Copyright
©The Author(s) 2023.
World J Clin Cases. Apr 16, 2023; 11(11): 2567-2575
Published online Apr 16, 2023. doi: 10.12998/wjcc.v11.i11.2567
Published online Apr 16, 2023. doi: 10.12998/wjcc.v11.i11.2567
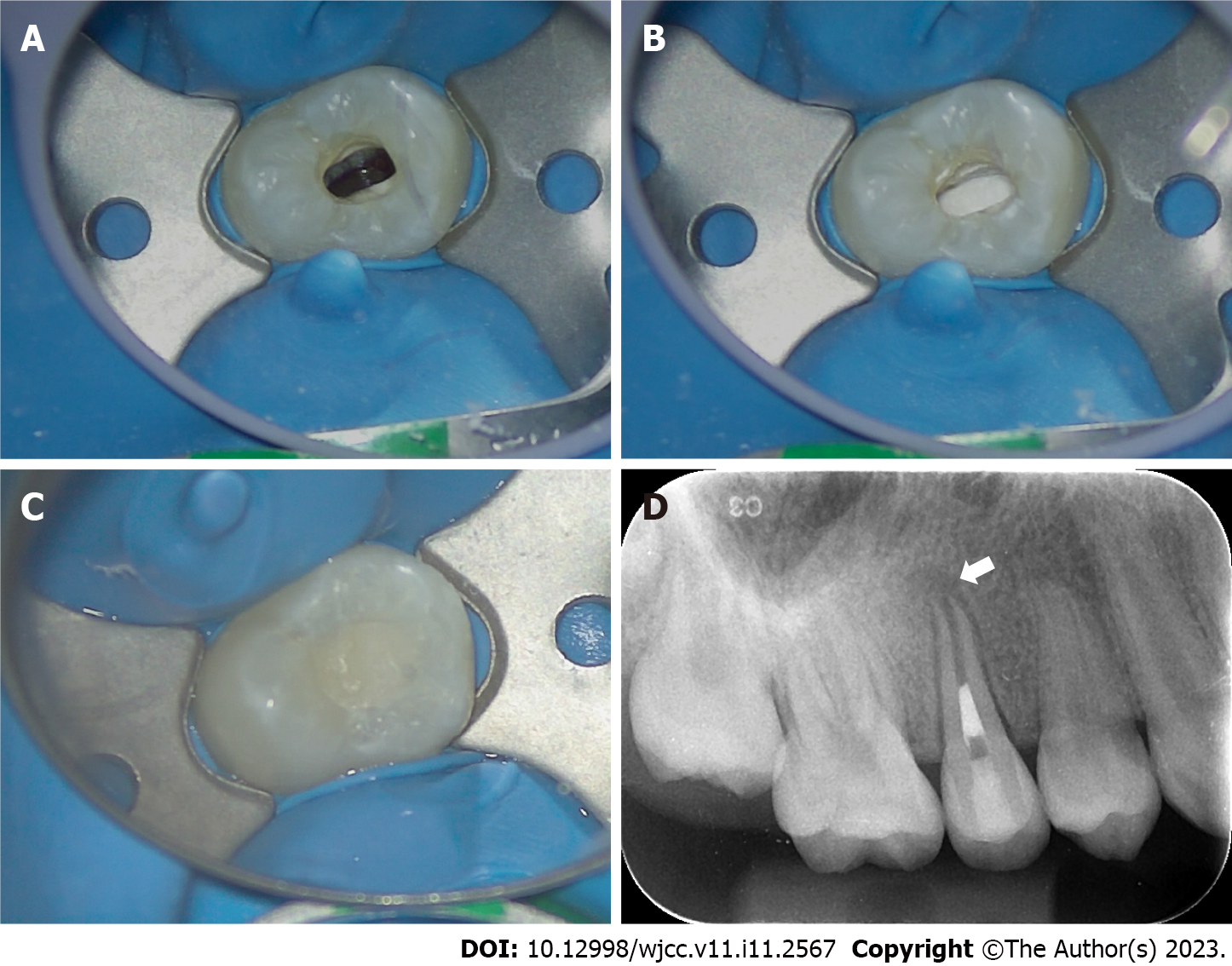
Figure 1 Preoperative photos of the right maxillary second premolar and the right mandibular second premolar.
A: Preoperative intraoral photo of the right maxillary second premolar. Note that the central cusp deformity had been polished during the patient’s last visit in another clinic, and a residual part was still visible (white arrow); B: Preoperative periapical radiograph of the right maxillary second premolar. Note that the apex of the root is open (white arrow), the root canal is wide, the dentinal wall is relatively thin (black arrow), and there is a hypodense area around the root apex; C: Preoperative periapical radiograph of the right mandibular second premolar. Note that the apex of the root is not closed (white arrow), the root canal is wide, the dentinal wall is thin (black arrow), and there is a hypodense area around the root apex.
Figure 2 Treatment process of revascularization in the right maxillary second premolar.
A: Blood filled in the root canal space after penetration of the periapical tissue by a #20 K-file; B: The coronal third of the root canal was sealed with iRoot BP plus; C: The access cavity was temporarily restored with glass ionomer cement; D: Postoperative periapical radiograph of the right maxillary second premolar. Note the obvious hypodense area around the root apex and the wide-open apex (white arrow); the root canal is wide, and the dentinal wall is relatively thin.
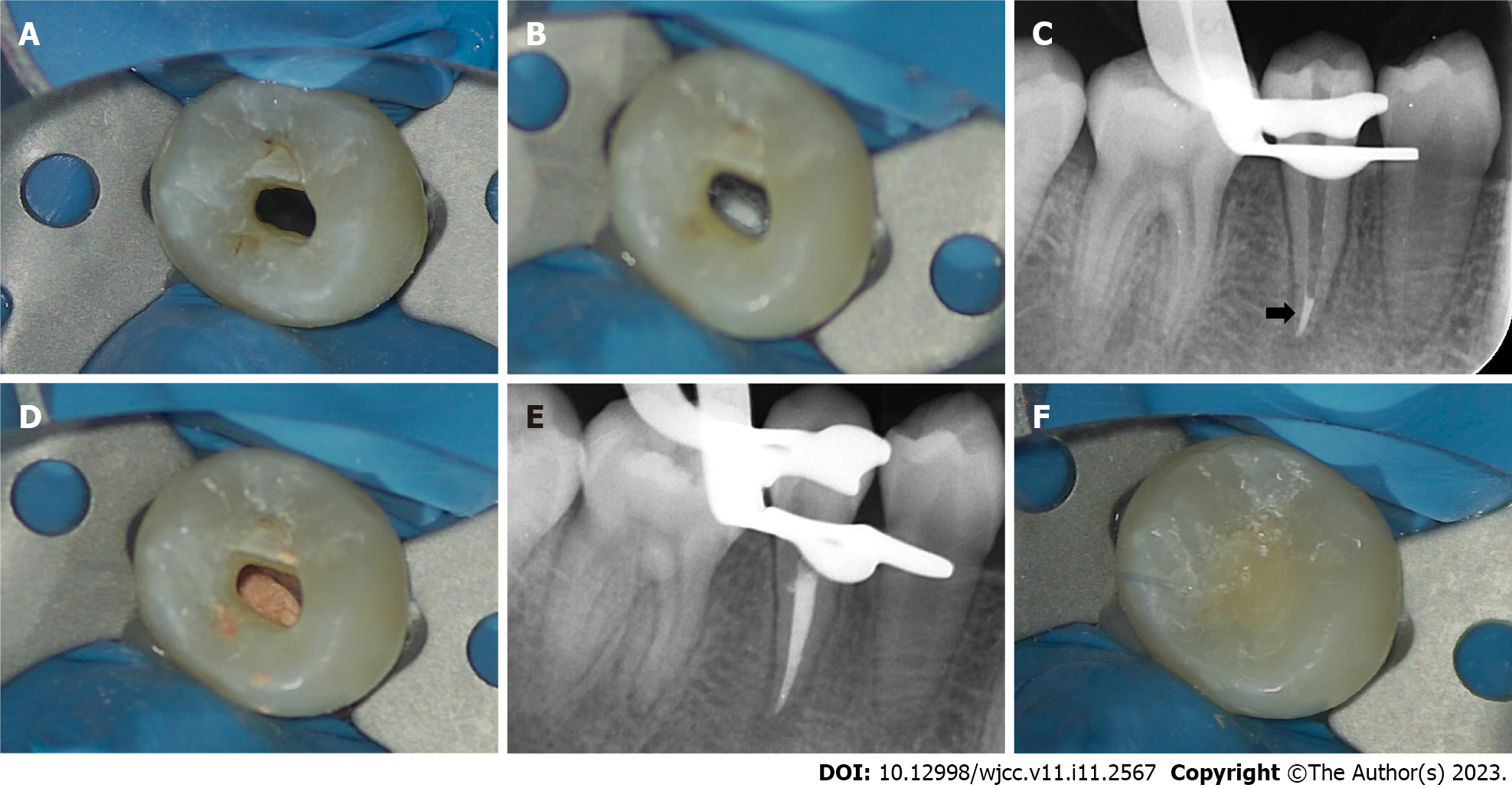
Figure 3 Treatment process of the right mandibular second premolar.
A: There was no obvious blood in the root canal after penetration of the periapical tissue by a #20 K-file; B: iRoot BP plus was placed in the apical third of the root canal and pressed tightly to form an apical barrier; C: Intraoral radiograph of the right mandibular second premolar after the placement of iRoot BP plus at the apical third of the root canal (black arrow); D and E: The coronal and middle third of the root canal was filled with hot gutta-percha; F: The access cavity was restored with light-cured composite resin.
Figure 4 Follow-up of the right maxillary second premolar.
A: 3-mo follow-up. The hypodense area around the root apex was significantly diminished, and the apex was obviously closed (white arrow); B: 6-mo follow-up. There was complete healing of the periapical hypodense area (white arrow). The thickness of the dentinal wall was slightly increased, and there seemed to be some scattered calcifications in the root canal (black arrow); C: 12-mo follow-up. The root canal was obviously narrowed, and the thickness of the dentinal wall was increased significantly (black arrow).
Figure 5 Follow-up of the right mandibular second premolar.
A: 3-mo follow-up. The hypodense area around the root apex was significantly diminished (white arrow); B: 6-mo follow-up. The periapical hypodense area was completely healed (white arrow); C: 12-mo follow-up. The periodontal ligament was narrowed (white arrow). Complete closure of the apex was observed, and there was an obvious calcification layer generated just around the apical barrier materials (black arrow).
- Citation: Chai R, Yang X, Zhang AS. Different endodontic treatments induced root development of two nonvital immature teeth in the same patient: A case report. World J Clin Cases 2023; 11(11): 2567-2575
- URL: https://www.wjgnet.com/2307-8960/full/v11/i11/2567.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i11.2567