Copyright
©The Author(s) 2023.
World J Clin Cases. Mar 6, 2023; 11(7): 1498-1505
Published online Mar 6, 2023. doi: 10.12998/wjcc.v11.i7.1498
Published online Mar 6, 2023. doi: 10.12998/wjcc.v11.i7.1498
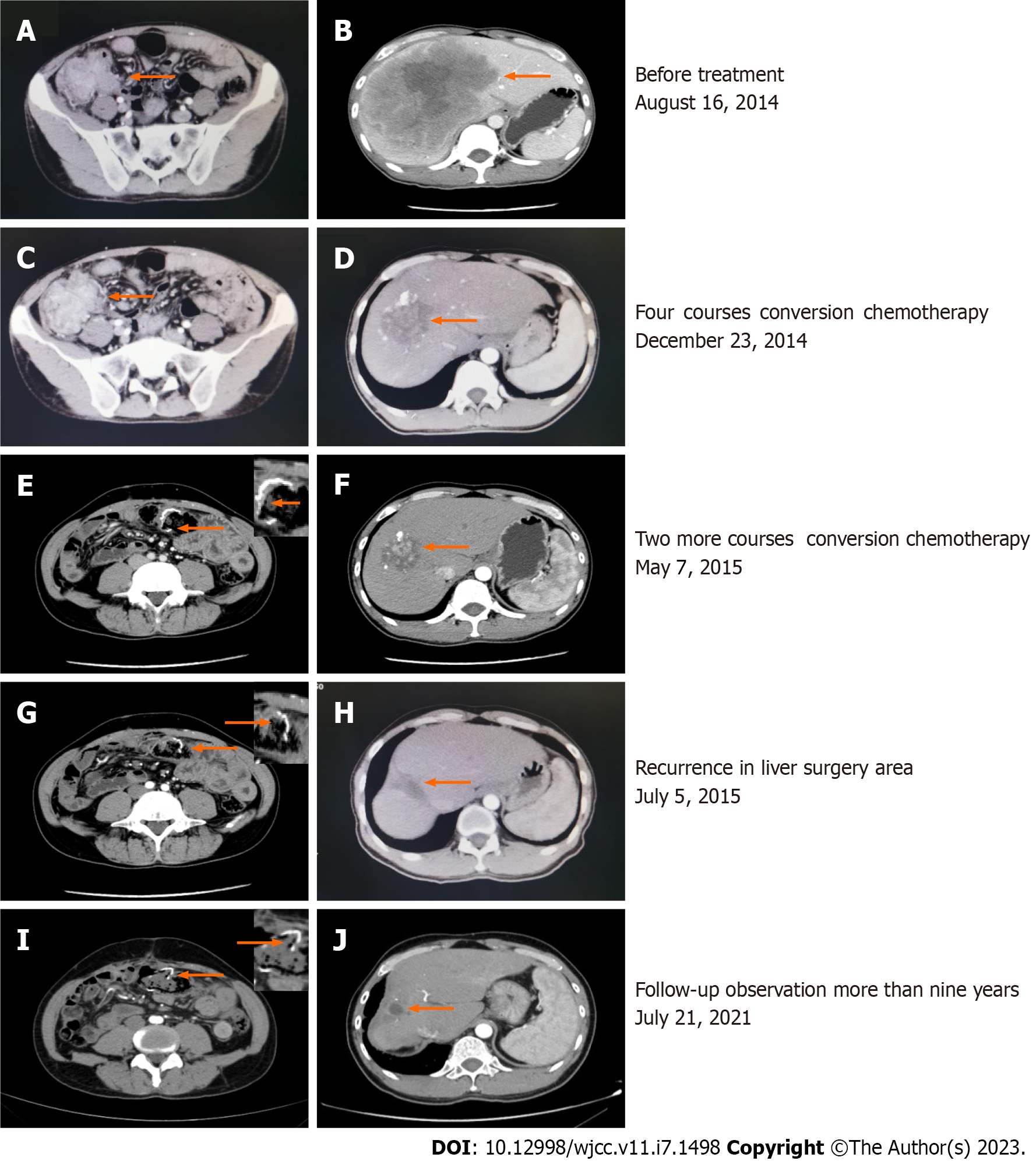
Figure 1 Enhanced computed tomography.
A: Malignant tumors in the ileocecal area and lymph nodes of varying sizes were observed adjacent to the mesangium, and metastasis was suspected; B: A huge liver metastasis in the right lobe of the liver, approximately 13.7 cm × 14.1 cm in size (arrow), with compression of the right portal vein; C and D: After four courses of treatment, the tumor in the ascending colon was not significantly reduced (6.8 to 5.4 cm), and the low-density metastatic lesion in the liver had shrunk from 14.1 to 5.9 cm; E, H, and I: The anastomosis in the colon cancer surgery area was unobstructed, and no abnormally enhanced lesions were seen; F: After another 2 cycles of conversion chemotherapy, the liver mass was significantly reduced to approximately 5.2 cm in size, with multiple lipiodol deposits on the edges; G: Residual liver parenchymal nodular enhancement in the right lobe of the liver (3.0 cm in length) that was considered a postoperative recurrence; J: A sheet-like low-density shadow was seen in the right lobe of the liver, with a size of approximately 1.6 cm × 1.5 cm, and no abnormal enhancement was observed.
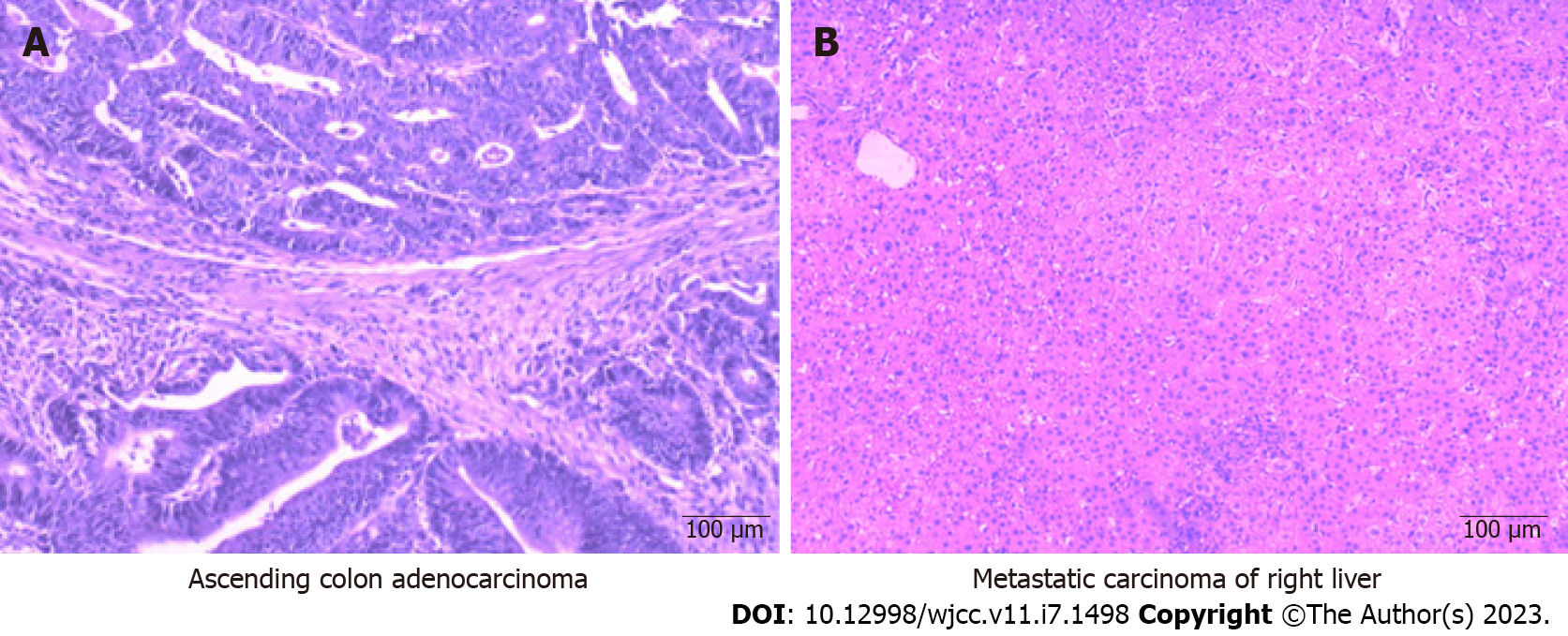
Figure 2 Hematoxylin-eosin staining (× 100).
A: The resected specimen (right colon) showed a massive moderately differentiated adenocarcinoma with necrosis. The cancer tissue invaded the entire intestinal wall and involved the nerves. Intratumoral vascular thrombosis was observed, and no cancer metastasis was seen in the peri-intestinal lymph nodes; B: The surgical resection specimen (right liver tumor) showed no cancerous cells in the liver metastasis, fibrous tissue hyperplasia, collagenous necrosis, and inflammatory cell infiltration, surrounding liver tissue congestion, hemorrhage, or inflammatory cell infiltration.
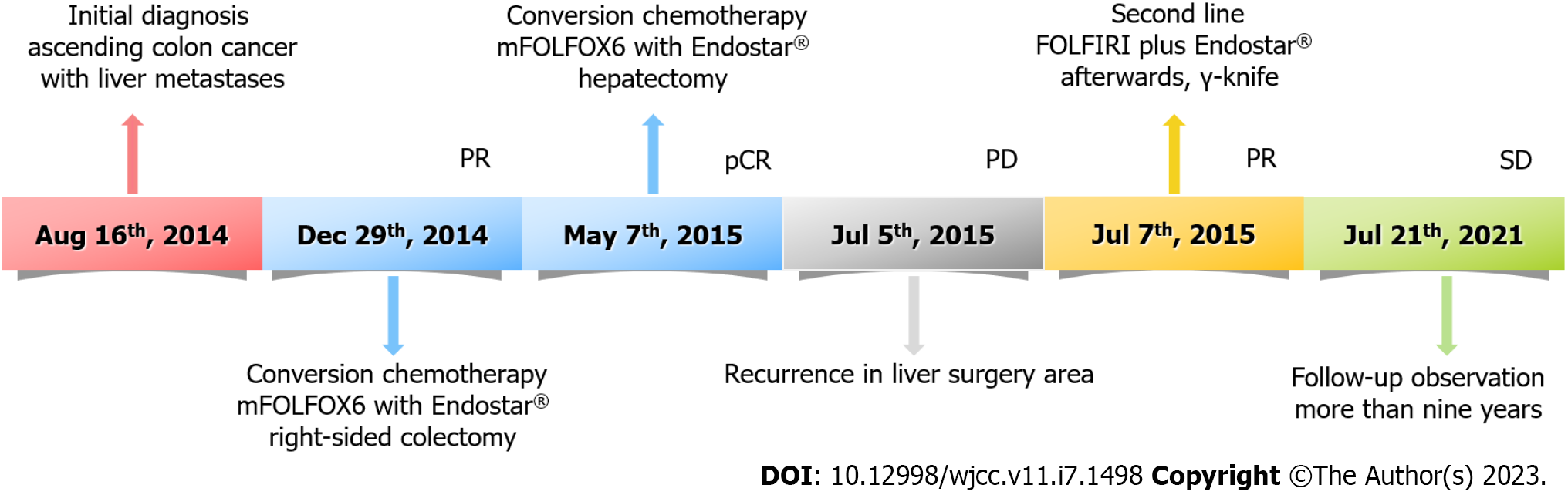
Figure 3 The timeline of treatment.
PR: Partial response; pCR: Pathologically complete response; PD: Progressive disease; SD: Stable disease; mFOLFOX6: 5-Fluorouracil/Leucovorin/oxaliplatin.
- Citation: Tan XR, Li J, Chen HW, Luo W, Jiang N, Wang ZB, Wang S. Successful multidisciplinary therapy for a patient with liver metastasis from ascending colon adenocarcinoma: A case report and review of literature. World J Clin Cases 2023; 11(7): 1498-1505
- URL: https://www.wjgnet.com/2307-8960/full/v11/i7/1498.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i7.1498