Copyright
©The Author(s) 2021.
World J Clin Cases. May 6, 2021; 9(13): 3185-3193
Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3185
Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3185
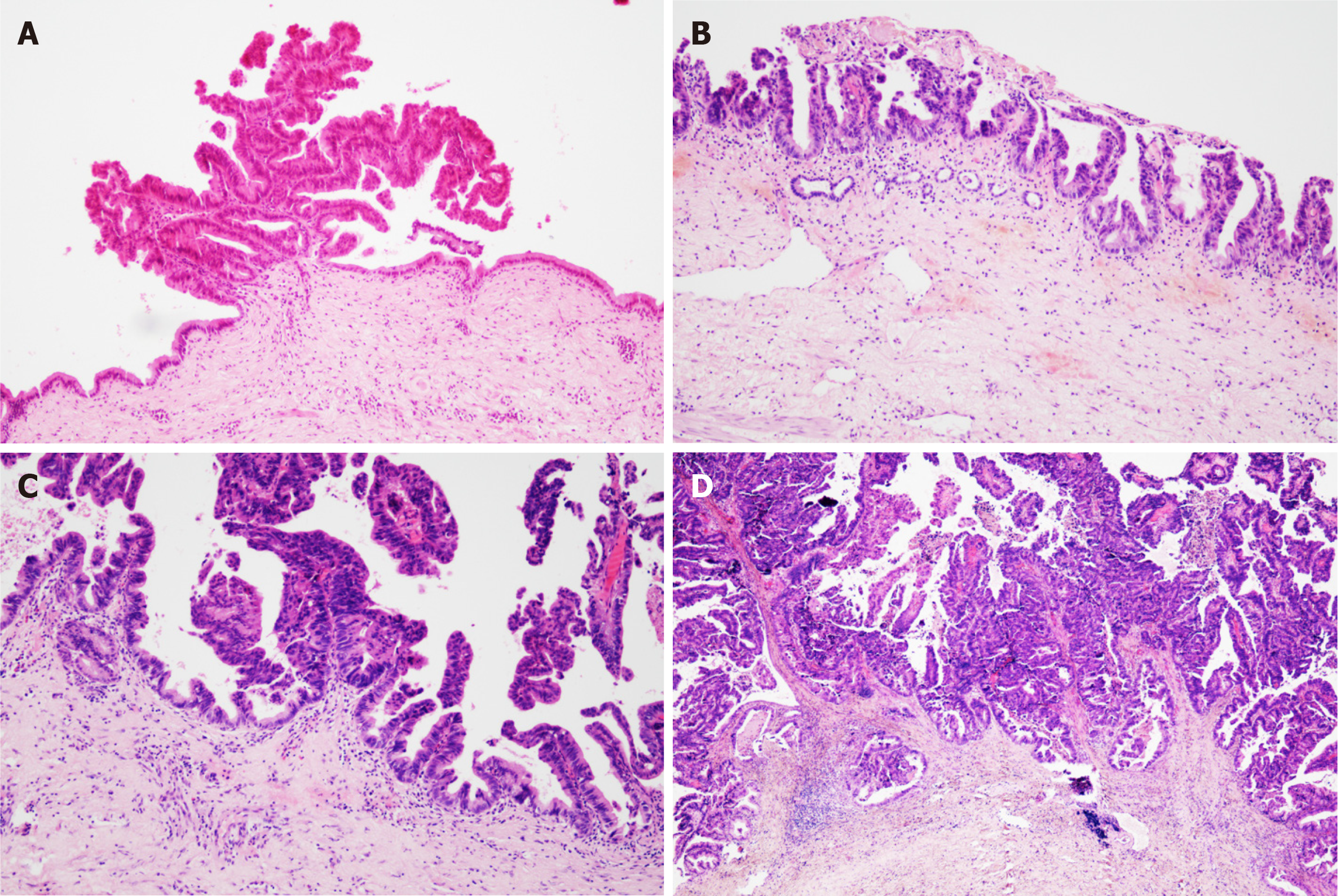
Figure 1 Pathological images.
A: Intrahepatic bile duct papilloma (IPNB)’s atypical hyperplasia; B: IPNB’s intraepithelial neoplasia; C: IPNB’s focal carcinomatosis; D: IPNB’s correlation with invasive cancer.
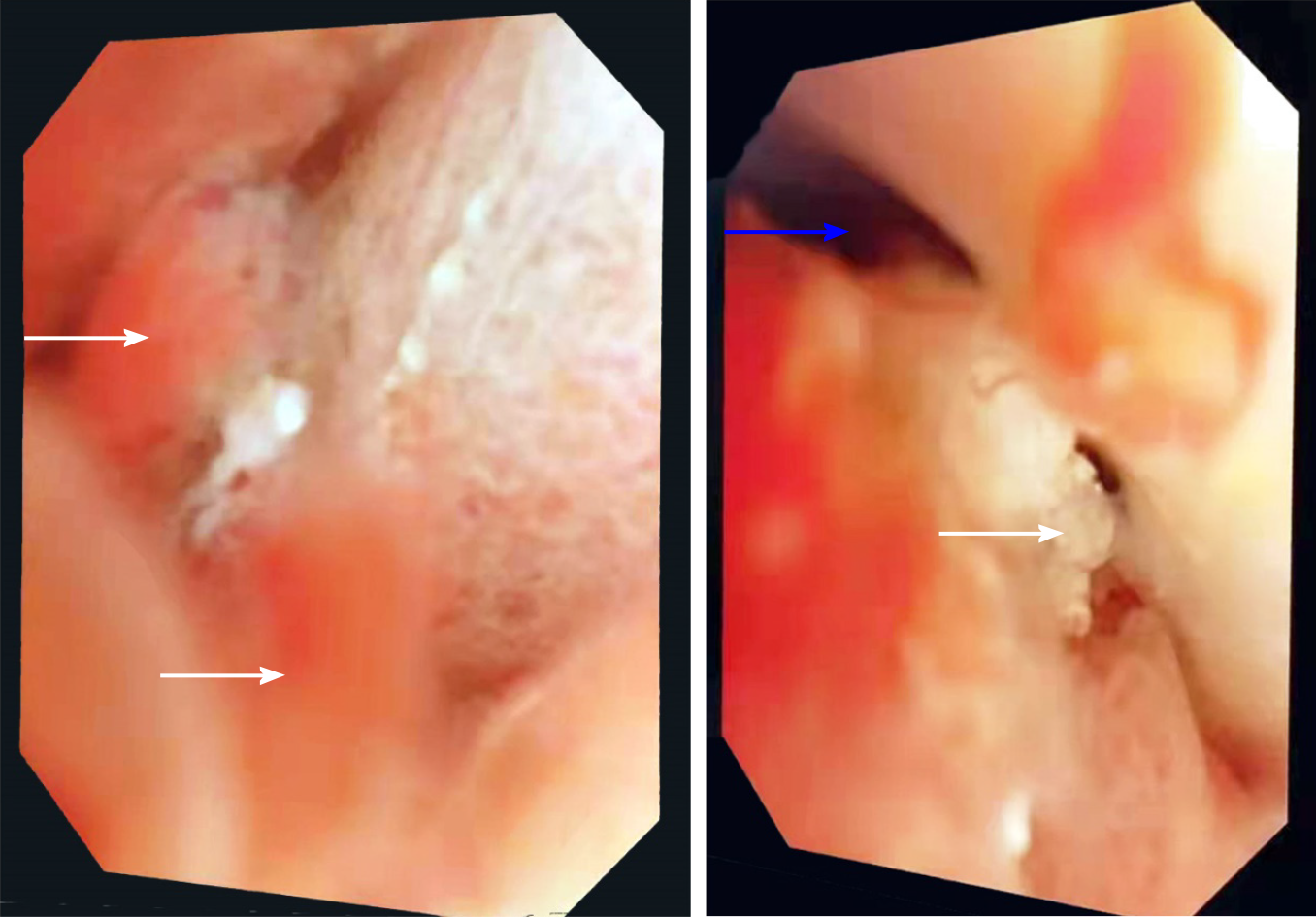
Figure 2 Choledochoscope images.
White arrows indicate papillary nodules or bulges. The blue arrow indicates that myxoid bile is attached to the bile duct wall in a strip shape.
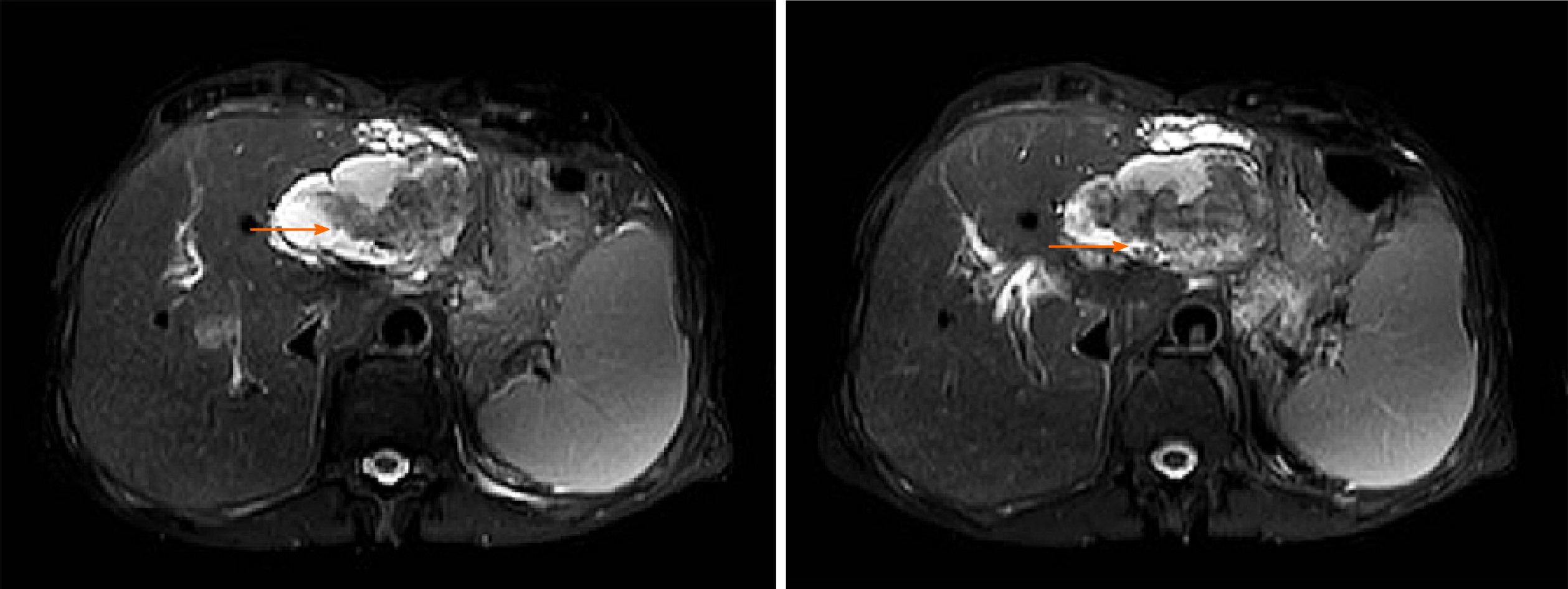
Figure 3 Magnetic resonance imaging of patients with intrahepatic bile duct papilloma.
Orange arrows indicate solid components floating in cystic lesions.
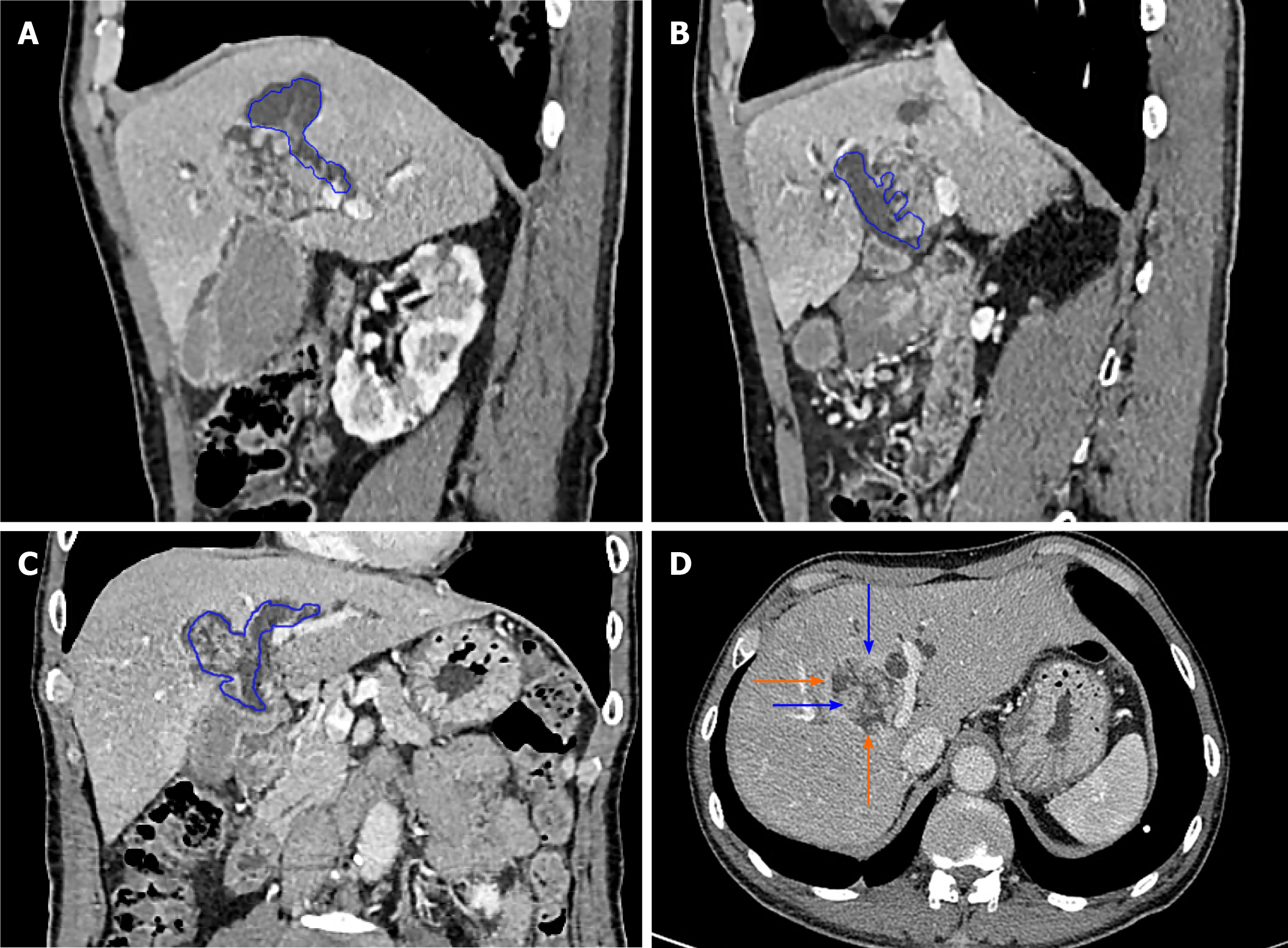
Figure 4 Intrahepatic bile duct papilloma whole abdominal plain scan and enhanced computed tomography scan.
A-C: Blue depicts that the tumour communicates with the bile duct, and bile duct dilatation can be seen; D: The orange arrow indicates a mucinous tumour, and the blue arrow indicates a mural nodule.
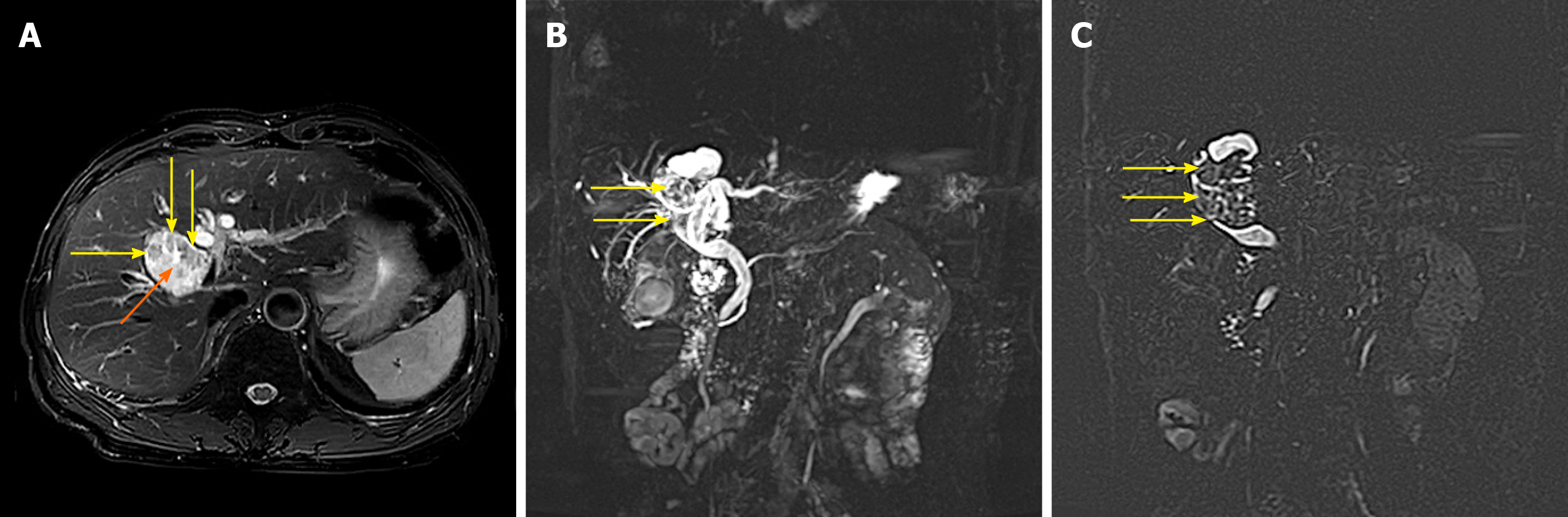
Figure 5 Magnetic resonance cholangiopancreatography images of patients with intrahepatic bile duct papilloma.
A: The tumour is cystic and solid, with a smooth wall, yellow arrow indicating a wall nodule and orange arrow indicating a mucinous tumour; B and C: The yellow arrow indicates that the tumour communicates with the bile duct.
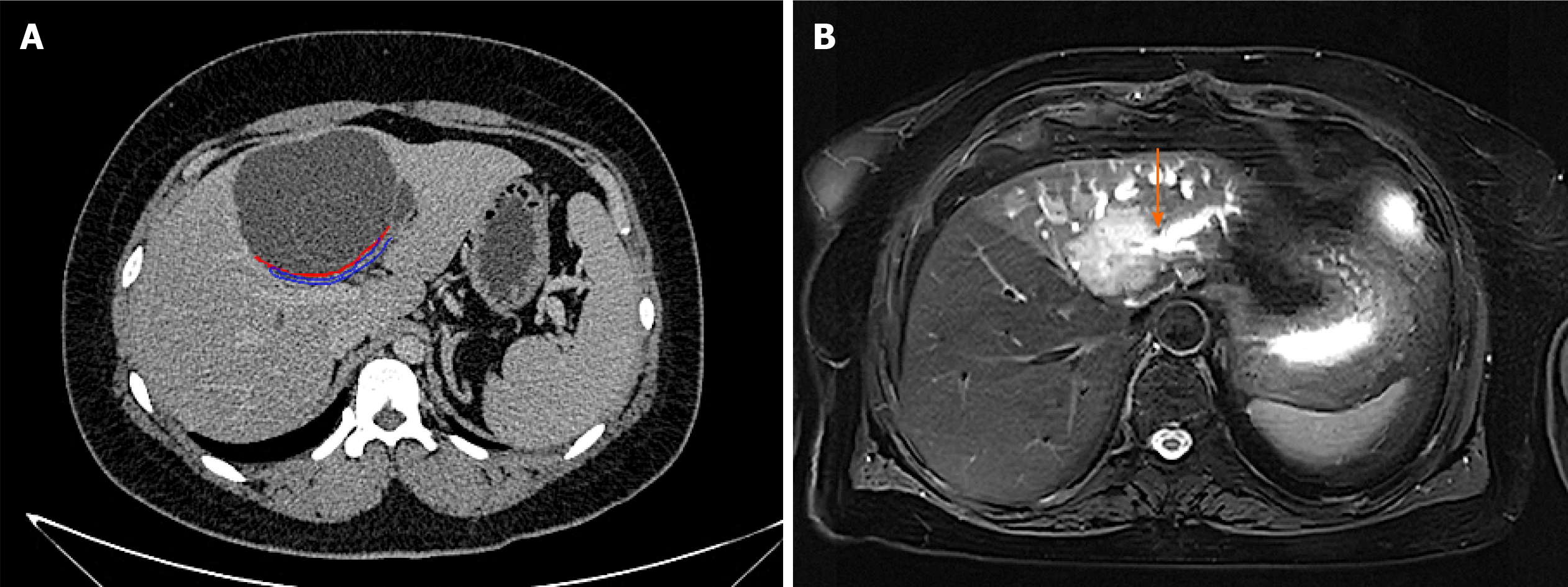
Figure 6 Differential diagnosis instructions.
A: Computed tomography image of mucinous cystic tumour of liver. It can be seen that the tumour does not communicate with bile duct. The orange arrow indicates the boundary of the tumour, and the blue arrow shows the bile duct compressed by the tumour; B: Magnetic resonance imaging image of cholangiocarcinoma. It can be seen that the boundary is not clear and smooth, and it invades into the liver, and the distal bile duct expands like a twig. The orange arrow indicates that the bile duct is out of shape and cut off at the lesion
- Citation: Yi D, Zhao LJ, Ding XB, Wang TW, Liu SY. Clinical characteristics of intrahepatic biliary papilloma: A case report. World J Clin Cases 2021; 9(13): 3185-3193
- URL: https://www.wjgnet.com/2307-8960/full/v9/i13/3185.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i13.3185