Published online Apr 26, 2022. doi: 10.4330/wjc.v14.i4.231
Peer-review started: December 5, 2021
First decision: January 25, 2022
Revised: February 2, 2022
Accepted: April 3, 2022
Article in press: April 3, 2022
Published online: April 26, 2022
Processing time: 134 Days and 5.8 Hours
Acute type A aortic dissection (ATAAD) is a life-threatening disease associated with high morbidity and mortality.
To evaluate the diameter of dissected ascending aorta in patients diagnosed with ATAAD and whether the aortic diameter is associated with preoperative adverse events.
A total of 108 patients diagnosed with ATAAD who underwent emergency operation under hypothermic circulatory arrest were enrolled in this study. Demographic characteristics and perioperative data were recorded. In all patients, preoperative chest and abdomen computed tomography (CT) scans were performed.
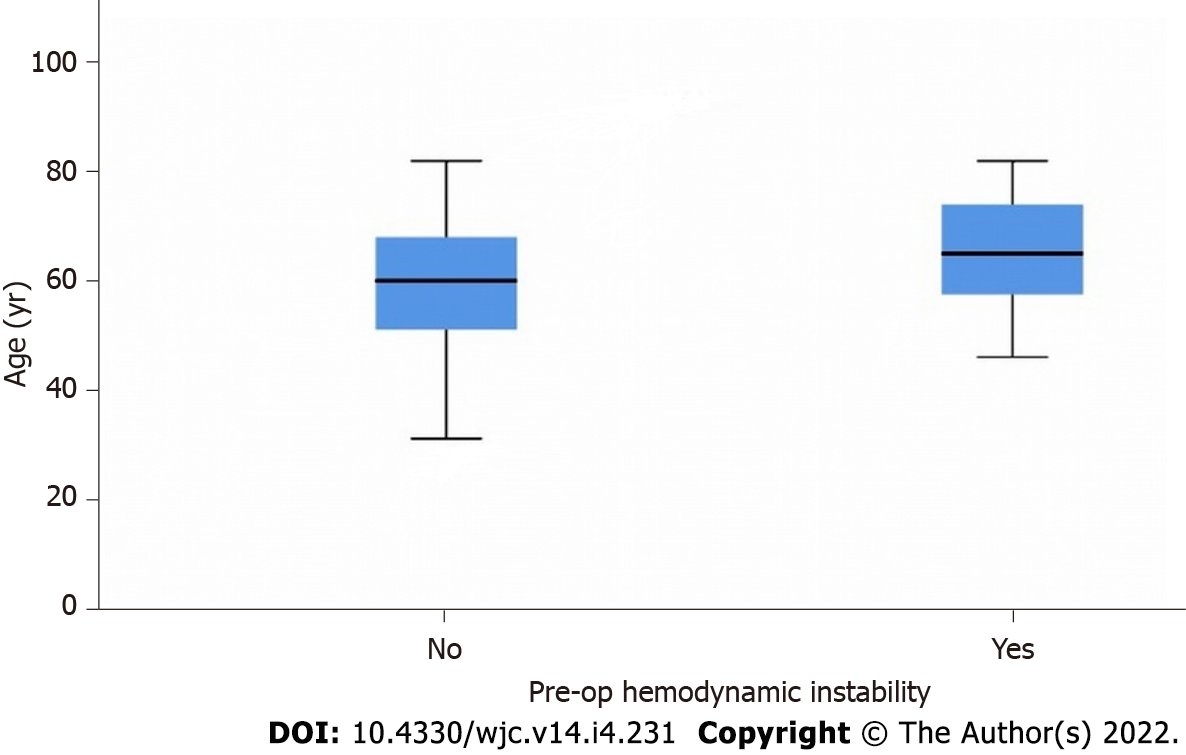
Median age of the patients was 61.5 (52.5-70.5) years and median body mass index (BMI) was 28.2 (25.1-32.6) cm2. The number of female patients was 37 (25%). Median diameter of the ascending aorta was 5.0 (4.5-6) cm and 53.8% of the patients had an aortic diameter < 5.0 cm, while 32.3% of the patients had an aortic diameter of 4.5cm and 72.0% had an ascending aorta diameter < 5.5 cm. The diameter of the ascending aorta did not differ in patients with vs without preoperative adverse events: Preoperative neurological dysfunction (P = 0.53) and hemodynamic instability (P = 0.43). Median age of patients with preoperative hemodynamic instability was 65 (57.5-74) years, while it was 60 (51-68) years in patients without (P = 0.04)
Although current guidelines suggest replacing the ascending aorta with a diameter > 5.5 cm, most of the patients with ATAAD had an aortic diameter of less than 5.5 cm. The diameter of the ascending aorta in patients diagnose with ATAAD is not associated with preoperative adverse events.
Core Tip: Do patients with an ascending aorta diameter < 5.5 cm undergo more aggressive surgery for prevention of acute type A aortic dissection (ATAAD)? Most of the patients (72.0%) with ATAAD had an ascending aorta diameter < 5.5 cm. An international taskforce should adapt the new data extracted from the most recent scientific evidence in the surgical treatment of the ascending aortic aneurysm.
- Citation: Samanidis G, Kanakis M, Georgiou C, Perreas K. Association of dissected ascending aorta diameter with preoperative adverse events in patients with acute type A aortic dissection. World J Cardiol 2022; 14(4): 231-238
- URL: https://www.wjgnet.com/1949-8462/full/v14/i4/231.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i4.231
Acute type A aortic dissection (ATAAD) is a life-threatening condition with excessive mortality and morbidity if not operated, reaching approximately 50% during the first 24 h and 70%-90% days and weeks after diagnosis[1-3]. Emergency surgical correction with replacement of the ascending aorta with or without aortic arch, despite being the treatment of choice, also carries a significant mortality and morbidity burden. Nowadays, emergency surgical correction of ATAAD under hypothermic circulatory arrest remains the treatment of choice[4-6]. On the other hand, the mortality rate of patients who underwent ATAAD repair is high at approximately 15%-25%[7-9].
The most common clinical manifestation of thoracic aorta dissection is acute chest pain. Due to the much commoner incidence of acute coronary syndrome (ACS), pulmonary embolism (PE), and other thoracic pathology, accurate diagnosis is frequently hindered or delayed. The sudden and insidious onset of symptoms, the delay in diagnosis, and the time required to transport of patients to cardiac surgery centers for treatment negatively affect the outcomes of these patients[10-12]. Replacement of the ascending aorta in patients with an enlarged aortic diameter is considered as an option for preventing acute aortic dissection. Existing and current guidelines recommend replacing the ascending aorta if the size reaches 5.5 cm in patients without Marfan syndrome[6,13]. On the other hand, the exact threshold of aortic size (< 5.5 cm) for early (preventive) operation remains a grey zone in current indications and guidelines, because in most patients with acute aortic dissection, the maximum aortic diameter is approximately 5 cm or less[14-17].
The present study evaluated the diameter of dissected ascending aorta in patients diagnosed with ATAAD and whether the aortic diameter is associated with preoperative adverse events.
The study period was 2010-2017. This retrospective study included 108 patients with ATAAD who underwent an emergency operation under hypothermic circulatory arrest with antegrade or retrograde cerebral perfusion. Patients with a known diagnosis of connective tissue disorder or Marfan syndrome or iatrogenic dissection were excluded. All demographic characteristics and perioperative data were recorded. In all patients, preoperative chest and abdomen computed tomography (CT) scans were performed. The ascending aorta diameter was calculated based on preoperative chest CT or CT angiography. The maximum diameter of the ascending aorta was defined as the diameter which included the true and false lumen of the ascending aorta. The method for measuring the maximum aortic diameter was double oblique short axis. All preoperative neurological dysfunctions (including temporary and permanent neurological dysfunctions) on admission were included in our database. Temporary neurological dysfunctions (TND) were defined if the patients had transient ischemic attack (TIA) or delirium or disorientation, while permanent neurological dysfunctions (PND) if the patients were admitted to hospital with hemiplegia or paraplegia or coma. Preoperative hemodynamic instability was defined as preoperative cardiac arrest or systolic blood pressure (< 80 mmHg) despite inotropic support or preoperatively diagnosed cardiac tamponade with hemodynamic consequences. The study was approved by the hospital’s institutional review board (546/30-04-2015).
Continuous variables are presented as the median (interquartile range), while categorical variables are presented as n (%). Normality of continuous variables was examined by Shapiro-Wilk test and Q-Q plot. Continuous variables were compared by Student’s t-test for the normally distributed, while Mann-Whitney and Kruskal-Wallis tests for the non-normally distributed variables. Chi-square or Fisher’s exact test was implemented for the rest variables (categorical variables). Correlation of ascending aorta diameter with continuous variables was evaluated by Spearman (rs) or Pearson (r) correlation coefficient. Univariable linear regression model was used to identify the association of demographics and other factors with diameter of the ascending aorta. The effect size was expressed by linear regression coefficient ‘’β’’. Binary univariable and multivariable logistic regression modeling was used to estimate the association of ascending aorta diameter with preoperative adverse events (neurological dysfunction and hemodynamic instability). Predictive ability is presented as odds ratio (OR). The Hosmer-Lemeshow goodness of fit test was performed for logistic regression analysis model. Confidence interval (CI) was set at 95% in all tests. Statistical significance was considered at P < 0.05. IBM SPSS Statistics for Windows, version 25 (IBM Corp., Armonk, NY, United States) was used in analysis.
Median age of the patients was 61.5 (52.5-70.5) years and median body mass index (BMI) was 28.2 (25.1-32.6) cm2. Thirty-seven (25%) were female patients. Median diameter of the ascending aorta was 5.0 (4.5-6) cm and 53.8% of patients had an aortic diameter < 5.0 cm, while 32.3% of the patients had an aortic diameter of 4.5 cm. In addition, 72.0% of the patients had an ascending aorta diameter < 5.5 cm. Coexisting aortic regurgitation was recorded in 26.8% of the patients, while history of hypertension was observed in 86.1%. Other demographic characteristics and preoperative details are listed in Table 1.
| Variable | Total number of patients (N = 108) |
| Age, yr, median (IQR) | 61.5 (52.5-70.5) |
| Body mass index, cm2, median (IQR) | 28.2 (25.1-32.6) |
| Female, n (%) | 37 (25) |
| History of hypertension, n (%) | 93 (86.1) |
| History of smoking, n (%) | 65 (60.2) |
| Aortic regurgitation, n (%) | 29 (26.8) |
| Left ventricle ejection fraction, %, median (IQR) | 45 (40-50) |
| Diabetes mellitus, n (%) | 11 (10.2) |
| Preoperative neurological dysfunction, n (%) | 22 (16.1) |
| Temporary neurological dysfunction | 14 (13.0) |
| Permanent neurological dysfunction | 3 (2.7) |
| Preoperative hemodynamic instability, n (%) | 35 (32.4) |
| Maximum diameter of ascending aorta, cm, median (IQR) | 5.0 (4.5-6) |
| NT-proBNP, pg/mL, median (IQR) | 377.5 (180-928) |
| D-Dimers, µg/L, median (IQR) | 5256.5 (2477-10000) |
We tested the correlation of aortic diameter with age, BMI, LVEF, D-dimer, and NT-proBNP. No correlation was detected between aortic diameter and age (r = 0.13, P = 0.20), BMI (r = 0.05, P = 0.67), LVEF (r = 0.08, P = 0.47), D-dimer (rs = -0.14, P = 0.31), or NT-proBNP (rs = 0.19, P = 0.14). No difference in ascending aorta diameters was observed between males vs females (P = 0.83), as well as between patients with vs without history of hypertension (P = 0.87) and smoking vs no smoking (P = 0.90). The BMI did not predict the diameter of the ascending aorta [β = 0.01, 95%CI: -0.05 to 0.08, P = 0.68]. Preoperative plasma creatinine was not associated with the diameter of the ascending aorta (β = 0.09, 95%CI: -0.19-0.36, P = 0.53).
The diameter of the ascending aorta did not differ in patients with vs without preoperative adverse events: Preoperative neurological dysfunction (P = 0.53) and hemodynamic instability (P = 0.43). In addition, univariable logistic regression analysis showed that aortic diameter did not predict the preoperative hemodynamic instability (OR = 1.2, 95%CI: 0.87-1.60, P = 0.29) or preoperative neurological dysfunction (OR = 1.0, 95%CI: 0.72-1.51, P = 0.81). Multivariable logistic regression analysis (adjusted for age, gender, and BMI) showed that aortic diameter did not predict preoperative neurological dysfunction (OR = 1.1, 95%CI: 0.68-1.74, P = 0.70) (Table 2). Furthermore, multivariable logistic regression analysis (adjusted for age, gender, BMI, and aortic diameter) revealed that only age predicted the preoperative hemodynamic instability (OR = 1.05, 95%CI: 1.01-1.11, P = 0.02), while diameter of the aorta did not (OR=1.1, 95%CI: 0.68-1.57, P = 0.86) (Table 3). Median age of the patients with preoperative hemodynamic instability was 65 (57.5-74) years, while it was 60 (51-68) years in those without (P = 0.04) (Figure 1). In conclusion, our analysis showed that no difference in dissected ascending aorta diameter was observed between patients who died in hospital vs who did not (P = 0.75). In addition, the diameter of dissected ascending aorta was not correlated with postoperative ICU or hospital stay (rs = -0.08, P = 0.45 and rs = -0.02, P = 0.85, respectively).
| Variable | P value | OR | 95%CI |
| Age | 0.28 | 1.1 | 0.97-1.09 |
| Gender | 0.46 | 1.7 | 0.38-8.12 |
| Body mass index | 0.42 | 1.1 | 0.92-1.19 |
| Diameter of ascending aorta | 0.70 | 1.1 | 0.68-1.74 |
Currently, American and European guidelines are in agreement regarding the main criterion for elective surgical aneurysm resection in the thoracic aorta: The size of the aortic diameter[6,13]. For non-syndromic, asymptomatic aortic aneurysmal disease, the indicative diameter threshold for elective replacement of the ascending aorta is 5.5 cm. However, these guidelines are relying on post-dissection diameter measurements, which are much larger than diameter size prior to dissection[6,13].
There is evidence to suggest that the size of the aorta significantly increases post-dissection[18]. Mansour et al[18] from the Aortic Institute at Yale-New Haven Hospital demonstrated that the mean aortic diameter at ATAAD was 54.2 mm, whereas the mean aortic diameter prior to dissection was only 45.1 mm[18]. Wu et al[19] described an 18% increase in aortic diameter after an ATAAD. Therefore, the pre-dissection aortic diameter falls in several studies well below the current threshold for elective surgical replacement of the ascending aorta. Saade et al[20] introduced the term aortic size index in order to stratify patients into risk groups. It was calculated by dividing the aortic diameter by the body surface area. However, 10 years later, researchers from the same institution argued against that theory and concluded that body surface area should not be taken into consideration[21]. The same researchers focused on the importance of aortic height index, which is calculated by dividing the aortic diameter by the patient’s height. An increased index is associated with an increased annual risk of aortic aneurysm complications[21]. Eliathamby et al[22] concluded that the aortic length (distance between the aortic valve and the innominate artery) was strongly correlated with the diameter of the ascending aorta. Wu et al[19] suggested the length-height index, which is calculated by dividing the aortic length by the patient’s height. An index > 7.5 cm/m was found to have an annual fivefold increased risk of aortic adverse events compared with patients with an index < 5.5 cm/m. However, genetic susceptibility should always be taken into account as it plays an important role in identifying high risk patients[19,23].
ATAAD continues to carry a high peri-operative mortality risk with rates reaching as high as 25%[23,24]. Many authors highlight the safety of preventive surgical replacement of the ascending aorta as published data on elective replacement of the ascending aorta is associated with mortality rates less than 3%[23,24]. For elective operations, postoperative stroke rates are also low with no more than 1.0% strokes noted when the operation takes place in a large volume aortic centre[25]. Moreover, emergency surgical operations show a 5-year survival rate of 37%, rather poorer than the rate (> 85%) related to elective surgical repair of the ascending aorta[25].
Although current guidelines suggest replacing the ascending aorta with a diameter ≥ 5.5 cm, many of the patients with ATAAD have an aortic diameter of less than 5.5 cm. The diameter of the ascending aorta in patients diagnosed with ATAAD is not associated with preoperative adverse events. An international taskforce should adapt the new data extracted from the most recent scientific evidence for the surgical treatment of the ascending aortic aneurysm.
Acute type A aortic dissection (ATAAD) is a life-threatening cardiovascular disease. Current guidelines recommend that ascending aortic replacement be performed when the ascending aorta is 5.5 cm in non-syndromic patients, while in syndormic patients, it should be replaced if the diameter reaches 4.5 cm in the sinus of Valsalva and 5.0 cm in the ascending aorta.
New approach for ascending aorta aneurysm management should be considered for prevention of ATAAD.
The objective of our study was to evaluate the correlation of the diameter of dissected ascending aorta in patients with ATAAD with preoperative adverse events, such as neurological dysfunctions and hemodynamic instability.
A retrospective analysis was performed on patients who were admitted to our hospital for ATAAD treatment. In all patients, the diameter of dissected ascending aorta was measured and its association with adverse events was analyzed.
The diameter of dissected ascending aorta was not associated with adverse events. Also, the diameter of the ascending aorta was not associated with 30-d mortality and ICU and hospital stay postoperatively.
Maybe the threshold of ascending aorta aneurysm should be revised for lower limits regarding the risk for late acute dissection
Randomized controlled studies including more patients should be performed to confirm our results and preventive ascending aorta replacement may be considered for prevention of ATAAD.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gluvic Z, Serbia; Peng D, China S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Khan H, Hussain A, Chaubey S, Sameh M, Salter I, Deshpande R, Baghai M, Wendler O. Acute aortic dissection type A: Impact of aortic specialists on short and long term outcomes. J Card Surg. 2021;36:952-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Luehr M, Merkle-Storms J, Gerfer S, Li Y, Krasivskyi I, Vehrenberg J, Rahmanian P, Kuhn-Régnier F, Mader N, Wahlers T. Evaluation of the GERAADA score for prediction of 30-day mortality in patients with acute type A aortic dissection. Eur J Cardiothorac Surg. 2021;59:1109-1114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Helgason D, Helgadottir S, Ahlsson A, Gunn J, Hjortdal V, Hansson EC, Jeppsson A, Mennander A, Nozohoor S, Zindovic I, Olsson C, Ragnarsson SO, Sigurdsson MI, Geirsson A, Gudbjartsson T. Acute Kidney Injury After Acute Repair of Type A Aortic Dissection. Ann Thorac Surg. 2021;111:1292-1298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 4. | Pupovac SS, Hemli JM, Bavaria JE, Patel HJ, Trimarchi S, Pacini D, Bekeredjian R, Chen EP, Myrmel T, Ouzounian M, Fanola C, Korach A, Montgomery DG, Eagle KA, Brinster DR. Moderate Versus Deep Hypothermia in Type A Acute Aortic Dissection Repair: Insights from the International Registry of Acute Aortic Dissection. Ann Thorac Surg. 2021;112:1893-1899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Li L, Zhou J, Hao X, Zhang W, Yu D, Xie Y, Gu J, Zhu T. The Incidence, Risk Factors and In-Hospital Mortality of Acute Kidney Injury in Patients After Surgery for Acute Type A Aortic Dissection: A Single-Center Retrospective Analysis of 335 Patients. Front Med (Lausanne). 2020;7:557044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ; ESC Committee for Practice Guidelines. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014;35:2873-2926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2374] [Cited by in RCA: 3103] [Article Influence: 282.1] [Reference Citation Analysis (0)] |
| 7. | Rylski B, Hoffmann I, Beyersdorf F, Suedkamp M, Siepe M, Nitsch B, Blettner M, Borger MA, Weigang E; Multicenter Prospective Observational Study. Acute aortic dissection type A: age-related management and outcomes reported in the German Registry for Acute Aortic Dissection Type A (GERAADA) of over 2000 patients. Ann Surg. 2014;259:598-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 121] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 8. | Jassar AS, Sundt TM 3rd. How should we manage type A aortic dissection? Gen Thorac Cardiovasc Surg. 2019;67:137-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Gudbjartsson T, Ahlsson A, Geirsson A, Gunn J, Hjortdal V, Jeppsson A, Mennander A, Zindovic I, Olsson C. Acute type A aortic dissection - a review. Scand Cardiovasc J. 2020;54:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 77] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 10. | Matthews CR, Madison M, Timsina LR, Namburi N, Faiza Z, Lee LS. Impact of time between diagnosis to treatment in Acute Type A Aortic Dissection. Sci Rep. 2021;11:3519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Pan E, Wallinder A, Peterström E, Geirsson A, Olsson C, Ahlsson A, Fuglsang S, Gunn J, Hansson EC, Hjortdal V, Mennander A, Nozohoor S, Wickbom A, Zindovic I, Gudbjartsson T, Jeppsson A. Outcome after type A aortic dissection repair in patients with preoperative cardiac arrest. Resuscitation. 2019;144:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Teman NR, Peterson MD, Russo MJ, Ehrlich MP, Myrmel T, Upchurch GR Jr, Greason K, Fillinger M, Forteza A, Deeb GM, Montgomery DG, Eagle KA, Isselbacher EM, Nienaber CA, Patel HJ. Outcomes of patients presenting with acute type A aortic dissection in the setting of prior cardiac surgery: an analysis from the International Registry of Acute Aortic Dissection. Circulation. 2013;128:S180-S185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, Eagle KA, Hermann LK, Isselbacher EM, Kazerooni EA, Kouchoukos NT, Lytle BW, Milewicz DM, Reich DL, Sen S, Shinn JA, Svensson LG, Williams DM; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology,American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons,and Society for Vascular Medicine. J Am Coll Cardiol. 2010;55:e27-e129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 945] [Cited by in RCA: 1034] [Article Influence: 68.9] [Reference Citation Analysis (0)] |
| 14. | Heuts S, Adriaans BP, Rylski B, Mihl C, Bekkers SCAM, Olsthoorn JR, Natour E, Bouman H, Berezowski M, Kosiorowska K, Crijns HJGM, Maessen JG, Wildberger J, Schalla S, Sardari Nia P. Evaluating the diagnostic accuracy of maximal aortic diameter, length and volume for prediction of aortic dissection. Heart. 2020;106:892-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 15. | Yamauchi T, Takano H, Takahashi T, Masai T, Sakaki M, Shirakawa Y, Kitabayashi K, Asano N, Toda K, Sawa Y; Osaka Cardiovascular Surgery Research Group (OSCAR). Equations Estimating the Predissected Diameter of the Ascending Aorta for Acute Type A Aortic Dissection. Ann Thorac Surg. 2019;108:481-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Wang D, Wang ZY, Wang JF, Zhang LL, Zhu JM, Yuan ZX, Wang Y. Values of aortic dissection detection risk score combined with ascending aorta diameter >40 mm for the early identification of type A acute aortic dissection. J Thorac Dis. 2018;10:1815-1824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Tozzi P, Gunga Z, Niclauss L, Delay D, Roumy A, Pfister R, Colombier S, Patella F, Qanadli SD, Kirsch M. Type A aortic dissection in aneurysms having modelled pre-dissection maximum diameter below 45 mm: should we implement current guidelines to improve the survival benefit of prophylactic surgery? Eur J Cardiothorac Surg. 2021;59:473-478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Mansour AM, Peterss S, Zafar MA, Rizzo JA, Fang H, Charilaou P, Ziganshin BA, Darr UM, Elefteriades JA. Prevention of Aortic Dissection Suggests a Diameter Shift to a Lower Aortic Size Threshold for Intervention. Cardiology. 2018;139:139-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 19. | Wu J, Zafar MA, Li Y, Saeyeldin A, Huang Y, Zhao R, Qiu J, Tanweer M, Abdelbaky M, Gryaznov A, Buntin J, Ziganshin BA, Mukherjee SK, Rizzo JA, Yu C, Elefteriades JA. Ascending Aortic Length and Risk of Aortic Adverse Events: The Neglected Dimension. J Am Coll Cardiol. 2019;74:1883-1894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 104] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 20. | Saade W, Vinciguerra M, Romiti S, Macrina F, Frati G, Miraldi F, Greco E. 3D morphometric analysis of ascending aorta as an adjunctive tool to predict type A acute aortic dissection. J Thorac Dis. 2021;13:3443-3457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Zafar MA, Li Y, Rizzo JA, Charilaou P, Saeyeldin A, Velasquez CA, Mansour AM, Bin Mahmood SU, Ma WG, Brownstein AJ, Tranquilli M, Dumfarth J, Theodoropoulos P, Thombre K, Tanweer M, Erben Y, Peterss S, Ziganshin BA, Elefteriades JA. Height alone, rather than body surface area, suffices for risk estimation in ascending aortic aneurysm. J Thorac Cardiovasc Surg. 2018;155:1938-1950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 184] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 22. | Eliathamby D, Gutierrez M, Liu A, Ouzounian M, Forbes TL, Tan KT, Chung J. Ascending Aortic Length and Its Association With Type A Aortic Dissection. J Am Heart Assoc. 2021;10:e020140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 23. | Rylski B, Branchetti E, Bavaria JE, Vallabhajosyula P, Szeto WY, Milewski RK, Desai ND. Modeling of predissection aortic size in acute type A dissection: More than 90% fail to meet the guidelines for elective ascending replacement. J Thorac Cardiovasc Surg. 2014;148:944-8.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 24. | Ziganshin BA, Zafar MA, Elefteriades JA. Descending threshold for ascending aortic aneurysmectomy: Is it time for a "left-shift" in guidelines? J Thorac Cardiovasc Surg. 2019;157:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 25. | Kuzmik GA, Sang AX, Elefteriades JA. Natural history of thoracic aortic aneurysms. J Vasc Surg. 2012;56:565-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 211] [Article Influence: 16.2] [Reference Citation Analysis (0)] |