Copyright
©The Author(s) 2022.
World J Clin Cases. Sep 16, 2022; 10(26): 9368-9377
Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9368
Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9368
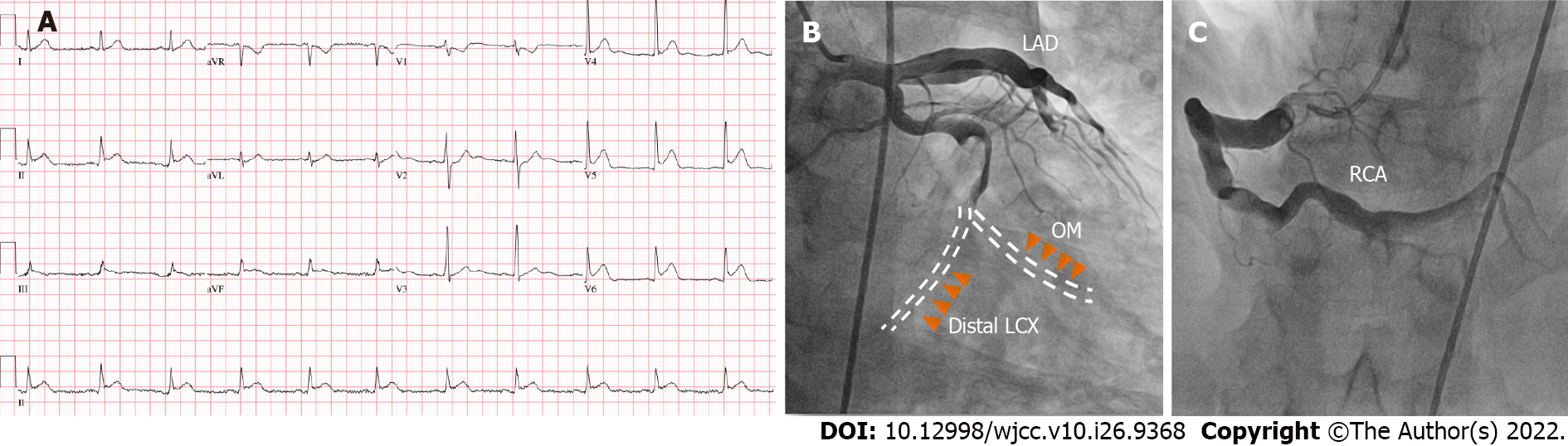
Figure 1 Electrocardiogram and coronary angiography.
A: Initial electrocardiogram in the emergency room. Sinus rhythm with ST-segment elevation in leads II, III and aVF; B: Coronary angiography revealed total occlusion of the distal left circumflex, shown as red arrowheads, and the obtuse marginal arteries with severely enlarged vessels and sluggish flow in the 15° right anterior oblique and 25° caudal projection, presented as yellow arrowheads; C: Aneurysmal dilatation in the proximal segment of the right coronary artery was observed in the 30° left anterior oblique projection. LAD: Left anterior descending; RCA: Right coronary artery; OM: Obtuse marginal; LCX: Left circumflex.
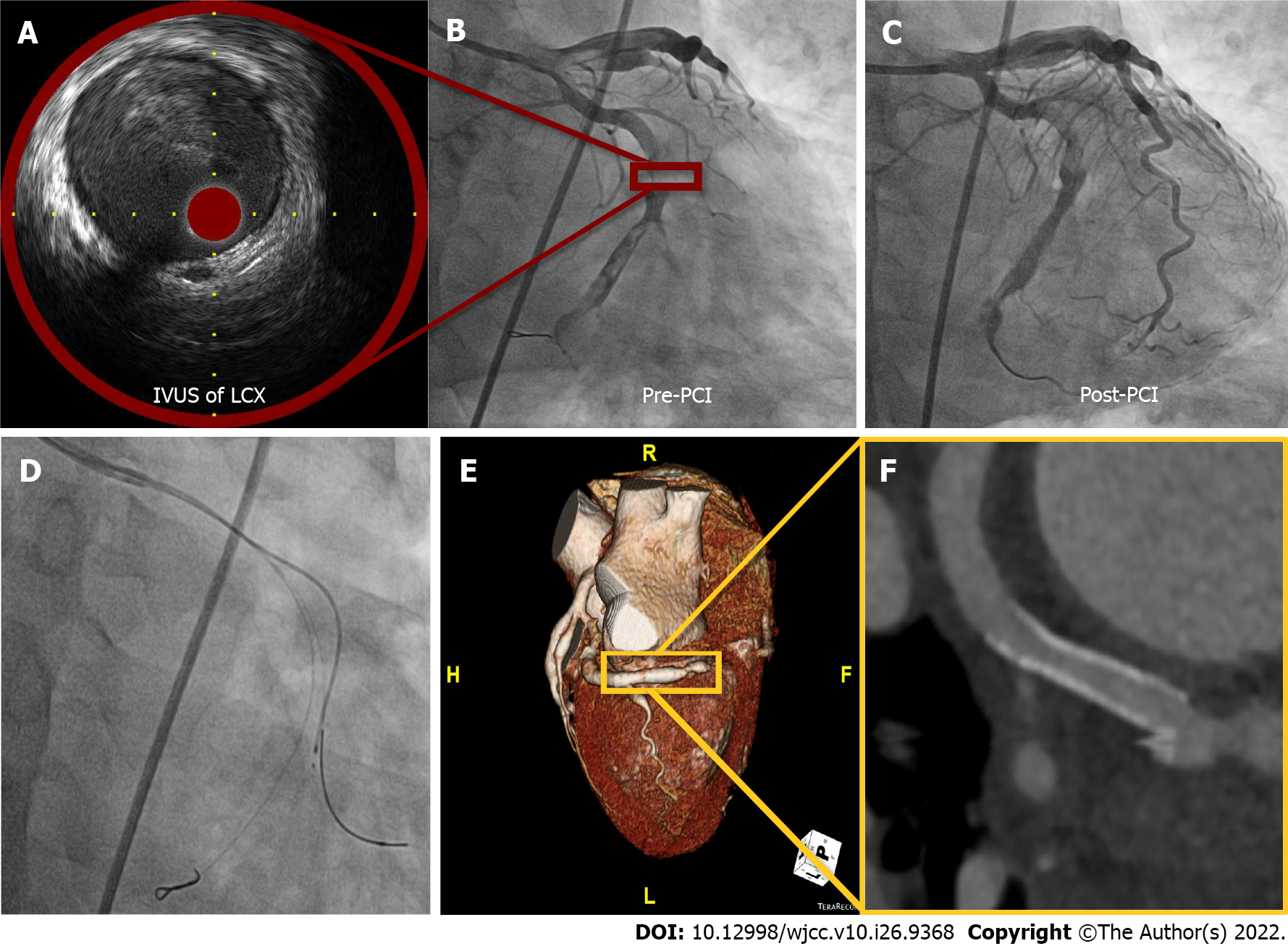
Figure 2 Coronary angiographic images and Intravascular ultrasound during percutaneous coronary intervention and follow-up coronary computerized tomography.
A: Images and Intravascular ultrasound (IVUS) showed a diameter of 6.0 mm with hazy material filling the distal left circumflex (LCX), suggestive of thrombosis; B: Fluoroscopy showed a thrombolysis in myocardial infarction 2 flow to the distal LCX with massive thrombi; C: A drug-eluting stent was successfully inserted into the culprit lesion without a no-reflow phenomenon; D: We were not able to further advance the IVUS catheter into the obtuse marginal due to resistance and/or angulation; E and F: Coronary computerized tomography performed one year later showed good patency at the LCX stent area and ectatic aneurysm in all coronary arteries. IVUS: Images and Intravascular ultrasound; LCX: Left circumflex; PCI: Percutaneous coronary intervention.
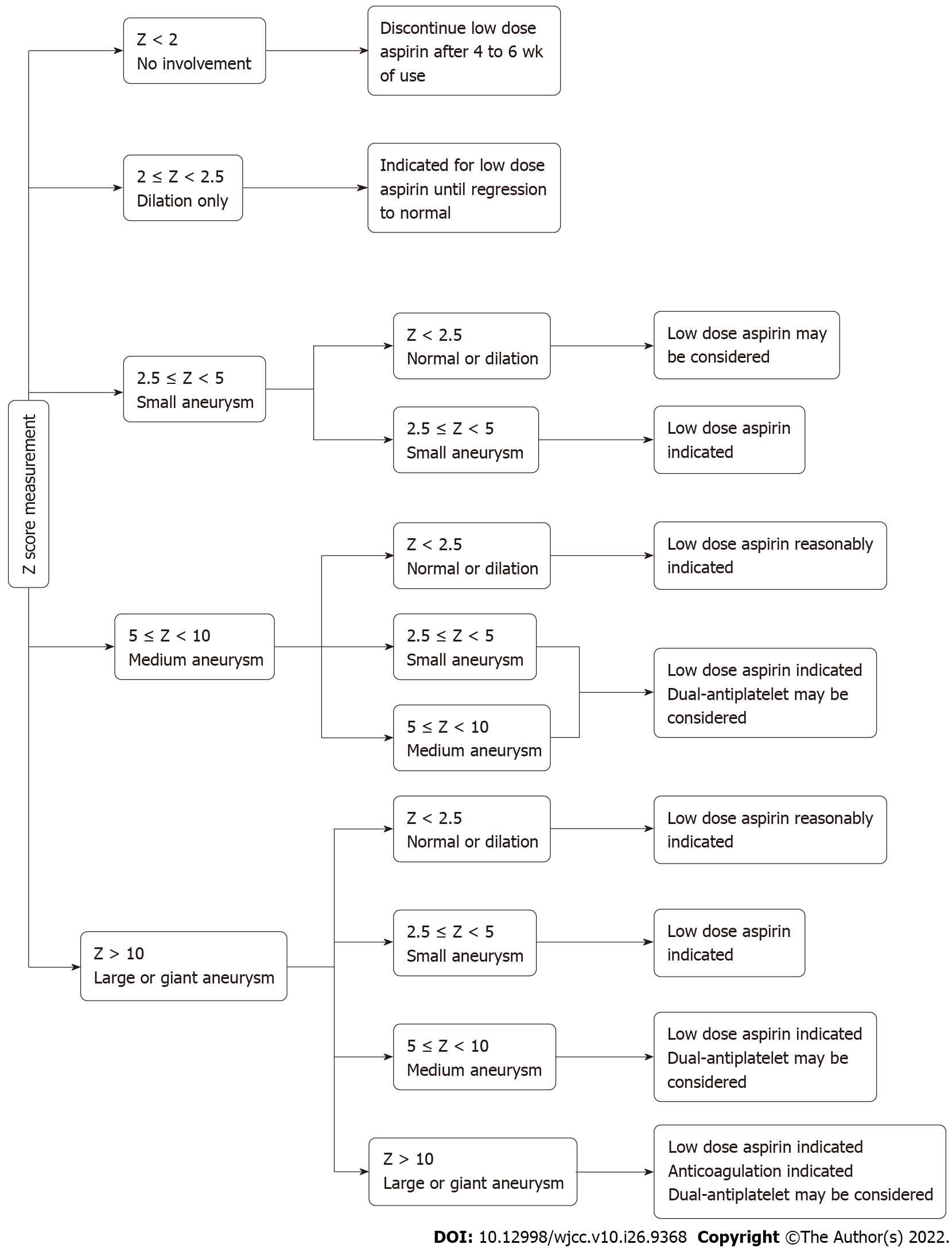
Figure 3
A summary of expert consensus of Kawasaki disease imaging surveillance and management.
- Citation: Lee J, Seo J, Shin YH, Jang AY, Suh SY. ST-segment elevation myocardial infarction in Kawasaki disease: A case report and review of literature. World J Clin Cases 2022; 10(26): 9368-9377
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9368.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9368