Copyright
©The Author(s) 2022.
World J Clin Cases. Oct 16, 2022; 10(29): 10713-10720
Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10713
Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10713
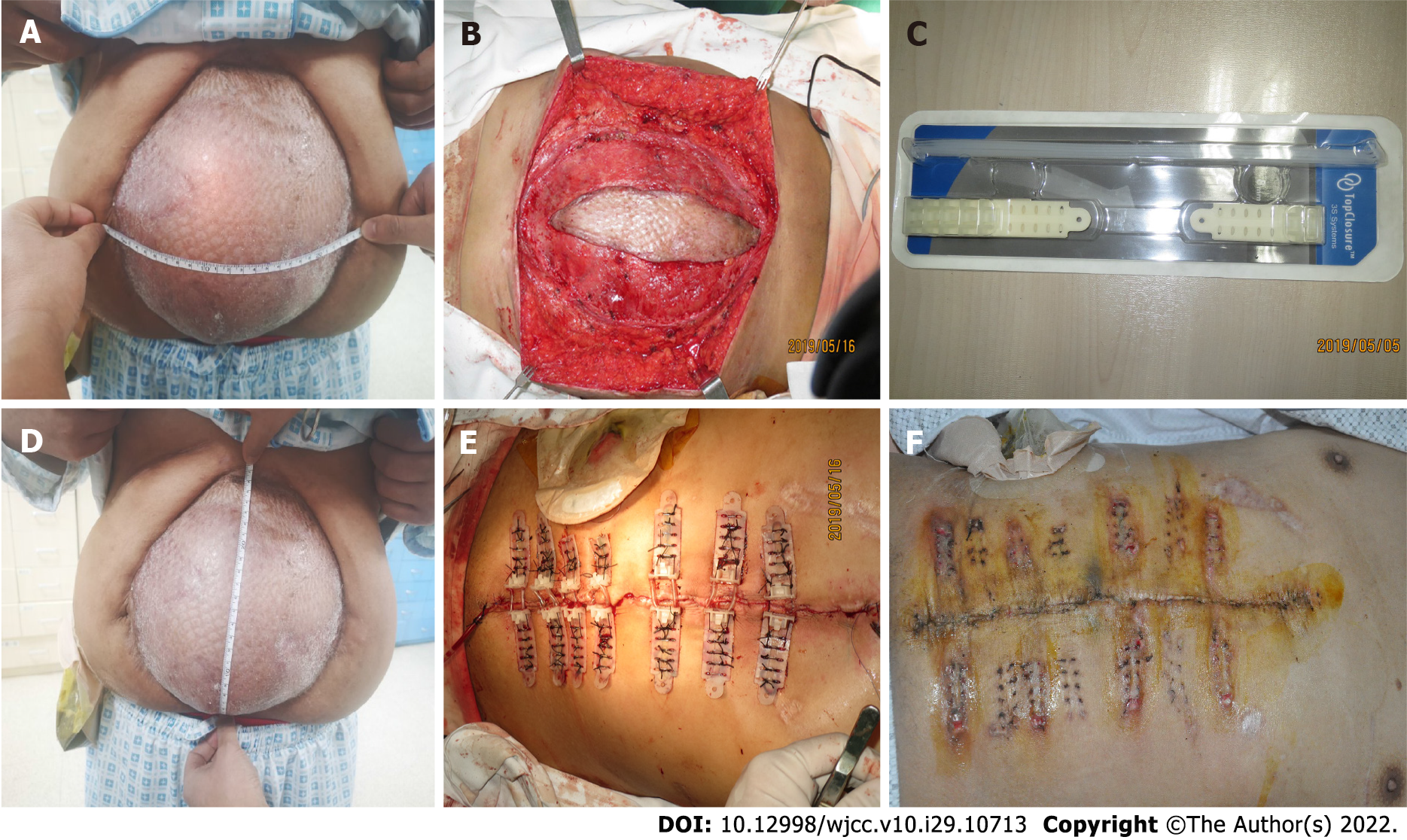
Figure 1 The patient’s first preoperative, intraoperative, and postoperative conditions in our department.
A: Length of the abdominal bulge when the patient was standing; B: Width of the abdominal bulge when the patient was standing; C: Grafted skin of the abdomen was carefully removed; D: Immediate primary closure was achieved, utilizing 7 Top Closure® and 8 mm sets; E: Top Closure® 1S 8 mm sets; F: Tension Relief System was removed 3 wk after installation.
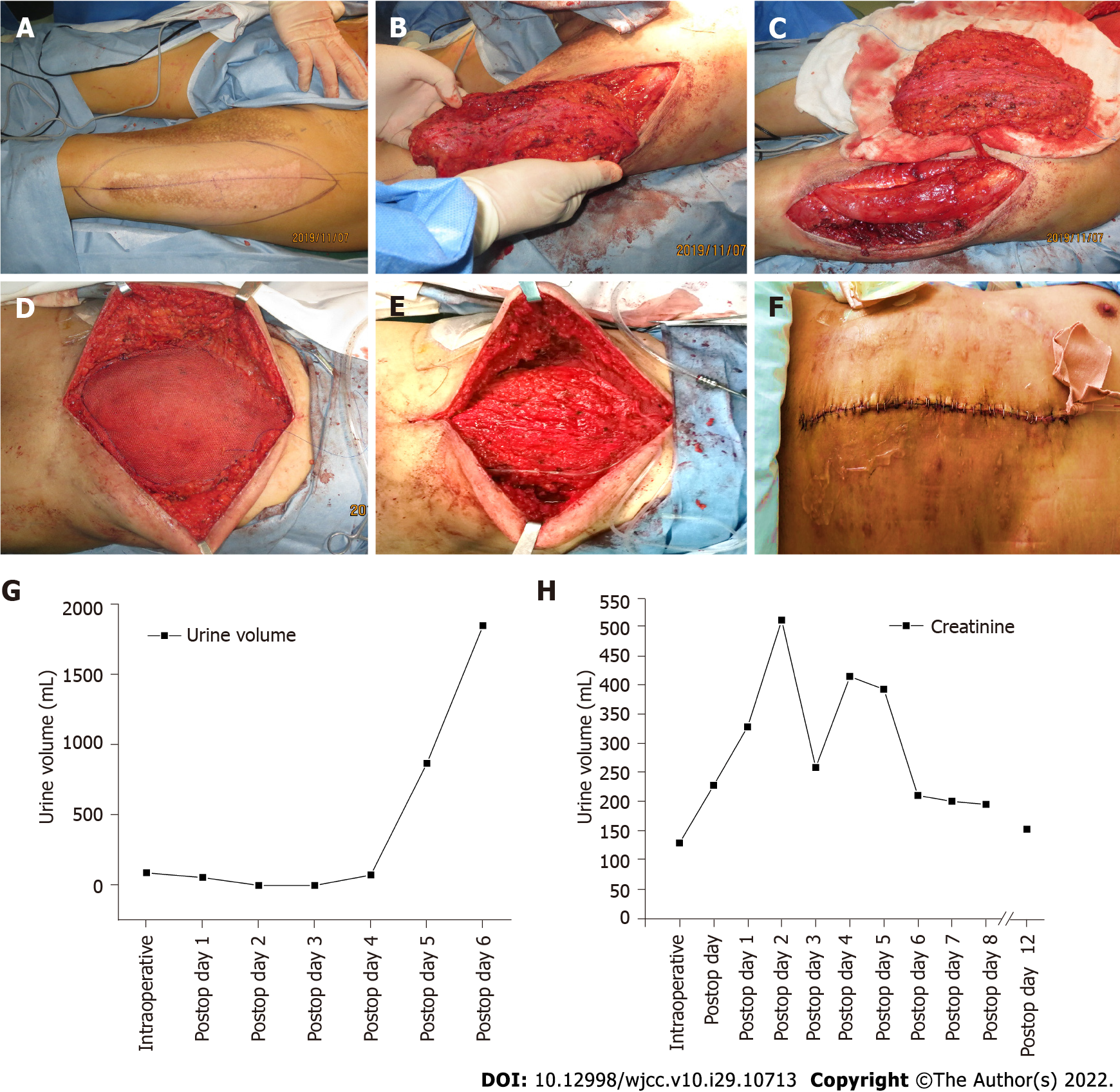
Figure 2 The patient’s surgical procedure and the dynamic changes in biochemical indicators.
A: The anterolateral thigh perforator (ALT) flap was designed preoperatively according to the size of the defect in the recipient area; B: The skin and subcutaneous tissue were incised and the ALT flap was separated from the surrounding tissue; C: The ALT flap was freed and the tip was broken; D: Mesh was used to reinforce the abdominal wall hernia; E: ALT flap was grafted to the abdomen and vascular anastomosis was performed; F: The abdominal wound was closed and the abdominal skin was sutured; G: The patient’s volume of urine changes over time; H: The patient’s creatinine values over time.
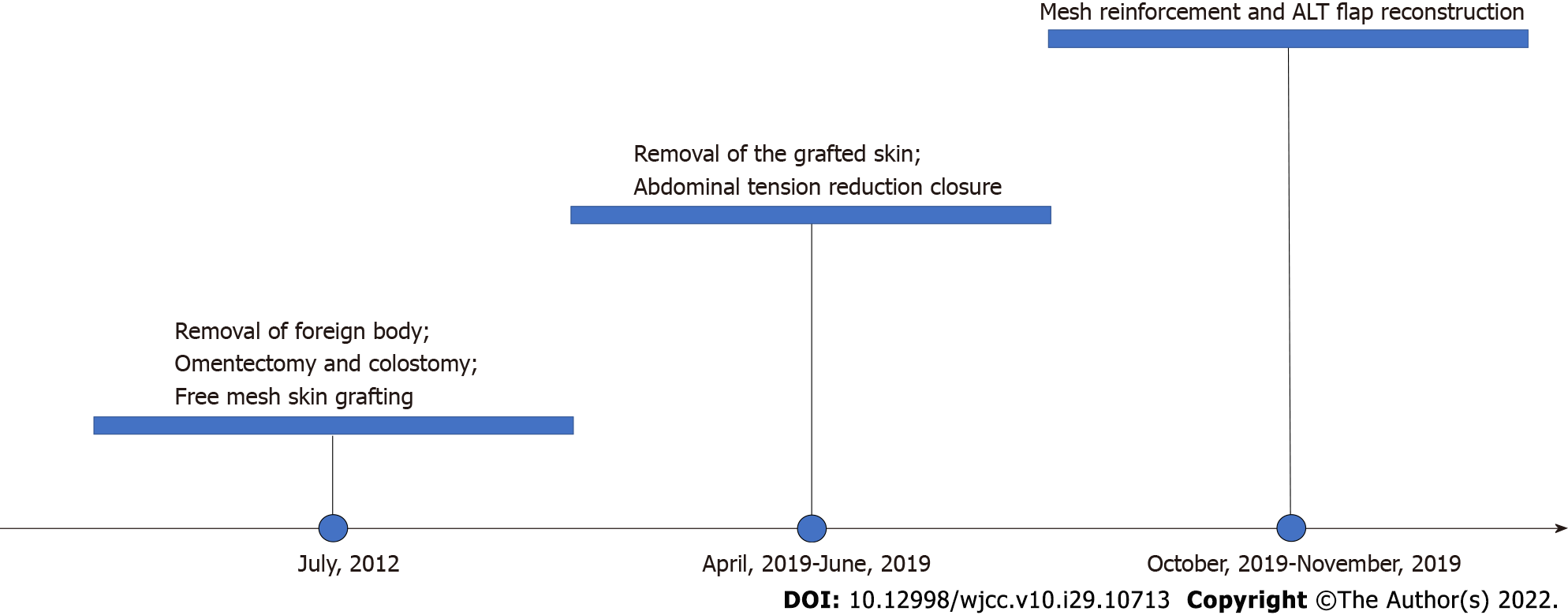
Figure 3 Timeline of treatment events.
ALT: Anterolateral thigh perforator.
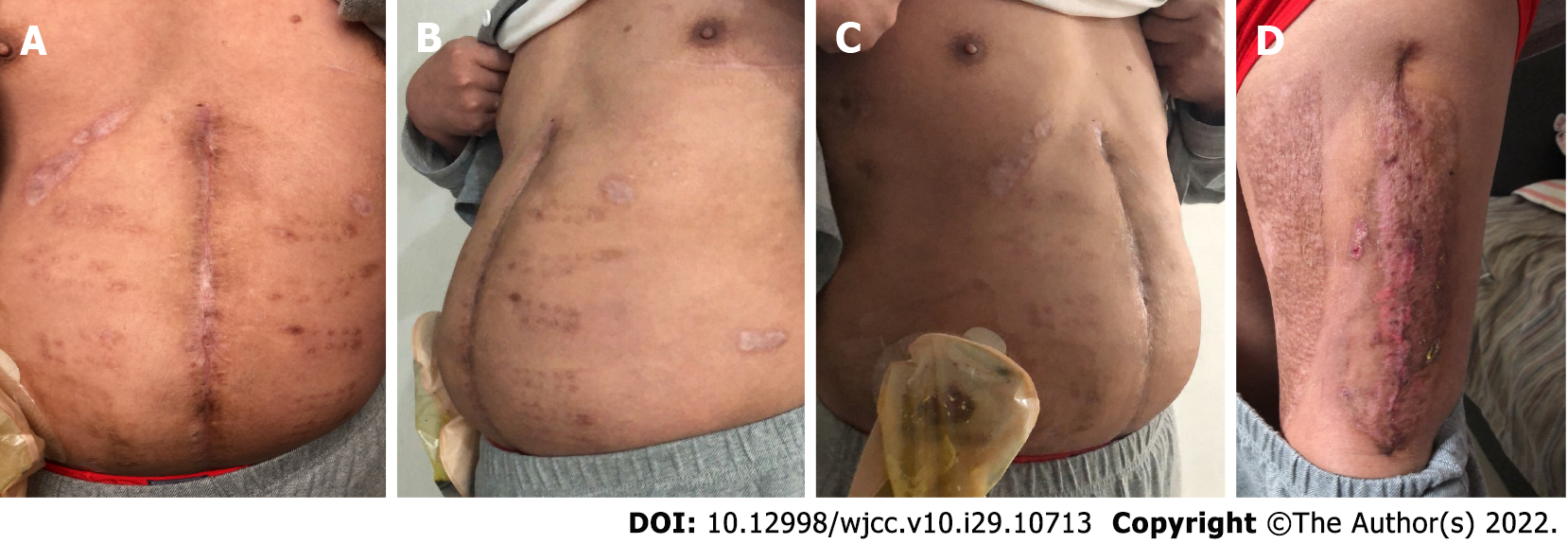
Figure 4 One year following surgery, the patient recovered well and reported significant improvement in quality of life without signs of hernial recurrence.
- Citation: Li Y, Xing JH, Yang Z, Xu YJ, Yin XY, Chi Y, Xu YC, Han YD, Chen YB, Han Y. Tension-reduced closure of large abdominal wall defect caused by shotgun wound: A case report. World J Clin Cases 2022; 10(29): 10713-10720
- URL: https://www.wjgnet.com/2307-8960/full/v10/i29/10713.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i29.10713