Published online Apr 24, 2017. doi: 10.5500/wjt.v7.i2.152
Peer-review started: November 23, 2016
First decision: January 16, 2017
Revised: February 20, 2017
Accepted: April 6, 2017
Article in press: April 10, 2017
Published online: April 24, 2017
Processing time: 150 Days and 18.1 Hours
To compare the outcomes between related and unrelated kidney transplantations.
Literature searches were performed following the Cochrane guidelines. We conducted a systematic review and a meta-analysis, which included 12 trials that investigated outcomes including the long-term (ten years), mid-term (one to five years), and short-term (one year) graft survival rate as well as the acute rejection rate. Meta-analyses were performed using fixed and random-effects models, which included tests for publication bias and heterogeneity.
No difference in graft survival rate was detected in patients who underwent living related kidney transplantations compared to unrelated (P = 0.44) transplantations after ten years. There were no significant differences between the graft survival rate in living related and unrelated kidney transplantations after a short- and mid-term follow-up (P = 0.35, P = 0.46). There were no significant differences between the acute rejection rate in living related and unrelated kidney transplantations (P = 0.06).
The long, mid and short term follow-up of living related and unrelated kidney transplantation showed no significant difference in graft survival rate. Also, acute rejection rate was not significantly different between groups.
Core tip: The long, mid and short term follow-up of living related and unrelated kidney transplantation showed no significant difference in graft survival rate. Also, acute rejection rate was not significantly different between groups.
- Citation: Simforoosh N, Shemshaki H, Nadjafi-Semnani M, Sotoudeh M. Living related and living unrelated kidney transplantations: A systematic review and meta-analysis. World J Transplant 2017; 7(2): 152-160
- URL: https://www.wjgnet.com/2220-3230/full/v7/i2/152.htm
- DOI: https://dx.doi.org/10.5500/wjt.v7.i2.152
Renal failure is a disease with a high rate of morbidity and mortality. By the end of 2001, with the help of dialysis and renal transplantations, approximately 1479000 people were kept alive. This number increased to 1783000 by the end of 2004[1]. Nowadays, renal transplantation has become the optimal treatment for patients with end-stage renal disease[2]. The recipients of renal transplant had a higher quality of life and a greater survival rate in comparison to patients who underwent dialysis. Due to these results, the demand of renal transplantations has increased over time, but the gap between supply and demand has widened. Consequently, the number of patients who are on the renal transplant waiting list for deceased-donor transplantation has increased and thousands of patients have died while waiting for their renal transplantation. This has made it necessary to search for alternatives.
During the past two decades, several approaches have been adopted to increase living related organ donations, but living unrelated donors remain an underutilized source. The result of living unrelated transplantations was widely disputed. While the Brazilian[3], Iranian[4,5], and Egyptian[6] experiences resulted in excellent outcomes that were superior to those in cadavers and were comparable to living related-donor transplantations, there were contradictory reports in several studies[7,8]. To our knowledge, there was no systematic review and meta-analysis that evaluated outcomes in patients who underwent living related vs unrelated kidney transplantations. This systematic review and meta-analysis was designed to compare the outcomes including the long-, mid- and short-term graft survival rate, and the acute rejection rate between related and unrelated kidney transplantations.
The review was conducted in accordance with the guidelines described in the Cochrane handbook for the systematic review and meta-analysis of interventions.
The criteria for studies included the following: (1) the patients considered had undergone living related or unrelated kidney transplantations; (2) the study involved the comparison of the outcomes in patients whom underwent kidney transplantation from related vs unrelated kidney donations; and (3) the primary outcome was long-term (ten years) graft survival rate, while the secondary outcomes were short-term (one year) and mid-term (one to five years) graft survival rate and acute rejection rate.
Both English language studies and non-English language studies were included in the meta-analysis.
Two independent reviewers completed a systematic computerized search of online databases, including PubMed, Ovid, MEDLINE, EMBASE, the Cochrane Controlled Trials Register, HealthSTAR, CINAHL, Google, and Google Scholar to locate studies exploring the evaluation outcomes of patients who underwent kidney transplantation from living related vs unrelated kidney donations published in any language throughout March 2016. The keywords used for the search included kidney transplant, related, unrelated, and living. Thereafter, a search on MEDLINE was refined to clinical trials. We also searched the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, Clinical Trials (http://www.clinicaltrials.gov), Centre watch (http://www.centerwatch.com), Trials Central (http://www.trialscentral.org/clinicaltrials.aspx), and the United Kingdom National Research Register (http://www.nrr.nhs.uk).
After reviewing the titles of these studies, we retrieved the abstracts that were appropriate for use in our study. We independently reviewed these abstracts and chose those studies that were potentially relevant to our work. We reviewed the bibliographies of all of the studies that were included to identify any additional studies which required inclusion. A data-extraction form was designed and agreed upon by the authors. Initially, two authors independently extracted the data, which were later reviewed jointly to reach an agreement on its accuracy. The data that were collected from all the manuscripts included the following fields: Number of patients, mean follow-up, recipient mean age, recipient sex, Immunosuppression regimen, the short-term, mid-term and long-term survival rate and the acute rejection rate, mean serum creatinine at 1 year and final follow-up, and post-transplant infectious complications. Disagreements were resolved by consensus or consultation with senior authors (Table 1). The authors of individual trials were contacted directly to provide additional information when necessary. We analysed the quality of studies with a questionnaire and only the studies that had a score greater than eight were included in our study (Table 2). In cases where the full text or data were not accessible, we tried to contact the authors in order to have them provided.
| Patients | Patients underwent kidney transplantation |
| Literature search | Keyword search in PubMed, Google scholar and Scopus |
| Databases | Pubmed, Ovid, MEDLINE, EMBASE, the Cochrane Controlled Trials Register, HealthSTAR, CINAHL, Google, and Google Scholar |
| Limits | Only comprehensive articles without time limit Humans In English |
| Keywords | Kidney transplantation Renal transplant Related Unrelated |
| Eligibility criteria | Article in Full-text (no abstracts) Unique publication (no duplicate articles) Reported each of the interested outcomes (graft survival rate, and acute rejection rate) Original report as determined from reading the abstract or if necessary the full text Outcome reported in a usable form (each surgical approach was reported as a separate cohort, no additional confounding treatments, no missing or unreliable data; could not have > 10% difference in values between text and tables Reported on surgical approaches of interest |
| Exclusion criteria | Duplicate patient population, where some or all of the same patients were included in a different study reporting on the same parameters (prevents double counting) Early case experience (prevents bias toward approaches with more experienced surgeons) |
| Data abstraction | Articles needed to report which contain each of outcome of interest to be included in the analysis Data were abstracted by two individuals into a custom database table including list of variables. 50% of articles were abstracted by one reviewer and other 50% with other one. The data for 50% of the articles was double-entered by a second individual, and any discrepancies were resolved through repeated review and discussion prior to data analysis All primary outcomes were then double-checked and any discrepancies resolved Variables in four types were abstracted from each study: Those necessary to determine inclusion and exclusion criteria, surgical approach, baseline patient characteristics, and clinical outcomes All studies were reviewed by two independent reviewers using the total QASs (Table 3) to assess the methodological quality of the studies that were included. Although the QASs were reported for each study, they were not used to weight the studies in the meta-analysis |
| Primary outcomes | Graft survival rate |
| Secondary outcomes | Acute rejection rate |
| Controls for Publication bias | Performed a funnel plot analysis |
| Was the assigned treatment adequately concealed prior to allocation? |
| 2 = method did not allow disclosure of assignment |
| 1 = small but possible chance of disclosure of assignment or unclear |
| 0 = quasi-randomized or open list/tables |
| Were the outcomes of participants who withdrew described and included in the analysis (intention-to-treat)? |
| 2 = withdrawals well described and accounted for in analysis |
| 1 = withdrawals described and analysis not possible |
| 0 = no mention, inadequate mention, or obvious differences and no adjustment |
| Were the outcome assessors blinded to treatment status? |
| 2 = effective action taken to blind assessors |
| 1 = small or moderate chance of unblinding of assessors |
| 0 = not mentioned or not possible |
| Were the treatment and control groups comparable at entry? (likely confounders may be age, partial or total rupture, activity level, acute or chronic injury) |
| 2 = good comparability of groups, or confounding adjusted for in analysis |
| 1 = confounding small; mentioned but not adjusted for |
| 0 = large potential for confounding, or not discussed |
| Were the participants blind to assignment status after allocation? |
| 2 = effective action taken to blind participants |
| 1 = small or moderate chance of unblinding of participants |
| 0 = not possible, or not mentioned (unless double-blind), or possible but not done |
| Were the treatment providers blind to assignment status? |
| 2 = effective action taken to blind treatment providers |
| 1 = small or moderate chance of unblinding of treatment providers |
| 0 = not possible, or not mentioned (unless double-blind), or possible but not done |
| Were care programes, other than the trial options, identical? |
| 2 = care programes clearly identical |
| 1 = clear but trivial differences |
| 0 = not mentioned or clear and important differences in care programes |
| Were the inclusion and exclusion criteria clearly defined? |
| 2 = clearly defined |
| 1 = inadequately defined |
| 0 = not defined |
| Were the interventions clearly defined? |
| 2 = clearly defined interventions are applied with a standardized protocol |
| 1 = clearly defined interventions are applied but the application protocol is not standardized |
| 0 = intervention and/or application protocol are poorly or not defined |
| Were the outcome measures used clearly defined? (by outcome) |
| 2 = clearly defined |
| 1 = inadequately defined |
| 0 = not defined |
| Were diagnostic tests used in outcome assessment clinically useful? (by outcome) |
| 2 = optimal |
| 1 = adequate |
| 0 = not defined, not adequate |
| Was the surveillance active, and of clinically appropriate duration? |
| 2 = active surveillance and appropriate duration |
| 1 = active surveillance, but inadequate duration |
| 0 = surveillance not active or not defined |
| Ref. | Number | Mean follow up (mo) | Recipient mean age (yr) | Recipient sex M/F | Immunosuppression regimen | One year graft survival rate | five years graft survival rate | 10 yr graft survival rate | Acute rejection rate | Mean serum Cr at 1 yr | Mean serum Cr at final follow up | Post-transplant infectious complications |
| Cortesini et al[9], 2002 | 302 vs 172 | 42 | 32.8 ± 7.3 vs 44 ± 9.9 | 215/87 vs 133/39 | Cyclosporine | 275 (91) vs 150 (87) | 232 (77) vs 136 (79) | 199 (66) vs 118 (69) | N/D | 1.9 ± 0.8 vs 2.0 ± 0.8 | 2.0 ± 0.8 vs 1.9 ± 0.8 | N/D |
| Simforoosh et al[5], 2016 | 411 vs 3305 | N/D | 27.6 ± 10.1 vs 35.6 ± 15.6 | 270/138 vs 2164/1136 | Cyclosporine | 89% vs 90% | 288 (70.2) vs 2697 (81.6) | 225 (54.9) vs 2350 (71.1) | N/D | N/D | N/D | N/D |
| Voiculescu et al[10], 2003 | 38 vs 24 | 19.6 ± 15.4 | 37.7 ± 12.1 vs 53.6 ± 7.8 | 26/12 vs 14/10 | Steroids, cyclosporine, mycophenolate mofetil | 36 (94.8) vs 24 (100) | N/D | N/D | 20 (52.5) vs 13 (54.2) | N/D | 1.76 ±0.6 vs 1.62 ±0.5 | 25 (66.7) vs 9 (36.4) |
| Ahmad et al[15], 2008 | 261 vs 61 | 45 | 28 ± 16 vs 48 ± 12 | N/D | Cyclosporine | 247 (94.8) vs 60 (98.4) | N/D | N/D | 107 (41) vs 21 (35) | N/D | N/D | N/D |
| Kizilisik et al[11], 2004 | 85 vs 24 | 36 | N/D | N/D | Cyclosporine, azathioprine, steroid, tacrolimus, mycofenolatemofetil | 81 (95) vs 23 (95.8) | 75(88.3) vs 21 (87.5) | N/D | 11(13) vs 5 (20) | N/D | N/D | 7 (8.3) vs 8 (3.5) |
| Park et al[12], 2004 | 36 vs 41 | N/D | 33.6 vs 38.3 | 21/15 vs 28/13 | Cyclosporine, steroid and mycophenolatemofetil | N/D | 30 (84) vs 36 (88.5) | 28 (78.8) vs 41 (74.7) | 11 (30) vs 13 (31) | N/D | N/D | N/D |
| Wolters et al[13], 2005 | 66 vs 29 | 35 | 31 ± 12.5 vs 51 ± 8.5 | 41/25 vs 23/6 | Cyclosporine/MMF/prednisone vs MMF/prednisone | N/D | 62 (94.7) vs 23 (94.7) | N/D | 6 (9) vs 5 (17.2) | N/D | N/D | N/D |
| Simforoosh et al[14], 2006 | 374 vs 1760 | 45.68 ± 46.80 | 28.97 ± 9.58 vs 33.46 ± 14.61 | N/D | Cyclosporine, azathioprine, and prednisone | 342 (91.6) vs 1610 (91.5) | 286 (76.4) vs 1432 (81.4) | 241 (64.4) vs 1200 (68.2) | N/D | N/D | N/D | N/D |
| Ishikawa et al[16], 2012 | 66 vs 44 | 12 | 36.1 ± 12.4 vs 55.0 ± 8.8 | 29/15 vs 38/28 | Plasmaphresis, tacro, celecpt, Basiliximab, rituximab, methyl prednisolone, cyclosporine, deoxypergualin | 65 (98.5) vs 43 (97.7) | N/D | N/D | 16 (24.2) vs 14 (31.8) | N/D | N/D | N/D |
| Santori et al[17], 2012 | 111 vs 24 | 128.17 ± 86.64 vs 103.53 ± 86.85 | 26.94 ± 13.51 vs 50.04 ± 8.86 | 78/33 vs 18/6 | Cyclosporine, tacro, steroids, celecept | N/D | N/D | 71 (63.8) vs 21 (87.8) | N/D | N/D | N/D | N/D |
| Matter et al[18], 2016 | 2075 vs 410 | 7.72 ± 6.15 | 28.8 ± 9.8 vs 34.8 ± 11.1 | 1554/521 vs 297/113 | Steroid- Azathioprine or MMF | 2012 (97) vs 389 (95) | 1784 (86) vs 340 (83) | 1660 (67) vs 270 (66) | 71 (3.4) vs 26 (6.3) | 1.38 ± 0.69 vs 1.35 ± 0.61 | 1.71 ± 1.04 vs 1.59 ± 0.89 | N/D |
| Ali et al[19] | 92 vs 143 | 5 | N/D | N/D | Methyl prednisolone, Cyclosporine or tacrolimus MMF | 90 (97) vs 141 (98.6) | 80 (86) vs 125 (87.4) | N/D | N/D | N/D | N/D | N/D |
The Review Manager Database (RevManversion 5.0, The Cochrane Collaboration 2008) was used to analyse the selected studies. Continuous data for each arm of a particular study were expressed as mean and standard deviation. Dichotomous data were expressed as proportions or risks, with the treatment effect reported as a relative risk with 95%CI.
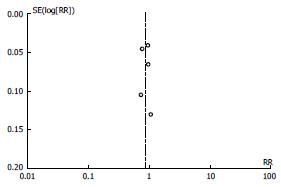
The data were analysed for the outcomes that were of interest to us. The risk ratio (RR) was defined as the number of patients with a successful graft survival rate. The RR referred to the multiplication of the rate of graft surveillance that occurred with the use of related and unrelated kidney transplantations. The heterogeneity between the studies was assessed using the χ2 test and the I2 statistic. The latter is a measure of the percentage of variation in data that results from heterogeneity as opposed to chance. A P value of < 0.1 and an I2 value > 50% were considered suggestive of statistical heterogeneity, prompting a random effects modelling estimate. Conversely, a non-significant chi-squared test result (a P value ≥ 0.1 and an I2 value ≤ 50%) only suggested that there was no evidence of heterogeneity; it did not necessarily imply that homogeneity existed because there may have been insufficient power to detect heterogeneity. The Mantel-Haenszel (M-H) method was used to combine the studies. If their significant heterogeneity were indicated (P < 0.1 and I2 > 50%), a random-effect model was used; if not, a fixed-effect model was used. In addition, funnel plots were constructed for the outcomes to assess publication bias, i.e., the tendency not to publish studies with negative results; the more asymmetric the funnel plot is, the more potential bias there is. The statistical significance was set at P < 0.05.
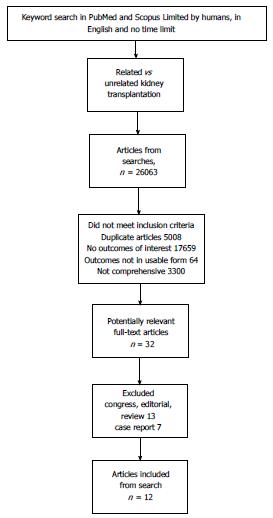
Using our search terms, 376 references were identified. The first search of studies exploring the evaluation of the outcomes of patients yielded the following results: PubMed (n = 11590), Ovid (n = 24), EMBASE (n = 3300), the Cochrane Controlled Trials Register (n = 9719), and Google Scholar (n = 1430). Out of these, we included 12 studies after applying our eligibility criteria to their titles and/or abstracts, excluding duplicates (Figure 1).
The eligible trials included 12 relevant comparisons (Table 3) involving 9954 participants. We could not assess the differences in the outcomes between post-operative infections, post-operative hypertension, diabetes, and post-operative creatinine due to the lack of data.
Cortesini et al[9] evaluated 527 kidney allografts from living donors. Of these, 302 living donors were first-degree relatives of the recipient and shared one haplotype (living related donor) and 172 were unrelated. They showed actuarial graft survival rates in the living related and living unrelated groups, which were 91% and 87% in 1 year, 77% and 79% in 5 years, and 66% and 69% in 9 years. In conclusion, they reported that kidney transplantation between unrelated donors and recipients might be a valid alternative in view of the cadaver organ shortage, its success as a procedure and its potential to provide the “gift of life” to both the patient and the family.
Voiculescu et al[10] evaluated 62 out of 112 potential living donors for types of rejections, complications, and kidney functions. Of them, 38 cases were living related and 24 cases were living unrelated. They showed that acute rejection rate was similar in both groups (52.2% vs 54.2%); however, there were more complications of infection in the living related group (66.7% vs 36.4%) and a trend showing more surgical complications in living related transplantations (28.9% vs 8.3%). They concluded that the results for the living unrelated group are equivalent to the living related transplantation group. They determined that careful selection of donors and recipients is a prerequisite for success.
Kizilisik et al[11] evaluated 109 living donor kidney transplants. Seventy-eight percent of living donors were from living related donors and 22% were from living unrelated donors. The resultant one- and three-year patient survival rates were 97.6% and 93.2%, with 1- and 3-year graft survival rates of 93.2% and 88.3%, respectively. Among the patients of Kizilisik et al[11], there were 6 delayed graft functions (5.5%), 16 acute cellular rejections (10%), and 10 chronic rejections (9%). They suggested that living donors represent a valuable source because of the limited number of cadaveric kidneys available for transplant and stated that the use of living-unrelated donors has produced an additional supply of organs.
Park et al[12] evaluated 77 living-donor renal transplants (41 were living unrelated and 36 were living related transplants). They reported that 11 recipients lost their grafts (6 from living unrelated and 5 from living related); most of these losses were due to chronic rejection (n = 7). Overall 3-, 5- and 10-year graft survival rates in live donors were 92.8%, 86.6% and 76.9%, respectively; for the living unrelated, the graft survival at 3-, 5- and 10-years was 91.9%, 88.5% and 74.7% vs 94%, 84% and 78.8% for the living related transplants. They concluded that acute rejection episodes markedly decreased long-term graft survival in live donor renal transplants, the use of living related transplants provides graft survival comparable with living related transplants, and proper management of acute rejection is essential for long-term graft survival.
Wolters et al[13] evaluated 95 living donor transplantations (69% related, 31% unrelated). They showed that at a mean follow-up of 35 mo, 94.7% of grafts were functioning. Three grafts were lost due to acute (in related transplants) or chronic (in unrelated transplants) rejection or due to multi-organ failures. They concluded that although HLA mismatching was significantly different between related and unrelated donors, no difference in the outcome was observed.
Simforoosh et al[14], between 1984 and 2004, evaluated 2155 kidney transplantations; out of this, 374 were from living related donors and 1760 were from unrelated donors. The resultant 1-, 3-, 5-, 10- and 15-year graft survival rates among the related group were 91.6%, 81.7%, 76.4%, 64.4% and 48.4%; and for unrelated group, these rates were 91.5%, 86.7%, 81.4%, 68.2% and 53.2%, respectively. Patient survivals for 1-, 3-, 5-, 10- and 15-years in the living related group were 94.6%, 91.9%, 83%, 79.5% and 73.9%; and in the unrelated group, these were 93.6%, 91.7%, 89.3%, 84% and 76.4%, respectively. They concluded that the results of living unrelated kidney transplantation upon long-term follow-up in a large number of cases was as effective as living related kidney transplantation.
Ahmad et al[15] retrospectively analysed the outcome of 322 living-donor renal transplants (related donors: 261; unrelated donors = 61). They reported that 33 grafts failed: 30 in the living related (11%) and 3 in the unrelated donor group (5%). Acute rejections occurred in 41% of recipients in the living related group and 35% of recipients in the unrelated group. One- and 3-year patient survival for the living related and unrelated group was 98.7% and 96.3% and 97.7% and 95%, respectively. One- and 3-year graft survival was equivalent at 94.8% and 92.3% for the living related, and at 98.4% and 93.7% for the living unrelated group, respectively. They concluded that the outcome of living related donors and living unrelated donors is comparable in terms of patient and graft survival, acute rejection rate, and the estimated GFR despite the differences in demographics, HLA matching, and re-transplants of recipients.
Ishikawa et al[16] evaluated 112 cases of living kidney transplantations including 46 (41%) unrelated donors and 66 cases of received kidneys from living related donors. They showed that the incidences of an acute rejection episode were 31.8% and 24.2% in the living unrelated and the related groups, respectively. They demonstrated that living transplantation from an unrelated group was equivalent to related ones.
Santori et al[17] evaluated 135 procedures using living donors (living related: 111; living unrelated: 24). They reported no significant difference in patient survival after stratifying for donor type (living related: 93.9%; unrelated donors: 95.8%) or in graft survival after stratifying for donor type (related: 63.8%; unrelated: 87.8%). After entering donor type as an independent variable in a univariate Cox regression, they showed no significance for either recipient or graft survival. They suggested that living unrelated donor utilization should be encouraged in kidney transplantation programmes.
Simforoosh et al[5] evaluated 3,716 kidney transplantations (411 related donors and 3305 unrelated donors). They showed that donor age was the only statistically significant predictor of graft survival rate (hazard ratio = 1.021; 95%CI: 1.012-1.031). Patient survival and graft survival was similar in transplantations from living unrelated and related donors. They concluded that transplants from LURDs might be proposed as an acceptable management for patients with end stage renal disease.
Matter et al[18] from March 1976 to December 2013, divided the patients into two groups: (1) 2075 kidney transplant recipients (1554 or 74.9% male and 521 or 25.1% female) for whom the donors were living related; (2) 410 kidney transplant recipients (297 or 72.4% male and 113 or 27.6% female) for whom the donors were living unrelated. They showed the percentages of patients with acute vascular rejection were significantly higher in the unrelated group, while percentages of patients with no rejection were significantly higher in the related group, but there were no significant differences regarding patient and graft survivals between both groups.
Ali et al[19] evaluated 250 kidney transplantations (92 related donors, 143 unrelated donors and 15 spouse). They showed the one-year graft survival for related and unrelated donor transplants was 98.9% and 91.8%, respectively. Graft survival was lower (82.9%) in recipients with acute rejection episodes. The patient survival at one-year was 94%. The three year graft and patient survival was 91% and 90%, respectively, and five-year survival for grafts and patients was 87.1% and 88%, respectively.
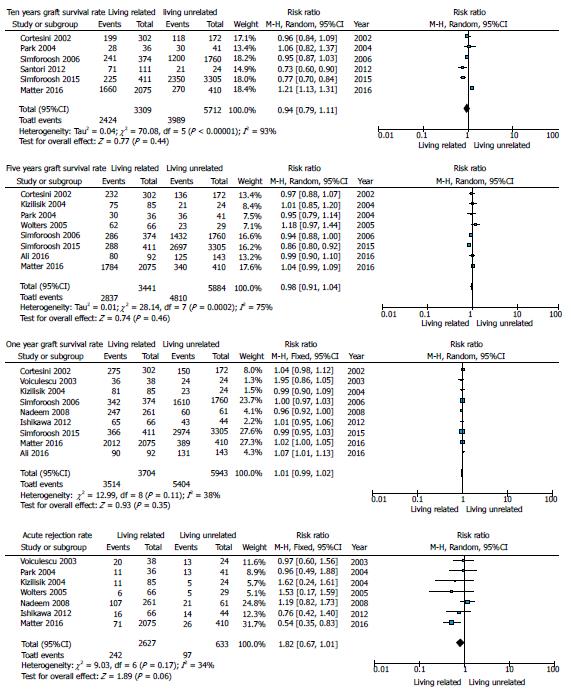
Long term (ten year) graft survival rate: We conducted random effect meta-analyses (Figure 2) because the results from the studies which reported ten years graft survival rate after living related and unrelated renal transplantation showed significant heterogeneity (P = 0.001). No significant difference in graft survival rate was detected after ten years in patients who underwent living related kidney transplantations in comparison to those who underwent unrelated kidney transplantations (P = 0.44) (Figure 3).
Mid-term (one to five year) graft survival rate: We conducted random effect meta-analyses because the results from studies reporting 1-5 years graft survival rate after living related and unrelated renal transplantation showed significant heterogeneity (P = 0.002). There were no significant differences between graft survival rate in living related and unrelated kidney transplantations after mid-term follow-ups (P = 0.46) (Figure 3).
Short-term (one year) graft survival rate: We conducted fixed effect meta-analyses because the results from the studies reporting one year graft survival rate after living related and unrelated renal transplantations showed no significant heterogeneity (P = 0.11). There were no significant differences between the graft survival rate in living related and unrelated kidney transplantations after a one year follow-up (P = 0.35) (Figure 3).
Acute rejection rate: We conducted fixed effect meta-analyses because the results from the studies reporting acute rejection rate after living related and unrelated renal transplantations showed no significant heterogeneity (P = 0.17). There were no significant differences between the acute rejection rate in living related and unrelated kidney transplantations (P = 0.06) (Figure 3).
This systematic meta-analysis showed that no significant difference existed in graft survival rate between living related and unrelated kidney transplantations in short, mid and long-term follow-ups.
In comparison to dialysis, transplantation has lengthened the patient’s survival and improved their quality of life; in the medical field, it has broadened knowledge; to sponsors, it has provided a cost-effective solution for a never-ending problem. On the other hand, the shortcoming of transplantation is the unavailability of enough donors. This led to scientists using living unrelated kidney transplantations as an available source, but there were strong controversies in this respect. A detailed analysis suggests that the difference was related to a “centre effect”. The inferior outcomes of living unrelated-donor transplantations were caused by the low standards of medical care in commercial transplantation programmes, the infections transmitted between the donor organs or patient non-compliance. After correcting these factors[20,21], the reports have shown no significant difference in graft outcomes when compared with living related transplantations. Our results support the finding that showed no significant difference between living related and unrelated kidney graft survival rates after mid-term and short-term follow-ups.
This systematic review and meta-analysis showed that the long-term graft survival rate has not a significant difference between the living related and the living unrelated groups. In our previous report[5], we evaluated the recipients of kidney transplants for 25 years and a comparable survival rate was found between the two groups. Park et al[12] reported the graft survival rates at 3, 5 and 10 years as 91.9%, 88.5% and 74.7% for the LURD vs 94%, 84% and 78.8% for the LRD transplants, with no significant difference. In contrast to our findings, previous studies showed no significant difference in long-term graft surveillance between the two groups[5,9,14]. This might be because of significant heterogeneity between the studies. As the funnel plot described, there is significant heterogeneity between the studies; therefore, in the future, more studies with a high quality of methodology are warranted.
While unrelated kidney transplantations are not widely accepted, the concern for transplantations continues to revolve around the issue of inadequate material benefits for potential donors[22]. The only model that resolved this issue was the model used in Iran. This model is organized by a non-profit organization known as the “Dialysis and Transplant Patients’ Association (DATPA)”[23]. The DATPA’s task is to assign appropriate donors for certain recipients and to offer medicolegal coverage. Donors receive a form of compensation from the government and the DATPA, and in addition, they are granted free life-long health insurance, and often, a “rewarding gift from the recipient”[23]. This model has been very successful over the past two decades in Iran, nearly eradicating the names on the transplant waiting list and gracefully providing a second chance at life for patients with ESRD; this model comprises over 75% of the total kidney transplant activity in Iran.
As a limitation, because of the lack of data, we could not evaluate the difference in HLA mismatches between the studies. Nevertheless, previous studies have reported equivalent short-, medium- and long-term outcomes of transplantation in LURD series in comparison to LRDs.
In conclusion, the long, mid and short-term follow-up of living related and unrelated kidney transplantation showed no significant difference in graft survival rate. Also, acute rejection rate was not significantly different between groups. We suggest that the Iranian model is a fair compromise because it avoids the rampant transplant commercialism.
The number of patients who are on the renal transplant waiting list for deceased-donor transplantation has increased and thousands of patients have died while waiting for renal transplantation. Despite this, no systematic review and meta-analysis has been performed yet.
Nowadays the outcomes of living related vs unrelated kidney transplantation are debatable. Worldwide research is directed towards the use of living unrelated kidney transplantation as a potential source.
In the present study, the authors investigated the outcomes of two kinds of sources in kidney transplantation by pooling results from different centres. This is the first report of a meta-analysis comparing these sources in receipts.
The present report provides an understanding of living unrelated kidney transplantation as an excellent source.
In this manuscript authors performed a meta-analysis to compare related and unrelated living donor kidney transplant outcome. Results indicate comparable outcome of kidney transplant from living unrelated vs related donors in the short, mid and long term follow up.
Manuscript source: Invited manuscript
Specialty type: Transplantation
Country of origin: Iran
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Friedman EA, Gheith O, Piancatelli D, Salvadori M, Shrestha BM S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Moeller S, Gioberge S, Brown G. ESRD patients in 2001: global overview of patients, treatment modalities and development trends. Nephrol Dial Transplant. 2002;17:2071-2076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 105] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Schnuelle P, Lorenz D, Trede M, Van Der Woude FJ. Impact of renal cadaveric transplantation on survival in end-stage renal failure: evidence for reduced mortality risk compared with hemodialysis during long-term follow-up. J Am Soc Nephrol. 1998;9:2135-2141. [PubMed] |
| 3. | Sesso R, Josephson MA, Anção MS, Draibe SA, Sigulem D. A retrospective study of kidney transplant recipients from living unrelated donors. J Am Soc Nephrol. 1998;9:684-691. [PubMed] |
| 4. | Ghods AJ. Renal transplantation in Iran. Nephrol Dial Transplant. 2002;17:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 68] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Simforoosh N, Basiri A, Tabibi A, Javanmard B, Kashi AH, Soltani MH, Obeid K. Living Unrelated Versus Related Kidney Transplantation: A 25-Year Experience with 3716 Cases. Urol J. 2016;13:2546-2551. [PubMed] |
| 6. | Barsoum RS. The Egyptian transplant experience. Transplant Proc. 1992;24:2417-2420. [PubMed] |
| 7. | Sever MS, Kazancioğlu R, Yildiz A, Türkmen A, Ecder T, Kayacan SM, Celik V, Sahin S, Aydin AE, Eldegez U. Outcome of living unrelated (commercial) renal transplantation. Kidney Int. 2001;60:1477-1483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Jha V, Chugh KS. The case against a regulated system of living kidney sales. Nat Clin Pract Nephrol. 2006;2:466-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Cortesini R, Pretagostini R, Bruzzone P, Alfani D. Living unrelated kidney transplantation. World J Surg. 2002;26:238-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Voiculescu A, Ivens K, Hetzel GR, Hollenbeck M, Sandmann W, Grabitz K, Balzer K, Schneider F, Grabensee B. Kidney transplantation from related and unrelated living donors in a single German centre. Nephrol Dial Transplant. 2003;18:418-425. [PubMed] |
| 11. | Kizilisik AT, Ray JM, Nylander WA, Langone AJ, Helderman JH, Shaffer D. Living donor kidney transplantation in a Veterans Administration medical center. Am J Surg. 2004;188:611-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Park YH, Min SK, Lee JN, Lee HH, Jung WK, Lee JS, Lee JH, Lee YD. Risk factors on graft survival of living donor kidney transplantation. Transplant Proc. 2004;36:2023-2025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Wolters HH, Heidenreich S, Dame C, Brockmann JG, Senninger N, Krieglstein CF. Living donor kidney transplantation: impact of differentiated immunosuppressive regimen. Transplant Proc. 2005;37:1616-1617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Simforoosh N, Basiri A, Fattahi MR, Einollahi B, Firouzan A, Pour-Reza-Gholi F, Nafar M, Farrokhi F. Living unrelated versus living related kidney transplantation: 20 years’ experience with 2155 cases. Transplant Proc. 2006;38:422-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Ahmad N, Ahmed K, Khan MS, Calder F, Mamode N, Taylor J, Koffman G. Living-unrelated donor renal transplantation: an alternative to living-related donor transplantation? Ann R Coll Surg Engl. 2008;90:247-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Ishikawa N, Yagisawa T, Kimura T, Sakuma Y, Fujiwara T, Nukui A, Yashi M. Kidney transplantation of living unrelated and ABO-incompatible donor-recipient combinations. Transplant Proc. 2013;45:1242-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Santori G, Barocci S, Fontana I, Bertocchi M, Tagliamacco A, Biticchi R, Valente U, Nocera A. Kidney transplantation from living donors genetically related or unrelated to the recipients: a single-center analysis. Transplant Proc. 2012;44:1892-1896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Matter YE, Nagib AM, Lotfy OE, Alsayed AM, Donia AF, Refaie AF, Akl AI, Abbas MH, Abuelmagd MM, Shaeashaa HA. Impact of Donor Source on the Outcome of Live Donor Kidney Transplantation: A Single Center Experience. Nephrourol Mon. 2016;8:e34770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Ali AA, Al-Saedi AJ, Al-Mudhaffer AJ, Al-Taee KH. Five years renal transplantation data: Single-center experience from Iraq. Saudi J Kidney Dis Transpl. 2016;27:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Terasaki PI, Cecka JM, Gjertson DW, Takemoto S. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med. 1995;333:333-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 927] [Cited by in RCA: 867] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 21. | Gheith O, Sabry A, El-Baset SA, Hassan N, Sheashaa H, Bahgat S, El-Shahawy el-M. Study of the effect of donor source on graft and patient survival in pediatric renal transplant recipients. Pediatr Nephrol. 2008;23:2075-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Delmonico FL. The development of the Declaration of Istanbul on Organ Trafficking and Transplant Tourism. Nephrol Dial Transplant. 2008;23:3381-3382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Ghods AJ, Savaj S. Iranian model of paid and regulated living-unrelated kidney donation. Clin J Am Soc Nephrol. 2006;1:1136-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 133] [Article Influence: 7.0] [Reference Citation Analysis (0)] |