center | CD | Italy | 90 | 7 |
| Mineccia et al[25] | 2020 | May 2007 to December 2018 | Observational | Single center | CD | Italy | 94 | 8 |
| Liska et al[26] | 2019 | January 2015 to April 2017 | Retrospective | Single center | CD and UC | United States | 671 | 8 |
| D'Andrea et al[27] | 2020 | January 2013 to December 2018 | Retrospective | Single center | CD and UC | United States | 753 | 8 |
| Zhu et al[28] | 2018 | December 2015 to December 2016 | RCT | Single center | CD | China | 32 | 8 |
| Vrecenak et al[29] | 2014 | December 2000 to December 2010 | Retrospective | Single center | CD | United States | 71 | 7 |
| West et al[30] | 2013 | January 2005 to January 2011 | Retrospective | Multi center | CD and UC | United Kingdom | 68 | 8 |
| Meunier et al[16] | 2021 | November 2015 to December 2019 | Retrospective | Multi center | Unknown | France | 160 | 8 |
The baseline information, including age, sex, body mass index, American Society of Anesthesia and surgical methods, was pooled, and no differences were found between the ERAS group and the non-ERAS group. The summary meta-analysis of baseline information in each study is shown in Table 2.
| Characteristics | Studies | Participants, ERAS/Non-ERAS | Odds ratio/mean difference (95%CI) | Heterogeneity |
| Baseline information | ||||
| Age, yr | 2 | 256/587 | 0.35 (-1.72, 2.78); P = 0.65 | I2 = 0%; P = 0.59 |
| Male | 7 | 644/1135 | 1.20 (0.98, 1.46); P = 0.08 | I2 = 0%; P = 0.74 |
| BMI, kg/m2 | 3 | 272/603 | -0.56 (-1.19, 0.06); P = 0.08 | I2 = 12%; P = 0.32 |
| ASA 1-2 | 4 | 549/1059 | 0.91 (0.73, 1.14); P = 0.41 | I2 = 0%; P = 0.77 |
| ASA 3-4 | 4 | 510/1059 | 1.10 (0.88, 1.37); P = 0.41 | I2 = 0%; P = 0.77 |
| Laparoscopic surgery | 4 | 563/1023 | 1.47 (0.90, 2.38); P = 0.12 | I2 = 62%; P = 0.05 |
| Open surgery | 4 | 460/1023 | 0.68 (0.42, 1.11); P = 0.12 | I2 = 62%; P = 0.05 |
| Surgical outcomes | ||||
| Operation time | 2 | 256/587 | -0.17 (-23.45, 23.10); P = 0.99 | I2 = 78%; P = 0.03 |
| Time to first flatus | 2 | 36/86 | -2.03 (-3.89, -0.17); P = 0.03 | I2 = 94%; P < 0.01 |
| Time to bowel movement | 3 | 81/112 | -1.08 (-1.60, -0.57); P < 0.01 | I2 = 71%; P = 0.03 |
| Post-operative hospital stay | 4 | 317/629 | -1.99 (-3.27, -0.71); P < 0.01 | I2 = 89%; P < 0.01 |
| Anastomotic fistula | 6 | 639/1200 | 0.36 (0.13, 0.95); P = 0.04 | I2 = 0%; P = 0.70 |
| Bleeding | 4 | 358/568 | 1.16 (0.48, 2.76); P = 0.75 | I2 = 0%; P = 0.80 |
| Readmission rate | 7 | 673/1234 | 0.72 (0.51, 1.00); P = 0.05 | I2 = 0%; P = 0.87 |
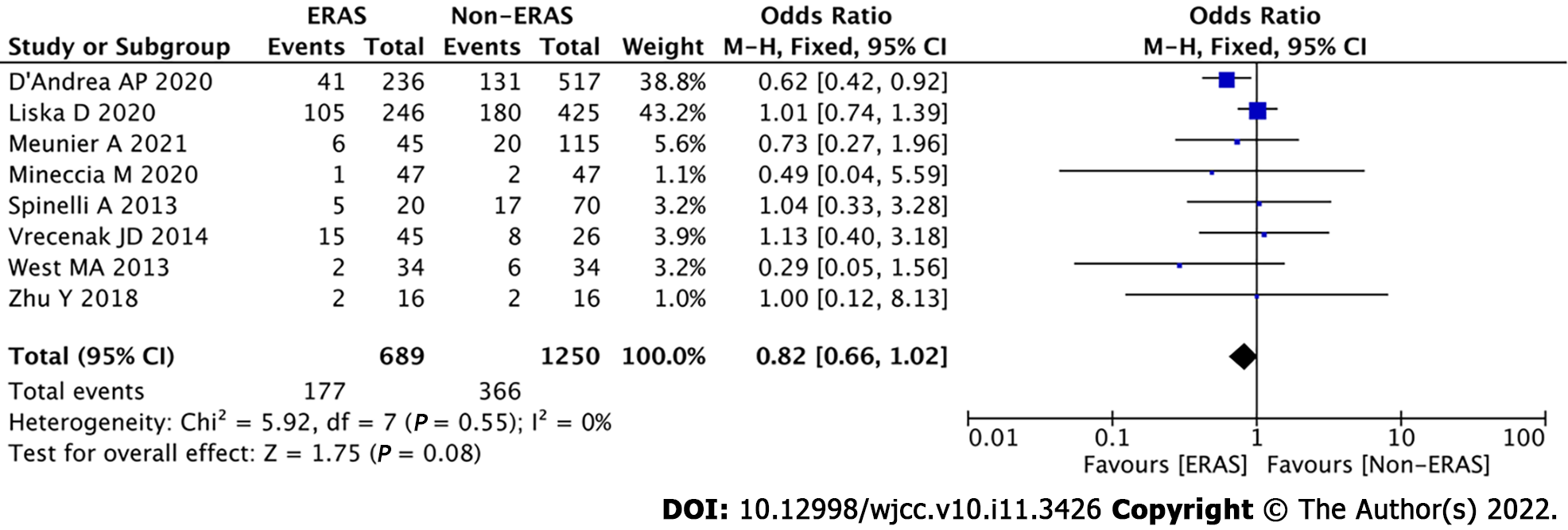
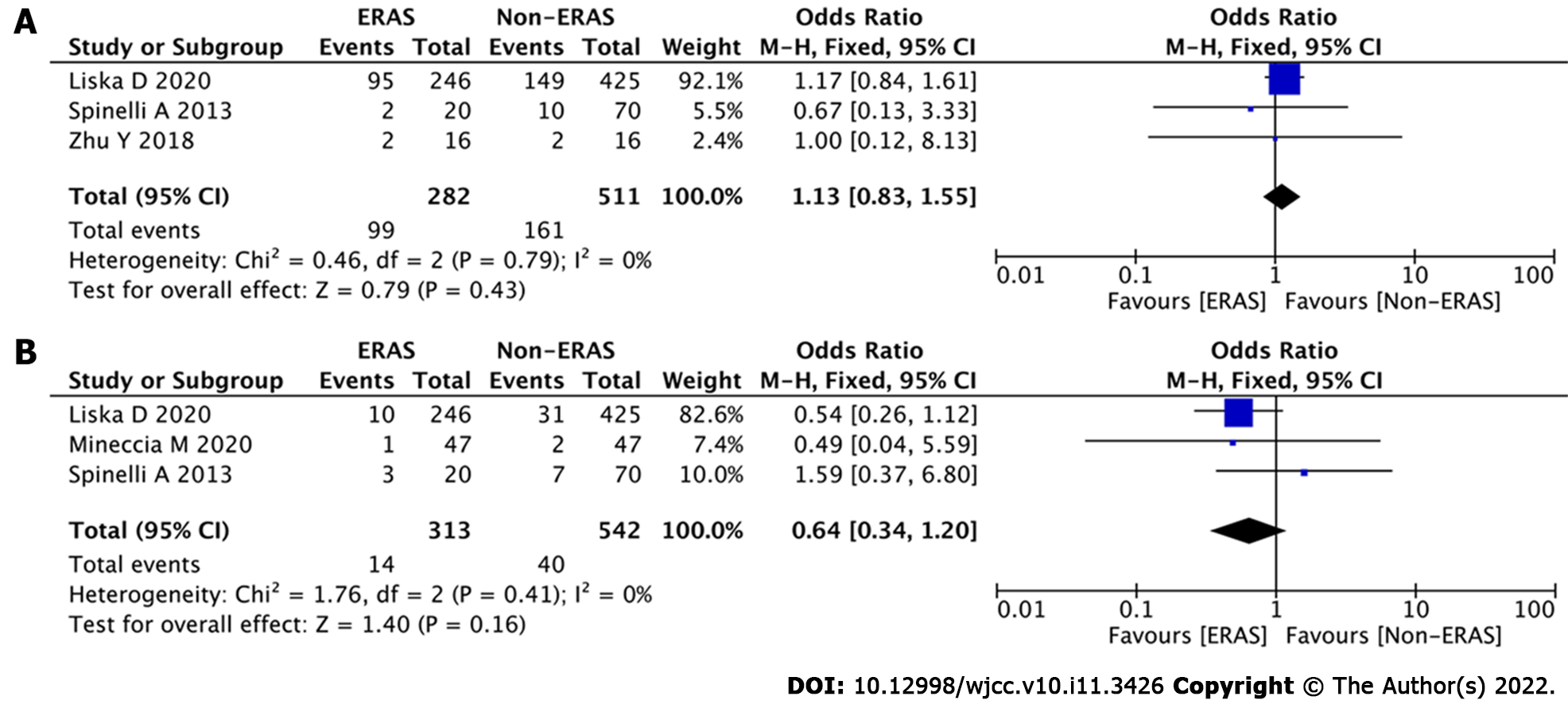
Data regarding overall complications were extracted from the eight studies. After pooling all of the data, no significance was found between the ERAS group and the non-ERAS group (OR = 0.82, 95%CI = 0.66 to 1.02, P = 0.08) (Figure 2). To analyze differences in minor and major complications, we conducted subgroup analysis. However, there were no significant differences between the ERAS group and the non-ERAS group in terms of minor complications (OR = 1.13, 95%CI = 0.83 to 1.55, P = 0.43) (Figure 3A) or major complications (OR = 0.64, 95%CI = 0.34 to 1.20, P = 0.16) (Figure 3B).
Other surgical outcomes were compared between the two groups as well. After pooling all of the data, the ERAS group had less time to first flatus (MD = -2.03, 95%CI = -3.89 to -0.17, P = 0.03), less time to bowel movement (MD = -1.08, 95%CI = -1.60 to -0.57, P < 0.01), less anastomotic fistula (OR = 0.36, 95%CI = 0.13 to 0.95, P = 0.04) and less postoperative hospital stay (MD = -1.99, 95%CI = -3.27 to -0.71, P < 0.01) than the non-ERAS group. However, no significant difference was found in operation time (MD = -0.17, 95%CI = -23.45 to 23.10, P = 0.99), bleeding (OR = 1.16, 95%CI = 0.48 to 2.76, P = 0.75) or readmission rate (OR = 0.72, 95%CI = 0.51 to 1.00, P = 0.05) (Table 2).
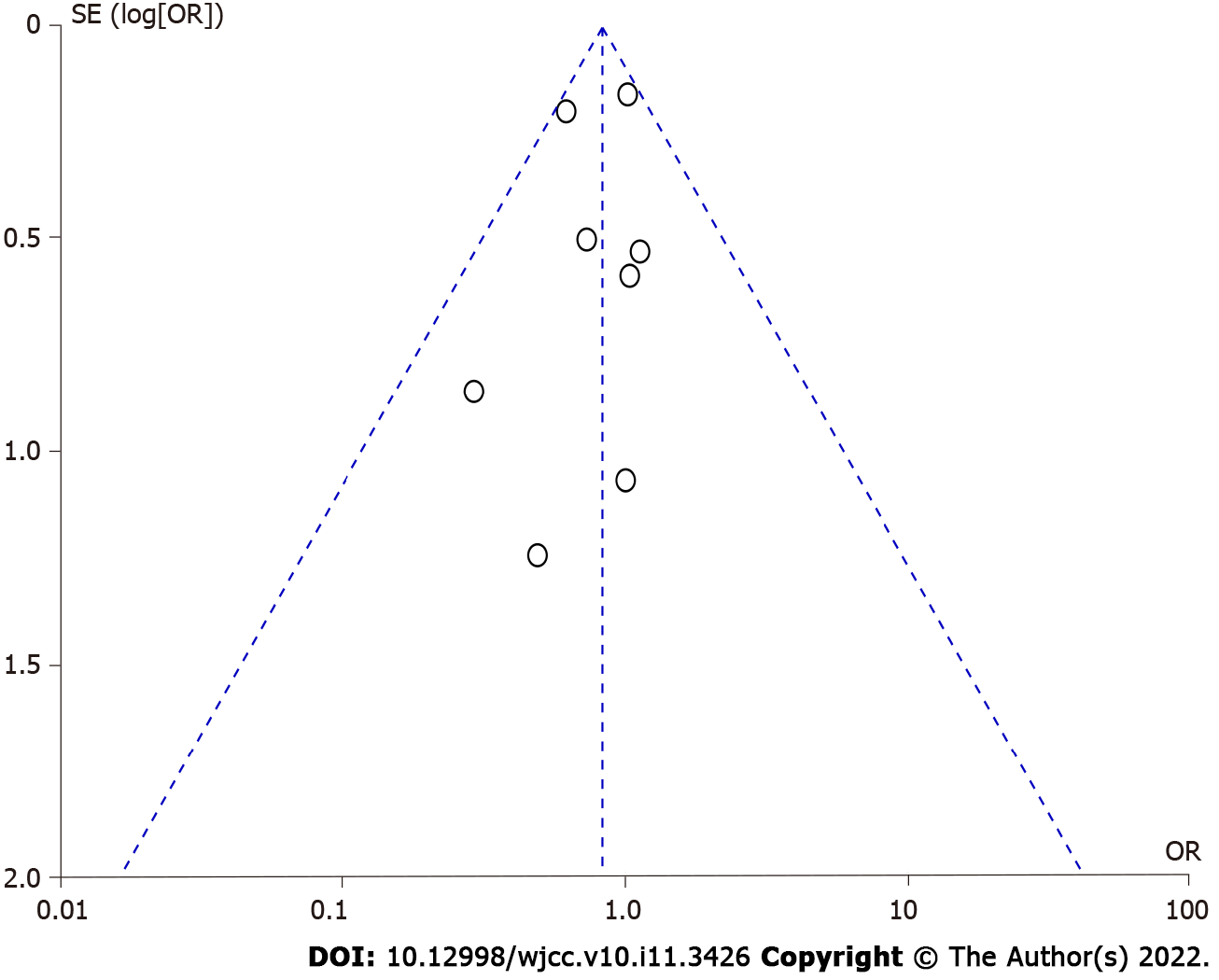
Repeated meta-analysis was performed by excluding one study at a time, and the exclusion of any one study did not significantly alter the results. Publication bias for the included studies was based on a visual inspection of the funnel plot. The funnel plot was symmetrical, and no obvious publication bias was found (Figure 4).
A total of eight studies with 1939 patients were included in this meta-analysis. There were no differences between the ERAS group and the non-ERAS group regarding baseline information. After pooling all of the data, no significance was found between the ERAS group and the non-ERAS group in terms of postoperative complications. However, the ERAS group had a lower prevalence of anastomotic fistula, less time to first flatus, less time to bowel movement and shorter postoperative hospital stays than the non-ERAS group.
IBD patients were at a higher risk of complications due to frequent malnutrition, immunosuppression, intra-abdominal abscess, anemia, fistula and intestinal obstruction than patients without IBD[27]. IBD patients who underwent surgery were more likely to have longer hospital stay, increased postoperative wound infections and higher readmission rates[15,31]. Furthermore, a longer pain relief time and a higher incidence of postoperative intestinal obstruction occurred in IBD patients[15]. Therefore, the ERAS protocol seemed to be a challenging task in IBD patients.
In this meta-analysis, we observed that no significance was found between the ERAS group and the non-ERAS group in terms of postoperative complications, and the results were similar to those of previous studies[24-26]. ERAS did not increase the complications after IBD surgery, so ERAS was considered a safe protocol. On the other hand, the ERAS group had a lower likelihood of anastomotic fistula, less time to first flatus, less time to bowel movement and shorter postoperative hospital stays than the non-ERAS group. ERAS might be an effective protocol after IBD surgery. The reduction in hospital stay brings cost savings and reduces the lost work time of family members, improves patient comfort and reduces exposure to hospital-acquired infections at the same time[17]. Moreover, the likelihood anastomotic fistula was significantly reduced in the ERAS group, which confirmed the safety of the ERAS protocol.
A reduction in hospital expenses in ERAS has been reported in other surgeries, including gastric cancer[7], colorectal cancer and esophagus cancer[9,10]. A previous study reported a reduction in hospital expenses; however, the number of studies was not sufficient to be included in this meta-analysis[28]. There was a lack of analgesic use, which required more follow-up studies confirming the beneficial details of ERAS.
A recent study reported that cancer patients undergoing laparoscopic surgery and ERAS treatment might have an immunological advantage[32]. Although no present studies evaluated the immune status of IBD patients undergoing the ERAS protocol, it is interesting to see whether similar benefits could be observed in the future. The success of ERAS depended on the patient's compliance and motivation, and this was important for IBD patients, who were mostly young and often had an active lifestyle[33,34]. Such preferred patients require rapid recovery in order to return to work and social activities quickly. It was also important to involve the patient's caregivers, as they could play an important role in identifying any signs and symptoms after the patient was discharged[24].
There were some certain limitations in the current meta-analysis. First, only eight studies (one RCT and seven non-RCTs) were included. Second, the number of subgroup analyses of time to first flatus, time to bowel movement, operation time and postoperative hospital stay were relatively small, therefore, the results were not robust, and larger studies are needed. Third, differences might occur between primary or recurrent IBD patients who underwent surgery, and furthermore, the outcomes might differ from CD and UC. Fourth, the use of steroids and biologics might affect the surgical outcomes. Therefore, multicenter, multiregional, prospective and high-quality RCTs should be carried out in the future.
In conclusion, ERAS was effective for the quicker recovery in IBD surgery and did not lead to increased complications.
To reduce surgical pressure and accelerate postoperative functional recovery, enhanced recovery after surgery (ERAS) has been recommended. Although the application of biologics in treating inflammatory bowel disease has changed treatment strategies, most patients with inflammatory bowel disease (IBD) still require surgery.
Many patients with IBD require surgery. The motivation of this meta-analysis was to examine the effect of ERAS in IBD surgery.
The aim of this meta-analysis was to evaluate the advantage of ERAS in IBD surgery.
The PubMed, EMBASE and Cochrane Library databases were searched from inception to March 21, 2021 to find eligible studies. The primary outcome was the postoperative complications. The secondary outcomes included operation time, time to first flatus, time to bowel movement, postoperative hospital stay and readmission.
A total of eight studies involving 1939 patients were included in this meta-analysis. There was no difference in baseline information between the ERAS group and the non-ERAS group. No significant difference was found between the ERAS group and the non-ERAS group in terms of postoperative overall complications. The ERAS group had a lower prevalence of anastomotic fistula, less time to first flatus, less time to bowel movement and shorter postoperative hospital stays than the non-ERAS group.
ERAS was effective for the quicker recovery in IBD surgery and did not lead to increased complications.
This meta-analysis provided a preliminary conclusion on the effect of ERAS in IBD surgery. Therefore, multicenter, multiregional, prospective and high-quality randomized controlled trials should be carried out in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Surlin VM, Romania S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1740] [Article Influence: 62.1] [Reference Citation Analysis (2)] |
| 2. | Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ. 2001;322:473-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 547] [Cited by in RCA: 539] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 3. | Lassen K, Soop M, Nygren J, Cox PB, Hendry PO, Spies C, von Meyenfeldt MF, Fearon KC, Revhaug A, Norderval S, Ljungqvist O, Lobo DN, Dejong CH; Enhanced Recovery After Surgery (ERAS) Group. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg. 2009;144:961-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 752] [Cited by in RCA: 799] [Article Influence: 49.9] [Reference Citation Analysis (0)] |
| 4. | Kehlet H. Fast-track colonic surgery: status and perspectives. Recent Results Cancer Res. 2005;165:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Ramírez JM, Blasco JA, Roig JV, Maeso-Martínez S, Casal JE, Esteban F, Lic DC; Spanish working group on fast track surgery. Enhanced recovery in colorectal surgery: a multicentre study. BMC Surg. 2011;11:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 6. | Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248:189-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1147] [Cited by in RCA: 1195] [Article Influence: 70.3] [Reference Citation Analysis (0)] |
| 7. | Wang LH, Zhu RF, Gao C, Wang SL, Shen LZ. Application of enhanced recovery after gastric cancer surgery: An updated meta-analysis. World J Gastroenterol. 2018;24:1562-1578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 54] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 8. | Jawahar K, Scarisbrick AA. Parental perceptions in pediatric cardiac fast-track surgery. AORN J. 2009;89:725-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Triantafyllou T, Olson MT, Theodorou D, Schizas D, Singhal S. Enhanced recovery pathways vs standard care pathways in esophageal cancer surgery: systematic review and meta-analysis. Esophagus. 2020;17:100-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 10. | Ni X, Jia D, Chen Y, Wang L, Suo J. Is the Enhanced Recovery After Surgery (ERAS) Program Effective and Safe in Laparoscopic Colorectal Cancer Surgery? J Gastrointest Surg. 2019;23:1502-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 11. | Milsom JW. Laparoscopic surgery in the treatment of Crohn's disease. Surg Clin North Am. 2005;85:25-34; vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Sokol H, Seksik P, Cosnes J. Complications and surgery in the inflammatory bowel diseases biological era. Curr Opin Gastroenterol. 2014;30:378-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Sica GS, Biancone L. Surgery for inflammatory bowel disease in the era of laparoscopy. World J Gastroenterol. 2013;19:2445-2448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 75] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (1)] |
| 14. | Aytac E, Stocchi L, Remzi FH, Kiran RP. Is laparoscopic surgery for recurrent Crohn's disease beneficial in patients with previous primary resection through midline laparotomy? Surg Endosc. 2012;26:3552-3556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Dai X, Ge X, Yang J, Zhang T, Xie T, Gao W, Gong J, Zhu W. Increased incidence of prolonged ileus after colectomy for inflammatory bowel diseases under ERAS protocol: a cohort analysis. J Surg Res. 2017;212:86-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Meunier A, Sorce G, Hardy PY, Coimbra C, Decker E, Joris J. Comparison of outcome after right colectomy with an enhanced recovery programme in patients with inflammatory bowel disease and patients operated on for other conditions: a monocentric retrospective study. Int J Colorectal Dis. 2021;36:757-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Grass F, Zhu E, Brunel C, Hübner M, Schoepfer A, Demartines N, Hahnloser D. Crohn's versus Cancer: Comparison of Functional and Surgical Outcomes after Right-Sided Resections. Dig Dis. 2021;39:106-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | McInnes MDF, Moher D, Thombs BD, McGrath TA, Bossuyt PM; and the PRISMA-DTA Group, Clifford T, Cohen JF, Deeks JJ, Gatsonis C, Hooft L, Hunt HA, Hyde CJ, Korevaar DA, Leeflang MMG, Macaskill P, Reitsma JB, Rodin R, Rutjes AWS, Salameh JP, Stevens A, Takwoingi Y, Tonelli M, Weeks L, Whiting P, Willis BH. Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: The PRISMA-DTA Statement. JAMA. 2018;319:388-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1683] [Cited by in RCA: 2069] [Article Influence: 295.6] [Reference Citation Analysis (0)] |
| 19. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24754] [Article Influence: 1178.8] [Reference Citation Analysis (0)] |
| 20. | Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8858] [Cited by in RCA: 12594] [Article Influence: 839.6] [Reference Citation Analysis (0)] |
| 21. | Wells GA, Shea BJ, O’Connell D, Peterson J, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2011. [cited November 1, 2011] Available from: https://www.researchgate.net/publication/261773681_The_Newcastle-Ottawa_Scale_NOS_for_Assessing_the_Quality_of_Non-Randomized_Studies_in_Meta-Analysis. |
| 22. | Ioannidis JP. Interpretation of tests of heterogeneity and bias in meta-analysis. J Eval Clin Pract. 2008;14:951-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 460] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 23. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46387] [Article Influence: 2108.5] [Reference Citation Analysis (3)] |
| 24. | Spinelli A, Bazzi P, Sacchi M, Danese S, Fiorino G, Malesci A, Gentilini L, Poggioli G, Montorsi M. Short-term outcomes of laparoscopy combined with enhanced recovery pathway after ileocecal resection for Crohn's disease: a case-matched analysis. J Gastrointest Surg. 2013;17:126-32; discussion p.132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 25. | Mineccia M, Menonna F, Germani P, Gentile V, Massucco P, Rocca R, Ferrero A. A retrospective study on efficacy of the ERAS protocol in patients undergoing surgery for Crohn disease: A propensity score analysis. Dig Liver Dis. 2020;52:625-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Liska D, Bora Cengiz T, Novello M, Aiello A, Stocchi L, Hull TL, Steele SR, Delaney CP, Holubar SD. Do Patients With Inflammatory Bowel Disease Benefit from an Enhanced Recovery Pathway? Inflamm Bowel Dis. 2020;26:476-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 27. | D'Andrea AP, Khetan P, Miller R, Sylla P, Divino CM. Outcomes After Bowel Resection for Inflammatory Bowel Disease in the Era of Surgical Care Bundles and Enhanced Recovery. J Gastrointest Surg. 2020;24:123-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 28. | Zhu Y, Xiang J, Liu W, Cao Q, Zhou W. Laparoscopy Combined with Enhanced Recovery Pathway in Ileocecal Resection for Crohn's Disease: A Randomized Study. Gastroenterol Res Pract. 2018;2018:9648674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 29. | Vrecenak JD, Mattei P. Fast-track management is safe and effective after bowel resection in children with Crohn's disease. J Pediatr Surg. 2014;49:99-102; discussion 102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 30. | West MA, Horwood JF, Staves S, Jones C, Goulden MR, Minford J, Lamont G, Baillie CT, Rooney PS. Potential benefits of fast-track concepts in paediatric colorectal surgery. J Pediatr Surg. 2013;48:1924-1930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Ban KA, Berian JR, Liu JB, Ko CY, Feldman LS, Thacker JKM. Effect of Diagnosis on Outcomes in the Setting of Enhanced Recovery Protocols. Dis Colon Rectum. 2018;61:847-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 32. | Veenhof AA, Vlug MS, van der Pas MH, Sietses C, van der Peet DL, de Lange-de Klerk ES, Bonjer HJ, Bemelman WA, Cuesta MA. Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg. 2012;255:216-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 246] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 33. | Feroci F, Kröning KC, Lenzi E, Moraldi L, Borrelli A, Scatizzi M. [The development of a fast track surgery program after laparoscopic colonic surgery in a General Surgery Unit]. Minerva Chir. 2010;65:127-136. [PubMed] |
| 34. | Ahmed J, Khan S, Lim M, Chandrasekaran TV, MacFie J. Enhanced recovery after surgery protocols - compliance and variations in practice during routine colorectal surgery. Colorectal Dis. 2012;14:1045-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 138] [Article Influence: 10.6] [Reference Citation Analysis (1)] |