Copyright
©The Author(s) 2024.
World J Clin Cases. Nov 26, 2024; 12(33): 6635-6643
Published online Nov 26, 2024. doi: 10.12998/wjcc.v12.i33.6635
Published online Nov 26, 2024. doi: 10.12998/wjcc.v12.i33.6635
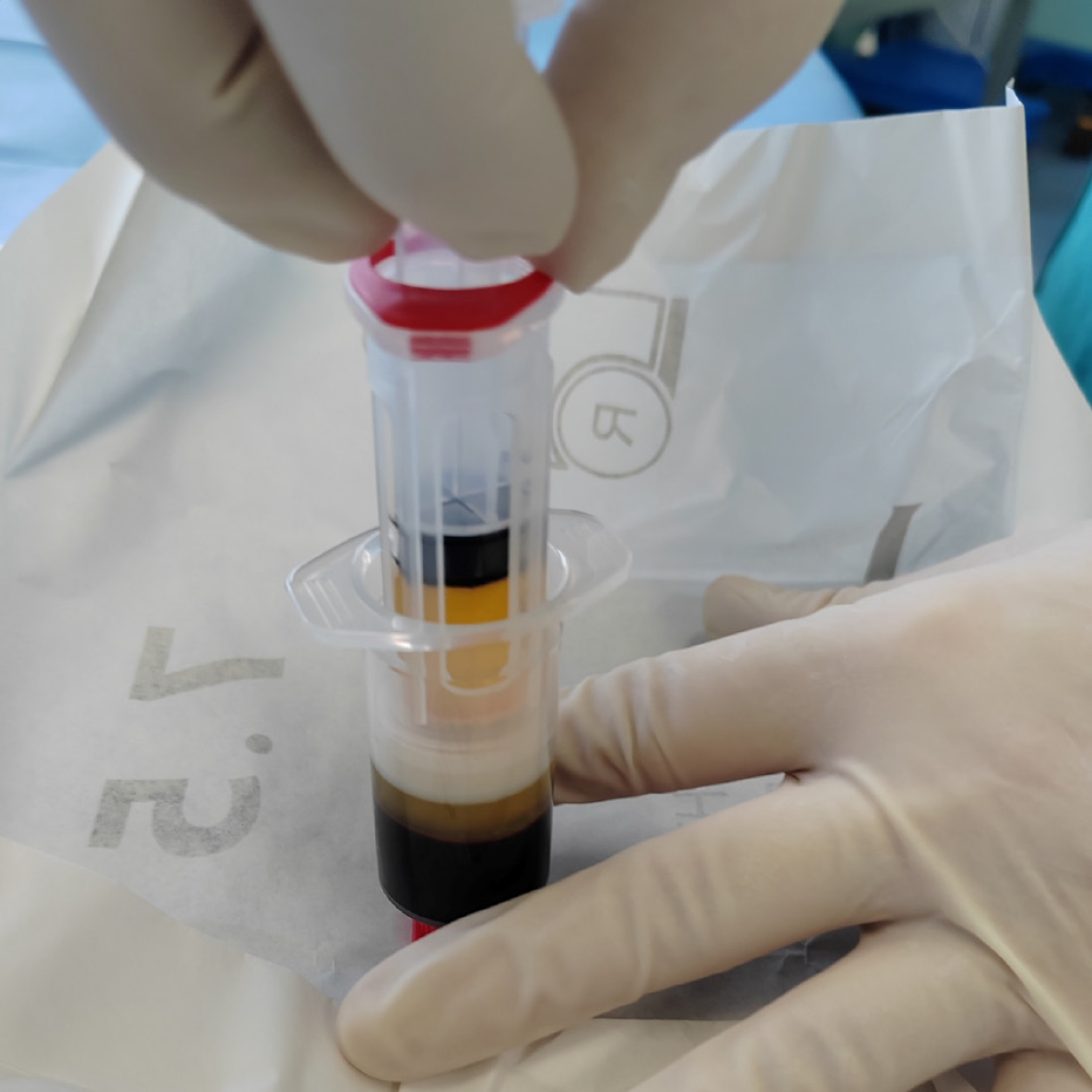
Figure 1 Platelet-rich plasma preparation technique.
After centrifugation of 15 mL venous blood taken from the patient, approximately 5–6 mL of platelet-rich plasma was obtained with the Arthrex ACP® Double-Syringe System under sterile conditions.
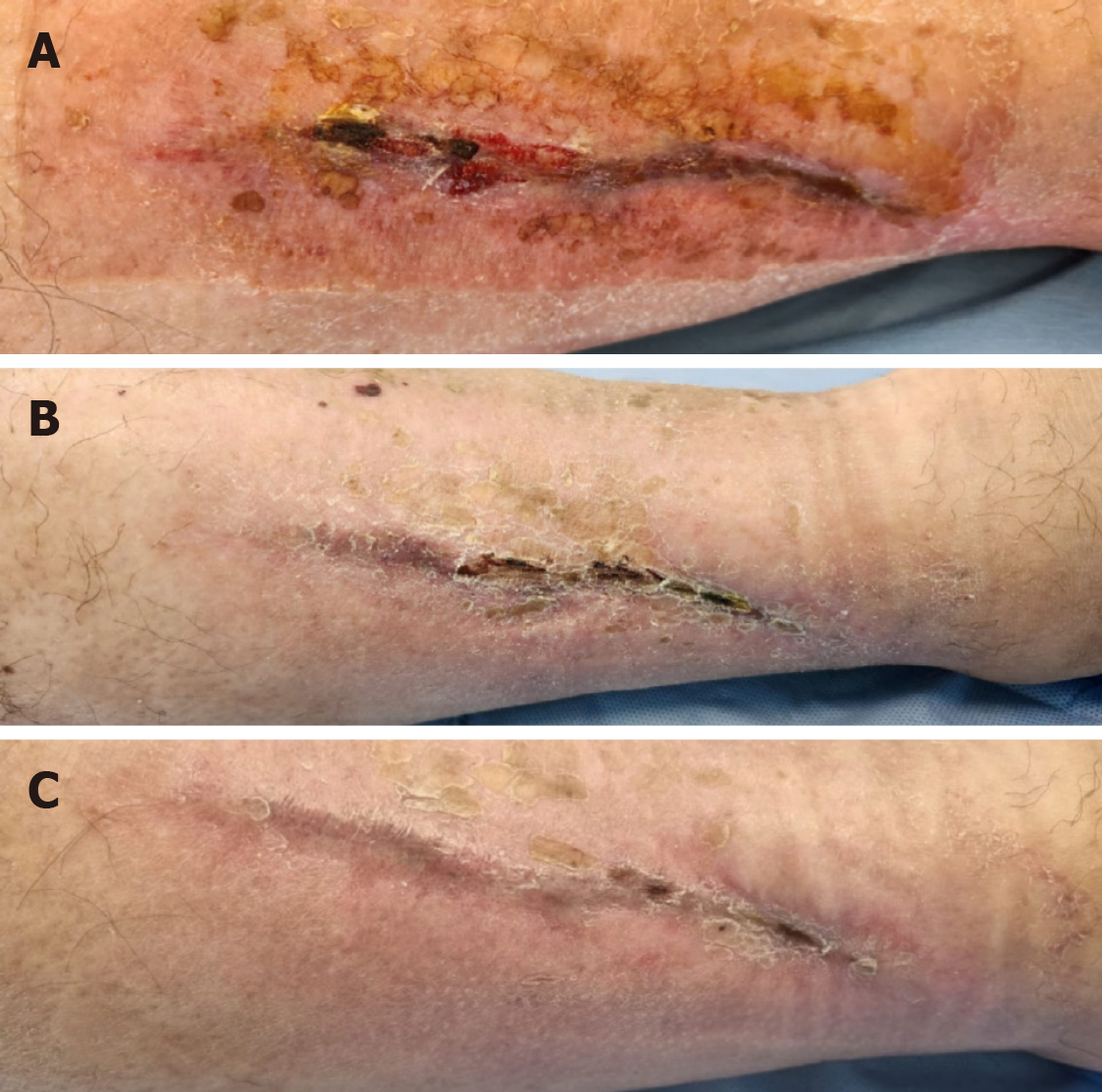
Figure 2 Wound images before and after the platelet-rich plasma treatment.
A: Wound after the microbiological swab, showing physiological flora, and immediately before the platelet-rich plasma (PRP) treatment protocol. For size reference, a sterile cloth impression measuring 20 cm × 10 cm can be seen on the skin; B: Two weeks after the first application of autologous PRP, the wound had improved and was beginning to close from the proximal portion to distal. The wound was curved and extended from the middle of the lower leg to the proximal ankle; C: Two weeks after three PRP applications, a very good healing response was seen, with almost complete closure of the wound area.
Figure 3 Healed wound at the follow-up appointment.
Six months after the third autologous platelet-rich plasma injection, at the follow-up appointment, the patient was asymptomatic with preserved skin integrity in the former wound area. The chronic wound healed with complete restitution of the epithelial layer of the skin.
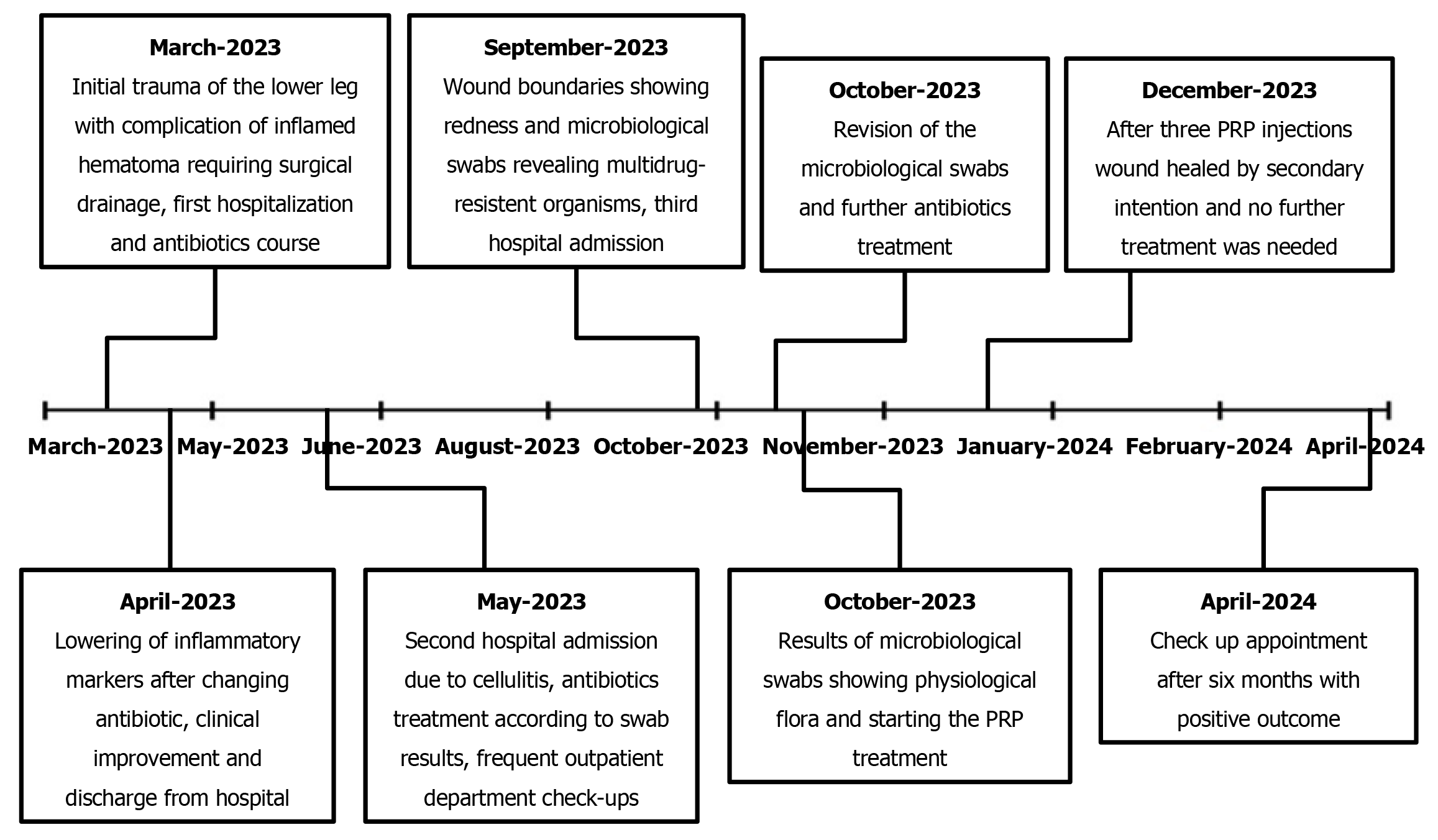
Figure 4 Case timeline.
Overview of the wound management and course of treatment. PRP: Platelet-rich plasma.
- Citation: Dimova A, Boroš M, Dimov S, Konjevod J, Svetec M. Platelet-rich plasma treatment for chronic wounds: A case report and literature review. World J Clin Cases 2024; 12(33): 6635-6643
- URL: https://www.wjgnet.com/2307-8960/full/v12/i33/6635.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i33.6635