Copyright
©The Author(s) 2022.
World J Clin Cases. Sep 26, 2022; 10(27): 9828-9833
Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9828
Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9828
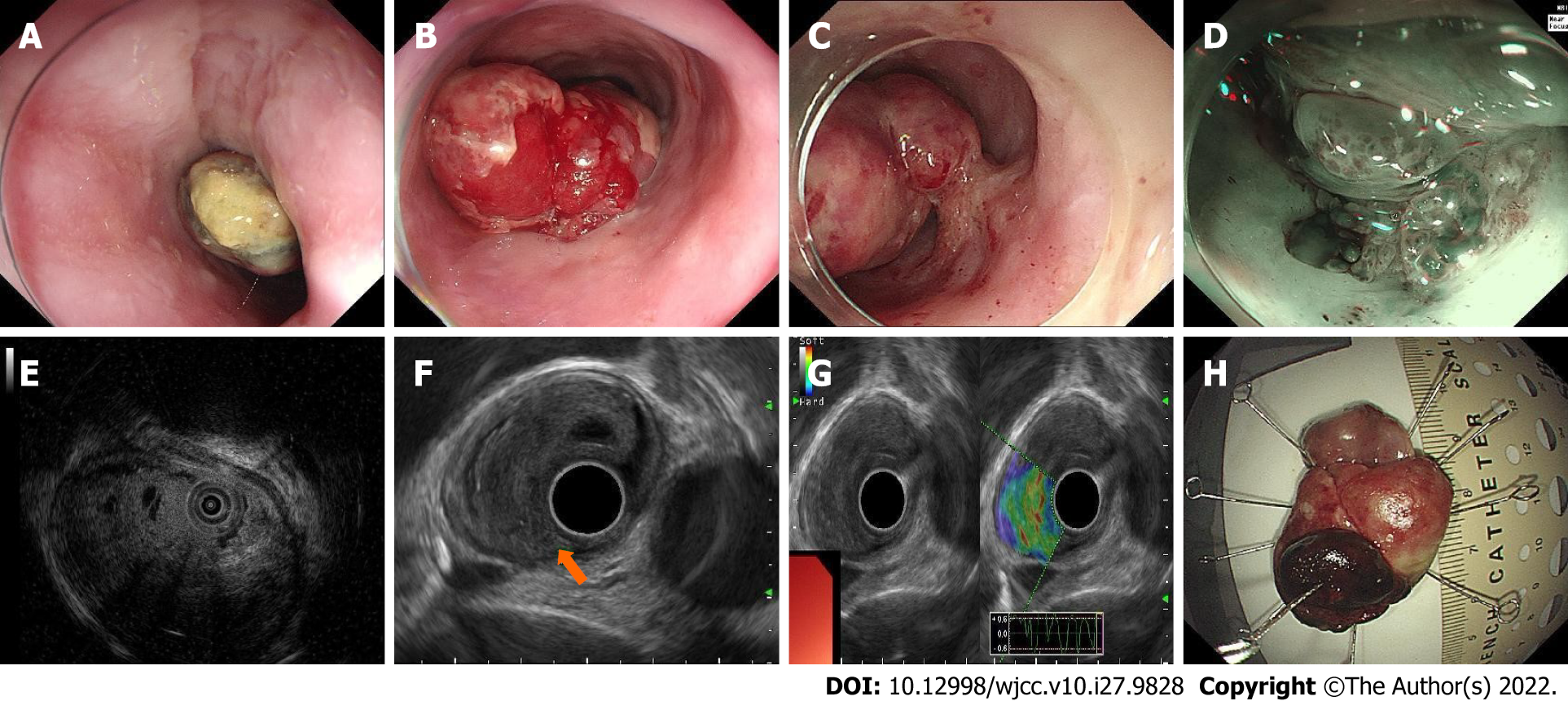
Figure 1 Endoscopic features of the lesion.
A: The oral side of the esophageal carcinosarcoma (ECS). The surface was covered with white pseudomembranous inflammation; B: The body of the ECS. The surface was hyperemic and eroded; C: The short peduncle connected to the wall of the esophagus; D: The peduncle component revealed by narrow-band imaging; E: Ultrasonic mini-probe; F: Endoscopic ultrasonography revealed that the origin of the ECS was from the submucosal layer and the inherent muscle layer was clear; G: Ultrasonic elastography revealed that the lesion was blue–green, with a tough texture; H: Macroscopic findings of the resected specimen.
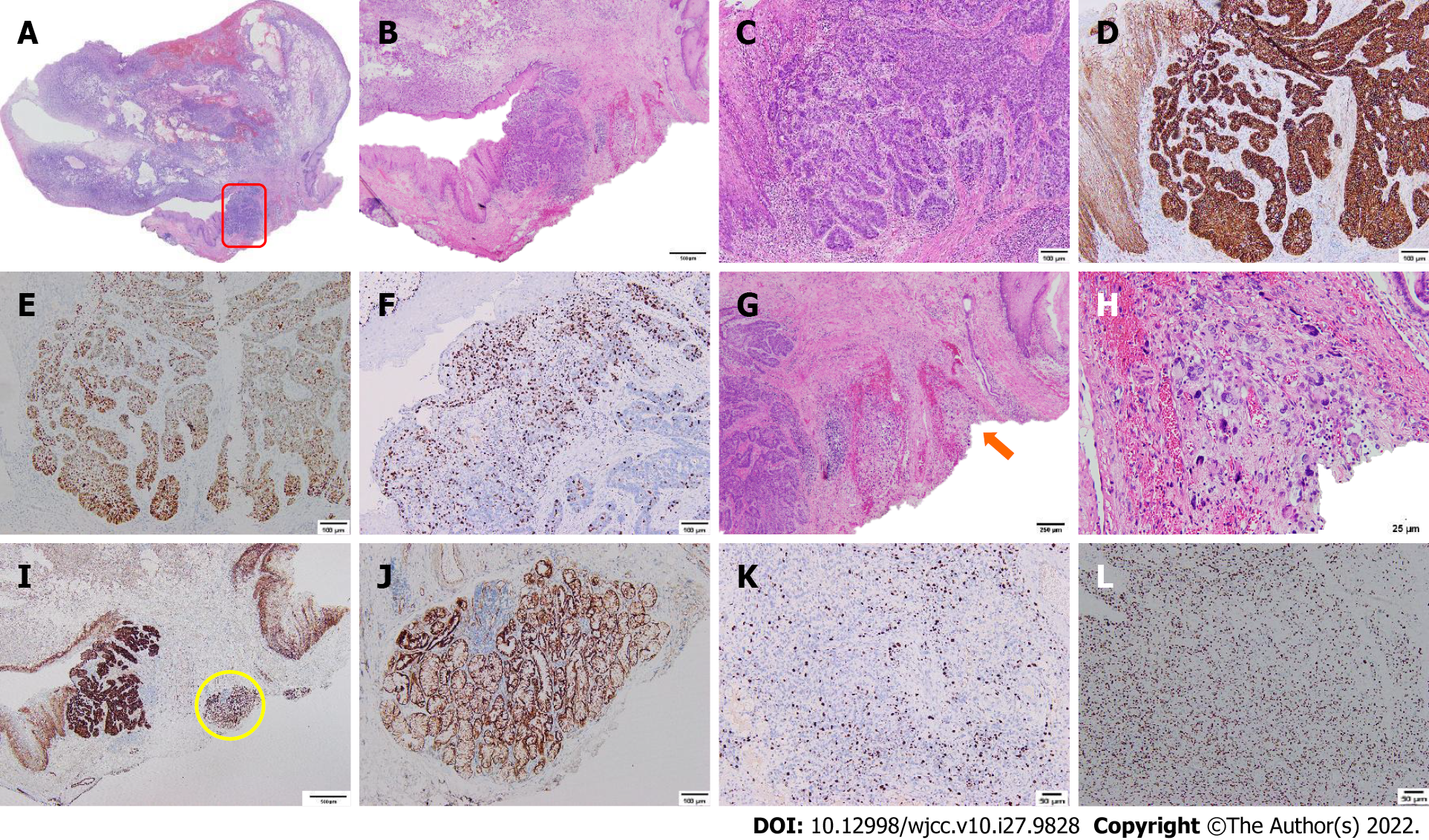
Figure 2 Histological and immunohistochemical findings of the esophageal carcinosarcoma.
A: Histological mapping of the esophageal carcinosarcoma; B and C: Hematoxylin-eosin staining of the basal-like squamous cell carcinoma (BSC) component (red rectangle, B × 20, C × 100); D: β-catenin staining of the BSC component (positive, × 100); E: P53 staining of the BSC component (positive, × 100); F: Ki-67 staining of the BSC component (30%, × 100); G and H: Hematoxylin-eosin staining of the sarcoma component (orange arrow, G × 40, H × 400); I and J: Immunopositive carcinomatous cells for β-catenin are closely adjacent to the invasion depth (yellow circle, × 20, × 100); K: Ki-67 staining of the sarcoma component (30%, × 100); L: P53 staining of the sarcoma component (positive, × 100).
- Citation: Ma XB, Ma HY, Jia XF, Wen FF, Liu CX. Misdiagnosis of an elevated lesion in the esophagus: A case report. World J Clin Cases 2022; 10(27): 9828-9833
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9828.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9828