Published online Apr 6, 2022. doi: 10.12998/wjcc.v10.i10.3194
Peer-review started: August 28, 2021
First decision: November 17, 2021
Revised: November 22, 2021
Accepted: February 22, 2022
Article in press: February 22, 2022
Published online: April 6, 2022
Processing time: 213 Days and 6.4 Hours
An intrauterine device (IUD) is a commonly used contraceptive among women in China. It is widely used because it is safe, effective, simple, economic, and reversible. Among the possible complications, an ectopic IUD in the bladder is rare. It occurs insidiously, has a long course, is associated with a high risk for injury, and is difficult to treat.
A 44-year-old woman was admitted for repeated episodes of urinary frequency, urgency, and dysuria over three months. Laboratory tests revealed significantly elevated urine leukocytes and bacteria. Urine culture suggested colonization with Enterococcus faecalis. Abdominal computed tomography images suggested an abnormally positioned IUD that was protruding into the bladder. Cystoscopy revealed a metallic foreign body with multiple stones on its surface in the left posterior bladder wall. The foreign body measured approximately 1 cm. Hysteroscopy revealed the arm of a V-type metal IUD embedded in the middle and upper sections of the anterior wall of the cervical canal. The majority of the IUD was located in the uterine cavity. Cystoscopy was performed, and a holmium laser was utilized to break the stones attached to the portion of the IUD in the bladder. The IUD was then removed through hysteroscopy.
Ectopic IUDs in the bladder can be diagnosed with thorough imaging and safely removed through cystoscopy or hysteroscopy.
Core Tip: The intrauterine device (IUD) is a commonly used method of birth control, and its displacement into the bladder is very rare. A patient was diagnosed with an ectopic IUD in the bladder after undergoing clinical and radiologic examinations. When patients of childbearing age present with recurrent hematuria, urinary tract infections, and have a history of IUD insertion, an ectopic IUD should be considered.
- Citation: Yu HT, Chen Y, Xie YP, Gan TB, Gou X. Ectopic intrauterine device in the bladder causing cystolithiasis: A case report. World J Clin Cases 2022; 10(10): 3194-3199
- URL: https://www.wjgnet.com/2307-8960/full/v10/i10/3194.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i10.3194
According to the 1998 annual report of the World Health Organization, intrauterine devices (IUDs) are a cost-effective, reversible contraceptive method. They are commonly used worldwide and are the main contraceptive method among Chinese women[1]. According to statistics, the incidence of IUD displacement is approximately 0.1%-0.3%[2]. The spontaneous displacement of an IUD into the peri-uterine area may cause serious complications, such as vesicouterine fistulas, intestinal perforation, hydronephrosis, and even renal failure[3-7]. Intravesical translocation of an IUD is rare and may present as suprapubic pain or discomfort, dysuria, recurrent urinary tract infections, or stone formation. Removal through endoscopy or open surgery is currently recommended as the best treatment option. Herein, we report a case of a patient who presented with recurrent urinary tract infections and was incidentally found to have an IUD partially positioned in the bladder through computed tomography (CT).
The primary complaints included urinary frequency, urgency, and pain over a period of three months.
A 44-year-old woman was hospitalized in our department for a 3-mo history of urinary frequency, urgency, and pain. She denied fever, lumbago, back pain, and hematuria.
The patient had no contributory medical history, except for an IUD implantation seven years prior.
The patient had no pertinent family history.
No obvious signs were found on physical examination. The patient did not demonstrate any pain on percussion of the bilateral renal areas or obvious tenderness along the path of the ureters. The patient exhibited normal external genitalia.
A routine urinary examination was performed when the patient first developed symptoms. The examination results were as follows: 844 red blood cells/uL, 1063 white blood cells/uL, and 1873 bacteria/uL. She was treated with antibiotics; however, after 3 mo, another routine urine analysis demonstrated 131 red blood cells/uL, 330 white blood cells/uL, and 432 bacteria/uL. After she was hospitalized, her urine test showed 3 red blood cells/uL, 25 white blood cells/uL, and 5 bacteria/uL. A urine culture demonstrated colonization with Enterococcus faecalis.
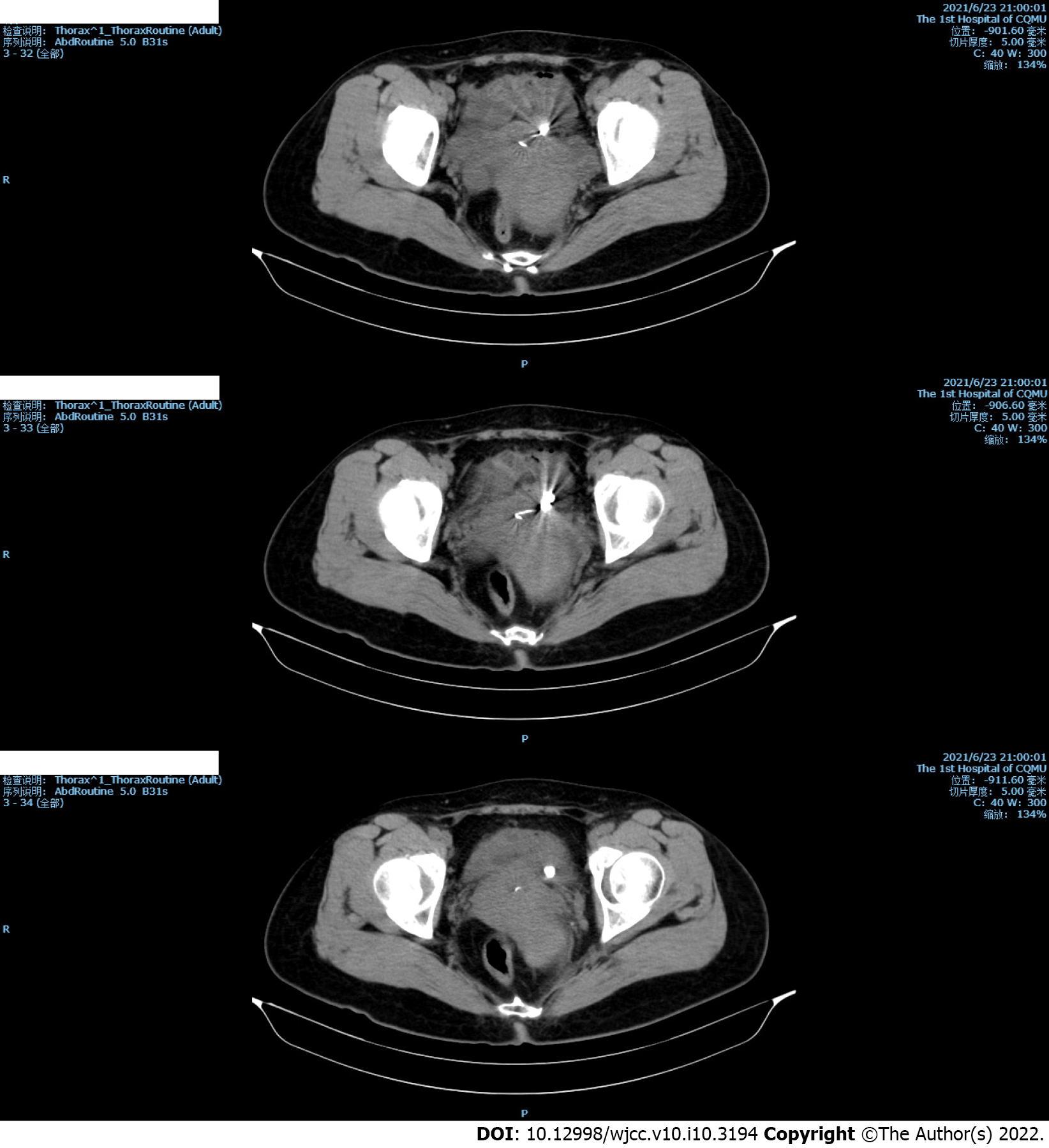
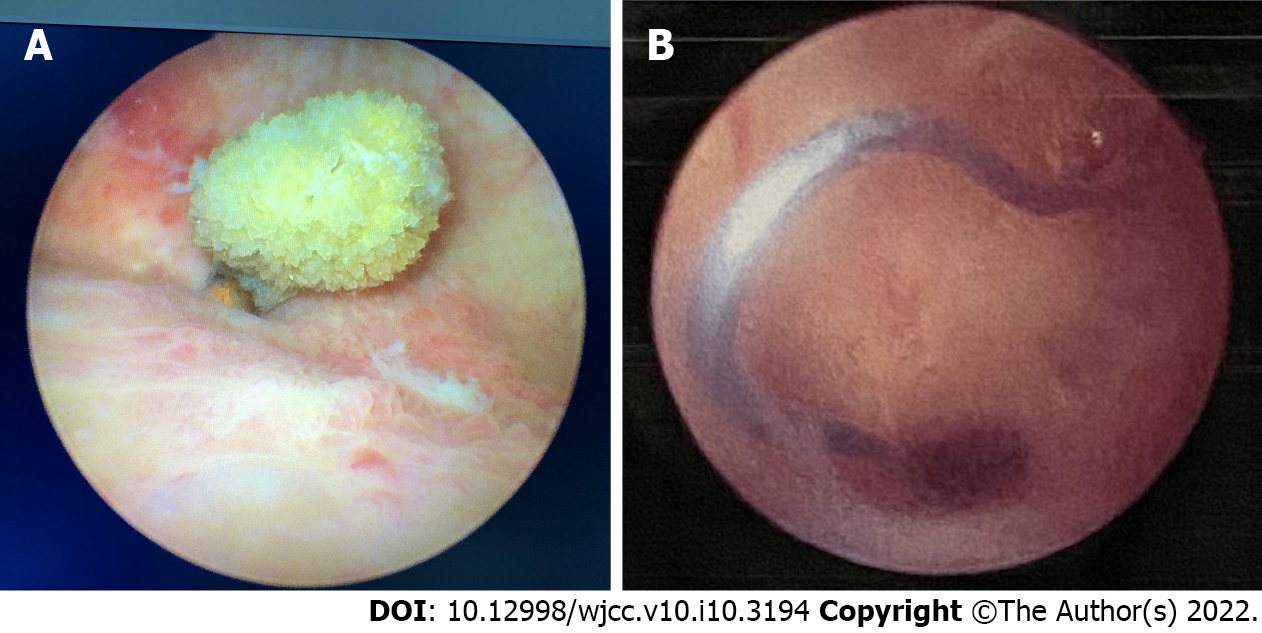
The patient had recurring symptoms of urinary tract infection. Combined with her history of IUD implantation, we considered IUD displacement. CT revealed an abnormally positioned IUD, which had penetrated the uterine wall and was protruding forward into the bladder (Figure 1). Cystoscopic and hysteroscopic exploration was subsequently scheduled. Cystoscopy was performed with a 22-Fr cystoscope with a 70° lens. Cystoscopy demonstrated an IUD, which had penetrated the left posterior bladder wall. Approximately 1 cm of the IUD was located in the bladder cavity, and a large number of stones were visible on its surface (Figure 2A). Subsequently, hysteroscopy demonstrated a V-shaped IUD in the middle section of the cervical canal. One of the arms of the IUD was notably incarcerated in the muscular layer of the canal (Figure 2B).
Considering the patient’s history and laboratory and imaging findings, the patient was diagnosed with an ectopic IUD.
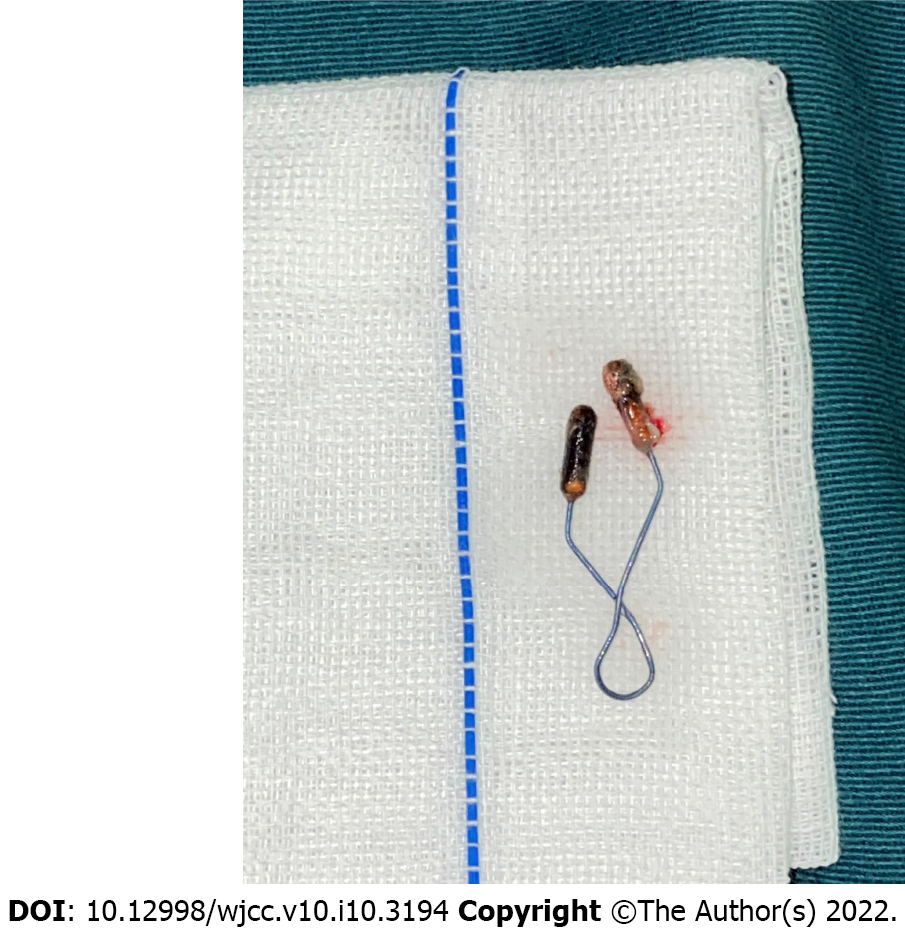
We administered cefoxitin (2 g intravenously every 8 h) based on the patient’s urine culture results and drug sensitivity test. CT, cystoscopy, and hysteroscopy demonstrated that majority of the IUD was located in the uterine cavity; however, the portion of the IUD in the bladder was complicated due to multiple stones. Thus, we decided to use a holmium laser (Lumenis, Holmium 1.0 J × 20 Hz) to break the stones during cystoscopy and removed the ectopic IUD from the uterine cavity with the hysteroscope (Figure 3). We reassessed the bladder and uterus at the end of the procedure and confirmed that there was no obvious bleeding or fistula.
The patient had no obvious hematuria or vaginal bleeding after surgery. The urinary catheter was removed after one week, and the patient's lower urinary tract symptoms showed complete resolution. A routine urine examination was performed after three months and demonstrated no obvious abnormalities.
As reported in the literature, IUDs are most commonly displaced into the omentum (26.7%), uterorectal depression (21.5%), colorectal cavity (10.4%), myometrium (7.4%), broad ligament (6.7%), or abdominal cavity (5.2%)[8]. The translocation of an IUD through uterine perforation and into the bladder wall is rare, with an incidence of approximately 0.05–1.3/1000[9]. Kart et al[10] reported 200 cases of ectopic IUDs, 90 of which were located in the bladder. Goldbach et al[11] reported a higher incidence of ectopic Multiload Cu375 (MCu) II functional IUDs compared to other IUDs. Sun et al[12] suggested that the MCu II IUD was similar to the V-type IUD as both have sharp side walls that easily distort when the device is handled or inserted incorrectly. The mechanism of IUD displacement is unclear but may be related to breastfeeding, the proximity of IUD implantation to recent delivery (up to 36 wk), surgeon’s experience and skill in implanting IUDs, or a history of cesarean section[13]. Esposito et al[14] proposed two mechanisms for IUD displacement, which included immediate perforation during insertion and a secondary process of gradual erosion.
Clinically, bladder injury caused by an IUD may present with dysuria, hematuria, and lower abdominal pain[15]. Most patients with IUDs have a medical history of urinary tract infections or hematuria for which they have received treatment. As reported, urinary tract infections are the most common manifestation of bladder perforation with an IUD. For patients with a history of IUD implantation, recurrent urinary tract infections or intermittent hematuria should increase the suspicion for an ectopic IUD. The diagnosis of an ectopic IUD in the bladder mainly depends on imaging examinations. B-mode ultrasonography can be utilized for screening, but a definitive diagnosis requires a CT, cystoscopy, or hysteroscopy. There is currently no standard surgical treatment for this condition. Displaced IUDs can be optimally managed through hysteroscopy, cystoscopy, laparoscopy, or a combination of these procedures, with the location of the ectopic IUD determining the treatment option[13,16-18]. A recent study proposed an innovative combination of carbon dioxide cystoscopy and laparoscopy for IUD removal with a partial cystectomy[17].
A review of the current literature indicated that patients with bladder stones caused by ectopic IUDs should undergo preoperative cystoscopy, hysteroscopy (or transvaginal ultrasound), and CT imaging to determine the location of the IUD and facilitate surgical planning[19]. In the present case, the V-type IUD was only displaced approximately 1 cm into the bladder. Cystolithiasis occurred in this short segment, but the majority of the IUD was still located in the uterine cavity. We elected to use a holmium laser to break the calculi on the portion of the IUD in the bladder, and then removed the IUD through the vagina.
In conclusion, we reported a case of an ectopic IUD in the bladder that was documented seven years after IUD insertion. Among women of childbearing age with a history of IUD placement, repeated lower urinary tract symptoms, and hematuria, an ectopic IUD in the bladder should be considered. Ultrasound or CT can be used to confirm the diagnosis. Cystoscopy and hysteroscopy should be performed to guide surgical treatment. Removal of the ectopic IUD through the urethra or vagina is the least traumatic course.
We acknowledge the patient for her cooperation and trust in our treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ismail MAA, Qin DR S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Cheung ML, Rezai S, Jackman JM, Patel ND, Bernaba BZ, Hakimian O, Nuritdinova D, Turley CL, Mercado R, Takeshige T, Reddy SM, Fuller PN, Henderson CE. Retained Intrauterine Device (IUD): Triple Case Report and Review of the Literature. Case Rep Obstet Gynecol. 2018;2018:9362962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Nouioui MA, Taktak T, Mokadem S, Mediouni H, Khiari R, Ghozzi S. A Mislocated Intrauterine Device Migrating to the Urinary Bladder: An Uncommon Complication Leading to Stone Formation. Case Rep Urol. 2020;2020:2091915. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | El-Hefnawy AS, El-Nahas AR, Osman Y, Bazeed MA. Urinary complications of migrated intrauterine contraceptive device. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:241-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Karsmakers R, Weis-Potters AE, Buijs G, Joustra EB. Chronic kidney disease after vesico-vaginal stone formation around a migrated intrauterine device. BMJ Case Rep. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Madden A, Aslam A, Nusrat NB. A Case of Migrating "Saf-T-Coil" Presenting With a Vesicovaginal Fistula and Vesicovaginal Calculus. Urol Case Rep. 2016;7:17-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Wang L, Li Y, Zhao XP, Zhang WH, Bai W, He YG. Hydronephrosis caused by intrauterine contraceptive device migration: three case reports with literature review. Clin Exp Obstet Gynecol. 2017;44:301-304. [PubMed] |
| 7. | Toumi O, Ammar H, Ghdira A, Chhaidar A, Trimech W, Gupta R, Salem R, Saad J, Korbi I, Nasr M, Noomen F, Golli M, Zouari K. Pelvic abscess complicating sigmoid colon perforation by migrating intrauterine device: A case report and review of the literature. Int J Surg Case Rep. 2018;42:60-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Gill RS, Mok D, Hudson M, Shi X, Birch DW, Karmali S. Laparoscopic removal of an intra-abdominal intrauterine device: case and systematic review. Contraception. 2012;85:15-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Heinberg EM, McCoy TW, Pasic R. The perforated intrauterine device: endoscopic retrieval. JSLS. 2008;12:97-100. [PubMed] |
| 10. | Kart M, Gülecen T, Üstüner M, Çiftçi S, Yavuz U, Özkürkçügil C. Intravesical Migration of Missed Intrauterine Device Associated with Stone Formation: A Case Report and Review of the Literature. Case Rep Urol. 2015;2015:581697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Goldbach AR, Hava S, Patel H, Khan M. IUD embedment in the fallopian tube: An unexpected location for a translocated IUD. Radiol Case Rep. 2018;13:788-792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Sun X, Xue M, Deng X, Lin Y, Tan Y, Wei X. Clinical characteristic and intraoperative findings of uterine perforation patients in using of intrauterine devices (IUDs). Gynecol Surg. 2018;15:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Uçar MG, Şanlıkan F, Ilhan TT, Göçmen A, Çelik Ç. Management of intra-abdominally translocated contraceptive devices, is surgery the only way to treat this problem? J Obstet Gynaecol. 2017;37:480-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Esposito JM, Zarou DM, Zarou GS. A Dalkon Shield imbedded in a myoma: case report of an unusual displacement of an intrauterine contraceptive device. Am J Obstet Gynecol. 1973;117:578-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Tosun M, Celik H, Yavuz E, Cetinkaya MB. Intravesical migration of an intrauterine device detected in a pregnant woman. Can Urol Assoc J. 2010;4:E141-E143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Liu L, Liu H, Zhang X. Intravesical migration of a Chinese intrauterine device and secondary stone formation: diagnostic investigation and laparoscopic management. Int Urogynecol J. 2015;26:1715-1716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Jin C, Fan Y, Zhang Q, Wang Y, Wu S, Jin J. Removal of foreign bodies embedded in the urinary bladder wall by a combination of laparoscopy and carbon dioxide cystoscopic assistance: Case report and literature review. Investig Clin Urol. 2016;57:449-452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Niu H, Zhang L, Yao S, Qu Q. Successful removal of an intrauterine device perforating the uterus and the bladder with the aid of a transurethral nephroscope. Int Urogynecol J. 2019;30:325-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Heinemann K, Reed S, Moehner S, Minh TD. Risk of uterine perforation with levonorgestrel-releasing and copper intrauterine devices in the European Active Surveillance Study on Intrauterine Devices. Contraception. 2015;91:274-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 112] [Article Influence: 11.2] [Reference Citation Analysis (0)] |