Published online Aug 24, 2024. doi: 10.5306/wjco.v15.i8.1110
Revised: July 10, 2024
Accepted: July 16, 2024
Published online: August 24, 2024
Processing time: 92 Days and 15 Hours
Non-Hodgkin's lymphoma (NHL) is a malignant tumor that originates from the lymphoid tissues and can potentially affect numerous organs within the body. Among these, the skin stands out as one of the primary sites affected by NHL, often presenting with multiple extra-nodal manifestations. In this report, we present an unusual case of NHL involving chronic wounds in the lower extremi
A 19-year-old male patient presented with ulceration of the skin on the left calf near the ankle accompanied by purulent discharge. Subsequent pathologic biopsy confirmed a diagnosis of NHL (extranodal NK/T-cell lymphoma, nasal type). Initial treatment comprised local radiotherapy and wound care; however, the wound exhibited prolonged non-healing. Consequently, the patient underwent a series of interventions including radiotherapy, wound enlargement excision debridement, and peroneal artery perforator flap grafting. Ultimately, successful healing was achieved with favorable postoperative outcomes characterized by good texture of the flap without any signs of rupture or infection.
The combination of radiotherapy, wound enlargement excision debridement, and peroneal artery perforator flap grafting may present a favorable treatment modality for chronic non-healing lower leg wounds resulting from NHL.
Core Tip: Non-Hodgkin's lymphoma represents the majority of lymphoma cases, and extranodal natural killer/T-cell lymphoma, a rare subtype, is characterized by its rarity, high aggressiveness, and poor prognosis. Skin lesions typically present as nodules and hard lumps, with wounds in the lower limbs being relatively uncommon. Here we present the case of a 19-year-old male diagnosed with non-Hodgkin's lymphoma due to an 11-month history of chronic skin breakdown with effusion on the left lower leg near the ankle. Conventional radiotherapy and wound care resulted in poor wound healing. However, after undergoing radiotherapy followed by wound enlargement excision debridement combined with peroneal artery perforator flap grafting, the wound healed successfully.
- Citation: Zhang PS, Wang R, Wu HW, Zhou H, Deng HB, Fan WX, Li JC, Cheng SW. Non-Hodgkin's lymphoma involving chronic difficult-to-heal wounds: A case report. World J Clin Oncol 2024; 15(8): 1110-1116
- URL: https://www.wjgnet.com/2218-4333/full/v15/i8/1110.htm
- DOI: https://dx.doi.org/10.5306/wjco.v15.i8.1110
Non-Hodgkin's lymphoma (NHL) is a malignant tumor originating from lymphatic tissues. Extranodal NK/T-cell lymphoma, as one of the rare types, has a relatively low incidence and can involve the nasal cavity, skin, testes, liver, and spleen. It most often manifests as nasal lesions; however, skin lesions on the lower extremities are uncommon[1,2]. Prolonged non-healing of skin wounds significantly impacts the patient's physical and mental health. Long-term radiotherapy may further complicate wound healing[3]. We here present a rare case of NHL involving chronic difficult-to-heal wounds of the lower extremities and to demonstrate successful outcomes following surgery with radiotherapy and wound enlargement excision debridement combined with peroneal artery perforator flap grafting.
A 19-year-old male presented with an 11-month history of chronic skin ulceration and purulent discharge in the left lower extremity adjacent to the ankle.
An external hospital provided the histopathological biopsy diagnosis of NHL. Unfortunately, the pathology image from the external hospital was missing. For further clarification, the pathology slides were sent to our hospital for examination. Before admission to our hospital, the patient underwent 6 cycles of chemoimmunotherapy (oxaliplatin 130 mg/m2 day 1 + sindelizumab 200 mg day 1, every 3 weeks), in addition to localized lesion radiotherapy 20 times (at a dose of 50 Gy) and wound dressing treatment. Despite these interventions, the wound did not heal over an extended period, prompting his transfer to our facility for further management.
The patient underwent a nasopharyngeal lesion biopsy in 2019, indicating the diagnosis of nasal NK/T cell lymphoma, with a history of long-term radiation therapy, but no other concomitant diseases.
The patient did not have any personal and family history of NHL.
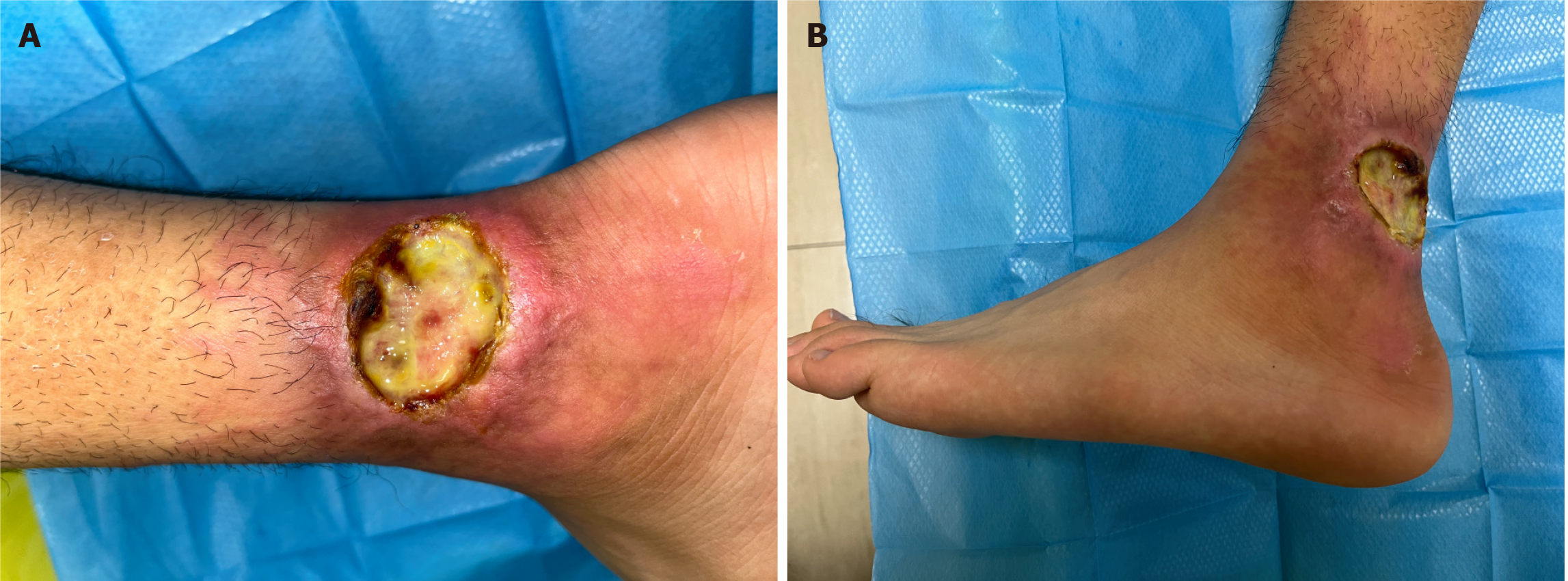
The patient presented with a temperature of 36.8 °C, heart rate of 68 beats/min, respiratory rate of 20 breaths/min, and blood pressure of 120/83 mmHg. On physical examination, the wound was identified in the distal part of the left calf near the lateral aspect of the ankle joint, measuring approximately 3 cm × 5 cm × 0.3 cm. The wound exhibited a light green secretion with exudate and central granulation fibrosis, accompanied by rolled-up edges with fibrosis and scarring. Additionally, redness, swelling, and hyperpigmentation were observed in the surrounding skin (Figure 1).
The levels of ultrasensitive C-reactive protein and ultrasensitive thyrotropin were 2.67 mg/L (reference value: < 1.0 mg/L) and 62.533 mIU/L (reference value 0.38-4.34 mIU/L), respectively; and culture of the wound secretion suggested Pseudomonas aeruginosa. The remaining parameters of routine blood, biochemistry, coagulation function, and calcitonin gene tests were within the normal range.
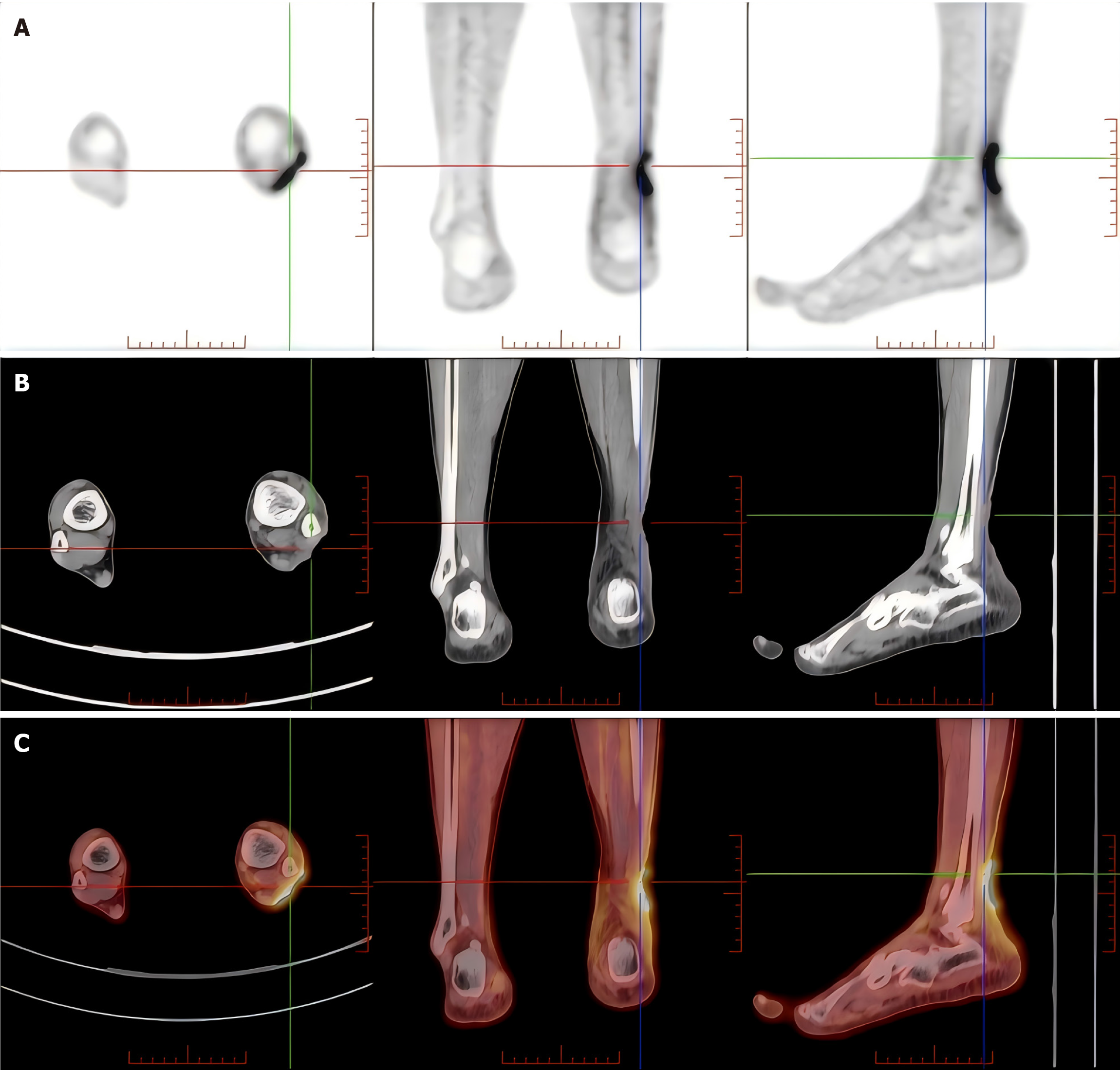
18F-fluorodeoxyglucose whole-body positron emission tomography/computed tomography (CT) revealed localized skin loss with soft tissue shadows and increased metabolism in the left calf near the ankle (Figure 2). Chest CT and color ultrasound of the left lower extremity vein showed no significant abnormalities.
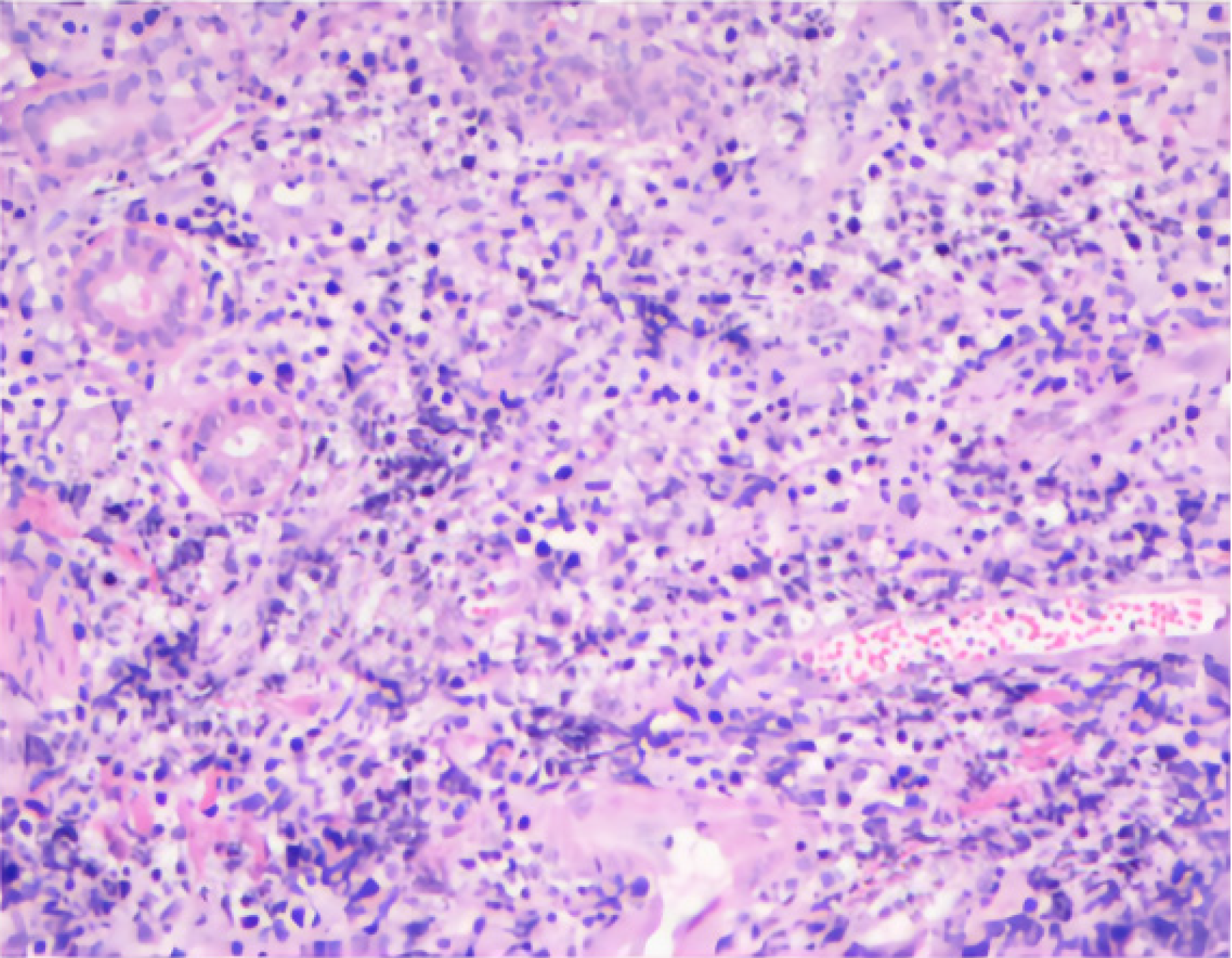
Pathological tissue sections obtained from the patient's previous hospital were sent to our institution for examination, and histopathological analysis of the wound confirmed the presence of extranodal NK/T-cell lymphoma of nasal type (Figure 3). Immunohistochemical analysis revealed that the tumor was positive for CD56, CD2, Ki67 (80%), and Granzyme B and negative for CD3. In situ hybridization showed that EBER was positive (Some pictures are missing).
The patient was diagnosed with extranodal NK/T-cell lymphoma of nasal type, and a subtype of NHL.
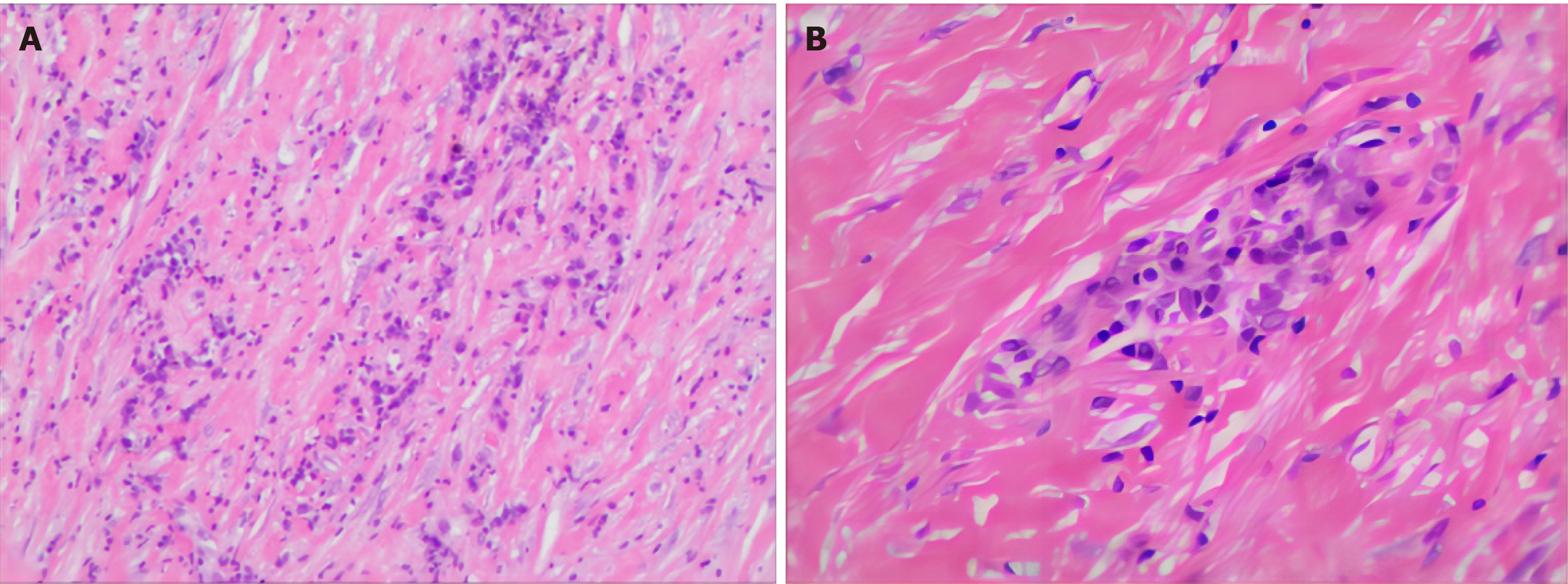
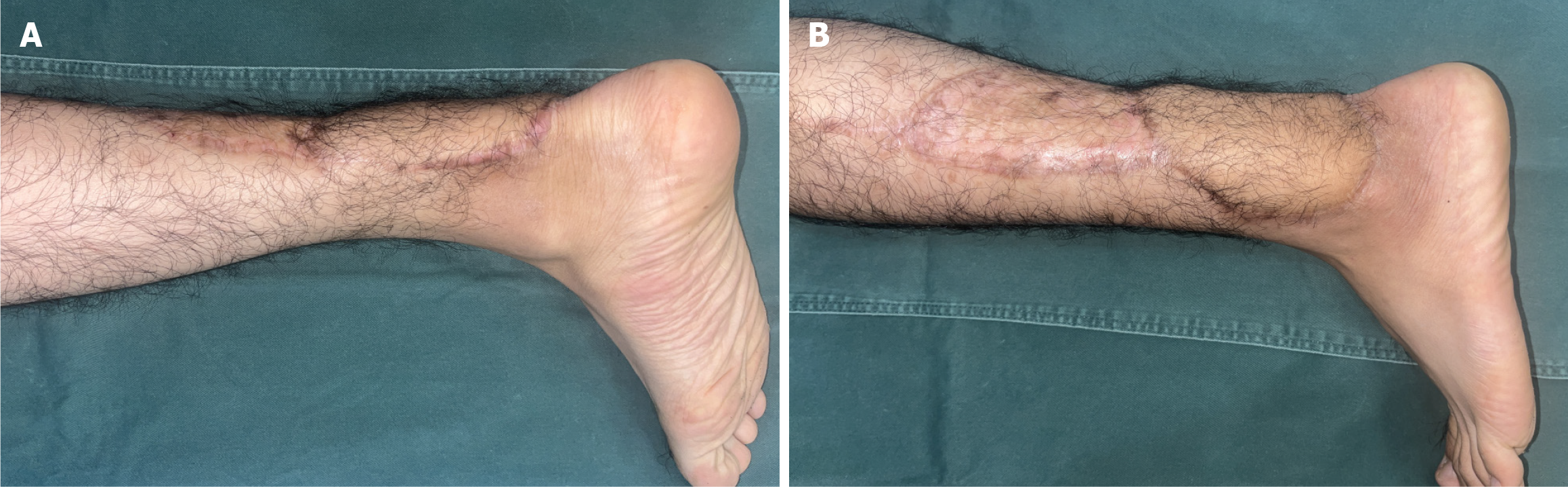
After receiving treatment with oxaliplatin, sindilizumab, and local radiotherapy, the patient was admitted to our hospital for further wound repair. He underwent wound expansion excision and debridement, which involved expanding the wound along the edge by approximately 3 mm to excise the ulcerated area. The cut edge was marked and sent for pathology examination, revealing chronic ulcerative changes accompanied by significant thickening of blood vessel walls and luminal occlusion, with no evidence of neoplastic lesions (Figure 4). Throughout this period, the wound was cleaned and dressings changed multiple times. When there was no obvious purulent secretion or necrotic tissue present on the wound, a re-examination of the left distal calf near the lateral ankle joint revealed a wound measuring approximately 5 cm × 7 cm × 0.3 cm with a few bright red granules on its surface. The Achilles tendon and several tendons of the peroneal longissimus tendon were exposed with dried-up surfaces and slightly reddened swollen surrounding skin (Figure 5A and B).
Considering further closure of the wound after early-stage necrotic tissue removal through debridement (with no bacterial growth observed in subsequent cultures), good granulation growth without obvious exudation led to peroneal artery perforator flap grafting in later stages. Skin from the left thigh was removed for full-thickness skin grafting at donor sites: Preoperative Doppler ultrasonography combined with infrared thermography facilitated localization labeling of peroneal artery perforators for routine flap design, cutting and removal. The transferred peroneal artery flap covered the wound areas while donor sites were closed using full-thickness skin grafts from the left thigh (Figure 5C-F).
During the follow-up visit 1 month later, it was observed that the wound had healed, the skin flap exhibited good texture, and there were no signs of rupture or infection. The postoperative outcome was deemed satisfactory. Follow-up was continued, and the patient returned to the hospital after 1 year for evaluation of the original surgical flap, which had healed well without any recurrence of lymphoma at the primary site of the tumor or other sites (Figure 6).
NHL is a malignant neoplasm of the lymphoid tissue arising from B and T cells, with the potential to manifest at any age and constituting approximately 90% of all lymphomas. It is also linked to a spectrum of etiological factors, encompassing infections, chronic inflammation, environmental triggers, and immunocompromised states, and it has the capacity to involve multiple organ systems including the kidneys, skin, ovaries, and the central nervous system[4,5]. Skin involve
Extranodal NK/T-cell lymphoma nasal type, a subtype of NHL, is associated with a poor prognosis. Localized radioimmunotherapy is a widely accepted treatment[7], but it commonly leads to side effects, with over 90% of patients experiencing skin reactions following radiotherapy or even late radiation tissue injury months or years later[8]. Radiotherapy primarily causes severe damage to the DNA of skin keratinocytes, fibroblasts, and endothelial cells, impairing their regenerative capacity and resulting in endothelial injury and occlusive endarteritis[9]. The challenge of healing skin tissue wounds after radiotherapy presents a significant surgical problem at present[10]. Therefore, routine wound dressing often proves ineffective, making surgical debridement and coverage with a vascular flap grafting appropriate options.
The patient presented with a recurrent NHL-related ulcerated wound on the left lower leg near the ankle, following a long history of radiation therapy. Despite prior treatment with immunotherapy, radiotherapy, and dressing changes at an outside hospital, poor wound healing persisted. Therefore, a treatment plan involving expanded debridement and peroneal artery perforator flap grafting was chosen to address the difficult-to-heal wound. Peroneal artery perforator flaps are commonly utilized for soft tissue defect wounds in specific regions of the lower extremities without causing damage to major blood vessels or nerves and have demonstrated satisfactory outcomes[11]. In this case, due to the recurrence of NHL and prolonged radiotherapy, limb-ulcerated wounds were observed which significantly impacted daily life. Consequently, the patient and family consented to pursue the aforementioned treatment plan. Following active intervention, necrotic tissue was absent after 2 weeks and fresh granulation tissue formed; complete wound healing was achieved after 1 month with a satisfactory therapeutic outcome.
We report a rare case of NHL involving chronic difficult-to-heal wounds of the lower extremities. The patient was successfully treated with radiotherapy combined with surgery, and the postoperative outcome was satisfactory during follow-up observation. We hope that this case will contribute to future treatment options, but more cases are needed to validate its feasibility, safety, and prognosis.
We thank the patient and his family for providing signed informed consent.
| 1. | Martella A, Willett C, Palta M, Czito B. The Selective Use of Radiation Therapy in Rectal Cancer Patients. Curr Oncol Rep. 2018;20:43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Goodlad JR, Cerroni L, Swerdlow SH. Recent advances in cutaneous lymphoma-implications for current and future classifications. Virchows Arch. 2023;482:281-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 22] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 3. | Velasco-Amador JP, Prados-Carmona A, Ruiz-Villaverde R. Radiation dermatitis in a patient treated for hepatocarcinoma. CMAJ. 2023;195:E122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 4. | Shankland KR, Armitage JO, Hancock BW. Non-Hodgkin lymphoma. Lancet. 2012;380:848-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 518] [Cited by in RCA: 486] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 5. | Bowzyk Al-Naeeb A, Ajithkumar T, Behan S, Hodson DJ. Non-Hodgkin lymphoma. BMJ. 2018;362:k3204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 66] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 6. | Sugaya M. Clinical Guidelines and New Molecular Targets for Cutaneous Lymphomas. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Cicone F, Santo G, Bodet-Milin C, Cascini GL, Kraeber-Bodéré F, Stokke C, Kolstad A. Radioimmunotherapy of Non-Hodgkin B-cell Lymphoma: An update. Semin Nucl Med. 2023;53:413-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Lin ZC, Bennett MH, Hawkins GC, Azzopardi CP, Feldmeier J, Smee R, Milross C. Hyperbaric oxygen therapy for late radiation tissue injury. Cochrane Database Syst Rev. 2023;8:CD005005. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Bennett MH, Feldmeier J, Hampson NB, Smee R, Milross C. Hyperbaric oxygen therapy for late radiation tissue injury. Cochrane Database Syst Rev. 2016;4:CD005005. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (1)] |
| 10. | Gieringer M, Gosepath J, Naim R. Radiotherapy and wound healing: principles, management and prospects (review). Oncol Rep. 2011;26:299-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Cheng L, Yang X, Chen T, Li Z. Peroneal artery perforator flap for the treatment of chronic lower extremity wounds. J Orthop Surg Res. 2017;12:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |