Copyright
©The Author(s) 2021.
World J Clin Cases. Oct 16, 2021; 9(29): 8871-8878
Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8871
Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8871
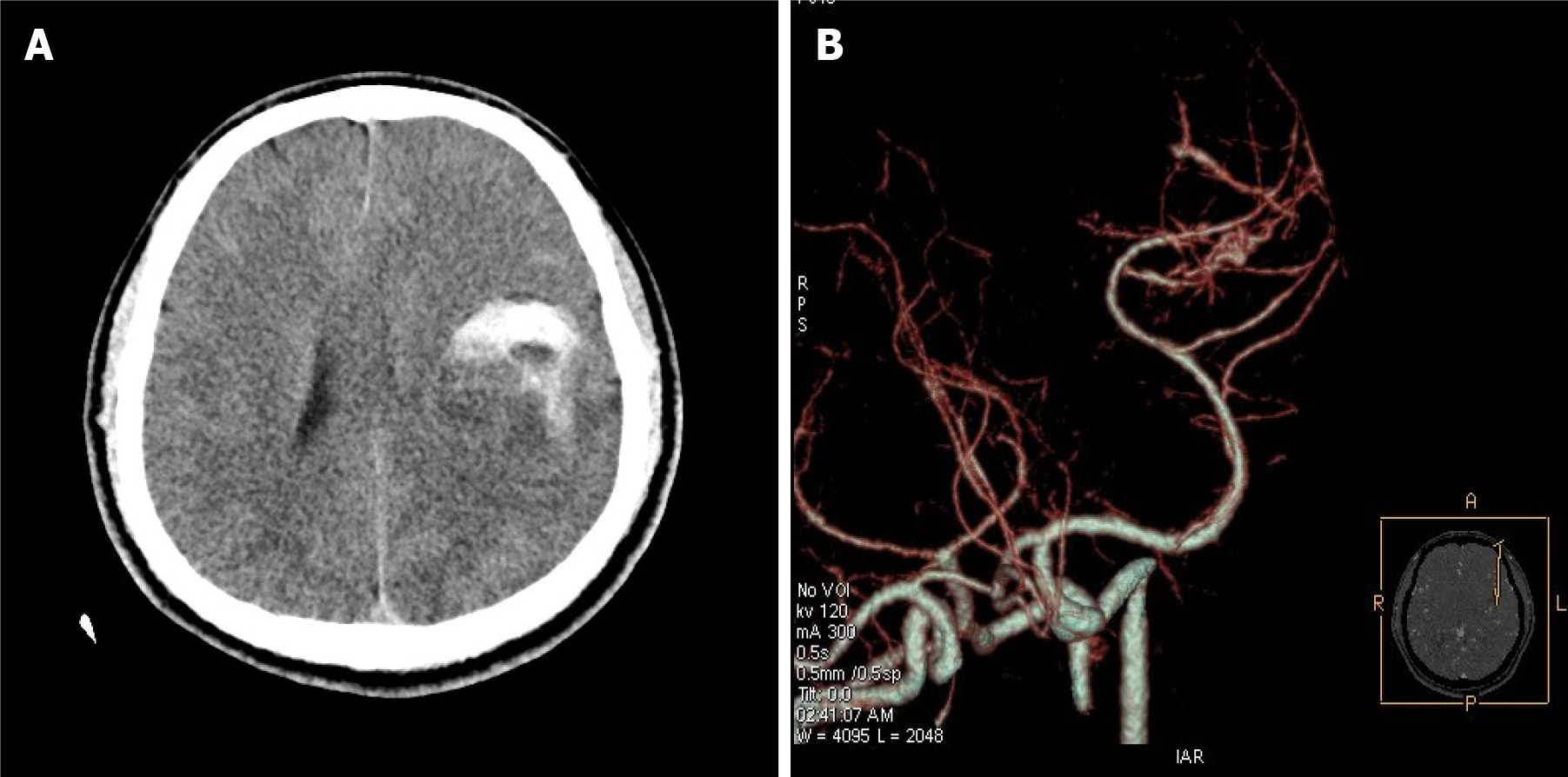
Figure 1 Preoperative computed tomography and computed tomography angiography.
A: Computed tomography (CT) indicated a round space on the left with high-density shadows, suggesting tumor with hemorrhage; B: CT angiography indicated the possibility of arteriovenous malformation of the left middle cerebral artery.
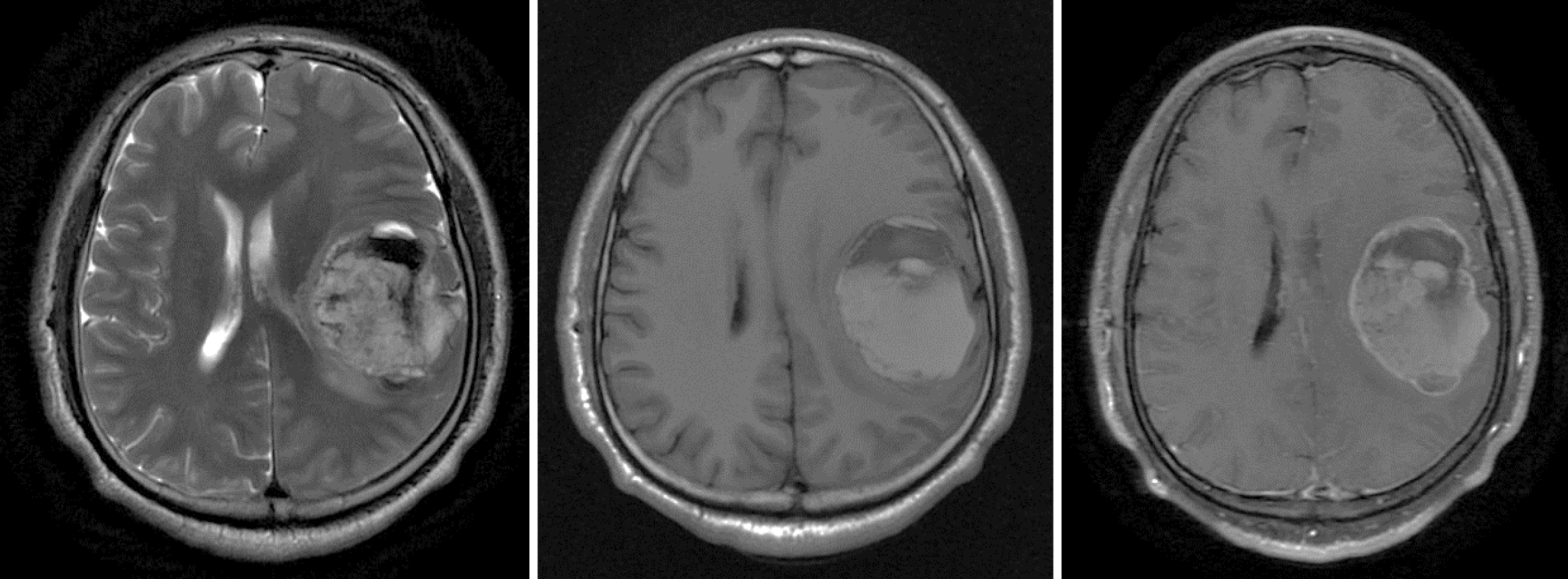
Figure 2 Preoperative magnetic resonance imaging.
Round abnormal signal occupying lesions on T2-weighted imaging (WI) and T1WI were long or short mixed signals, associated with cystic and minimal edema. The wall and substantial part of the lesion were enhanced.
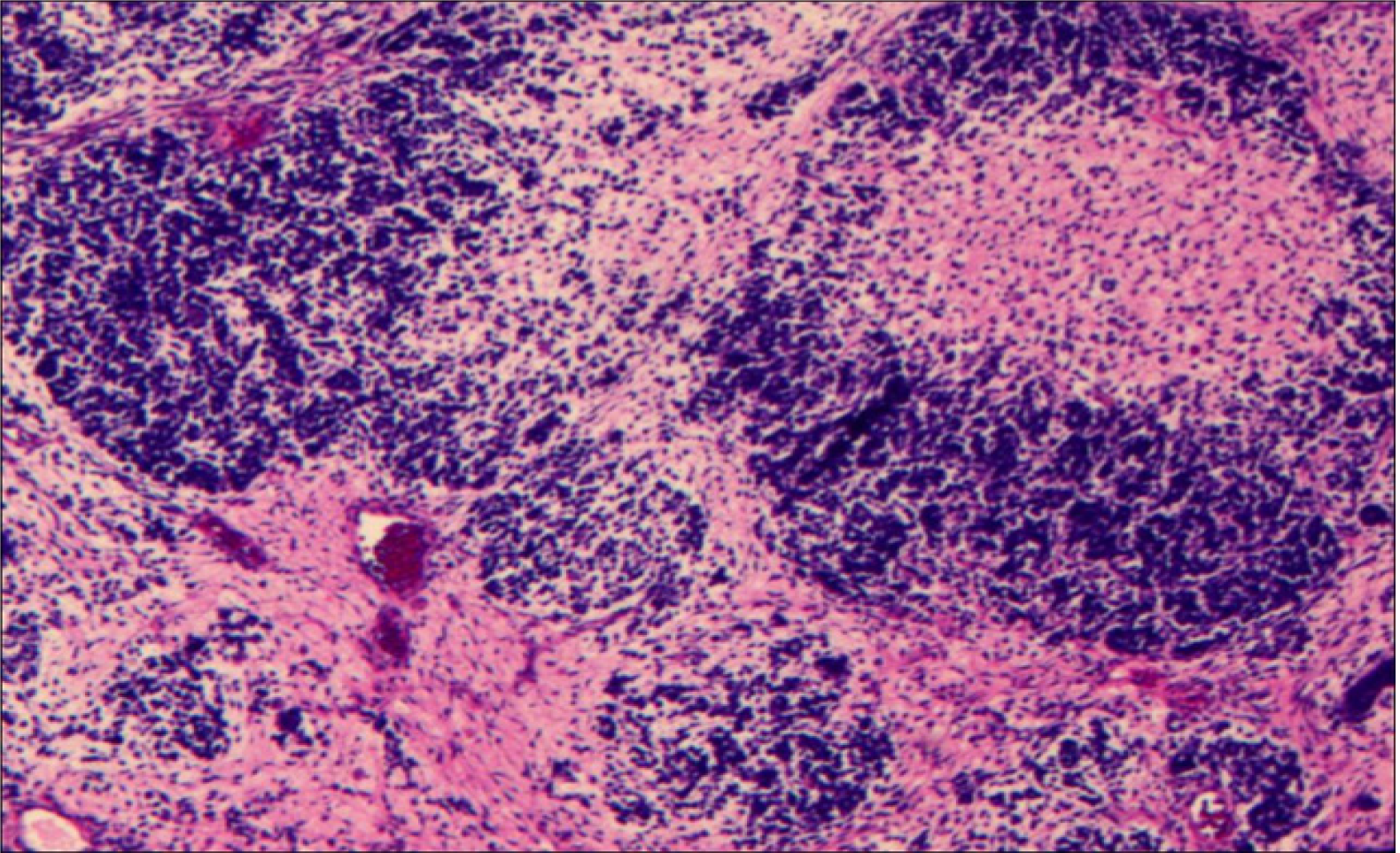
Figure 3 Pathological examination of the tumor tissue.
Hematoxylin–eosin staining of the tumor cells showed diffuse growth with cellular atypia and mitotic figures. Image at 40 × magnification.
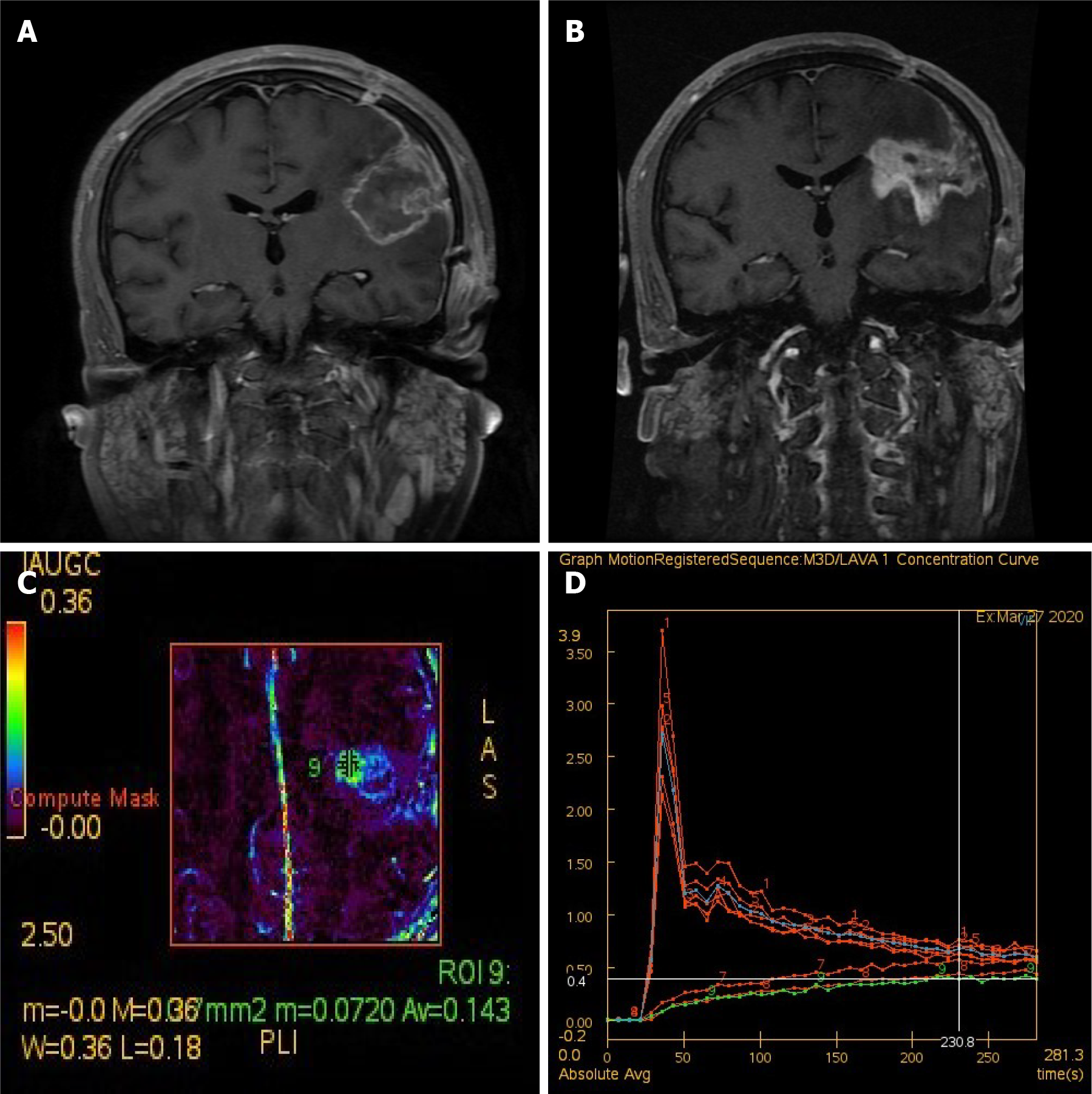
Figure 4 Imaging changes after treatment of synovial sarcoma.
A: Enhanced T1-weighted imaging (T1WI) after craniotomy indicated tumor removal; B-D: Perfusion-weighted imaging 6 mo after craniotomy (3 mo after radiotherapy). Enhanced T1WI indicated that the lesion was larger than before (B). Analysis of the enlarged part of the lesion (the area marked by 9 in C) suggested that the enlarged lesion is hypoperfusion, and radiation necrosis was considered (C and D).
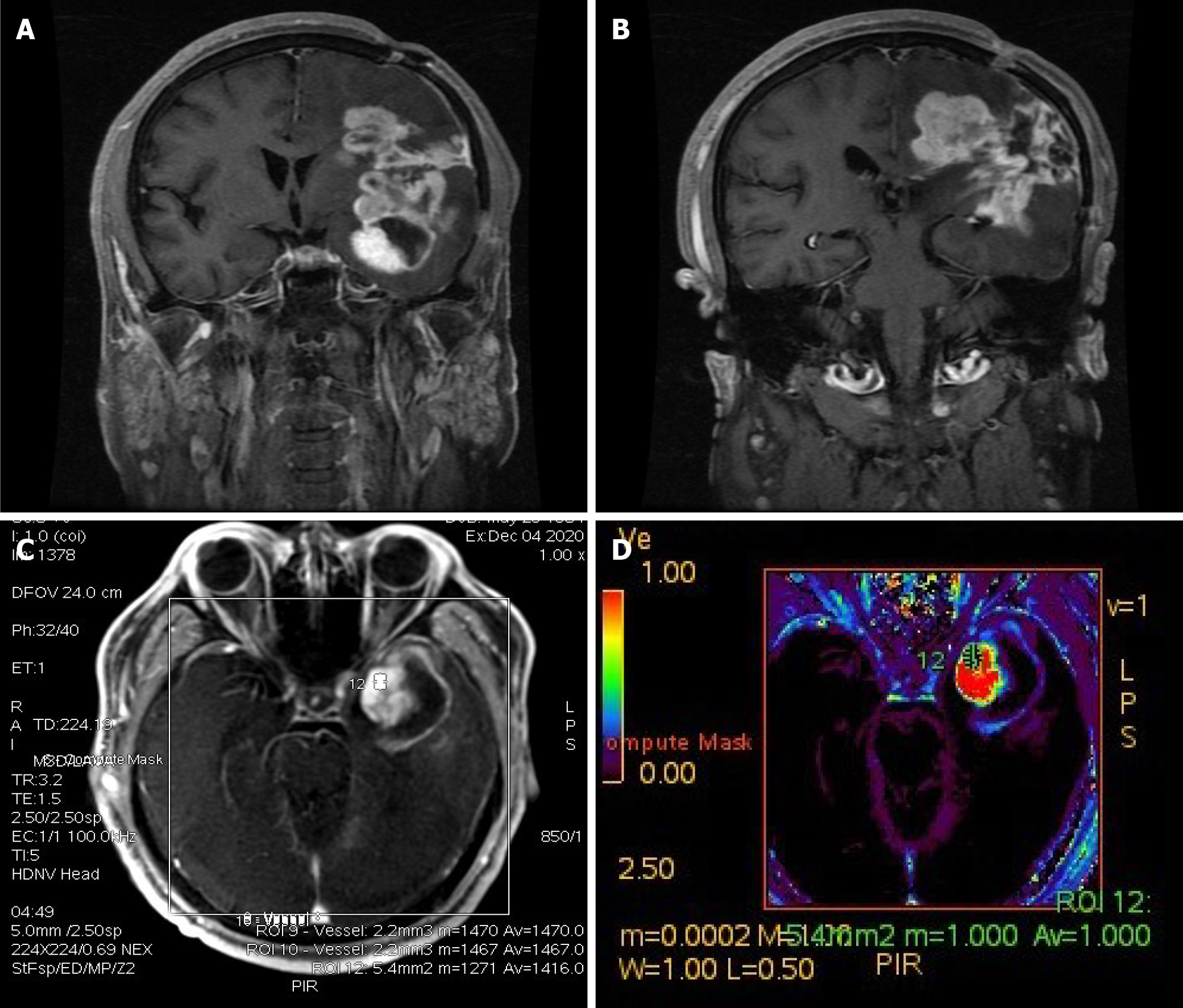
Figure 5 Imaging changes during patient follow-up.
A and B: Enhanced T1-weighted imaging 16 mo after craniotomy indicated enlargement of the lesion; C and D: Perfusion-weighted imaging of the enlarged part of the lesion (area marked by 12 in C) suggested that the enlarged lesion had high perfusion, and tumor recurrence was considered.
- Citation: Wang YY, Li ML, Zhang ZY, Ding JW, Xiao LF, Li WC, Wang L, Sun T. Primary intracranial synovial sarcoma with hemorrhage: A case report. World J Clin Cases 2021; 9(29): 8871-8878
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8871.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8871