Copyright
©The Author(s) 2019.
World J Clin Cases. Sep 26, 2019; 7(18): 2687-2703
Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2687
Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2687
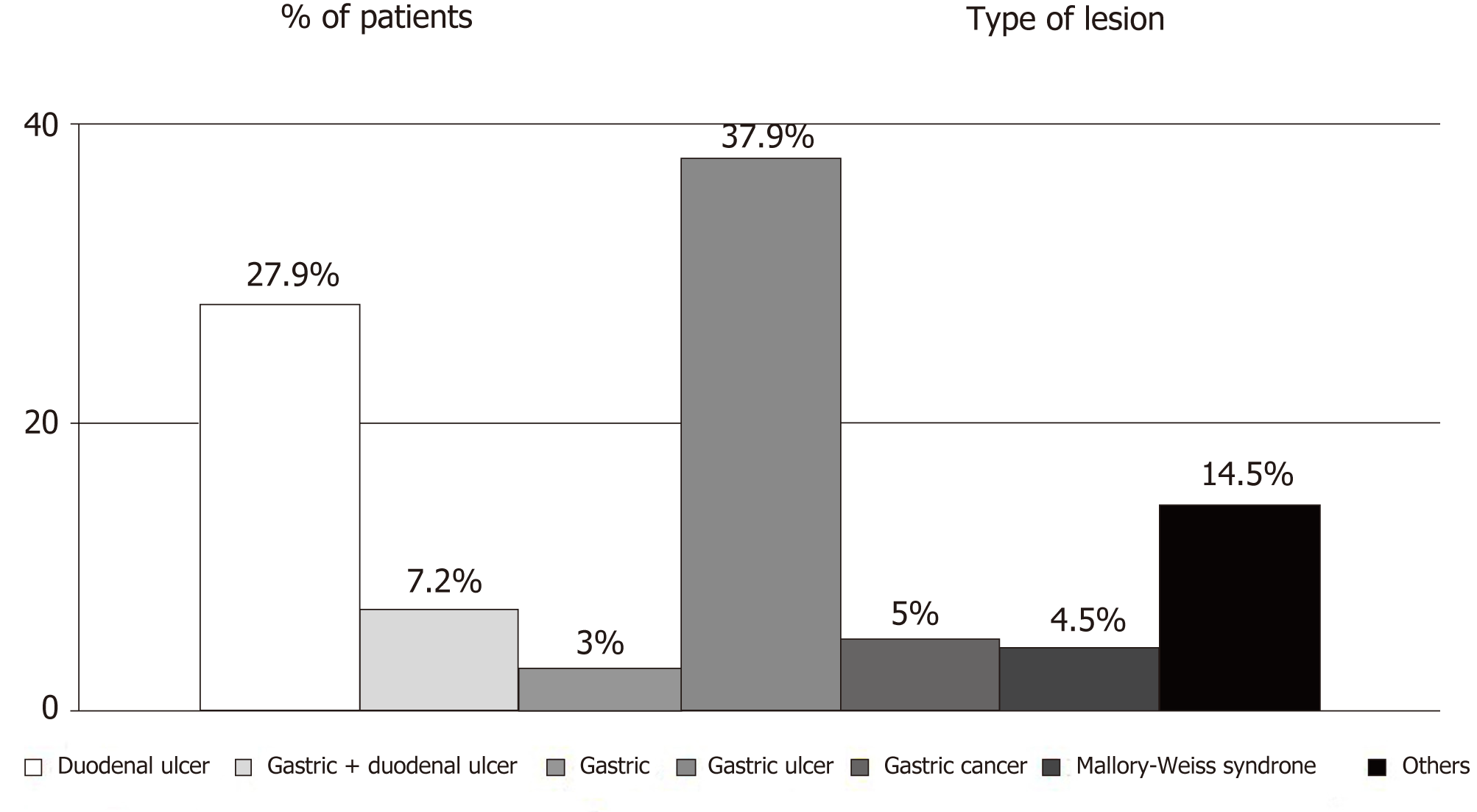
Figure 1 Etiology of non-variceal upper digestive bleeding.
Others include the following lesions: Dieulafoy lesions, duodenitis, dicumarinic overdose, pancreatic tumor invasions, telangiectasia, reflux and post-caustic esofagitis, esophageal ulcers, esophageal neoplasm, hiatal hernia, portal gastropathy, malignant ampuloma and unknown causes of bleeding.
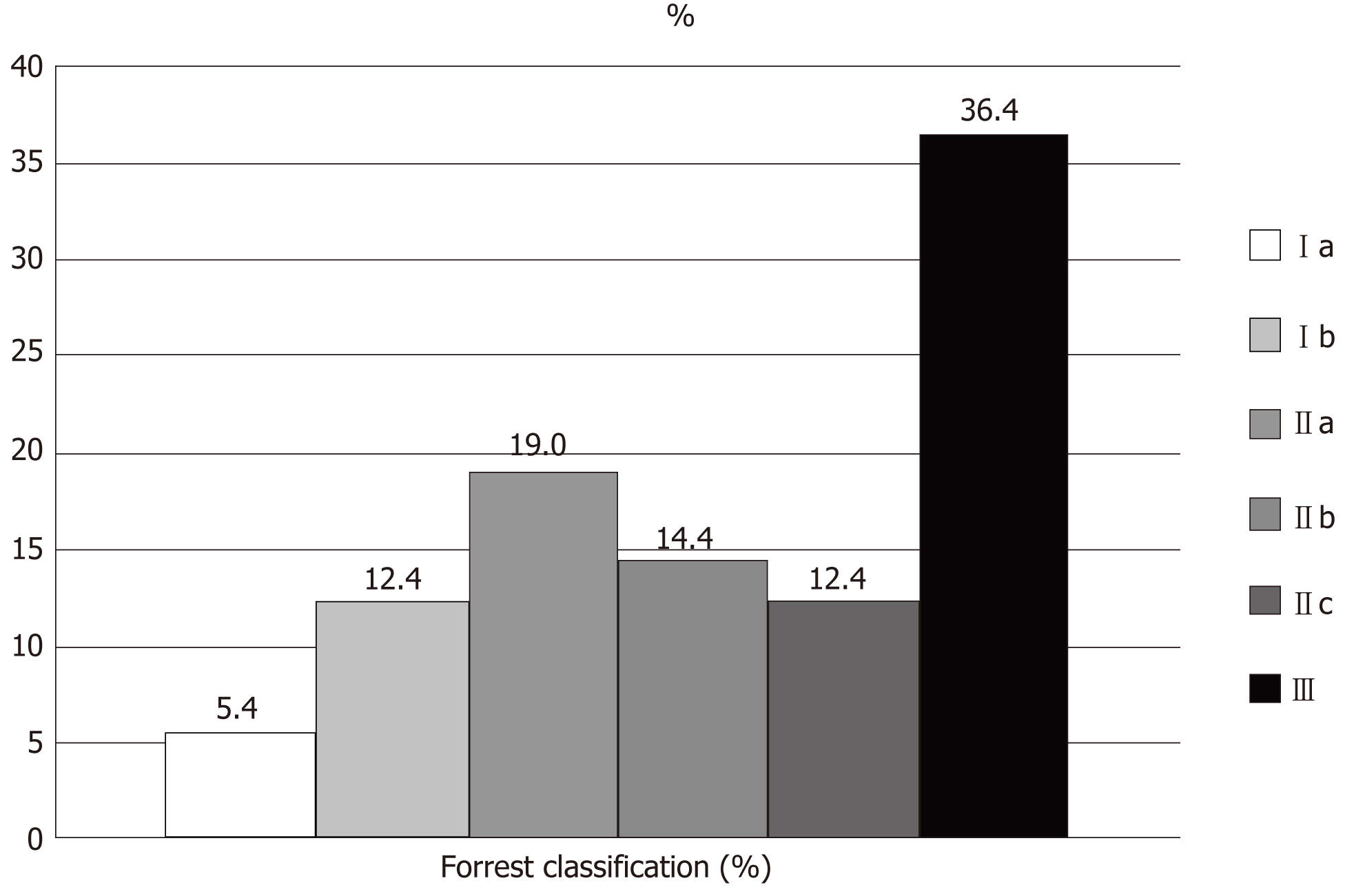
Figure 2 Endoscopic Forrest classification of upper digestive bleeding from peptic ulcers.
Ia: Active spurting; Ib: Active oozing: IIa: Non-bleeding visible vessel; IIb: Adherent clot; IIc: Flat pigmented spot; III: Clean ulcer base.
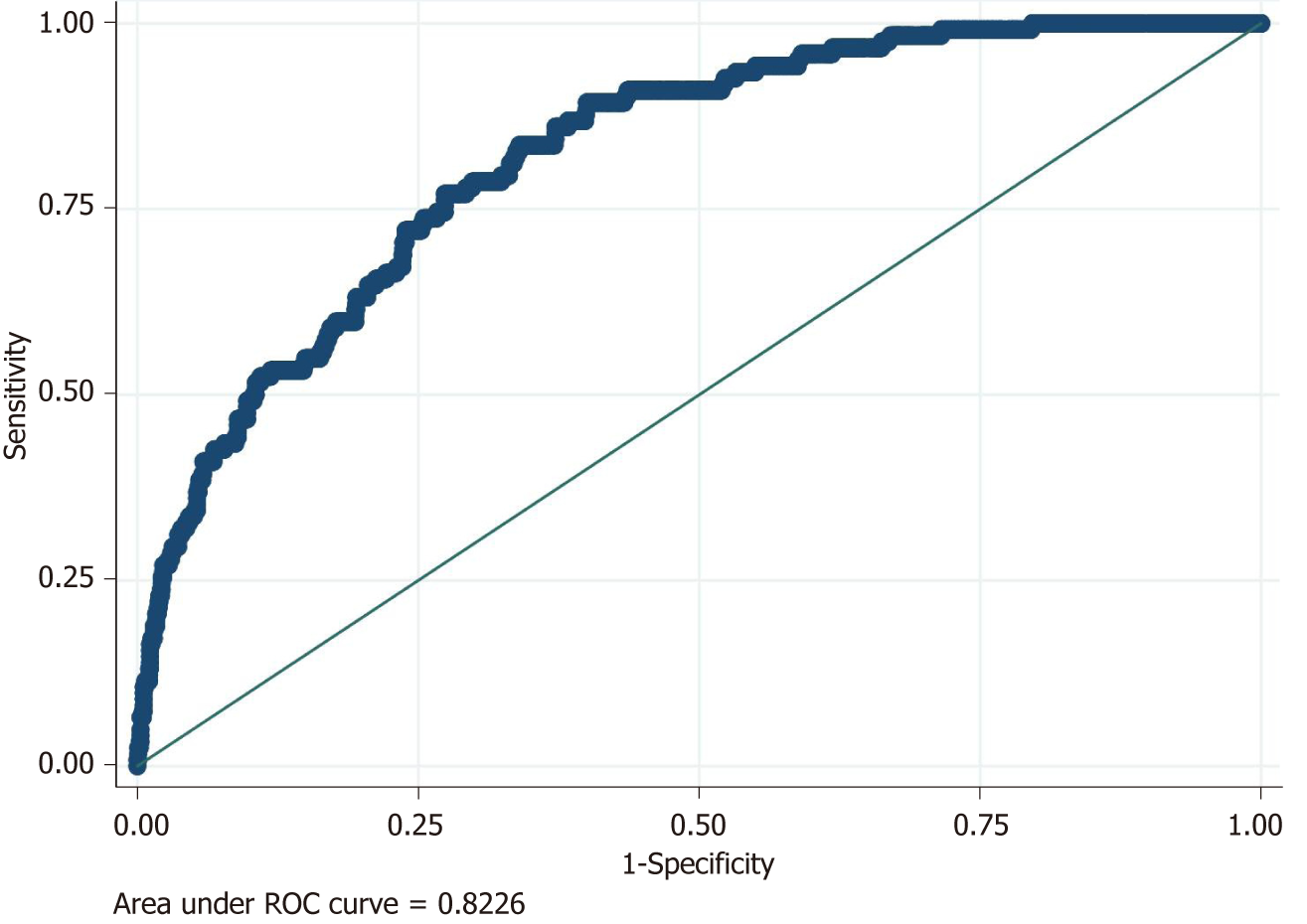
Figure 3 Logistic model for rebleeding: Accuracy of the predictive model for rebleeding using area under ROC curve (AUROC).
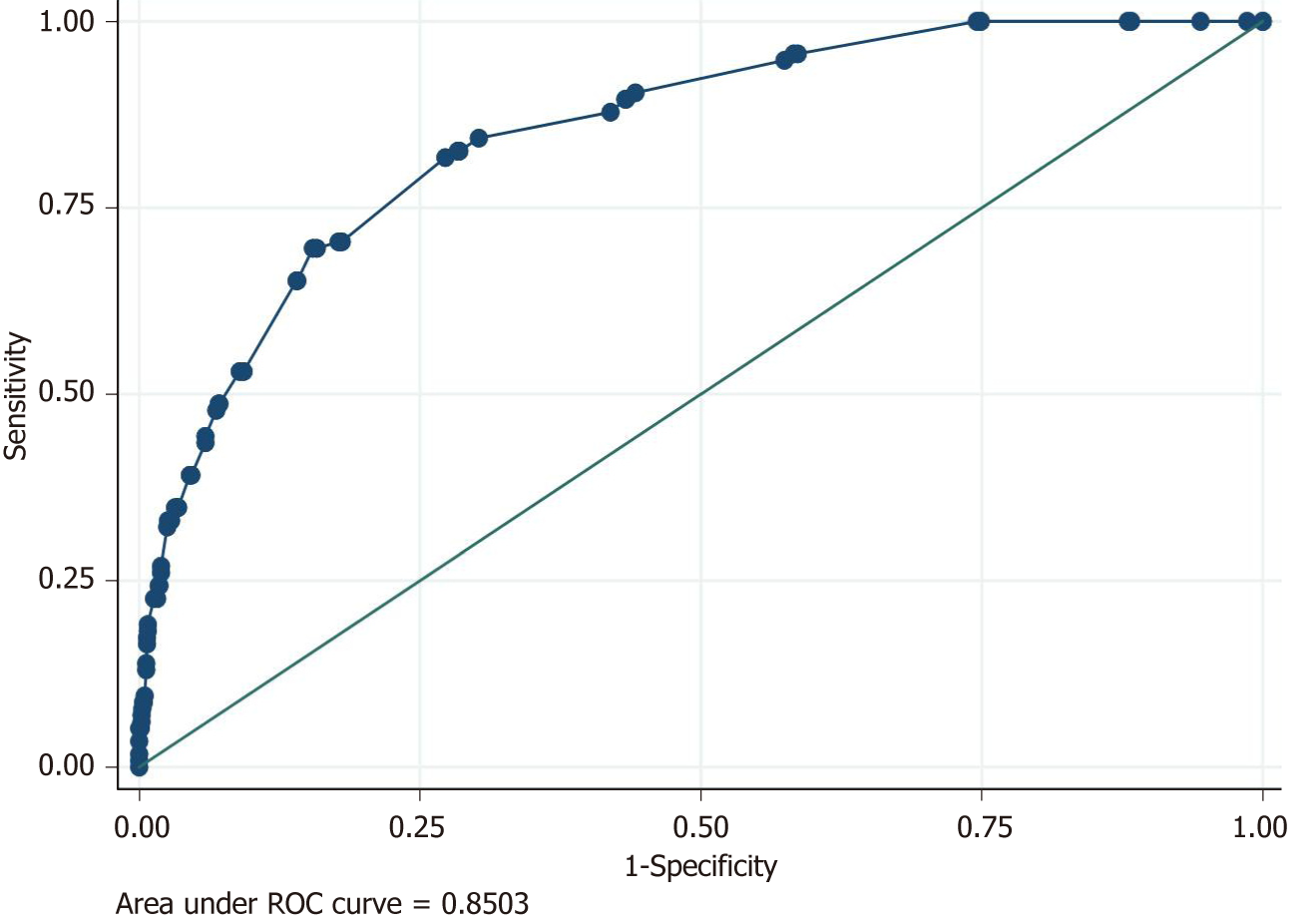
Figure 4 Logistic model for death: Accuracy of the predictive model for death using area under ROC curve (AUROC).
- Citation: Lazăr DC, Ursoniu S, Goldiş A. Predictors of rebleeding and in-hospital mortality in patients with nonvariceal upper digestive bleeding. World J Clin Cases 2019; 7(18): 2687-2703
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2687.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2687