Published online Apr 6, 2022. doi: 10.12998/wjcc.v10.i10.3143
Peer-review started: August 13, 2021
First decision: October 20, 2021
Revised: November 2, 2021
Accepted: January 25, 2022
Article in press: January 25, 2022
Published online: April 6, 2022
Processing time: 228 Days and 3.5 Hours
Annually, there are an estimated 1187000 new patients worldwide diagnosed with haematological malignancies. Effective strategies are needed to alleviate side effects and prevent the physical and psychosocial degeneration of patients in active treatment for haematological malignancies.
To explore the effects of physical exercise on quality of life (QoL) of patients with haematological malignancies and thrombocytopenia.
Cochrane Library, PubMed and Embase were searched for all relevant articles reporting randomized controlled trials (RCTs) that were published up to 31 July 2021. Two authors independently selected articles in accordance with the inclusion criteria, evaluated their quality, and collected information. Any controversy was resolved through discussion with a third senior author. The PRISMA 2009 checklist was followed.
Seven RCTs were selected in the systematic review and three were included in the final meta-analysis. There were significant differences in QoL between physical exercise groups [mean score difference = 8.81; 95% confidence interval (CI): 1.81-15.81, P = 0.01], especially in emotional functioning (mean score difference = 12.34; 95%CI: 4.64-20.04, P = 0.002) and pain (mean score difference = –12.77; 95%CI: -3.91 to -21.63, P = 0.005).
Physical exercise has clinical effects on QoL and improves emotional function and pain indices of patients with haematological malignancies and thrombocytopenia.
Core Tip: Effective strategies are needed to alleviate side effects and prevent the physical and psychosocial degeneration of patients in active treatment for haematological malignancies. This meta-analysis examined the effects of physical exercise on quality of life (QoL) of patients with haematological malignancies and thrombocytopenia. The results indicated that physical exercise improves the QoL of these patients, especially in terms of emotional functioning and pain management.
- Citation: Yang YP, Pan SJ, Qiu SL, Tung TH. Effects of physical exercise on the quality-of-life of patients with haematological malignancies and thrombocytopenia: A systematic review and meta-analysis. World J Clin Cases 2022; 10(10): 3143-3155
- URL: https://www.wjgnet.com/2307-8960/full/v10/i10/3143.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i10.3143
Annually, there are an estimated 1187000 new patients worldwide diagnosed with haematological malignancies, including leukaemia, myeloma, and lymphoma, resulting in 690000 deaths[1]. The main treatments for haematological malignancies include chemotherapy, immunotherapy, and autologous or allogeneic stem cell transplantation[2]. The combination of the primary disease and the direct side effects exerted by high-dose chemotherapy may lead to a decrease in physical exercise[3]. Repeated treatments for the disease, hospitalisation, and prolonged immobility can produce adverse effects including a lack of energy, whole body muscle weakness, physical de-conditioning, fatigue, and increased psychological stress, reducing health-related quality of life (HRQoL)[4-6]. Effective strategies are needed to alleviate side effects and prevent the physical and psychosocial degeneration of patients in active treatment for haematological malignancies[7].
Physical exercise has been indicated to be the most promising and effective rehabilitation strategy for cancer patients[8-10]. Systematic reviews reported that physical exercise can positively impact the muscle strength and HRQoL of cancer patients[11-15]. Exercise not only effectively improves the QoL and physical functions of patients with different demographic and clinical characteristics[13], but can mitigate fatigue, pain, insomnia, and dyspnoea in cancer patients[15]. It has been found that exercise does not have a beneficial effect in relation to complaints of nausea/vomiting, loss of appetite, astriction, and diarrhoea[15].
There are positive effects exerted by physical exercise on patients with haematological malignancy, whereas consistent evidence supporting the administration of physical exercise in patients with a haematological malignancy and thrombocytopenia is lacking[16-20]. It has been proposed that exercise reduces the risk of cerebral, intramuscular and joint haemorrhage in deeply thrombocytopenic patients[21]. The prevailing advice for haematological malignancy patients is to rest and sleep more, especially if they have thrombocytopenia, and to avoid intensive and high-energy physical activity, without taking note of the negative effects such as thromboembolic diseases, pressure ulcers, deconditioning, contractures, fatigue, and atelectasis[22]. Some other studies have not indicated clear findings in relation to this advice[21,23,24].
This study aimed to examine the effects of physical exercise on the QoL of haematological malignancy patients with thrombocytopenia, and to provide an evidence-based medical basis for the application and promotion of physical exercise.
This study was conducted using randomized controlled trials (RCTs) to assess the effect of physical exercise on the QoL of haematological malignancy patients with thrombocytopenia. We complied with the checklist of PRISMA[25]. The protocol was registered in the PROSPERO International Prospective Register of Systematic Review (number: CRD42021256897). We searched PubMed, Cochrane Library and Embase databases for all relevant articles published up to 31 July 2021. The literature search strategy included a mix of MeSH and free-text terms associated with the key concepts of haematological malignancy, physical exercise intervention, and QoL (Table 1). No limitations were imposed regarding the written language used.
| Search strategy in Pubmed | Similar search run in Cochrane Library and EMBASE |
| Hematologic malignancy | Title/Abstract |
| Hematologic malignancies | Title/Abstract |
| Hematological malignancy | Title/Abstract |
| Hematological malignancies | Title/Abstract |
| Hematopoietic malignancies | Title/Abstract |
| Hematopoietic malignancy | Title/Abstract |
| Haematological cancer | Title/Abstract |
| Hematologic cancer | Title/Abstract |
| Hematopoietic cancer | Title/Abstract |
| Leukaemia | Title/Abstract |
| Leukemia | Title/Abstract |
| Myeloma | Title/Abstract |
| Lymphoma | Title/Abstract |
| Hematopoietic stem cell transplantation | Title/Abstract |
| 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 | |
| Aerobic exercises | All fields |
| Resistance exercises | All fields |
| Physical exercises | All fields |
| Exercise intervention | All fields |
| Physical activity | All fields |
| 16 OR 17 OR 18 OR 19 OR 20 | |
| Quality of life | Title/Abstract |
| 15 AND 21 AND 22 |
Research articles were selected if the following criteria were met: (1) Study design was an RCT; (2) Experimental and control groups were diagnosed with haematological malignancies (patient age ≥ 18 years); (3) Physical exercise was the main intervention for the experimental group, and various physical activities designed to improve patient QoL were included; and (4) Patients underwent chemotherapy and had thrombocytopenia during the exercise intervention period. Articles were excluded if: (1) No original data were included; and (2) Physical exercise intervention was discontinued if patients had a platelet count > 20000/μL without active bleeding, severe anaemia, fever, infections or diarrhoea, or if there was no mention of platelet counts.
Two independent authors (Yang YP and Pan SJ) selected the relevant articles based on the inclusion criteria. The study type, study subject and intervention measures were assessed, and eligible studies were included after evaluating the full text. Detailed information was examined from the literature to perform the meta-analysis, and any disagreements that arose were discussed with a third senior author (Tung TH). Basic literature parameters (first author, year of publication and country, study group assignment, randomization for subjects, types of participants, intervention period, outcome, and measurements) were extracted by two independent authors and cross-checked.
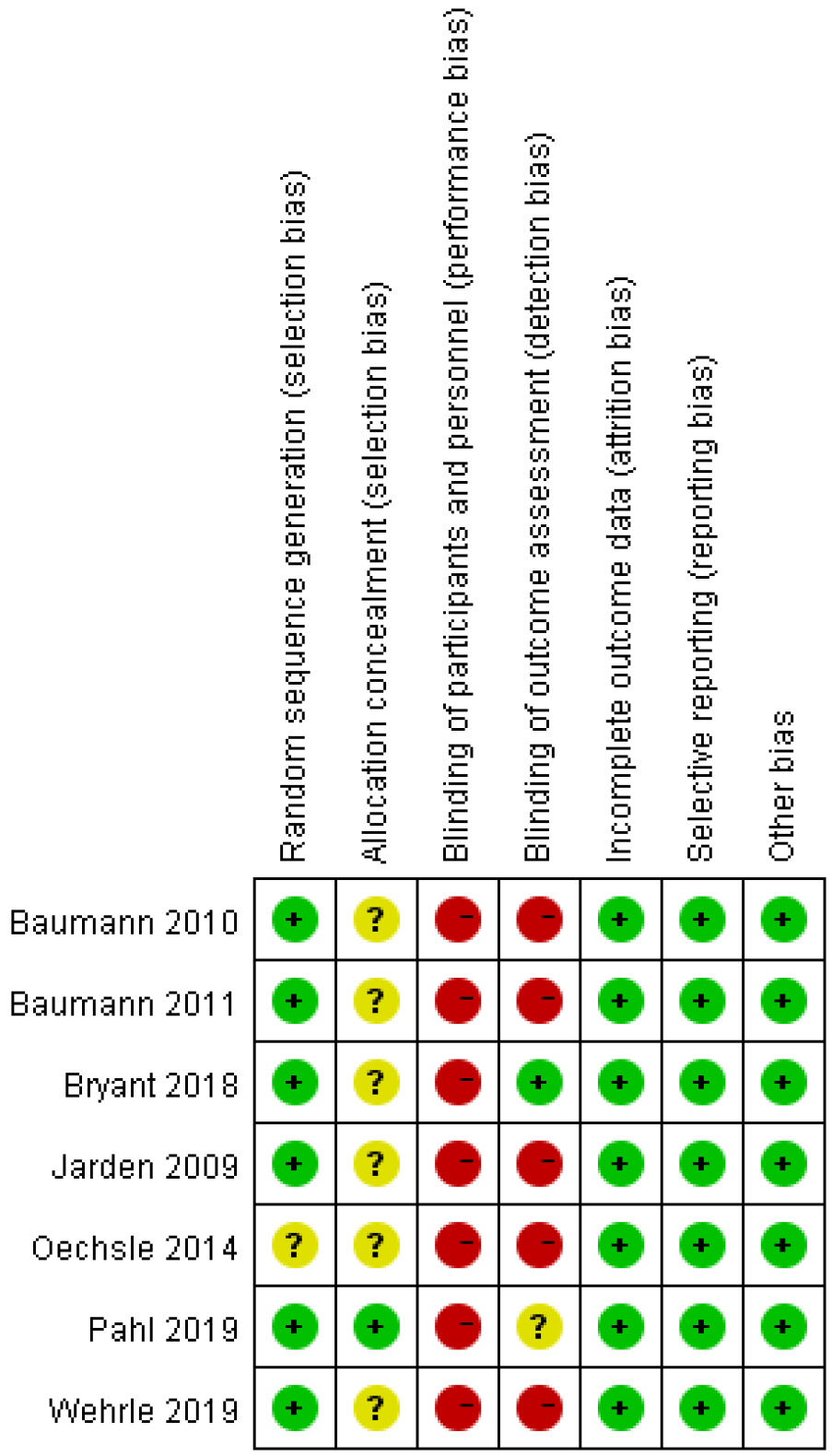
Two authors applied the Cochrane Collaboration Tool to examine the quality of selected articles[26]. The risk assessment tool included selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias. For each domain the bias ratings were low risk, high risk, or unclear risk, according to whether the specific domain was shown.
We used Review Manager version 5.3[27] to calculate the overall effect exerted by physical exercise on QoL for haematological malignancy patients with thrombocytopenia. In the calculation of continuous data, weighted mean differences of 95% confidence intervals (CIs) were used for each trial. In addition, we assessed heterogeneity using the X2 test and assessed the magnitude of the heterogeneity using the I2statistic. Heterogeneity in a meta-analysis refers to the variation in study outcomes between articles. We used a fixed-effect model when I2was no more than 50%.
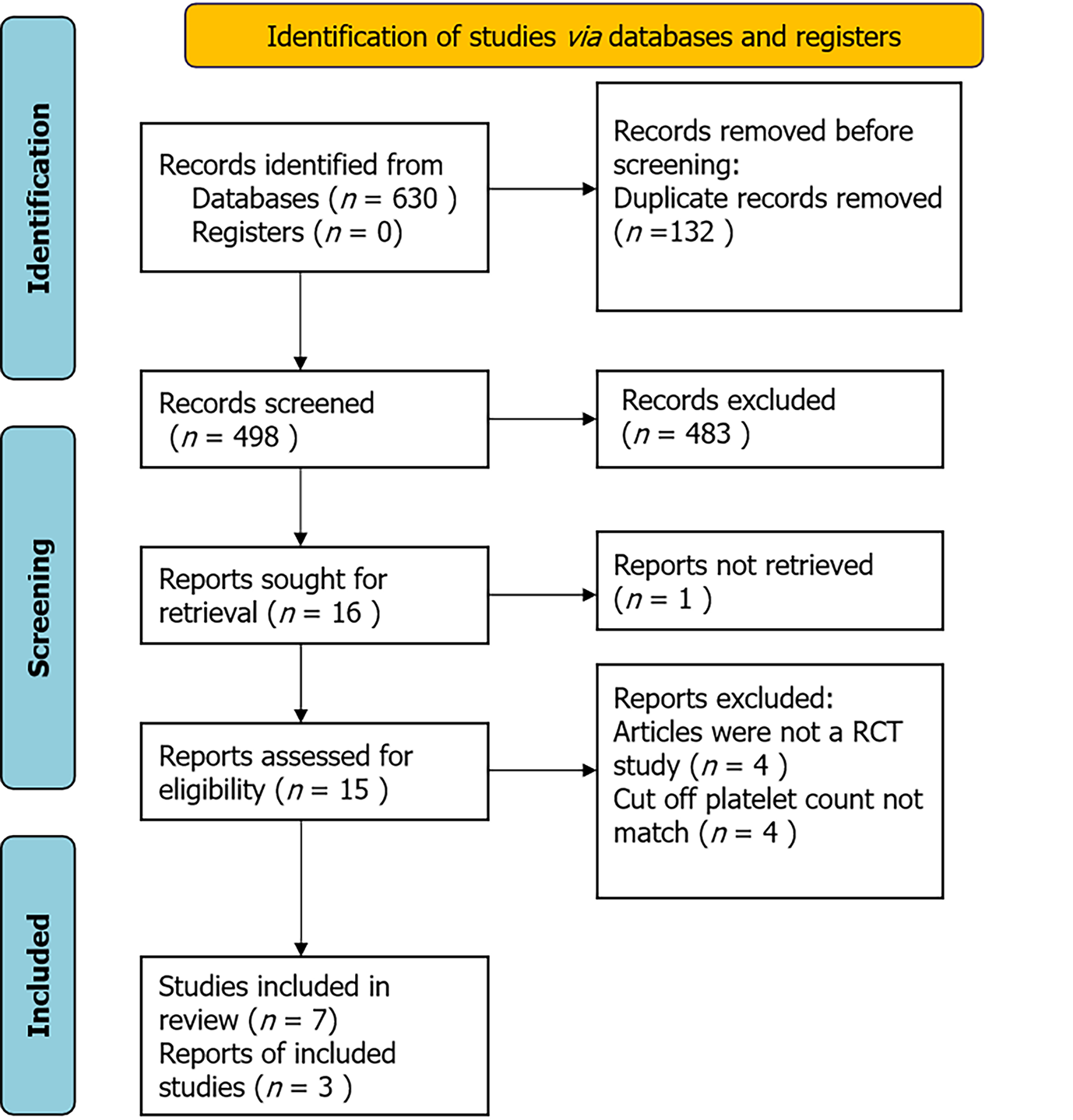
A total of 630 references were acquired from the Cochrane Library, PubMed and Embase databases and we discarded 132 duplicate publications. After reviewing the abstracts, 15 articles were reviewed in full. Of those, four non-RCTS were excluded. The other four papers were also excluded, in which exercise sessions were suspended in patients with platelets < 50000/μL and < 80000/μL without any abnormal clinical symptoms, which had strongly influenced their attendance during the exercises intervention and might have led to an underestimation of the effects of physical exercise on the QoL. At the end of the screening procedure, seven papers reporting on RCTs met the inclusion criteria[28-33]. The PRISMA flow diagram shows the article screening process (Figure 1).
A total of 121 patients were assigned to the intervention group and 121 to the control group. The references we included were published as full texts and we summarize the baseline information and provide it in Table 2. The timing of exercise intervention was mainly when patients were undergoing haematopoietic stell cell transplantation (HSCT) and during chemotherapy. The exercise conducted in the intervention group in the RCTs included aerobic, resistance and stretching exercise, as well as body vibration training[28-34]. In one RCT, aerobic and resistance exercise programmes were performed in two different groups, and the data from both groups were extracted and analyzed separately[33]. Participants recruited in this arm of the review were adults with haematological malignancy patients at various disease stages who also had thrombocytopenia. Five of the articles were conducted in Germany[29-31,33,34], and one each in the United States[32], and Denmark[28].
| Ref. | Year | Country | Assigned group | Randomly assigned participants (N) | Types of any participants | Intervention time | Outcomes |
| Jarden et al[28] | 2009 | Copenhagen | Control: Eoutine care | 16 | Adult patients scheduled for a myeloablative allo-HSCT platelets > 20 × 109/L | 6 mo | Quality of life (EORTC QLQ-C30): (1) At 3 mo, case (65.1 ± 15.9) vs control (51.9 ± 20.2); P = 0.841; (2) At 6 mo, case (72.8 ± 20.0) vs control (58.3 ± 21.5); P = 0.603 |
| Experimental: Stretching exercises; resistance training; relaxation and psychoeducation | 13 | ||||||
| Baumann et al[29] | 2010 | Germany | Control: Routine care | 25 | Adult patients with the indication of an HSCT platelets > 30 × 109/L | The entire hospitalization phase | Quality of life (EORTC QLQ-C30): Case (61.2 ± 22.8) vs control (61.7 ± 22.1); P = 0.926 |
| Experimental: Aerobic endurance, training and ADL-training | 24 | ||||||
| Baumann et al[30] | 2011 | Germany | Control: Routine care | 16 | Adult patients undergoing an allo-HSCT platelets > 10 × 109/L | The whole inpatient time | Quality of life (EORTC QLQ-C30): Case (68.6± 11.2) vs control (56.3 ± 17.6) |
| Experimental: Aerobic endurance, training and ADL-training, interval training, resistance training | 17 | ||||||
| Oechsle et al[31] | 2014 | Germany | Control: Routine care | 24 | Adult patients with acute myeloid leukemia platelets > 20 × 109/L | During the hospitalization 21 d (range: 16-33 d) | Quality of life (EORTC QLQ-C30): Case 50 vs control 50. P = 0.66 |
| Experimental: Endurance training, resistance exercises | 24 | ||||||
| Bryant et al[32] | 2018 | United States | Control: Routine care | 9 | Adult newly diagnosed with acute leukemia platelets > 10 × 109/L | During the hospitalization | PROMIS short form measures, self-reported measures of HRQOL |
| Experimental:Aerobic training, resistance training | 8 | ||||||
| Wehrle et al[33] | 2019 | Germany | Control: Routine care | 8 | Adult patients diagnosed with AL platelets > 10 × 109/L | During induction chemotherapy | Quality of life (EORTC QLQ-C30): Case 1 62.5 (45.8-70.8) case 2 50.0 (33.3-58.3); vs control 66.7 (45.8-66.7) |
| Experimental 1: Aerobic training | 8 | ||||||
| Experimental 2: Resistance training | 6 | ||||||
| Pahl et al[34] | 2020 | Germany | Control: Routine care | 23 | Adult patients during allo-HSCT, platelets > 20 × 109/L | During the hospitalization | After hospitalization, CG patients reported reduced QoL (P = 0.015), IG’s QoL remained unchanged |
Figure 2 shows the assessments of the risk of bias of the articles included by the Cochrane Collaboration Tool. All seven articles lacked a description of how selection bias was prevented during from the allocation sequence. Six of the trials failed to clearly indicate whether patients were blinded, since it was not feasible to blind the patients when they were conducting physical exercise. A low quality of evidence was reached for the results of QoL due to the lack of blinding of study participants and outcome evaluations, and the allocation concealment. However, in respect of blinding, it is inappropriate to blind the physical exercise intervention group and their teachers.
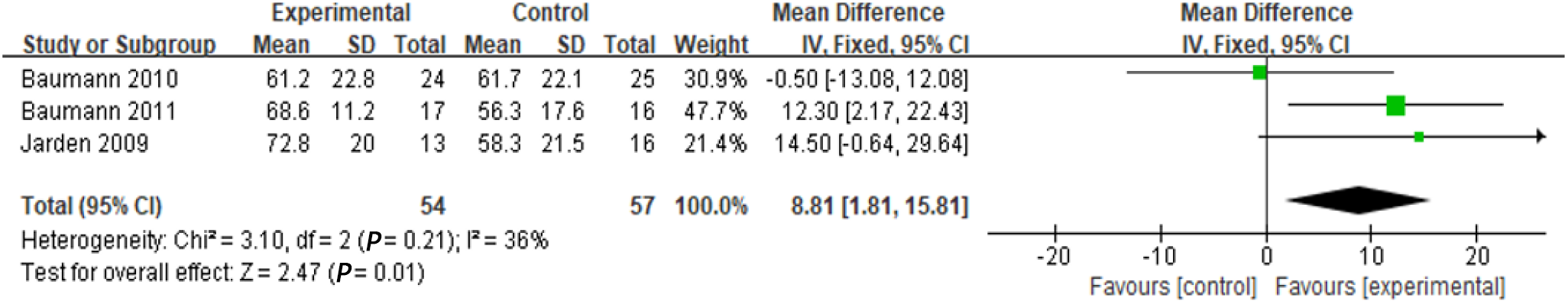
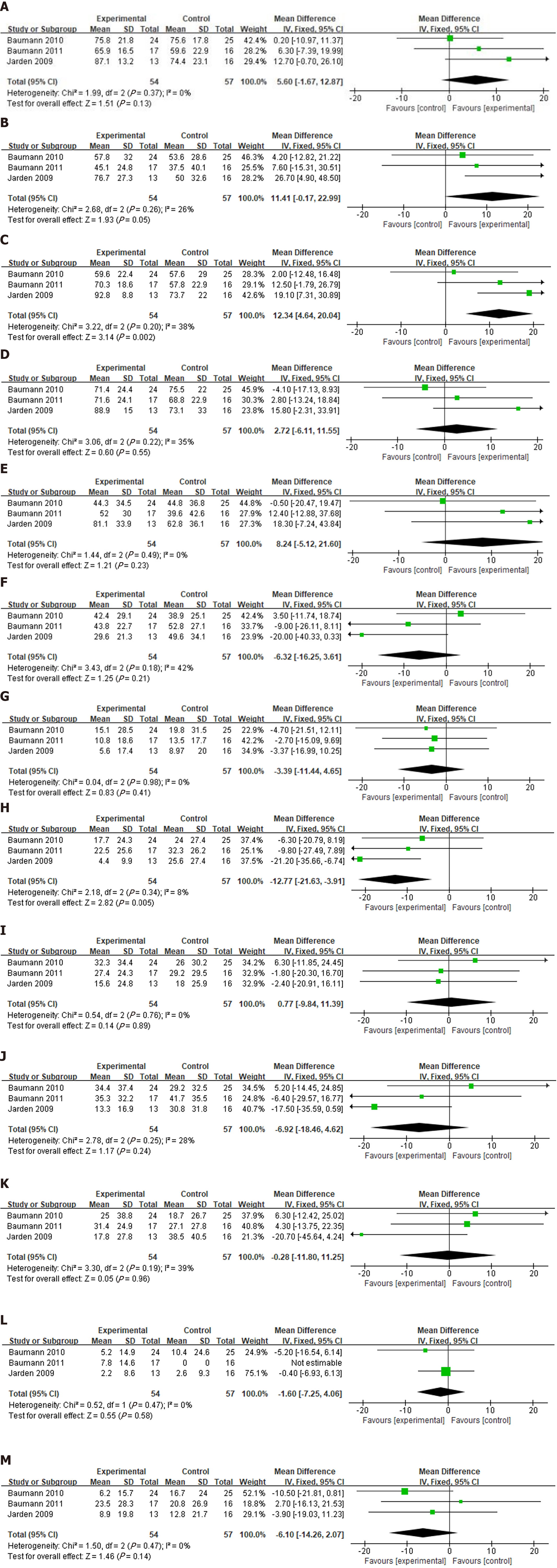
In this study, QoL was assessed by analyzing the scores for various domains from the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire C30, (EORTC QLQ-C30)[28-30]. There were 111 individuals recruited for the mentioned outcomes (54 in the intervention group, 57 in the control group). The QLQ-C30 scores for global functioning and the domains of the QLQ-C30 questionnaires were analyzed. A total of 14 outcomes were obtained, representing global aspects and each aspect of QoL. The global functioning of QLQ-C30 results is illustrated in Figure 3. Physical exercise groups exhibited significantly different QoL scores (mean score difference = 8.81; 95%CI: 1.81-15.81, P = 0.01). The QLQ-C30 results are shown in Figures 4A-M. The physical exercise intervention group exhibited significantly different scores for emotional functioning (mean score difference =12.34; 95%CI: 4.64-20.04, P < 0.01) and pain (mean score difference = –12.77; 95%CI: -21.63 to -3.91, P < 0.01) compared to the controls.
To the best of our knowledge, this is the first meta-analysis of QoL assessments testing physical exercise interventions in patients with haematological malignancies and thrombocytopenia. The beneficial effects on QoL in haematological malignancy patients have been shown by previous studies[18-22]. The present study also found a robust correlation between administration of exercise interventions and enhancement of QoL in patients with haematological malignancies and thrombocytopenia, especially in terms of emotional functioning and pain. Therefore, this implies that patients with haematological malignancies and thrombocytopenia may achieve a significant benefit from exercise interventions. There should be some caution over the interpretation of this finding since there were numerous confounding factors (e.g., disparity of baseline characteristics, quality control of intervention process, completion efficiency of subjects, and different assessment tools), which may have influenced the analysis of the findings. In addition, QoL is the reduction in inflammation following the execution of physical exercise.
Previous studies reported the benefits of physical exercise on emotional functioning in haematological malignancy patients, and the results of the present study are consistent with that evidence[33,35]. One study indicated that emotional functioning was significantly improved in the exercise intervention group of patients with acute leukaemia, and it was suggested that the psychosocial aspects of the intervention (the socialisation and communication between the exercise trainers and patients) might have a positively impact on QoL[33]. Another study suggested the benefit of exercise on pain in lymphoma patients, although a lack of reliable evidence was presented[35]. We found that exercise had an effect on pain in haematological malignancy patients.
Due to the clinical instability of haematological malignancy patients, physical conditions and blood values varied during therapy, and the exercise training protocols should be adjusted daily, which may lead to an underestimation or overestimation of the effect of physical exercise[36]. Typically, platelet counts drop following chemotherapy, with the lowest count occurring 7-10 d post-chemotherapy, and the count can take 2-3 wk to recover[37]. For this reason, such RCTs were insufficiently conducted for physical exercise interventions in patients with haematological malignancies and thrombocytopenia.
Although the data gathered in some studies support the safety of exercise interventions because no adverse effects were reported[33,38], adverse events are rare in general and less likely to be observed in studies with a limited sample size. Furthermore, while adverse events are an important consideration in patients with haematological malignancies and thrombocytopenia, we failed to consider these due to the lack of reporting in the articles reviewed. Patients with severe thrombocytopenia are at risk of spontaneous bleeding and should not undergo physical exercise without prior consultation with their attending physician.
In general, a person’s physical performance level can be determined by aerobic capacity and muscle strength, which can considerably impact patient QoL[33]. Resistance training could counteract the substantial loss of strength that occurs during acute therapy[39]. Although the articles included here were RCTs, it was difficult to control the exercise intensity of each participant, and there was inevitably bias involved due to the inapplicability of blinded methods. To examine the most effective type, duration and intensity of exercise, further trials with more participants and a rigorous study design should be conducted to measure the effect of exercise on QoL. In addition, longer follow-up times are required to observe any possible long-term effects. The comparability of the study data could be improved by standardizing measurement instruments.
This study had several limitations that should be considered. The major limitation was the insufficient number of available RCTs. Thus, the statistical power was low and we were unable to do subgroup analysis among patients with acute leukaemias and HSCT due to the small study sample size. Second, the physical exercise intervention was not uniform, for example, in terms of the exercise type, intensity, time and frequency. Subgroup analyses were not conducted for the exercise types. Further RCTs should be conducted to examine the different effects exerted by exercise types on global and the other domains of QLQ-C30. Third, the included studies achieved a low level of evidence, which demonstrates that more high-quality research should be conducted to reduce the risk of bias and draw more robust conclusions regarding physical exercise interventions. Fourth, as the articles reviewed here were conducted in only three nations (i.e., Germany, United States and Denmark), the results might not be generalized to haematological malignancy patients elsewhere. On the whole, in Mainland China, patients and their family members are conservative and superstitious. Medical and rehabilitation providers, as well as patients and families, voiced their concern that physical exercise and mobilization may cause bleeding in the patients[23]. Although some patients expressed a desire for exercise support, they were also afraid of bleeding and injury[40].
It has been suggested that physical exercise positively impacts patients with haematological malignancies and thrombocytopenia. This study found evidence that physical exercise improves the QoL of these patients, especially in terms of emotional functioning and pain management. Subsequent trials should include an adequate sample size, participants from a wide range of ethnic groups should be recruited and efficacy and safety outcomes should be measured and reported. In addition, the effect exerted by exercise intervention should be examined over longer durations following the intervention. In addition, further studies should include a control group who receive physical exercise and blinded testing of physical and psychological performance.
Annually, there are an estimated 1187000 new patients worldwide diagnosed with haematological malignancies, including leukaemia, myeloma, and lymphoma, resulting in 690000 deaths. Effective strategies are needed to alleviate side effects and prevent the physical and psychosocial degeneration of patients in active treatment for haematological malignancies.
The prevailing advice for haematological malignancy patients is to rest and sleep more, especially if they have thrombocytopenia, and to avoid intensive and high-energy physical activity, without taking note of the negative effects such as thromboembolic diseases, pressure ulcers, deconditioning, contractures, fatigue, and atelectasis. Some other studies have not indicated clear findings in relation to this advice.
This study aimed to examine the effects of physical exercise on the quality of life (QoL) of haematological malignancy patients with thrombocytopenia, and to provide an evidence-based medical basis for the application and promotion of physical exercise.
This study was conducted using randomized controlled trials (RCTs) to assess the effect of physical exercise on the QoL of haematological malignancy patients with thrombocytopenia. We complied with the checklist of PRISMA[25]. The protocol was registered in the PROSPERO International Prospective Register of Systematic Review (number: CRD42021256897). We searched PubMed, Cochrane Library and Embase databases for all relevant articles published up to 31 July 2021.
Seven RCTs were selected in the systematic review and three were included in the final meta-analysis. There were significant differences in QoL between physical exercise groups [mean score difference = 8.81; 95% confidence interval (CI): 1.81-15.81, P = 0.01], especially in emotional functioning (mean score difference = 12.34; 95%CI: 4.64-20.04, P = 0.002) and pain (mean score difference = –12.77; 95%CI: -3.91 to -21.63, P = 0.005).
It has been suggested that physical exercise positively impacts patients with haematological malignancies and thrombocytopenia. This study found evidence that physical exercise improves the QoL of these patients, especially in terms of emotional functioning and pain management.
Subsequent trials should include an adequate sample size, participants from a wide range of ethnic groups should be recruited and efficacy and safety outcomes should be measured and reported. In addition, the effect exerted by exercise intervention should be examined over longer durations following the intervention. In addition, further studies should include a control group who receive physical exercise and blinded testing of physical and psychological performance.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gaman MA S-Editor: Wang JJ L-Editor: A P-Editor: Guo X
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55806] [Article Influence: 7972.3] [Reference Citation Analysis (132)] |
| 2. | Knips L, Bergenthal N, Streckmann F, Monsef I, Elter T, Skoetz N. Aerobic physical exercise for adult patients with haematological malignancies. Cochrane Database Syst Rev. 2019;1:CD009075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 3. | Redaelli A, Stephens JM, Brandt S, Botteman MF, Pashos CL. Short- and long-term effects of acute myeloid leukemia on patient health-related quality of life. Cancer Treat Rev. 2004;30:103-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 67] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Goswami P, Oliva EN, Ionova T, Else R, Kell J, Fielding AK, Jennings DM, Karakantza M, Al-Ismail S, Collins GP, McConnell S, Langton C, Salek S. Quality-of-life issues and symptoms reported by patients living with haematological malignancy: a qualitative study. Ther Adv Hematol. 2020;11:2040620720955002. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Mounier N, Anthony S, Busson R, Thieblemont C, Ribrag V, Tilly H, Haioun C, Casasnovas RO, Morschhauser F, Feugier P, Delarue R, Ysebaert L, Sebban C, Broussais-Guillaumot F, Damaj G, Nerich V, Jais JP, Laborde L, Salles G, Henry-Amar M. Long-term fatigue in survivors of non-Hodgkin lymphoma: The Lymphoma Study Association SIMONAL cross-sectional study. Cancer. 2019;125:2291-2299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Baytan B, Aşut Ç, Çırpan Kantarcıoğlu A, Sezgin Evim M, Güneş AM. Health-Related Quality of Life, Depression, Anxiety, and Self-Image in Acute Lymphocytic Leukemia Survivors. Turk J Haematol. 2016;33:326-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | McCabe MS, Bhatia S, Oeffinger KC, Reaman GH, Tyne C, Wollins DS, Hudson MM. American Society of Clinical Oncology statement: achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31:631-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 357] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 8. | van Waart H, Stuiver MM, van Harten WH, Geleijn E, Kieffer JM, Buffart LM, de Maaker-Berkhof M, Boven E, Schrama J, Geenen MM, Meerum Terwogt JM, van Bochove A, Lustig V, van den Heiligenberg SM, Smorenburg CH, Hellendoorn-van Vreeswijk JA, Sonke GS, Aaronson NK. Effect of Low-Intensity Physical Activity and Moderate- to High-Intensity Physical Exercise During Adjuvant Chemotherapy on Physical Fitness, Fatigue, and Chemotherapy Completion Rates: Results of the PACES Randomized Clinical Trial. J Clin Oncol. 2015;33:1918-1927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 447] [Article Influence: 44.7] [Reference Citation Analysis (0)] |
| 9. | Schmitz KH, Campbell AM, Stuiver MM, Pinto BM, Schwartz AL, Morris GS, Ligibel JA, Cheville A, Galvão DA, Alfano CM, Patel AV, Hue T, Gerber LH, Sallis R, Gusani NJ, Stout NL, Chan L, Flowers F, Doyle C, Helmrich S, Bain W, Sokolof J, Winters-Stone KM, Campbell KL, Matthews CE. Exercise is medicine in oncology: Engaging clinicians to help patients move through cancer. CA Cancer J Clin. 2019;69:468-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 475] [Article Influence: 79.2] [Reference Citation Analysis (0)] |
| 10. | Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, Zucker DS, Matthews CE, Ligibel JA, Gerber LH, Morris GS, Patel AV, Hue TF, Perna FM, Schmitz KH. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc. 2019;51:2375-2390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1595] [Cited by in RCA: 1702] [Article Influence: 283.7] [Reference Citation Analysis (0)] |
| 11. | Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC, Snyder C. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;CD007566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 268] [Cited by in RCA: 397] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 12. | Buffart LM, Sweegers MG, May AM, Chinapaw MJ, van Vulpen JK, Newton RU, Galvão DA, Aaronson NK, Stuiver MM, Jacobsen PB, Verdonck-de Leeuw IM, Steindorf K, Irwin ML, Hayes S, Griffith KA, Lucia A, Herrero-Roman F, Mesters I, van Weert E, Knoop H, Goedendorp MM, Mutrie N, Daley AJ, McConnachie A, Bohus M, Thorsen L, Schulz KH, Short CE, James EL, Plotnikoff RC, Arbane G, Schmidt ME, Potthoff K, van Beurden M, Oldenburg HS, Sonke GS, van Harten WH, Garrod R, Schmitz KH, Winters-Stone KM, Velthuis MJ, Taaffe DR, van Mechelen W, José Kersten M, Nollet F, Wenzel J, Wiskemann J, Brug J, Courneya KS. Targeting Exercise Interventions to Patients With Cancer in Need: An Individual Patient Data Meta-Analysis. J Natl Cancer Inst. 2018;110:1190-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 13. | Buffart LM, Kalter J, Sweegers MG, Courneya KS, Newton RU, Aaronson NK, Jacobsen PB, May AM, Galvão DA, Chinapaw MJ, Steindorf K, Irwin ML, Stuiver MM, Hayes S, Griffith KA, Lucia A, Mesters I, van Weert E, Knoop H, Goedendorp MM, Mutrie N, Daley AJ, McConnachie A, Bohus M, Thorsen L, Schulz KH, Short CE, James EL, Plotnikoff RC, Arbane G, Schmidt ME, Potthoff K, van Beurden M, Oldenburg HS, Sonke GS, van Harten WH, Garrod R, Schmitz KH, Winters-Stone KM, Velthuis MJ, Taaffe DR, van Mechelen W, Kersten MJ, Nollet F, Wenzel J, Wiskemann J, Verdonck-de Leeuw IM, Brug J. Effects and moderators of exercise on quality of life and physical function in patients with cancer: An individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev. 2017;52:91-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 394] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 14. | Sweegers MG, Altenburg TM, Brug J, May AM, van Vulpen JK, Aaronson NK, Arbane G, Bohus M, Courneya KS, Daley AJ, Galvao DA, Garrod R, Griffith KA, Van Harten WH, Hayes SC, Herrero-Román F, Kersten MJ, Lucia A, McConnachie A, van Mechelen W, Mutrie N, Newton RU, Nollet F, Potthoff K, Schmidt ME, Schmitz KH, Schulz KH, Sonke G, Steindorf K, Stuiver MM, Taaffe DR, Thorsen L, Twisk JW, Velthuis MJ, Wenzel J, Winters-Stone KM, Wiskemann J, Chin A Paw MJ, Buffart LM. Effects and moderators of exercise on muscle strength, muscle function and aerobic fitness in patients with cancer: a meta-analysis of individual patient data. Br J Sports Med. 2019;53:812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 15. | Nakano J, Hashizume K, Fukushima T, Ueno K, Matsuura E, Ikio Y, Ishii S, Morishita S, Tanaka K, Kusuba Y. Effects of Aerobic and Resistance Exercises on Physical Symptoms in Cancer Patients: A Meta-analysis. Integr Cancer Ther. 2018;17:1048-1058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 82] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 16. | Gheyasi F, Baraz S, Malehi A, Ahmadzadeh A, Salehi R, Vaismoradi M. Effect of the Walking Exercise Program on Cancer-Related Fatigue in Patients with Acute Myeloid Leukemia Undergoing Chemotherapy. Asian Pac J Cancer Prev. 2019;20:1661-1666. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Lanfranconi F, Zardo W, Moriggi T, Villa E, Radaelli G, Radaelli S, Paoletti F, Bottes E, Miraglia T, Pollastri L, Vago P, Nichelli F, Jankovic M, Biondi A, Balduzzi A. Precision-based exercise as a new therapeutic option for children and adolescents with haematological malignancies. Sci Rep. 2020;10:12892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Fukushima T, Nakano J, Ishii S, Natsuzako A, Sakamoto J, Okita M. Low-intensity exercise therapy with high frequency improves physical function and mental and physical symptoms in patients with haematological malignancies undergoing chemotherapy. Eur J Cancer Care (Engl). 2018;27:e12922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Zimmer P, Oberste M, Bloch W, Schenk A, Joisten N, Hartig P, Wolf F, Baumann FT, Garthe A, Hallek M, Elter T. Impact of aerobic exercise training during chemotherapy on cancer related cognitive impairments in patients suffering from acute myeloid leukemia or myelodysplastic syndrome - Study protocol of a randomized placebo-controlled trial. Contemp Clin Trials. 2016;49:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvão DA, Pinto BM, Irwin ML, Wolin KY, Segal RJ, Lucia A, Schneider CM, von Gruenigen VE, Schwartz AL; American College of Sports Medicine. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42:1409-1426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1802] [Cited by in RCA: 1937] [Article Influence: 129.1] [Reference Citation Analysis (0)] |
| 21. | Elter T, Stipanov M, Heuser E, von Bergwelt-Baildon M, Bloch W, Hallek M, Baumann F. Is physical exercise possible in patients with critical cytopenia undergoing intensive chemotherapy for acute leukaemia or aggressive lymphoma? Int J Hematol. 2009;90:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Paul KL. Rehabilitation and exercise considerations in hematologic malignancies. Am J Phys Med Rehabil. 2011;90:S88-S94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Ibanez K, Espiritu N, Souverain RL, Stimler L, Ward L, Riedel ER, Lehrman R, Boulad F, Stubblefield MD. Safety and Feasibility of Rehabilitation Interventions in Children Undergoing Hematopoietic Stem Cell Transplant With Thrombocytopenia. Arch Phys Med Rehabil. 2018;99:226-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Morishita S, Nakano J, Fu JB, Tsuji T. Physical exercise is safe and feasible in thrombocytopenic patients with hematologic malignancies: a narrative review. Hematology. 2020;25:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 1308] [Article Influence: 327.0] [Reference Citation Analysis (1)] |
| 26. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24807] [Article Influence: 1771.9] [Reference Citation Analysis (3)] |
| 27. | Scientific Research An Academic Publisher. Review Manager (RevMan) (2014) Version 5.3. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration. [cited 5 August 2021]. Available from: https://www.scirp.org/reference/ReferencesPapers.aspx?ReferenceID=2534983. |
| 28. | Jarden M, Baadsgaard MT, Hovgaard DJ, Boesen E, Adamsen L. A randomized trial on the effect of a multimodal intervention on physical capacity, functional performance and quality of life in adult patients undergoing allogeneic SCT. Bone Marrow Transplant. 2009;43:725-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 165] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 29. | Baumann FT, Kraut L, Schüle K, Bloch W, Fauser AA. A controlled randomized study examining the effects of exercise therapy on patients undergoing haematopoietic stem cell transplantation. Bone Marrow Transplant. 2010;45:355-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 119] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 30. | Baumann FT, Zopf EM, Nykamp E, Kraut L, Schüle K, Elter T, Fauser AA, Bloch W. Physical activity for patients undergoing an allogeneic hematopoietic stem cell transplantation: benefits of a moderate exercise intervention. Eur J Haematol. 2011;87:148-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 31. | Oechsle K, Aslan Z, Suesse Y, Jensen W, Bokemeyer C, de Wit M. Multimodal exercise training during myeloablative chemotherapy: a prospective randomized pilot trial. Support Care Cancer. 2014;22:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 32. | Bryant AL, Deal AM, Battaglini CL, Phillips B, Pergolotti M, Coffman E, Foster MC, Wood WA, Bailey C, Hackney AC, Mayer DK, Muss HB, Reeve BB. The Effects of Exercise on Patient-Reported Outcomes and Performance-Based Physical Function in Adults With Acute Leukemia Undergoing Induction Therapy: Exercise and Quality of Life in Acute Leukemia (EQUAL). Integr Cancer Ther. 2018;17:263-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 33. | Wehrle A, Kneis S, Dickhuth HH, Gollhofer A, Bertz H. Endurance and resistance training in patients with acute leukemia undergoing induction chemotherapy-a randomized pilot study. Support Care Cancer. 2019;27:1071-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 34. | Pahl A, Wehrle A, Kneis S, Gollhofer A, Bertz H. Whole body vibration training during allogeneic hematopoietic cell transplantation-the effects on patients' physical capacity. Ann Hematol. 2020;99:635-648. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 35. | Cox MC, Nusca SM, Di Landro F, Marsilli G, Stella G, Sigona M, Ponzelli F, Passerini Desideri J, Di Gregorio F, Santoboni F, Vetrano M, Trischitta D, Manno R, Vulpiani MC. Exercise training (ET) in adult and elderly patients receiving anti-lymphoma treatments is feasible and may improve the provision of care. Leuk Lymphoma. 2021;62:560-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 36. | Fioritto AP, Oliveira CC, Albuquerque VS, Almeida LB, Granger CL, Denehy L, Malaguti C. Individualized in-hospital exercise training program for people undergoing hematopoietic stem cell transplantation: a feasibility study. Disabil Rehabil. 2021;43:386-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Jeevanantham D, Rajendran V, McGillis Z, Tremblay L, Larivière C, Knight A. Mobilization and Exercise Intervention for Patients With Multiple Myeloma: Clinical Practice Guidelines Endorsed by the Canadian Physiotherapy Association. Phys Ther. 2021;101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 38. | Zhou Y, Zhu J, Gu Z, Yin X. Efficacy of Exercise Interventions in Patients with Acute Leukemia: A Meta-Analysis. PLoS One. 2016;11:e0159966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 39. | Padilha CS, Marinello PC, Galvão DA, Newton RU, Borges FH, Frajacomo F, Deminice R. Evaluation of resistance training to improve muscular strength and body composition in cancer patients undergoing neoadjuvant and adjuvant therapy: a meta-analysis. J Cancer Surviv. 2017;11:339-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 94] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 40. | Craike MJ, Hose K, Courneya KS, Harrison SJ, Livingston PM. Perceived benefits and barriers to exercise for recently treated patients with multiple myeloma: a qualitative study. BMC Cancer. 2013;13:319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |