Published online Sep 9, 2021. doi: 10.5492/wjccm.v10.i5.290
Peer-review started: April 9, 2021
First decision: July 27, 2021
Revised: July 28, 2021
Accepted: August 6, 2021
Article in press: August 6, 2021
Published online: September 9, 2021
Processing time: 153 Days and 8 Hours
The clinical benefits of steroid administration during cardiac arrest remain unclear. Several studies reported that patients who received steroids after achieving a return of spontaneous circulation (ROSC) had better outcomes, but few studies have investigated the benefits of steroid administration during resuscitation. We hypothesized that administration of steroid during cardiac arrest would be associated with better clinical outcomes in adults with cardiac arrest.
To investigate the effect of steroid administration during cardiac arrest and the outcomes of resuscitation.
We included studies of participants older than 18 years of age who experienced cardiac arrest and included at least one arm that received corticosteroids during cardiac arrest. A literature search of PubMed and Embase on 31 January 2021 retrieved placebo-controlled studies without limitation for type, location, and initial presenting rhythm of cardiac arrest. The study outcomes were reported by odds ratios (ORs) compared with placebo. The primary outcome was survival rate at hospital discharge. Secondary outcomes included a sustained ROSC, survival rate at hospital admission, and neurological outcome at hospital discharge.
Six studies including 146262 participants were selected for analysis. The risk of bias ranged from low to high for randomized-controlled trials (RCTs) and low (for non-RCTs). Steroid administration was associated with increased survival at hospital discharge [OR: 3.51, 95% confidence interval (CI): 1.98-6.20, P < 0.001], and steroid administration during cardiac arrest was associated with both an increased rate of sustained ROSC (OR: 1.81, 95%CI: 1.91-4.02, P < 0.001) and a favorable neurological outcome at hospital discharge (OR: 3.02, 95%CI: 1.26-7.24, P = 0.01).
Steroid administration during cardiac arrest was associated with better outcomes of resuscitation. Further study of the use of steroid in the selected circumstances are warranted.
Core Tip: Several studies have demonstrated that patients who receive steroids after achieving a return of spontaneous circulation (ROSC) had better outcomes. Few studies have investigated steroid administration during resuscitation, and the results are not clear. We conducted a systematic review and meta-analysis of the clinical benefits of steroids during cardiac arrest. The analysis included six studies and found that steroid administration during cardiac arrest was associated with better outcomes of resuscitation, including survival rate at hospital discharge, sustained ROSC, and favorable neurological outcome at hospital discharge.
- Citation: Wongtanasarasin W, Krintratun S. Clinical benefits of corticosteroid administration during adult cardiopulmonary resuscitation: A systemic review and meta-analysis. World J Crit Care Med 2021; 10(5): 290-300
- URL: https://www.wjgnet.com/2220-3141/full/v10/i5/290.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v10.i5.290
Cardiac arrest is an important public health problem worldwide. In the United States, cardiac arrest accounts for around 320000 to 360000 deaths each year[1,2]. A study in the United States reported a rate of return of spontaneous circulation (ROSC) of up to 72%[3]. Nevertheless, the reported global outcomes of 30% for ROSC, 8% survival at hospital discharge, 11% 1-mo survival, and 7.7% 1-year survival are quite different[4]. Improving the overall survival of cardiac arrest depends on multiple factors, including type of initial presenting rhythm, bystander cardiopulmonary resuscitation (i.e., CPR), the witnesses present, and interventions during and after resuscitation[5-7].
Previous studies have demonstrated that patients who receive hydrocortisone or methylprednisolone after achieving ROSC had improved survival after cardiac arrest[7-9]. On the other hand, studies of corticosteroid administration during resuscitation are few and unclear[10,11]. A randomized-controlled trial (RCT) by Mentzelopoulos et al[9] found that a combination of vasopressin, steroid, and epinephrine administered during resuscitation and with post-resuscitation shock resulted in improved survival at hospital discharge with a favorable neurological outcome. However, Tsai et al[11] reported that administration of hydrocortisone during cardiac arrest was associated with an improved ROSC rate in out-of-hospital cardiac arrest (referred to as OHCA) patients but was not associated with increased survival at hospital discharge. For that reason, we conducted an up-to-date systematic review and meta-analysis to investigate the effect of steroid administration during cardiac arrest and on the outcomes of resuscitation, including survival rate at hospital discharge, sustained ROSC, survival at hospital admission, and neurological outcomes at discharge.
This systematic review and meta-analysis was prepared following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (i.e., PRISMA) statement guidelines[12]. The protocol was prospectively registered with PROSPERO international prospective register of systematic reviews in health and social care (ID: CRD42021227093).
Two authors independently searched two standard databases, PubMed and Embase, from their inception until 31 January 2021, without language restriction. The search words “steroid,” “glucocorticoid,” “methylprednisolone,” “dexamethasone,” “cardiac arrest,” “cardiopulmonary resuscitation,” “heart arrest,” and “cardiopulmonary arrest” were the Medical Subject Headings used, in combination and with various spellings and endings. We also searched relevant reviews and their references to identify additional eligible studies. In addition, we searched for any unpublished trials registered on the “clinicaltrials.gov” Internet site.
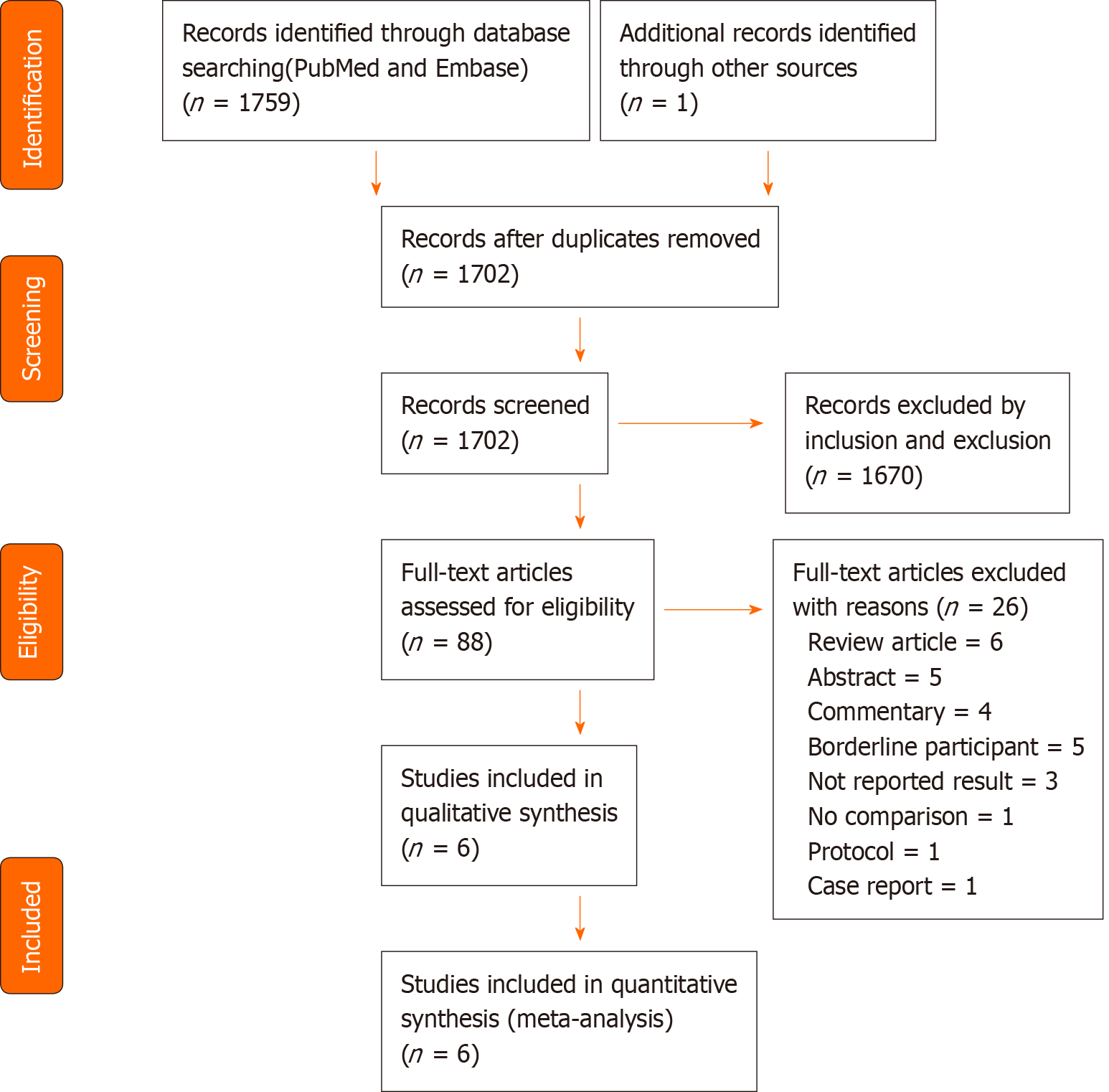
The selection criteria were: (1) Inclusion of adults ≥ 18 years of age with cardiac arrest, regardless of initial presenting rhythm and location (i.e., inpatient or out-of-hospital); (2) At least one arm having received a corticosteroid during cardiac arrest; (3) Reporting of one of the following, sustained ROSC defined as not requiring CPR for a consecutive 15 min[9] or 20 min[7] or longer, survival at hospital admission, survival at hospital discharge, and neurological outcome at discharge. We excluded animal studies, studies without a control group (e.g., case reports, case series), and review articles. Two authors independently screened the search results to identify eligible studies. Full-text articles of the retrieved studies were collected and independently assessed by two authors against the prespecified criteria (Figure 1). Any disagreements were discussed with a third-party and concluded by consensus.
The primary outcome was survival to hospital discharge. The secondary outcomes were sustained ROSC, survival to hospital admission, and favorable neurological outcome at discharge, which was defined as a cerebral performance category score of 1-2 or a modified Rankin Score (commonly referred to as mRS) of 0-3.
Two authors individually extracted data from the selected articles using a standard data collection form. The data included basic characteristics (first author, publication year, study design, study location and setting, number and age of participants), initial presenting rhythm, treatment and interventions in the study groups, and the outcomes of interest. In cases of incomplete or missing data, or for clarification, we attempted to contact the corresponding author by email. Two authors independently assessed the risk of study bias using the Good Research for Comparative Effectiveness (referred to as GRACE) checklist for observational studies and the modified version of the Cochrane Collaboration tool for assessing the trial risk of bias for RCTs[13,14]. Discrepancies in the extracted data were resolved by discussion and overall consensus.
Data were imported into prepared record forms. In the meta-analysis, pooled odds ratios (ORs) were calculated by the Mantel-Haenszel method as summary measures for analysis of the dichotomous outcomes of interest. Heterogeneity among the included studies was estimated by the I2 statistic (the percentage of total variability across studies due to heterogeneity). Values of < 25%, 25%-50%, and > 50% were considered as low, moderate, and high heterogeneity, respectively[15]. Data were pooled with a fixed-effect model, but if there was evidence of high heterogeneity (I2 > 50%), a random-effects model was used instead. Publication bias arising from small-study effects was evaluated by visual examination of funnel plots and Egger’s test. Review Manager version 5.3 (Nordic Cochrane Center, Cochrane Collaboration, 2014, Copenhagen, Denmark) was used to perform the quantitative statistical analysis[16]. All tests were two-tailed, and P values < 0.05 were considered statistically significant.
The PRISMA flow diagram (Figure 1) shows how the 1760 retrieved studies were screened for inclusion in the review and meta-analysis. After removing duplicate studies, 1702 remained. Of those, 1670 were excluded following screening of the abstract to identify the inclusion and exclusion criteria. Full-text copies of the remaining 32 publications were screened before selecting six studies (Table 1) with a total of 146262 participants for inclusion in the systematic review and meta-analysis.
| Ref. | Age, yr | Study design, country/territory, enrollment period | Sample size (exposure/control) | Location | Shockable initial rhythm (exposure/control), % | Witnessed arrest (exposure/control), % | Bystander CPR (exposure/control), % | Intervention | Comparator | Outcomes of interest |
| Bolvardi et al[17], 2016 | 68.9 ± 16.0 | RCT, Iran, 2015 | 50 (25/25) | OHCA | 28 (20/36) | N/A | N/A | 1 mg epinephrine plus 125 mg methylpredni-solone during the first cycle of resuscitation | 1 mg epinephrine plus saline during the first cycle of resuscitation | Successful resuscitation; Survival to hospital discharge; Neurological outcomes at hospital discharge |
| Mentzelopoulos et al[9], 2009 | 67.4 | RCT, Greece, Jul 2006 to Mar 2007 | 100 (48/52) | IHCA | 14 (15/13) | 81 (79/83) | N/A | 1 IU vasopressin plus 1 mg epinephrine for the first 5 CPR cycles and 40 mg methylprednisolone. Shock after resuscitation was treated with stress-dose hydrocortisone (300 mg daily for 7 d with gradual tapering) | Placebo (saline) plus 1 mg epinephrine for the first 5 CPR cycles. Shock after resuscitation was treated with saline placebo | Sustained ROSC; Survival to hospital discharge |
| Mentzelopoulos et al[7], 2013 | 63.0 | RCT, Greece, Sep 2008 to Oct 2010 | 268 (130/138) | IHCA | 16.8 (16.7/16.9) | 92.2 (91.3/93/1) | N/A | 1 IU vasopressin plus 1 mg epinephrine for the first 5 CPR cycles and 40 mg methylprednisolone. Shock after resuscitation was treated with stress-dose hydrocortisone (300 mg daily for 7 d with gradual tapering) | Placebo (saline) plus 1 mg epinephrine for the first 5 CPR cycles. Shock after resuscitation was treated with saline placebo | ROSC ≥ 20 min; Survival to hospital discharge; Neurological outcomes at hospital discharge |
| Paris et al[10], 1984 | N/A | RCT, United States, Mar 1982 to Jan 1983 | 83 (37/46) | OHCA | 48.2 (41.3/56.8) | N/A | 30.1 (36.9/21.6) | 100 mg dexamethasone | The same volume of saline | Survival to hospital admission; Survival to hospital discharge |
| Tsai et al[11], 2007 | 72.5 ± 16.2 | Prospective non-RCT, Taiwan, Oct 2004 to Jul 2005 | 97 (36/61) | Non-trauma, OHCA | 10.3 (11/10) | 75.3 (83/71) | N/A | 100 mg hydrocortisone | Saline as placebo | Sustained ROSC; Survival to hospital discharge |
| Tsai et al[18], 2016 | 68.2 | Retrospective, Taiwan, 2004-2011 | 145644 (2912/142732) | IHCA (at the ED) | 20.6 (33.4/20.3) | N/A | N/A | Any forms of steroid use | No steroid use | Survival to hospital admission; Survival to hospital discharge; 1-yr survival |
A total of six articles, published between 1984 and 2016, were included for data extraction and meta-analysis. Four were RCTs[7,9,10,17], one was prospective non-RCT[11], and the other was a retrospective study[18]. The studies were conducted in Asia (n = 3), Europe (n = 2), and North America (n = 1). Three studies included patients with OHCA[10,11,17] and three included patients with in-hospital cardiac arrest[7,9,18]. Two trials evaluated the clinical benefits of co-intervention with corticosteroid, vasopressin, or epinephrine protocols[7,9]. Four trials directly investigated the efficacy of steroids alone, including methylprednisolone[17], dexamethasone[10], hydrocortisone[11], and other steroids[18]. More than three-fourths of the cardiac arrests were witnessed. All studies reported the efficacy of corticosteroids on survival to hospital discharge. Table 1 summarizes the characteristics of the included studies. The risk of bias was high in two of the RCTs and low in two. Randomization and deviation from the intended interventions contributed to high risk of bias. All four RCTs had a low risk of bias for measurement of outcome. Both non-RCTs were determined to be of sufficient quality and having a low risk of bias according to the GRACE checklist. Table 2 summarizes the risk of bias assessment.
| Randomized-controlled trials | ||||||||||||||||
| Ref. | Randomization | Deviation from the intended interventions | Missing outcome data | Measurement of outcome | Selection of the reported result | Overall | ||||||||||
| Bolvardi et al[17], 2016 | Low | High | Some concerns | Low | Some concerns | High | ||||||||||
| Mentzelopoulos et al[9], 2009 | Low | Low | Low | Low | Low | Low | ||||||||||
| Mentzelopoulos et al[7], 2013 | Low | Low | Low | Low | Low | Low | ||||||||||
| Paris et al[10], 1984 | High | Low | Some concerns | Low | Some concerns | High | ||||||||||
| Non-randomized-controlled trials | ||||||||||||||||
| Ref. | Adequate treatment | Adequate outcomes | Objective outcomes | Valid outcomes | Similar outcomes | Covariates recorded | New initiators | Concurrent comparators | Covariates accounted for | Immortal time bias | Sensitivity analysis | |||||
| D1 | D2 | D3 | D4 | D5 | D6 | M1 | M2 | M3 | M4 | M5 | ||||||
| Tsai et al[11], 2007 | + | + | + | + | + | + | + | + | + | + | + | |||||
| Tsai et al[18], 2016 | + | + | + | + | + | + | + | + | + | + | + | |||||
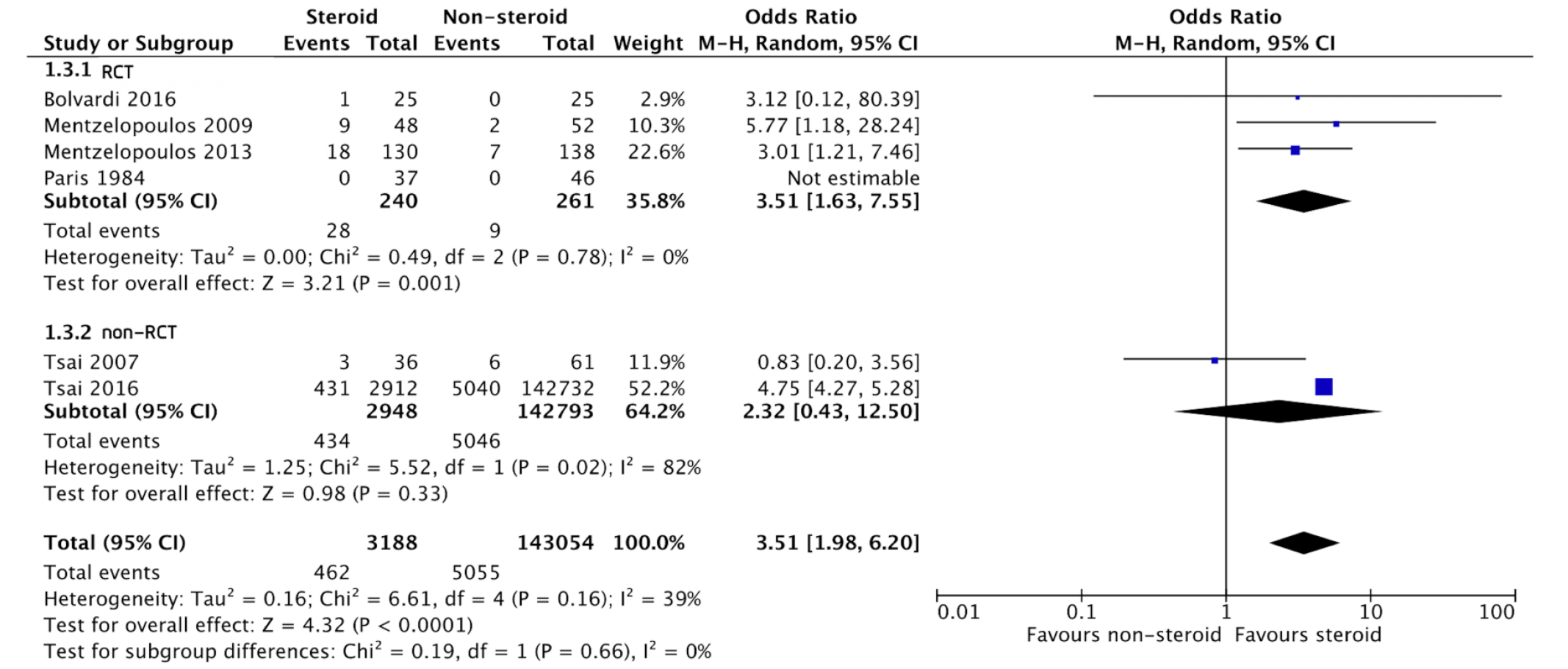
Overall survival rate at hospital discharge: All six studies reported the association between steroid use and the survival rate at hospital discharge[7,9-11,17,18]. Four of the six were RCTs and two were non-RCTs. The overall effect size demonstrated a significant association between steroid use and survival rate at hospital discharge [OR: 3.51, 95% confidence interval (CI): 1.98-6.20, P < 0.001]. Subgroup analyses found that for the RCTs, effect size had a significant association between steroid administration and survival rate at hospital discharge (OR: 3.51, 95%CI: 1.63-7.55, P = 0.001). Conversely, steroids given during cardiac arrest in the non-RCT studies were not associated with increased survival rate at hospital discharge (OR: 2.32, 95%CI: 0.43-12.50, P = 0.33). There was no significant heterogeneity between the subgroups (I2 = 0%, P = 0.66; Figure 2).
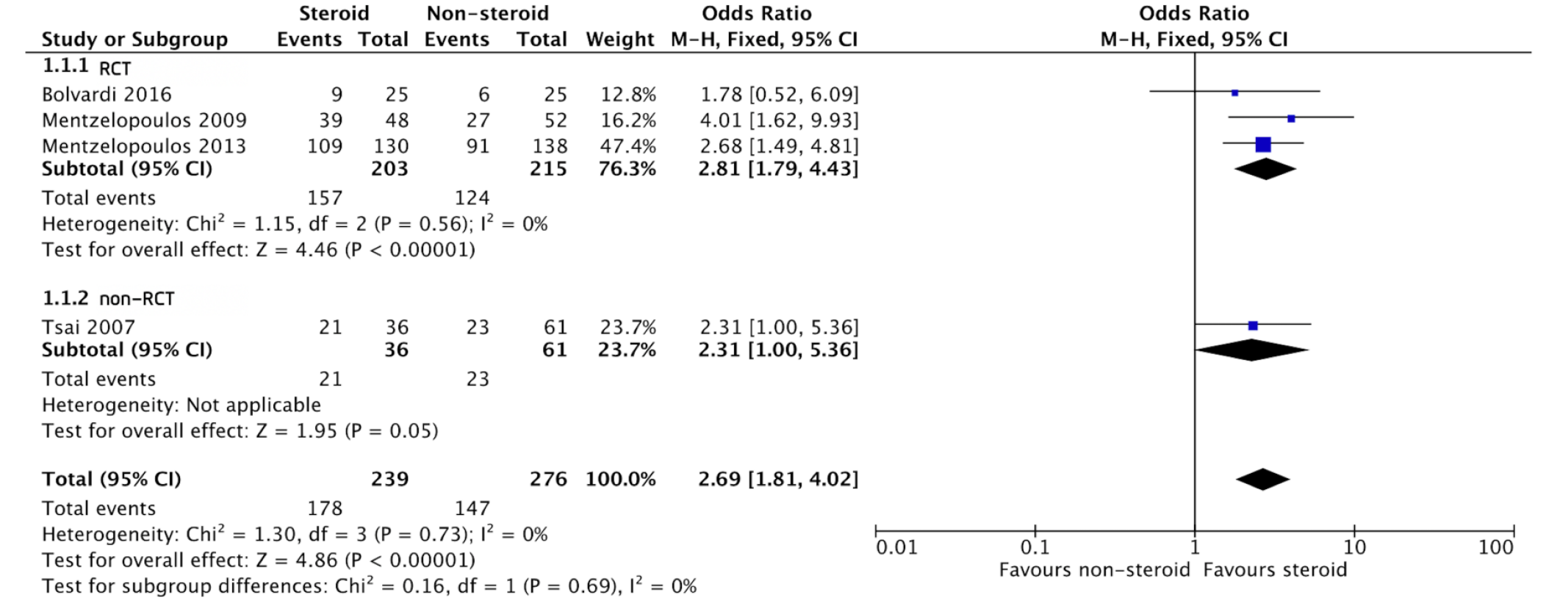
Rate of sustained ROSC: Four studies examined the association between steroid use and the rate of sustained ROSC[7,9,11,17]. The pooled data was homogeneous (I2 = 0%, P < 0.001). Patients who received a steroid during cardiac arrest had a better chance of sustained ROSC (OR: 2.69, 95%CI: 1.81-4.02, P < 0.001) than those who had not received a steroid. Subgroup analyses yielded similar results for RCTs and non-RCTs (Figure 3).
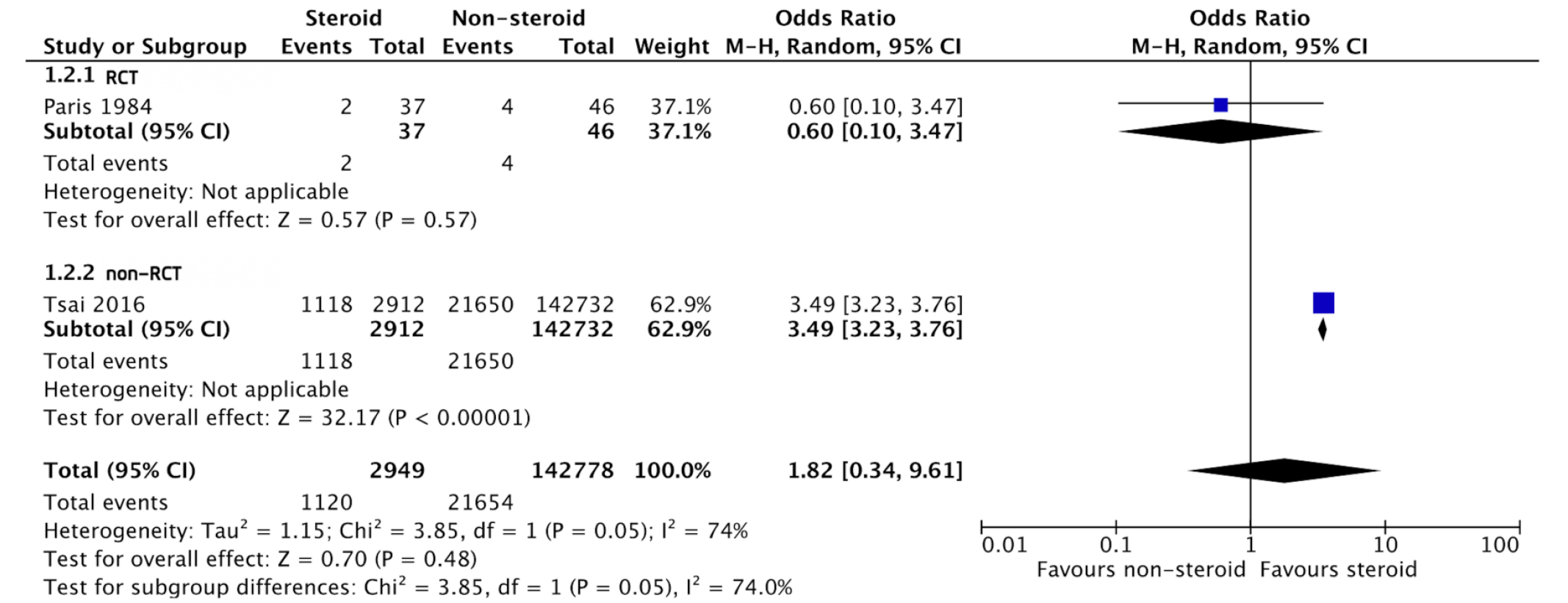
Overall survival rate at hospital admission: Two studies reported the association between steroid use and overall survival at hospital admission[10,18]. One was an RCT and the other was a non-RCT. Steroid administration during cardiac arrest did not show a survival benefit at hospital admission based on the pooled data (OR: 1.82, 95%CI: 0.34-9.61, P = 0.48; Figure 4).
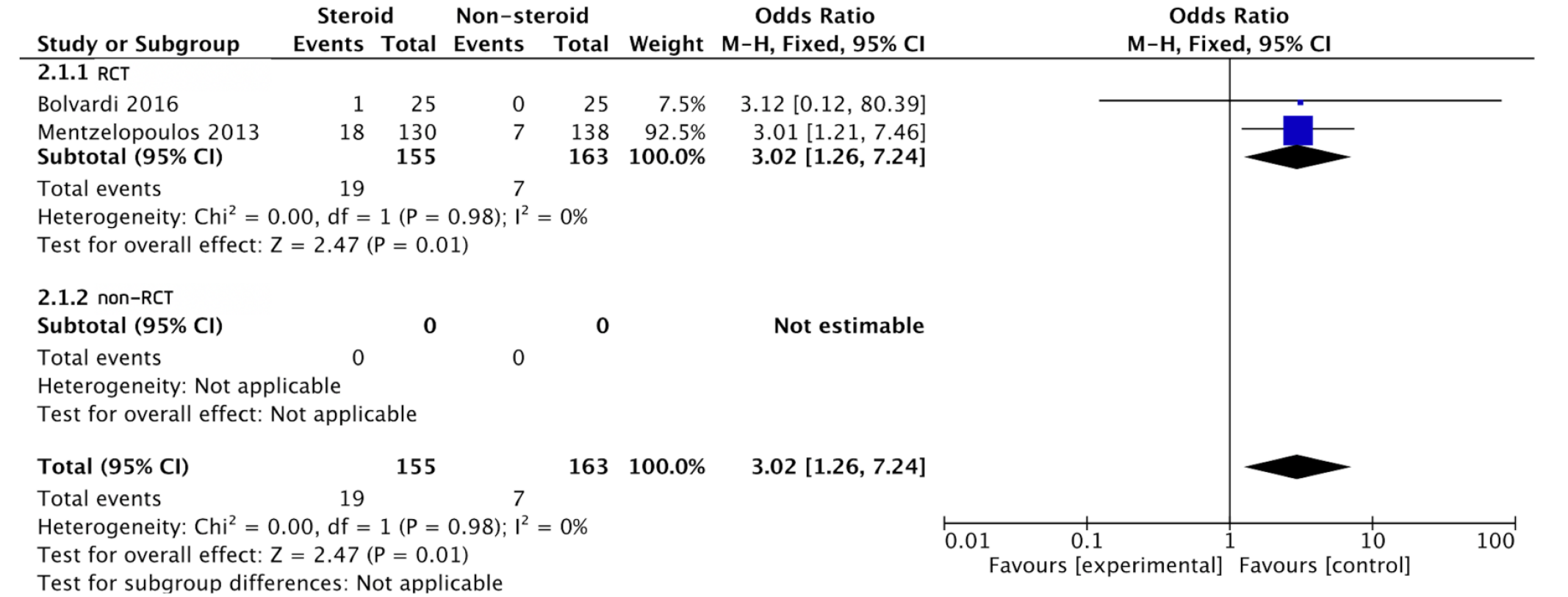
Favorable neurological outcomes at hospital discharge: Two studies investigated the association between steroid use and the neurological outcome at hospital discharge and both were RCTs[7,17]. The overall effect size indicated that administration of steroid during cardiac arrest was significantly associated with an increased rate of favorable neurological outcomes at hospital discharge (OR: 3.02, 95%CI: 1.26-7.24, P = 0.01; Figure 5).
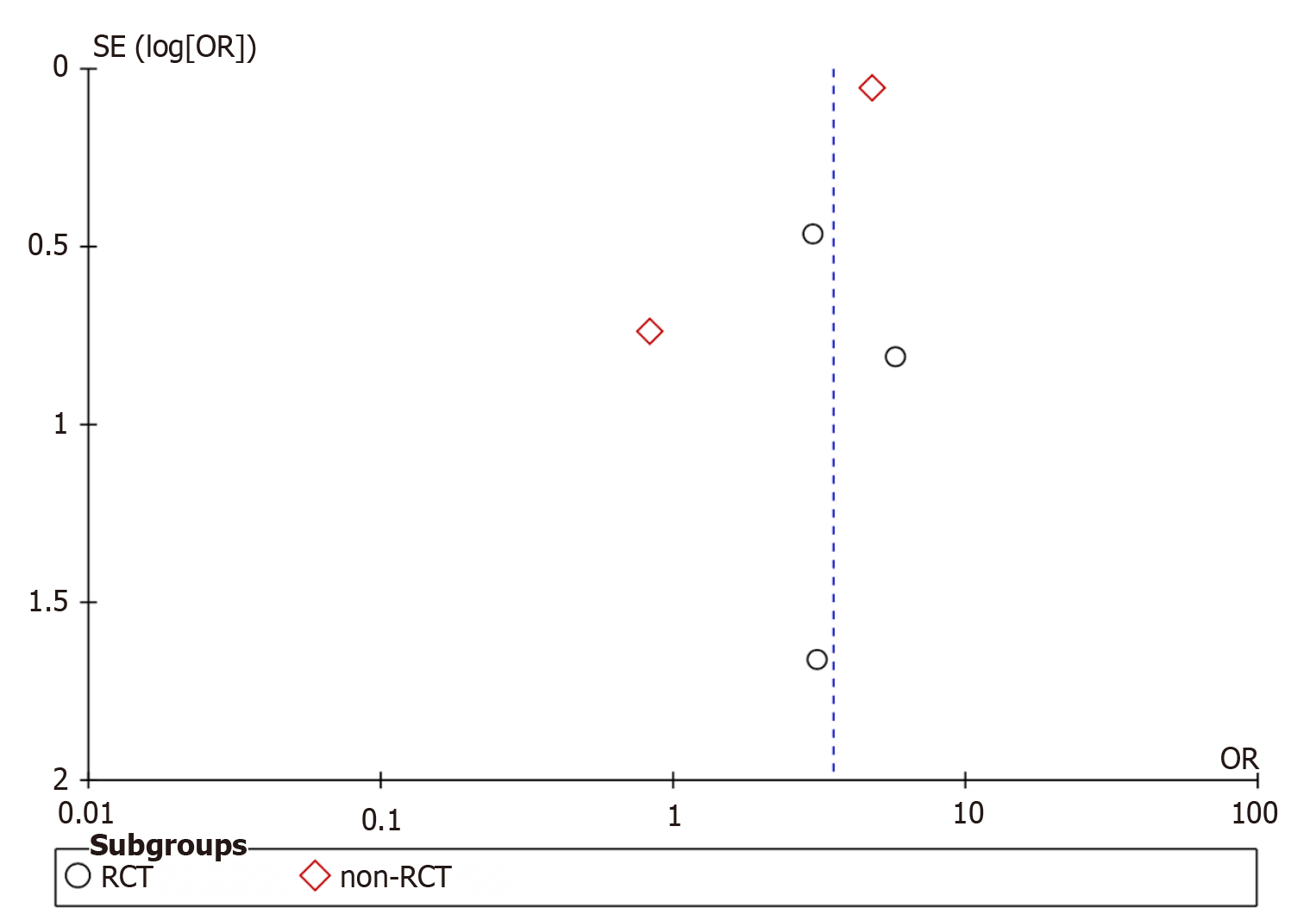
Publication bias: As shown in the funnel plot for the meta-analysis of the effect of steroid use and the primary outcome of survival rate at hospital discharge (Figure 6), there was no evidence of significant publication bias.
This meta-analysis compared the evidence on the use of steroids in adult cardiac arrest with placebo or no use of steroids. Review of the evidence found that steroid use was associated with an increased survival rate at hospital discharge, sustained ROSC, and favorable neurological outcomes at discharge. The overall study risk of bias ranged from low in two RCTs and both non-RCTs to high in two RCTs.
The administration of corticosteroids during cardiac arrest has been proposed for decades; however, there is no strong evidence to support the efficacy of steroids to improve the outcomes of resuscitation[7,19]. Recent studies have described cardiac arrest-related adrenal insufficiency, finding that the condition was associated with increased mortality[19,20]. Ito et al[20] reported that cortisol levels were moderately low during and after cardiac arrest and CPR, which suggests impairment of adrenal function. Corticosteroids have anti-inflammatory and anti-apoptotic activity that can prevent organ toxicity, especially in patients with cardiac arrest[21]. The findings of this review are consistent with previous studies that documented the benefits of steroid administration in patients who survived cardiac arrest[8,22,23]. Patients who received steroids during cardiac arrest had better outcomes than those who did not receive steroids. The corticosteroid effects included short-term survival, represented by the rate of sustained ROSC, and survival at hospital discharge. Cardiac arrest results in a sepsis-like stage, with interruption of blood flow that leads to inadequate oxygen delivery, vasodilation, and cytokine activation[24,25]. Corticosteroid administration has been shown to improve cardiovascular function and to reduce a catecholamine surge, thereby decreasing inflammation and reversing the shock that occurs after cardiac arrest[7,11,19].
Two studies included in this review demonstrated a benefit of the combined administration of vasopressin, methylprednisolone, and epinephrine on improved survival at hospital discharge[7,9]. Cardiac arrest causes an overwhelming release of several stress hormones[7,25,26]. Vasopressin is a non-adrenergic vasopressor that is released from the anterior pituitary gland[27], and stimulation of plasma adrenocorticotropin (commonly known as ACTH) release by vasopressin might preserve hemodynamic function and promote ROSC[28,29].
This review has some limitations. First, the use of steroids defined in this review was different among studies, which resulted in inconclusive evidence and findings that might not be generalized to other populations. Second, our review did not mention the harmful effects of steroid administration, which might influence the clinical outcomes. Third, we included both RCTs and non-RCTs in the meta-analysis. Despite analysis of both groups separately, non-RCTs such as retrospective of observational studies carry a high risk of confounding by indication and selection bias and may have led to the heterogeneity observed in this study. Furthermore, considering all of the included studies, Tsai et al[18] had enrolled up to 95% of the participants in this review. However, the results of this study do not conflict from those of other studies. Finally, the included studies were conducted in different places and at different times. Standard guidelines regarding the management of patients with cardiac arrest usually update every 5 years, which will lead to variability in interventions and protocols across included studies.
Although the overall risk of bias of included studies ranged from low to high, steroid administration during cardiac arrest was associated with an increased rate of survival at hospital discharge, sustained ROSC, and favorable neurological outcome at hospital discharge. Steroid use may be optional for adults with cardiac arrest; however, further study concerning the use of steroid in the prepared protocol and selected circumstances are warranted.
The clinical benefits of steroid administration during adult cardiac arrest remain controversial. According to the latest guidelines for managing adult cardiac arrest, steroid was not routinely recommended giving during resuscitation.
Previous studies have shown that patients who receive steroids after return of spontaneous circulation (ROSC) have improved outcomes. In contrast, few studies have investigated the benefits of steroid administration during resuscitation and the results are unclear.
The objectives of this review were to investigate the clinical benefits of steroids during adult cardiac arrest, including the survival rate at hospital discharge, sustained ROSC, the survival rate at hospital admission, and neurological outcome at hospital discharge.
We conducted a systematic review and meta-analysis.
Steroid administration was associated with increased survival at hospital discharge. Steroid administration during cardiac arrest was associated with an increased rate of sustained ROSC and a favorable neurological outcome at hospital discharge.
Although we could not draw firm conclusions, the use of steroids during cardiac arrest was associated with improved outcomes of resuscitation.
Further study concerning the use of steroid in the prepared protocol and selected circumstances are warranted.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: Thai College of Emergency Physician.
Specialty type: Critical care medicine
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Santomauro M S-Editor: Gao CC L-Editor: A P-Editor: Wang LYT
| 1. | Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56-e528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4294] [Cited by in RCA: 5897] [Article Influence: 982.8] [Reference Citation Analysis (5)] |
| 2. | Holmberg MJ, Ross CE, Fitzmaurice GM, Chan PS, Duval-Arnould J, Grossestreuer AV, Yankama T, Donnino MW, Andersen LW; American Heart Association’s Get With The Guidelines–Resuscitation Investigators. Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States. Circ Cardiovasc Qual Outcomes. 2019;12:e005580. [PubMed] |
| 3. | Chan PS, Tang Y; American Heart Association's Get With the Guidelines®‐Resuscitation Investigators. Risk-Standardizing Rates of Return of Spontaneous Circulation for In-Hospital Cardiac Arrest to Facilitate Hospital Comparisons. J Am Heart Assoc. 2020;9:e014837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, Zong Q, Chen S, Lv C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 533] [Article Influence: 106.6] [Reference Citation Analysis (0)] |
| 5. | Skogvoll E, Nordseth T, Sutton RM, Eftestøl T, Irusta U, Aramendi E, Niles D, Nadkarni V, Berg RA, Abella BS, Kvaløy JT. Factors affecting the course of resuscitation from cardiac arrest with pulseless electrical activity in children and adolescents. Resuscitation. 2020;152:116-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Czapla M, Zielińska M, Kubica-Cielińska A, Diakowska D, Quinn T, Karniej P. Factors associated with return of spontaneous circulation after out-of-hospital cardiac arrest in Poland: a one-year retrospective study. BMC Cardiovasc Disord. 2020;20:288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Mentzelopoulos SD, Malachias S, Chamos C, Konstantopoulos D, Ntaidou T, Papastylianou A, Kolliantzaki I, Theodoridi M, Ischaki H, Makris D, Zakynthinos E, Zintzaras E, Sourlas S, Aloizos S, Zakynthinos SG. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest: a randomized clinical trial. JAMA. 2013;310:270-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 224] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 8. | Niimura T, Zamami Y, Koyama T, Izawa-Ishizawa Y, Miyake M, Koga T, Harada K, Ohshima A, Imai T, Kondo Y, Imanishi M, Takechi K, Fukushima K, Horinouchi Y, Ikeda Y, Fujino H, Tsuchiya K, Tamaki T, Hinotsu S, Kano MR, Ishizawa K. Hydrocortisone administration was associated with improved survival in Japanese patients with cardiac arrest. Sci Rep. 2017;7:17919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Mentzelopoulos SD, Zakynthinos SG, Tzoufi M, Katsios N, Papastylianou A, Gkisioti S, Stathopoulos A, Kollintza A, Stamataki E, Roussos C. Vasopressin, epinephrine, and corticosteroids for in-hospital cardiac arrest. Arch Intern Med. 2009;169:15-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 176] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 10. | Paris PM, Stewart RD, Deggler F. Prehospital use of dexamethasone in pulseless idioventricular rhythm. Ann Emerg Med. 1984;13:1008-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Tsai MS, Huang CH, Chang WT, Chen WJ, Hsu CY, Hsieh CC, Yang CW, Chiang WC, Ma MH, Chen SC. The effect of hydrocortisone on the outcome of out-of-hospital cardiac arrest patients: a pilot study. Am J Emerg Med. 2007;25:318-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47200] [Article Influence: 2950.0] [Reference Citation Analysis (0)] |
| 13. | Dreyer NA, Velentgas P, Westrich K, Dubois R. The GRACE checklist for rating the quality of observational studies of comparative effectiveness: a tale of hope and caution. J Manag Care Spec Pharm. 2014;20:301-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1361] [Cited by in RCA: 2932] [Article Influence: 488.7] [Reference Citation Analysis (0)] |
| 15. | Fletcher J. What is heterogeneity and is it important? BMJ. 2007;334:94-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 397] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 16. | The Nordic Cochrane Centre. Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. |
| 17. | Bolvardi E, Seyedi E, Seyedi M, Abbasi AA, Golmakani R, Ahmadi K. Studying the influence of epinephrine mixed with prednisolone on the neurologic side effects after recovery in patients suffering from cardiopulmonary arrest. Biomed Pharmacol J. 2016;9:209-214. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Tsai MS, Chuang PY, Yu PH, Huang CH, Tang CH, Chang WT, Chen WJ. Glucocorticoid use during cardiopulmonary resuscitation may be beneficial for cardiac arrest. Int J Cardiol. 2016;222:629-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Varvarousi G, Stefaniotou A, Varvaroussis D, Xanthos T. Glucocorticoids as an emerging pharmacologic agent for cardiopulmonary resuscitation. Cardiovasc Drugs Ther. 2014;28:477-488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Ito T, Saitoh D, Takasu A, Kiyozumi T, Sakamoto T, Okada Y. Serum cortisol as a predictive marker of the outcome in patients resuscitated after cardiopulmonary arrest. Resuscitation. 2004;62:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Hall ED. Neuroprotective actions of glucocorticoid and nonglucocorticoid steroids in acute neuronal injury. Cell Mol Neurobiol. 1993;13:415-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 101] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Tsai MS, Chuang PY, Huang CH, Tang CH, Yu PH, Chang WT, Chen WJ. Postarrest Steroid Use May Improve Outcomes of Cardiac Arrest Survivors. Crit Care Med. 2019;47:167-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Donnino MW, Andersen LW, Berg KM, Chase M, Sherwin R, Smithline H, Carney E, Ngo L, Patel PV, Liu X, Cutlip D, Zimetbaum P, Cocchi MN; Collaborating Authors from the Beth Israel Deaconess Medical Center’s Center for Resuscitation Science Research Group. Corticosteroid therapy in refractory shock following cardiac arrest: a randomized, double-blind, placebo-controlled, trial. Crit Care. 2016;20:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 24. | Liu B, Zhang Q, Li C. Steroid use after cardiac arrest is associated with favourable outcomes: a systematic review and meta-analysis. J Int Med Res. 2020;48:300060520921670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Adrie C, Adib-Conquy M, Laurent I, Monchi M, Vinsonneau C, Fitting C, Fraisse F, Dinh-Xuan AT, Carli P, Spaulding C, Dhainaut JF, Cavaillon JM. Successful cardiopulmonary resuscitation after cardiac arrest as a "sepsis-like" syndrome. Circulation. 2002;106:562-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 707] [Cited by in RCA: 734] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 26. | Smithline H, Rivers E, Appleton T, Nowak R. Corticosteroid supplementation during cardiac arrest in rats. Resuscitation. 1993;25:257-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Cuzzo B, Padala SA, Lappin SL. Treasure Island. In: Treasure Island. London: Faber and Faber Limited, 2021: 180. [DOI] [Full Text] |
| 28. | Lindner KH, Haak T, Keller A, Bothner U, Lurie KG. Release of endogenous vasopressors during and after cardiopulmonary resuscitation. Heart. 1996;75:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 124] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 29. | Kornberger E, Prengel AW, Krismer A, Schwarz B, Wenzel V, Lindner KH, Mair P. Vasopressin-mediated adrenocorticotropin release increases plasma cortisol concentrations during cardiopulmonary resuscitation. Crit Care Med. 2000;28:3517-3521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |