Copyright
©The Author(s) 2022.
World J Clin Cases. May 16, 2022; 10(14): 4632-4639
Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4632
Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4632
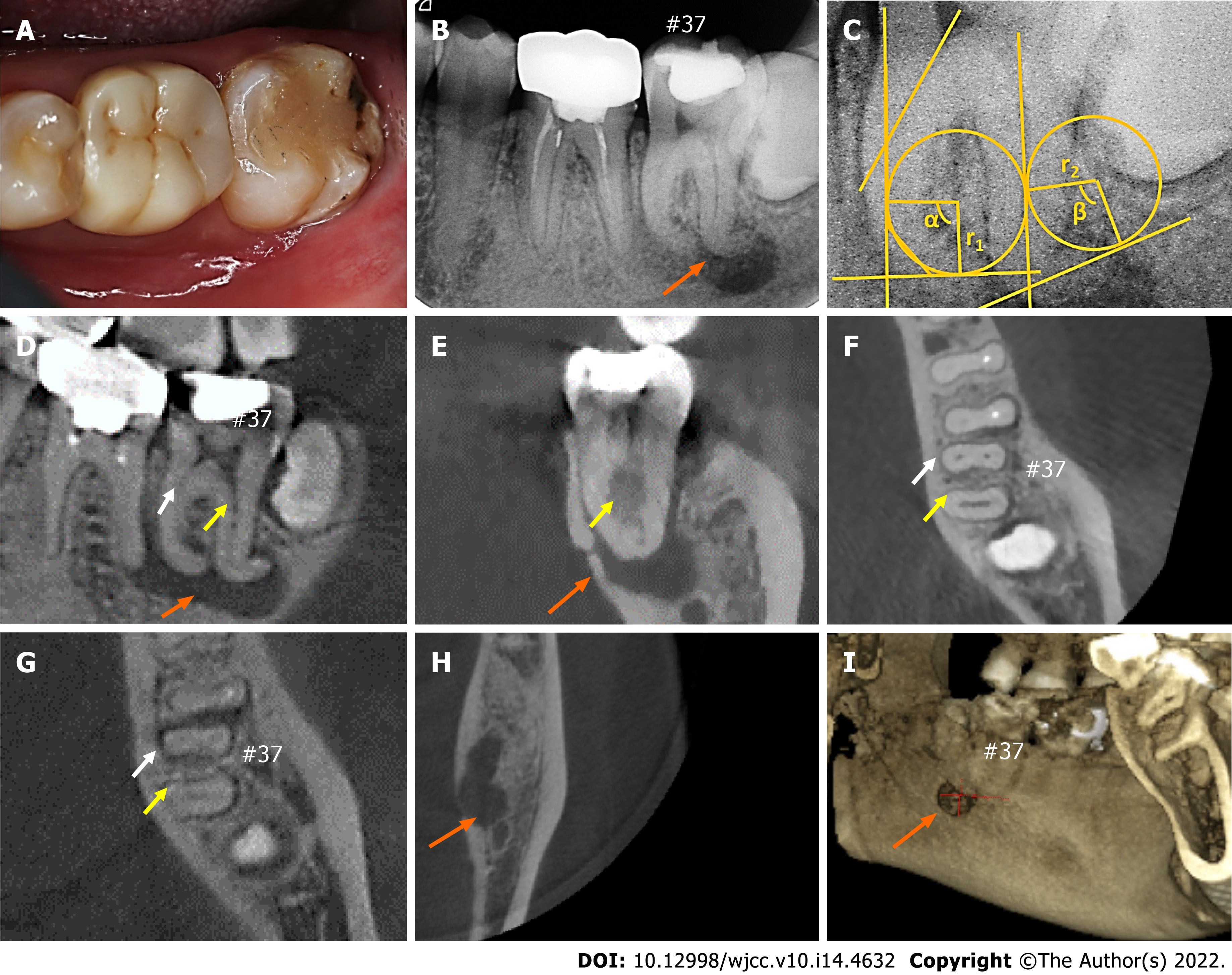
Figure 1 Initial clinical situation (#37).
A: Photograph of the mandibular second molar; B: Preoperative periapical radiograph of the molar; C: Measurement of the radius of the curvature and angles; D and E: Sagittal (D) and coronal (E) dimensions obtained from cone beam computed tomography (CBCT); F-H: Axial dimensions obtained from CBCT; I: Three-dimensional reconstruction of CBCT images presenting the perforation of the lingual cortical plate. White and yellow arrows represent the mesial root canals and a distal root canal, respectively; orange arrows show the regions of large periapical radiolucency.
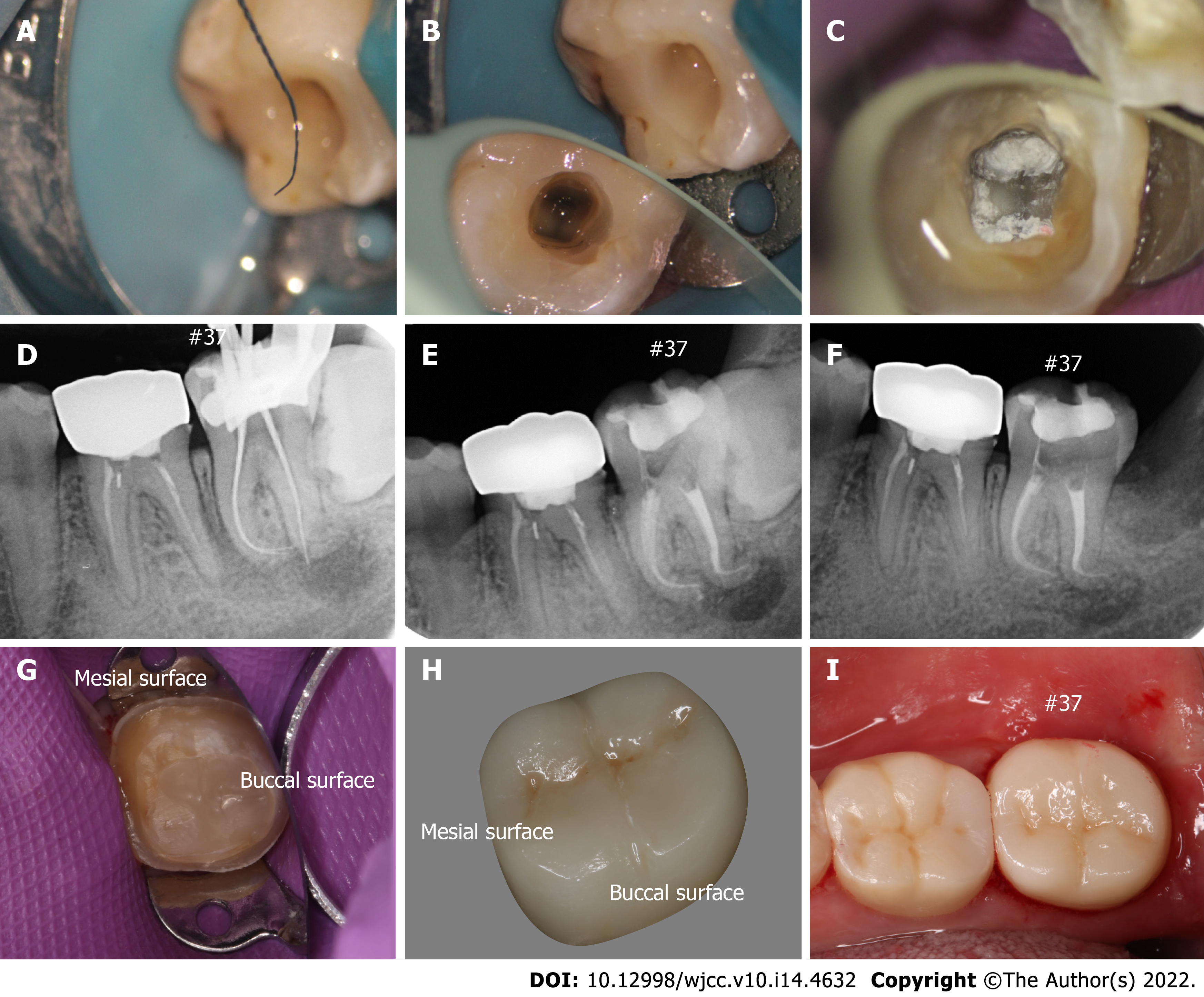
Figure 2 Treatment of the mandibular second molar.
A: Severe curvature of the file in the canal apex; B: Preoperative image; C: Postoperative image of the bottom medullary chamber; D: Radiograph for working length determination; E: Final radiograph after the operation; F: Follow-up at 2 wk; G: The tooth after crown preparation; H: Ceramic crown; I: Occlusal surface after restoration.
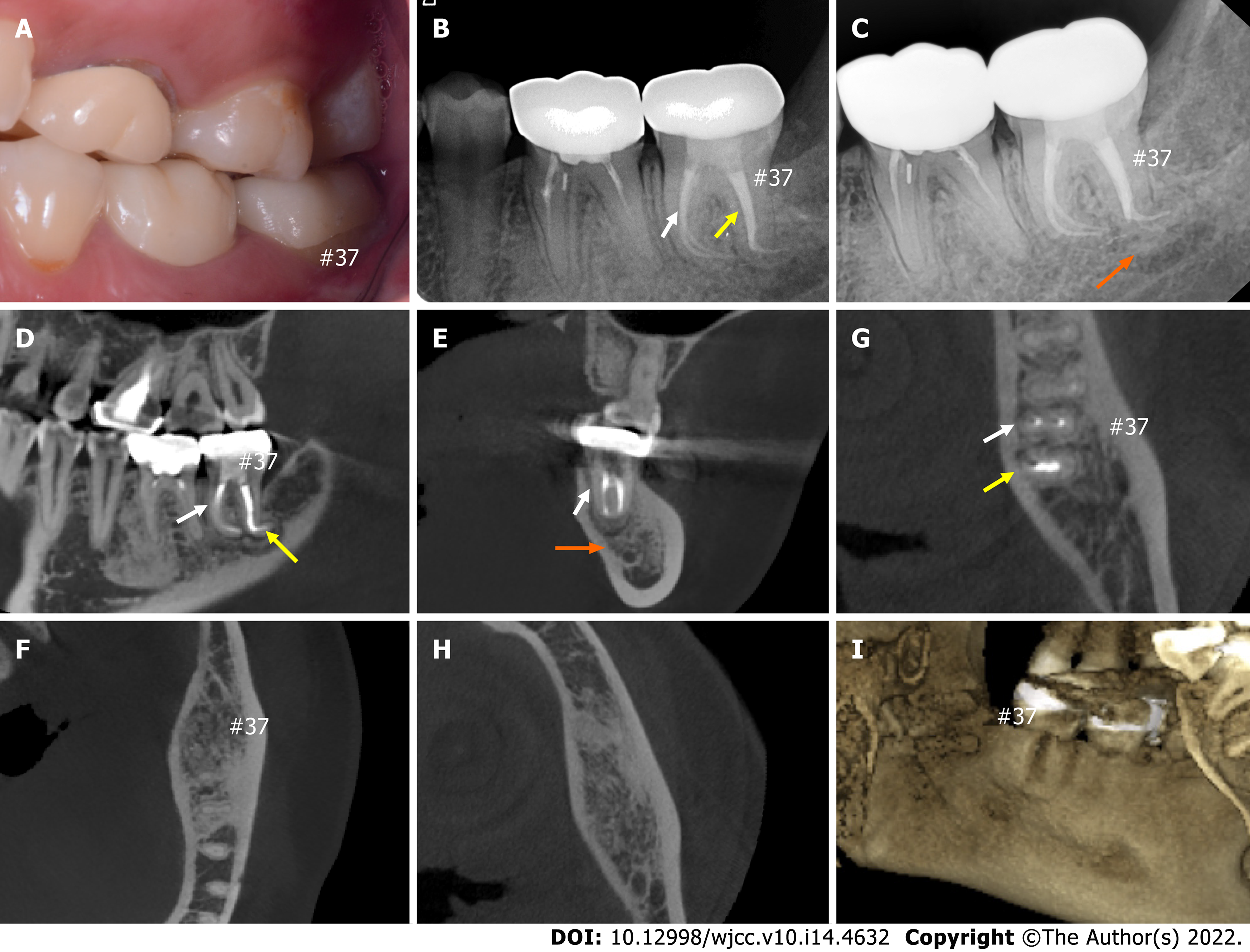
Figure 3 Post-treatment situation of the mandibular second molar and follow-ups.
A: Occlusive situation of the left molars; B and C: Three-month (B) and one-year (C) radiographic follow-up images demonstrating healing of the periapical lesion; D-H: Cone beam computed tomography (CBCT) images at 1-year radiographic follow-up; I: Three-dimensional reconstruction of CBCT images presenting healing of the lingual cortical plate. White and yellow arrows represent the mesial root canals and a distal root canal, respectively; orange arrows show the regions of periapical healing.
- Citation: Xu LJ, Zhang JY, Huang ZH, Wang XZ. Successful individualized endodontic treatment of severely curved root canals in a mandibular second molar: A case report. World J Clin Cases 2022; 10(14): 4632-4639
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4632.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4632