Copyright
©The Author(s) 2024.
World J Clin Cases. Sep 26, 2024; 12(27): 6045-6056
Published online Sep 26, 2024. doi: 10.12998/wjcc.v12.i27.6045
Published online Sep 26, 2024. doi: 10.12998/wjcc.v12.i27.6045
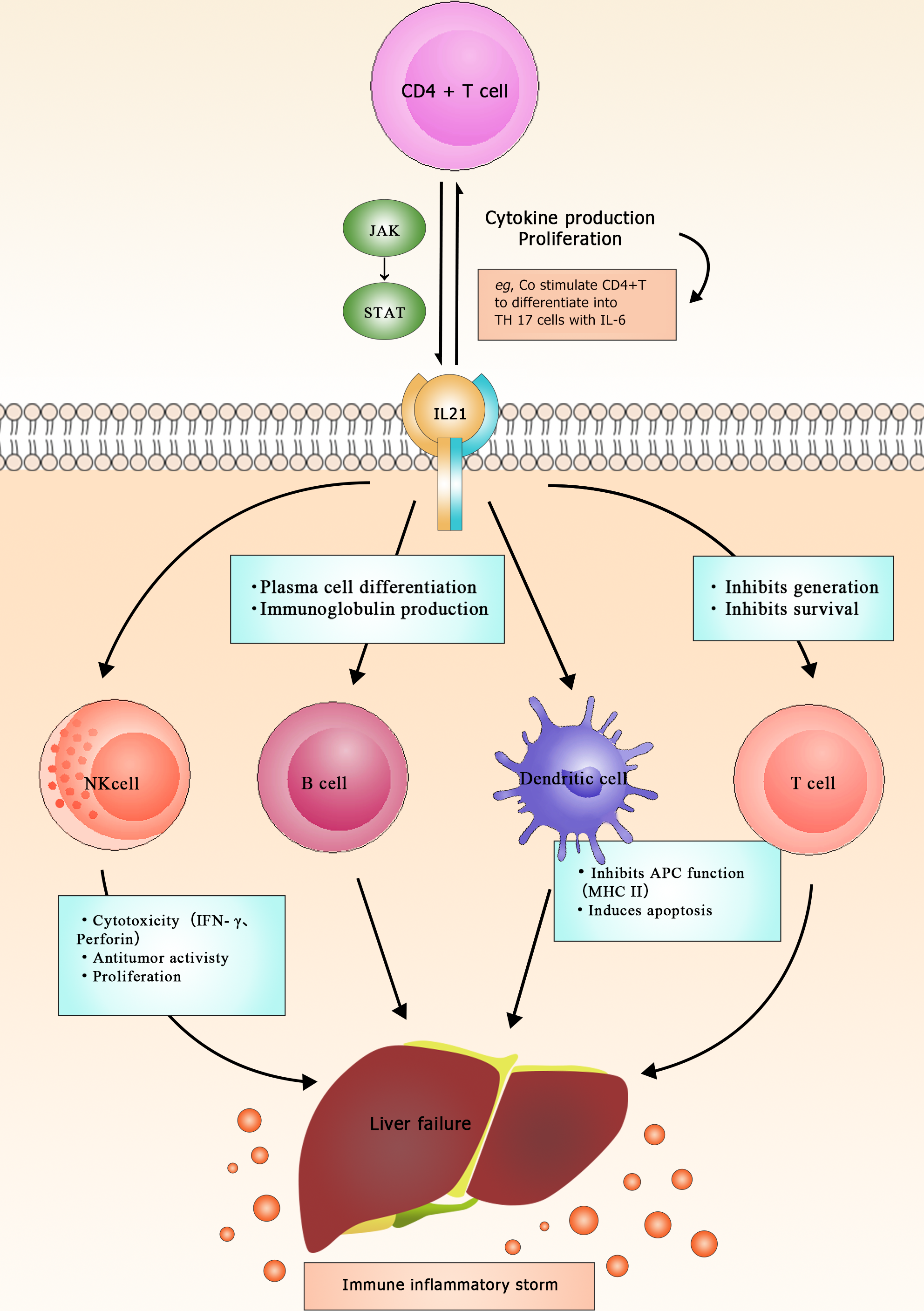
Figure 1 Mechanism of interleukin 21 in liver failure (diagram depicts various immune cells, including CD4+ T cells, natural killer cells, B cells, T cells, and dendritic cells, along with their interactions and functions).
The central role of interleukin 21 (IL-21) is highlighted, as it is secreted by CD4+ T cells and influences the differentiation of B cells into plasma cells, leading to immunoglobulin production, while also inhibiting T cell survival and generation. Additionally, IL-21 can stimulate dendritic cells to induce apoptosis, further impacting the immune response). APC: Anaphase-promoting complex; IFN-γ: Interferon gamma.
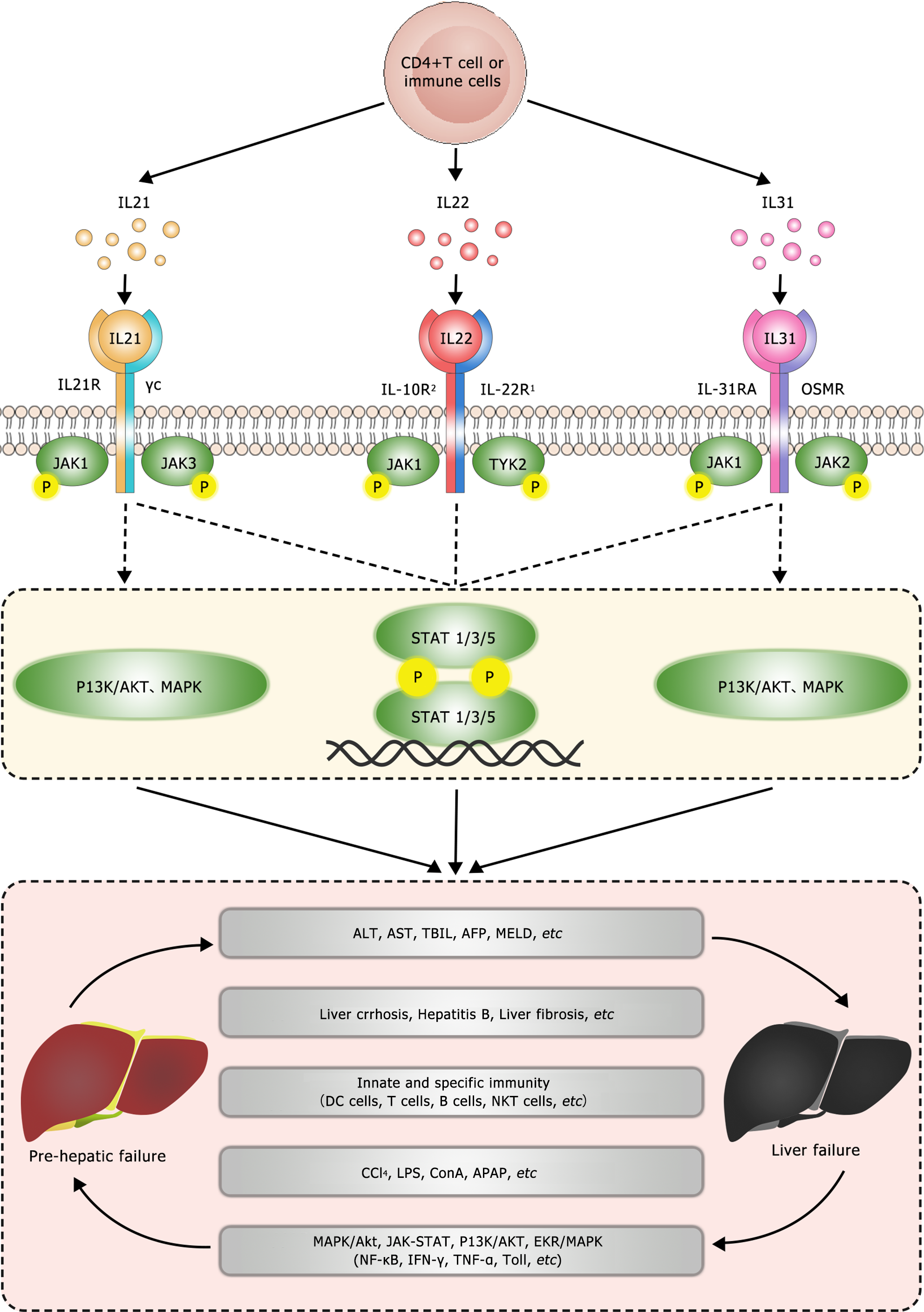
Figure 2 Molecular mechanisms underlying the involvement of interleukin 21 (IL-21), IL-22, and IL-31 in liver failure (diagram depicts the signaling pathway of ILs and their involvement in liver failure).
It starts with a CD4+ T cell or immune cell at the top, which secretes three different types of interleukin (IL): IL-21, IL-22, and IL-31. Each IL binds to its specific receptor on the cell surface: IL-21 binds to the IL-21 receptor (IL-21R), IL-22 binds to the IL-10R2 and IL-22R1, and IL-31 binds to the IL-31RA and oncostatin M receptor (OSMR). These receptors activate downstream signaling pathways involving Janus kinase 1 (JAK1), JAK2, JAK3, and tyrosine kinase 2 (TYK2), which phosphorylate signal transducer and activator of transcription (STAT) proteins. The activated STAT proteins then translocate to the nucleus and regulate gene expression, activating phosphoinositide 3-kinase (PI3K)/AKT and mitogen-activated protein kinase (MAPK) signaling pathways. The diagram shows that these signaling events ultimately lead to liver failure through various mechanisms, including increased levels of liver enzymes (alanine aminotransferase [ALT], aspartate aminotransferase [AST], total bilirubin [TBIL], alpha-fetoprotein [AFP], model for end-stage liver disease [MELD]), liver cirrhosis, hepatitis B, and liver fibrosis, which highlights the complex interplay between immune cells, ILs, and signaling pathways in the pathogenesis of liver failure.) APAP: Acetaminophen; CCl4: Carbon tetrachloride; ConA: Concanavalin A; LPS: Lipopolysaccharides.
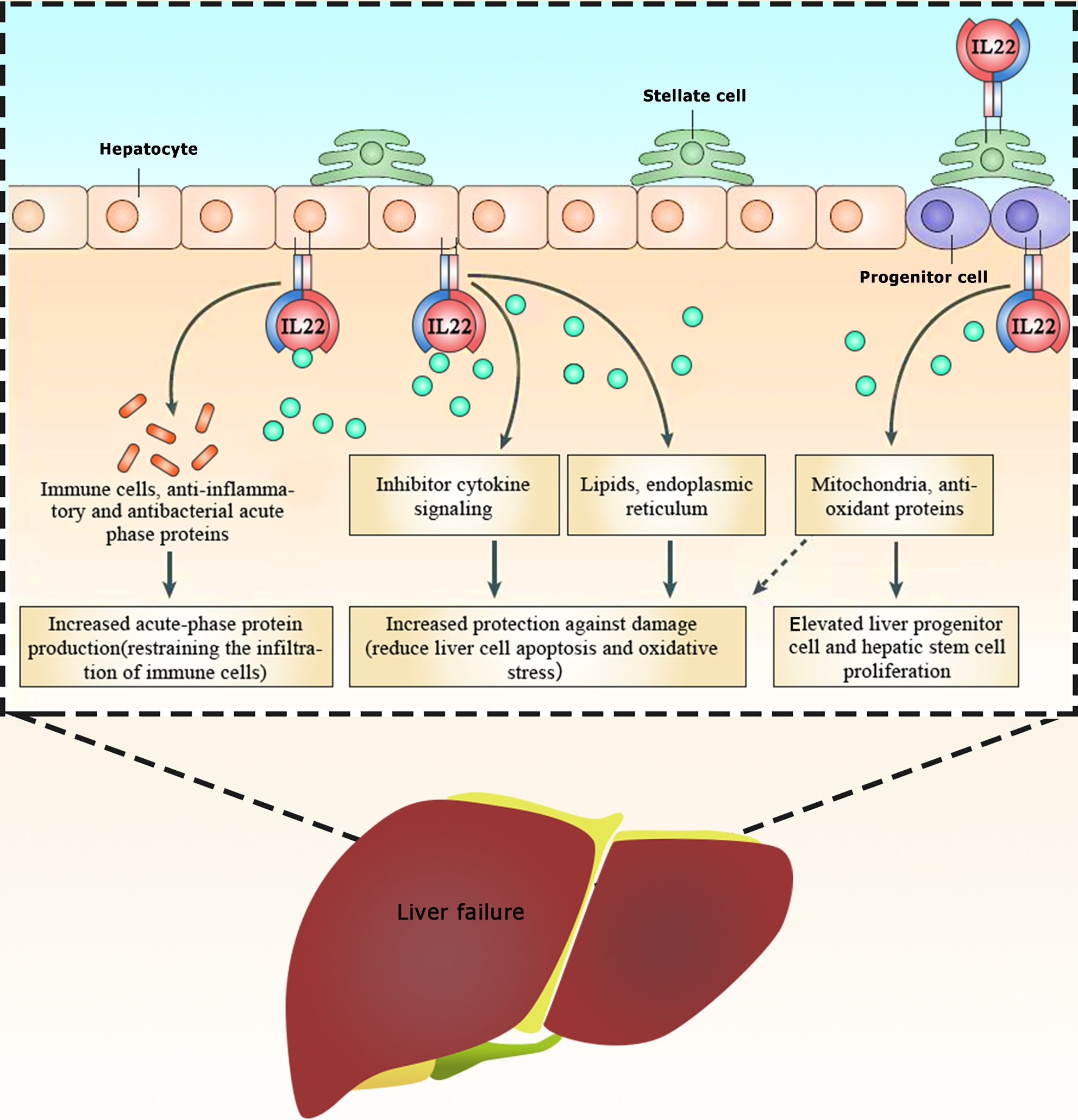
Figure 3 Mechanism of interleukin 22 (IL-22) in liver failure (diagram illustrates the protective role of IL-22 in liver health and its potential benefits in preventing liver failure).
Interleukin 22 (IL-22) is secreted by immune cells, specifically progenitor cells, and binds to receptors on the surface of hepatocytes, stellate cells, and progenitor cells. This binding triggers a series of downstream effects: (1) Hepatocytes: IL-22 acts on hepatocytes by increasing the production of acute-phase proteins, which help fight infection and inflammation. This, in turn, helps restrain the infiltration of immune cells, reducing inflammation and protecting the liver from damage; (2) Stellate cells: IL-22's interaction with stellate cells increases protection against damage and reduces liver cell apoptosis (cell death) and oxidative stress; (3) Progenitor cells: IL-22 stimulates the production of mitochondria and antioxidant proteins in progenitor cells. This promotes the proliferation of liver progenitor cells and hepatic stem cells, which are crucial for liver regeneration).
- Citation: Lin Y, Yan GJ, Liu MY, Cao Y, Zhang K, Wang N, Long FL, Mao DW. Review of the potential value of serum interleukin levels as prognostic biomarkers of liver failure. World J Clin Cases 2024; 12(27): 6045-6056
- URL: https://www.wjgnet.com/2307-8960/full/v12/i27/6045.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i27.6045