Copyright
©The Author(s) 2021.
World J Clin Cases. Feb 26, 2021; 9(6): 1475-1482
Published online Feb 26, 2021. doi: 10.12998/wjcc.v9.i6.1475
Published online Feb 26, 2021. doi: 10.12998/wjcc.v9.i6.1475
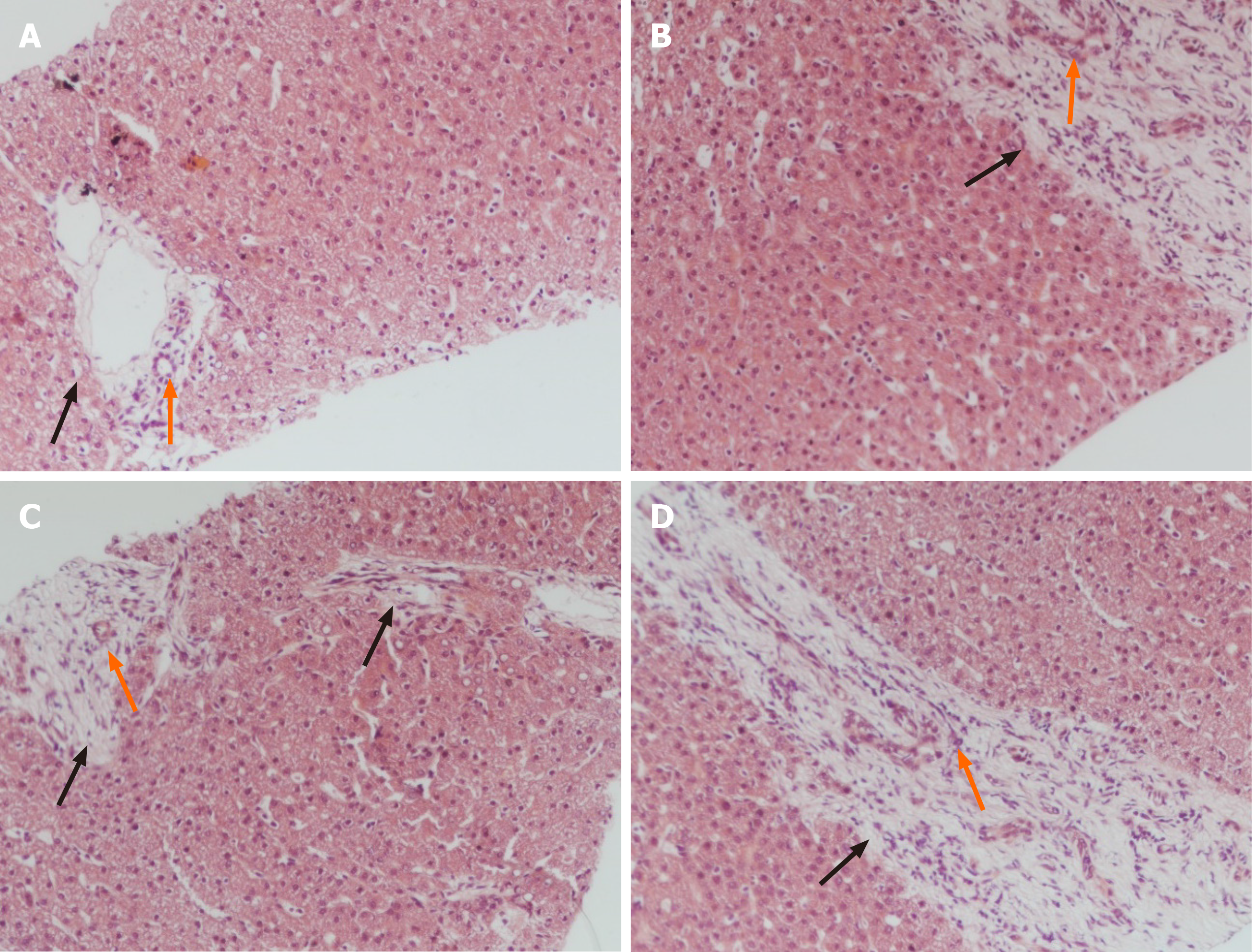
Figure 1 Histologic biopsy of the patient’s liver showing congenital hepatic fibrosis.
A: The markedly enlarged portal tracts (black fork); B-D: Widened fibrous septa (black forks); A-D: Proliferating bile ducts (orange forks) (hematoxylin and eosin stain, × 100).
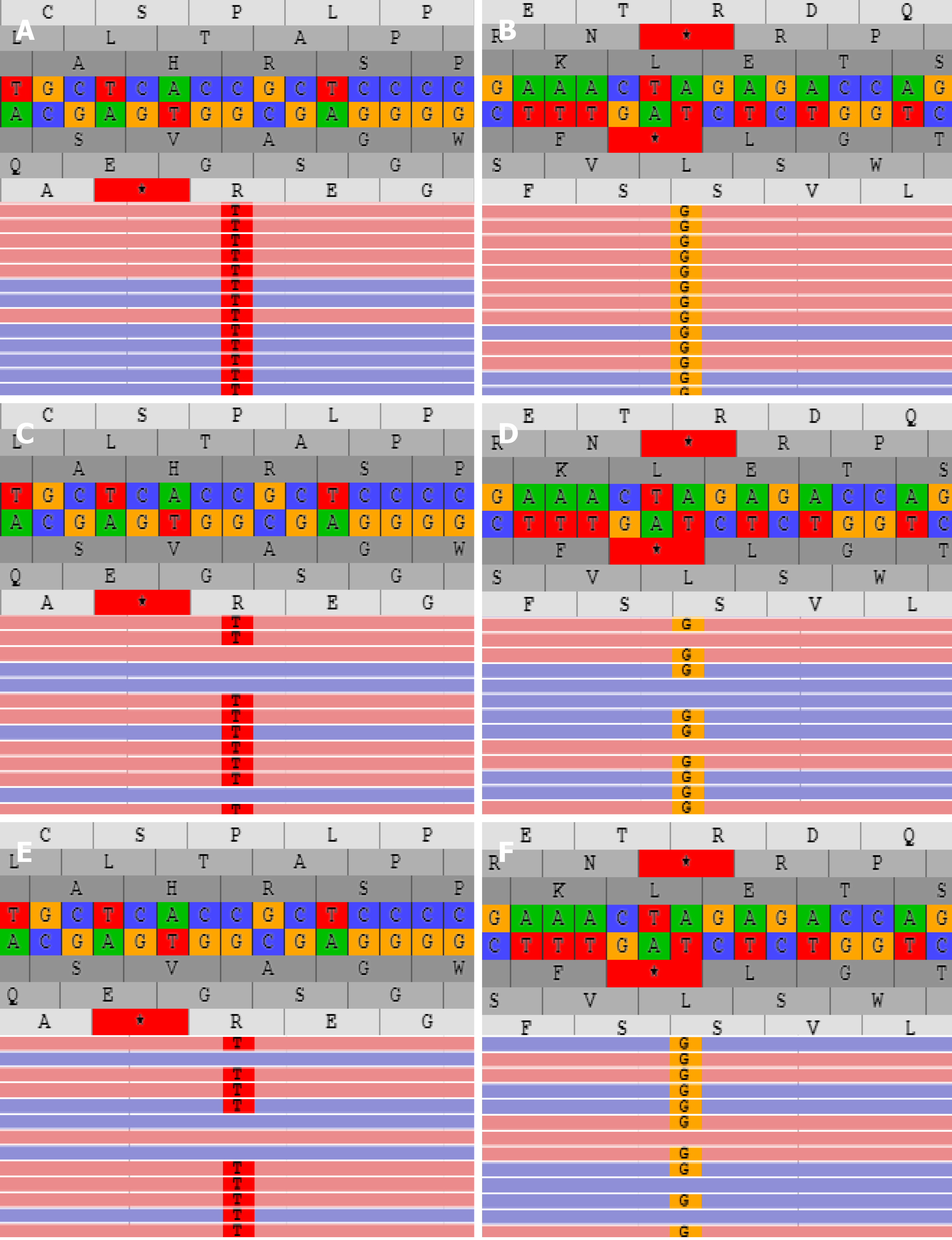
Figure 2 PKHD1 and DUOX2 mutations analysis of the patient and his family.
A and B: The proband carried the homozygous mutation c.2141-3T>C of PKHD1 (A) and c.2921G>A of DUOX2 gene (B); C and D: The father had heterozygous c.2141-3T>C of PKHD1 (C) and c.2921G>A of DUOX2 gene (D); E and F: The mother carried heterozygous c.2141-3T>C of PKHD1 (E) and c.2921G>A of DUOX2 gene (F).
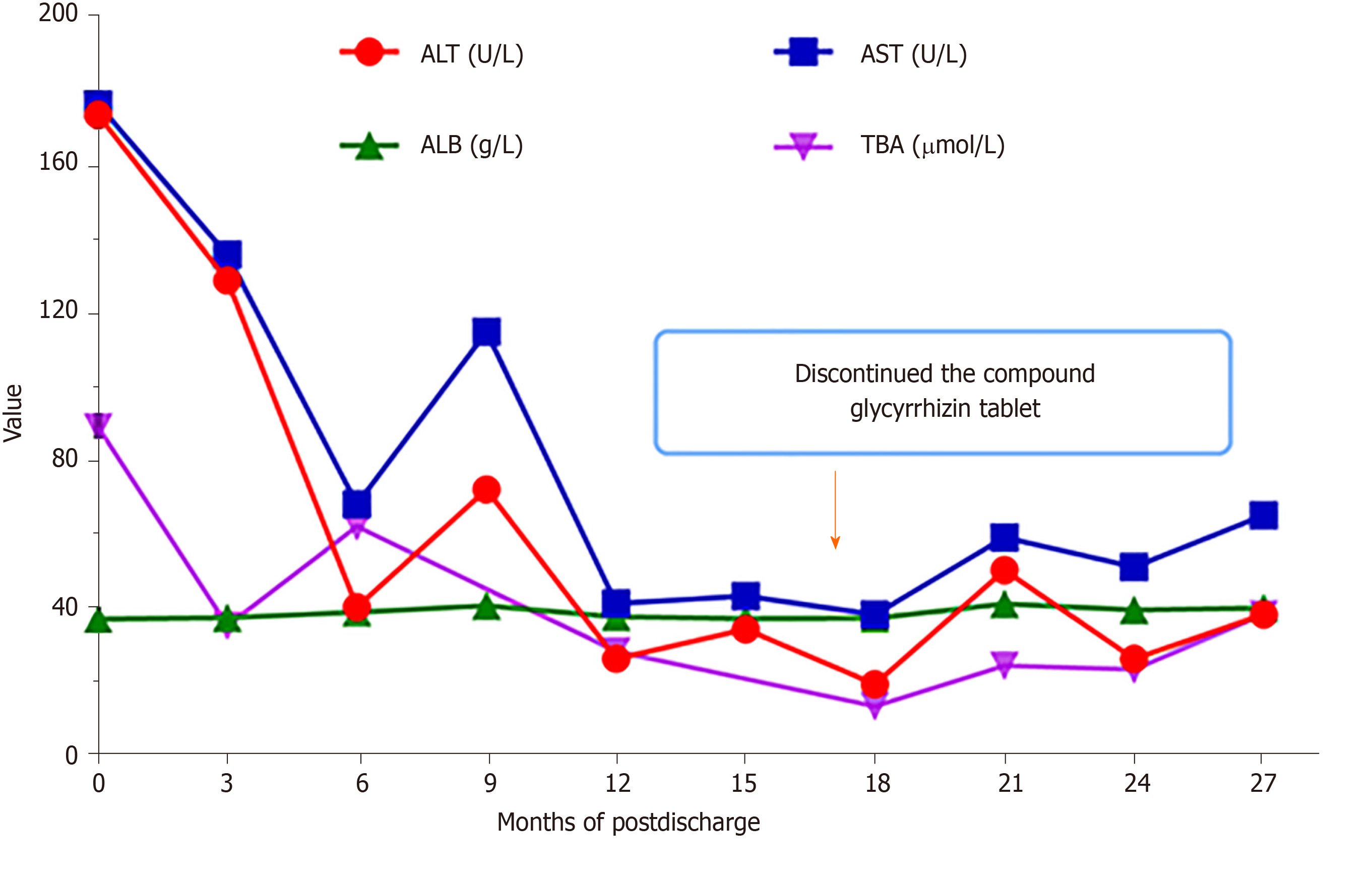
Figure 3 Patient’s liver function indices approximately 2 years after follow-up.
The patient’s increased transaminases resolved a year after hospitalization, and the compound glycyrrhizin tablet was discontinued at 15 mo after hospital discharge. Albumin remained within normal levels, despite the level of total serum bile acid being slightly elevated. ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; ALB: Albumin; TBA: Total serum bile acid.
- Citation: Xiao FF, Wang YZ, Dong F, Li XL, Zhang T. Congenital hepatic fibrosis in a young boy with congenital hypothyroidism: A case report. World J Clin Cases 2021; 9(6): 1475-1482
- URL: https://www.wjgnet.com/2307-8960/full/v9/i6/1475.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i6.1475