Published online Feb 27, 2024. doi: 10.4240/wjgs.v16.i2.491
Peer-review started: November 21, 2023
First decision: December 12, 2023
Revised: December 23, 2023
Accepted: January 12, 2024
Article in press: January 12, 2024
Published online: February 27, 2024
Processing time: 96 Days and 1.8 Hours
Transjugular intrahepatic portosystemic shunt (TIPS) placement is a procedure that can effectively treat complications of portal hypertension, such as variceal bleeding and refractory ascites. However, there have been no specific studies on predicting long-term survival after TIPS placement.
To establish a model to predict long-term survival in patients with hepatitis cirrhosis after TIPS.
A retrospective analysis was conducted on a cohort of 224 patients who un
The indication (variceal bleeding or ascites), shunt reasonability (reasonable or unreasonable), ICGR15, post
The NDC model can accurately predict long-term survival after the TIPS procedure in patients with hepatitis cirrhosis, help identify high-risk patients and guide follow-up management after TIPS implantation.
Core Tip: The core finding of this article is that a newly developed Cox regression model (NDC) outperforms the existing scoring models, such as the Child-Pugh, model for end-stage liver disease (MELD), MELD-sodium and the Freiburg index of post-transjugular intrahepatic portosystemic shunt (TIPS) survival, in predicting long-term survival after TIPS placement in patients with hepatitis cirrhosis. In the NDC model, considered factors such as indication for TIPS, shunt reasonability, indocyanine green retention rate at 15 min, post-portal venous pressure gradient, percentage decrease in portal venous pressure, and total bilirubin are considered. It provided a more accurate prediction of 6-year survival, allowing for the identification of high-risk patients who may need closer follow-up after the procedure.
- Citation: Lv YF, Zhu B, Meng MM, Wu YF, Dong CB, Zhang Y, Liu BW, You SL, Lv S, Yang YP, Liu FQ. Development of a new Cox model for predicting long-term survival in hepatitis cirrhosis patients underwent transjugular intrahepatic portosystemic shunts. World J Gastrointest Surg 2024; 16(2): 491-502
- URL: https://www.wjgnet.com/1948-9366/full/v16/i2/491.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i2.491
The techniques for and practical experience with transjugular intrahepatic portosystemic shunt (TIPS) placement have significantly evolved over the past three decades[1,2]. These advancements have led to the recommendation of these gui
Several scoring models have been used in clinical practice to assess the prognosis of patients who underwent TIPS implantation. The most widely used tool is the model for end-stage liver disease (MELD), which mainly predicts 3-month mortality among patients with cirrhosis[7,8] and is more accurate than the traditional Child-Pugh score in assessing the severity of liver disease[9]. The MELD score was subsequently modified by incorporating the serum sodium level, re
Patients aged 18-80 years with hepatitis cirrhosis who underwent elective TIPS implantation for the management of refractory ascites and variceal bleeding were retrospectively recruited from January 2013 to January 2017 at Beijing Shijitan Hospital. Eighteen patients with hepatocellular carcinoma, 26 patients with missing clinical data, 9 patients with severe cardiorenal disease, 36 patients who were lost to follow-up within a year, and 7 patients who underwent TIPS revision procedures were excluded. In brief, the final dataset consisted of 224 patients who were randomly divided into a training set (n = 157) and a validation set (n = 67) at a 7:3 ratio (Figure 1). The diagnosis of hepatitis cirrhosis and portal hypertension was established through the utilization of imaging and endoscopic studies, clinical observations, and la
All clinical and laboratory characteristics that were assessed within 72 h prior to the TIPS procedure were collected by 2 physicians from the medical records. The collection of follow-up data was conducted through telephone interviews and outpatient visits, with the follow-up endpoints being death, liver transplantation, or study closure (January, 2023). Sur
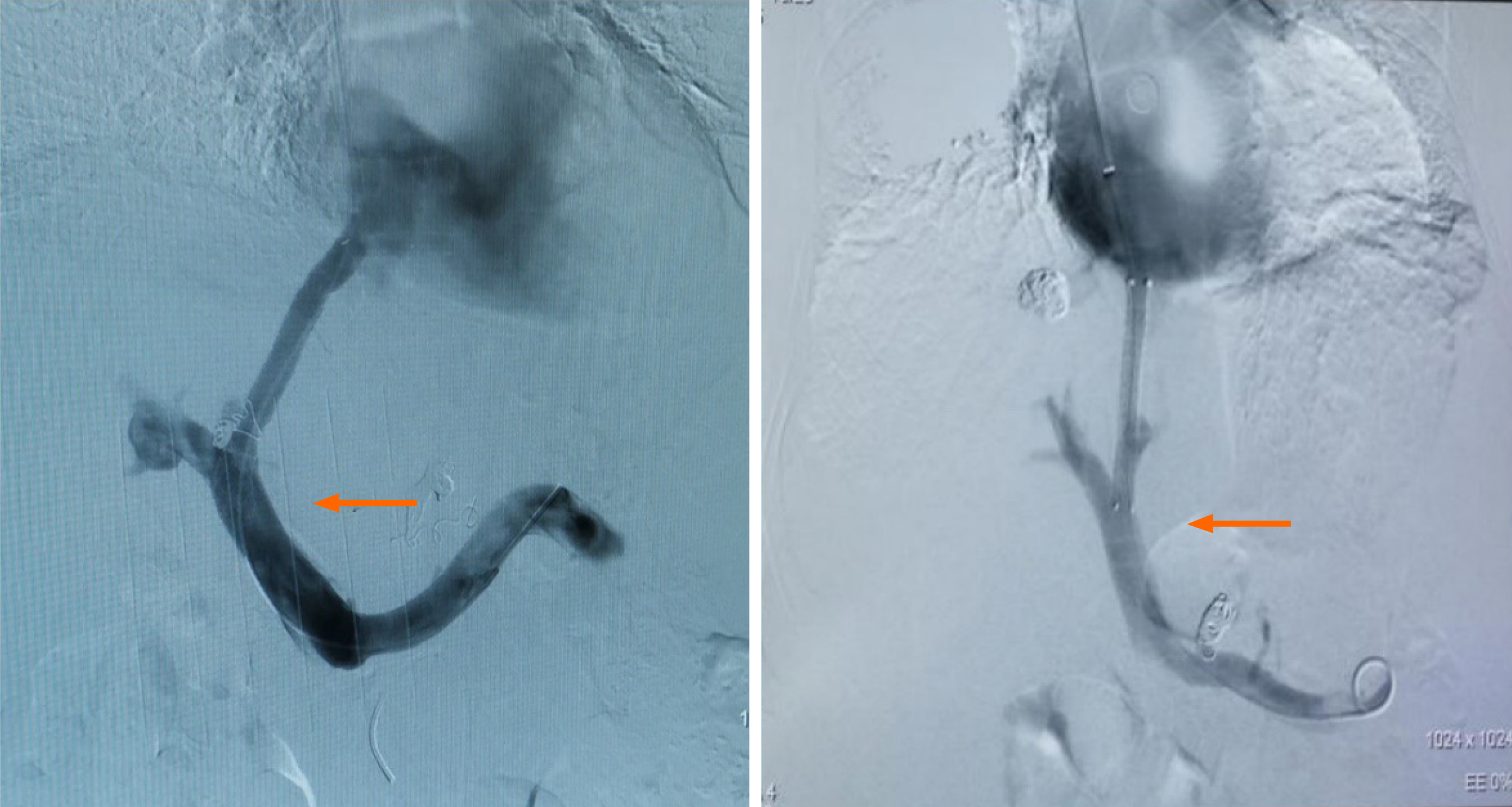
TIPS implantation mainly involves creating a shunt between the portal vein and the hepatic vein to reduce pressure in the portal system[16]. The procedure is conducted by a radiologist who utilizes fluoroscopic guidance to insert a catheter through the jugular vein into the hepatic vein. Following this, hepatic venography was performed to ascertain the exact location and anatomical features of the hepatic vein and inferior vena cava (IVC) junction. Subsequently, the portal vein was punctured, portal venography was conducted, the parenchymal tract was dilated, and a reasonable shunt was esta
Remarkably, there is no universally accepted criterion for shunt reasonability, which is related to various factors, such as the shunt channel diameter[17] and the spatial relationship between the stent and the blood vessels. In terms of safety, the core factors considered are short-, medium- and long-term efficacy and quality of life. Thus, a reasonable shunt should result in a 30%-50% decrease in portal venous pressure (PVP) or a decreased PPG of 6-12 mmHg[18]. Addi
This retrospective study was conducted to determine the predictive value of an alternative score for 6-year survival in patients after TIPS implantation for refractory ascites or/and secondary prophylaxis for variceal bleeding. SPSS (version 27.0, IBM Corp., Armonk, New York) and R (version 4.3.1, R development Core Team) were used for the statistical analyses. SPSS is primarily used for basic statistical tests, such as between-group comparisons of qualitative or quan
A total of 320 patients who underwent TIPS placement were included in this study. Based on the given inclusion and exclusion criteria, 224 patients were eventually included. Table 1 describes the basic and clinical characteristics of the patients. The main etiology was hepatitis cirrhosis, and the indications for TIPS implantation were refractory ascites (training: 21% vs validation: 24%), secondary prophylaxis for variceal bleeding (training: 57% vs validation: 55%) and both (22% vs 21%). The survival rates were similar in the training and validation cohorts (49.9% vs 39.1%, P = 0.233).
| Training cohort (n = 157) | Validation cohort (n = 67) | P value | |
| Age (yr) | 51.9 ± 11.4 | 54.8 ± 9.0 | 0.05 |
| Sex, n (%) | 0.714 | ||
| Male | 123 (78) | 51 (76) | |
| Female | 34 (22) | 16 (24) | |
| Etiology of cirrhosis, n (%) | 0.251 | ||
| Hepatitis B | 137 (87) | 62 (92) | |
| Hepatitis C | 20 (13) | 5 (8) | |
| Indication, n (%) | 0.935 | ||
| Variceal bleeding | 89 (57) | 37 (55) | |
| Ascites | 34 (21) | 16 (24) | |
| Both | 34 (22) | 14 (21) | |
| Shunt, n (%) | 0.118 | ||
| Reasonable | 83 (53) | 43 (64) | |
| Unreasonable | 74 (47) | 24 (36) | |
| HE before TIPS, n (%) | 0.015 | ||
| Grade 0 | 155 (99) | 62 (92) | |
| Grade 1-2 | 1 (0.5) | 1 (2) | |
| Grade 3-4 | 1 (0.5) | 4 (6) | |
| Ascites, n (%) | 0.199 | ||
| None | 70 (45) | 26 (39) | |
| Mild | 30 (19) | 9 (13) | |
| Severe | 57 (36) | 32 (48) | |
| Pre-PPG (mmHg) | 26.1 ± 6.0 | 27.4 ± 7.7 | 0.153 |
| Post-PPG (mmHg) | 13.4 ± 5.8 | 14.2 ± 6.2 | 0.530 |
| PVP% | 32.2 ± 13.5 | 32.6 ± 12.1 | 0.587 |
| Laboratory values | |||
| ALT (U/L) | 26.2 ± 25.3 | 23.7 ± 12.0 | 0.686 |
| AST (U/L) | 35.4 ± 32.6 | 31.8 ± 13.5 | 0.596 |
| ALB (g/L) | 36.1 ± 4.6 | 35.7 ± 4.6 | 0.736 |
| Na (mmol/L) | 139.5 ± 4.2 | 138.1 ± 4.5 | 0.014 |
| ICGR15 (%) | 39.7 ± 16.1 | 43.0 ± 17.7 | 0.150 |
| INR | 1.3 ± 0.2 | 1.3 ± 0.2 | 0.514 |
| Cr (mol/L) | 70.3 ± 24.0 | 76.6 ± 33.9 | 0.362 |
| Tbil (mol/L) | 26.3 ± 14.9 | 28.3 ± 16.6 | 0.440 |
| WBC (× 109/L) | 3.3 ± 2.4 | 3.5 ± 2.7 | 0.942 |
| PLT (× 109/L) | 95.4 ± 25.0 | 98.9 ± 25.9 | 0.231 |
| HGB (g/L) | 100.1 ± 89.8 | 98.3 ± 82.7 | 0.984 |
| Child-Pugh | 6.9 ± 1.5 | 7.2 ± 1.7 | 0.152 |
| Child classification, n (%) | 0.142 | ||
| Child A | 68 (43) | 22 (33) | |
| Child B | 82 (52) | 41 (61) | |
| Child C | 7 (5) | 4 (6) | |
| MELD | 8.0 ± 4.3 | 9.0 ± 5.1 | 0.295 |
| MELD-Na | 9.0 ± 5.7 | 11.2 ± 6.6 | 0.032 |
| FIPS | -1.0 ± 0.8 | -0.8 ± 0.8 | 0.111 |
| 6-yr survival (%) | 49.9% | 39.1% | 0.233 |
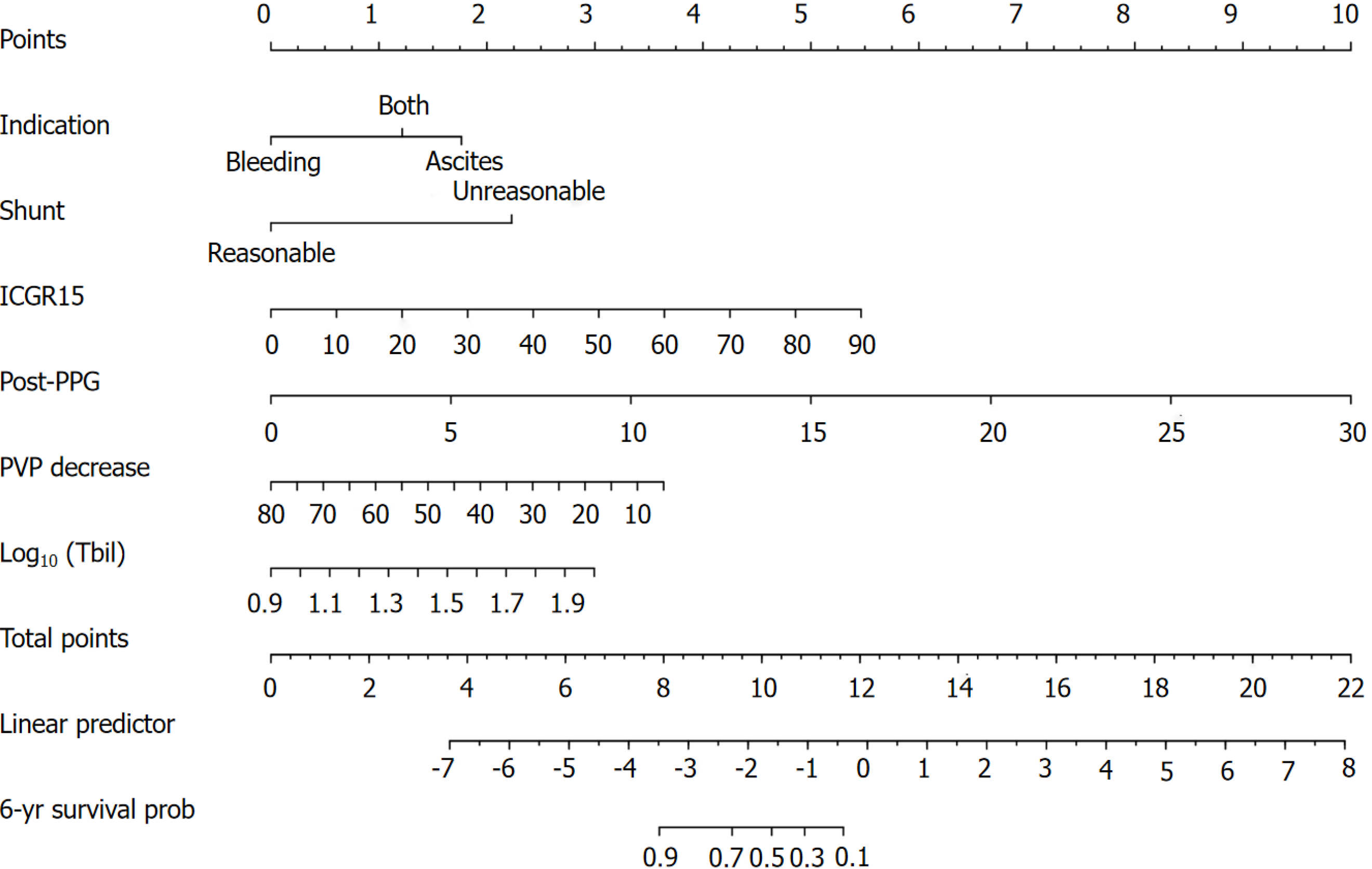
First, univariate Cox proportional hazards regression analysis was carried out to select potentially important prognostic factors (P < 0.05) for multivariate Cox regression analysis (Table 2). The Akaike information criterion (AIC) was applied in a backward stepwise regression to select the best model, with smaller AICs indicating better results. To avoid multicollinearity, the Child-Pugh, MELD, MELD-Na, and FIPS scores were not included in the model, and preoperative HE was not analyzed in the model because most of the included patients did not have HE. The results of the multivariate analysis showed that the indication (variceal bleeding or ascites), shunt reasonability (reasonable or unreasonable), indocyanine green retention rate at 15 min (ICGR15), preoperative and postoperative portal venous pressure gradient (pre-PPG and post-PPG), percentage of PVP decrease (PVP%) and Tbil were found to be independent factors affecting survival after TIPS placement. The pre-PPG was not included in the final model because the overall C statistic of the model decreased by 0.45% (P = 0.17), and there was a correlation between the pre-PPG and post-PPG (Spearman correlation coefficient 0.62, P < 0.05). Using the regression coefficients (Table 2), the linear predictor was calculated as follows: Linear predictor = 1.45 × indication (0-variceal bleeding, 1-ascites) or 1 × indication (0-variceal bleeding, 1-both) + 1.83 × shunt reasonability (0-unreasonable, 1-reasonable) + 0.05 × ICGR15 + 0.27 × post-PPG + (-0.04) × PVP% + 2.24 × Log10 (Tbil). Finally, the newly developed Cox (NDC) model was developed in the form of a nomogram (Figure 3).
| Univariable model | Multivariable model | |||||||
| HR | 95%CI | P value | HR | 95%CI | P value | |||
| Etiology | 0.29 | 1.34 | 0.60-2.98 | 0.48 | ||||
| Indication | ||||||||
| Variceal bleeding | ||||||||
| Ascites | 1.36 | 3.90 | 2.01-7.58 | < 0.001 | 1.45 | 4.27 | 2.04-8.94 | < 0.001b |
| Both | 1.01 | 2.76 | 1.34-5.65 | 0.006 | 1.00 | 2.72 | 1.24-5.97 | 0.01b |
| Shunt | 1.20 | 3.33 | 1.87-5.94 | < 0.001 | 1.83 | 6.26 | 2.67-14.63 | < 0.001b |
| Age | -0.02 | 0.99 | 0.96-1.01 | 0.18 | ||||
| Pre-PPG | 0.10 | 1.10 | 1.05-1.15 | < 0.001 | ||||
| Post-PPG | 0.25 | 1.29 | 1.21-1.37 | < 0.001 | 0.27 | 1.32 | 1.22-1.42 | < 0.001b |
| PVP decrease | -0.09 | 0.92 | 0.89-0.94 | < 0.001 | -0.04 | 0.96 | 0.93-1.00 | 0.03a |
| ALT | -0.001 | 1.00 | 0.99-1.01 | 0.81 | ||||
| AST | 0.0008 | 1.00 | 0.99-1.01 | 0.83 | ||||
| ALB | -0.004 | 1.00 | 0.94-1.06 | 0.88 | ||||
| Na | -0.05 | 0.95 | 0.89-1.02 | 0.13 | ||||
| ICGR15 | 0.04 | 1.04 | 1.03-1.06 | < 0.001 | 0.05 | 1.05 | 1.03-1.07 | < 0.001b |
| 1/INR | -2.99 | 0.05 | 0.003-0.77 | 0.03 | ||||
| Log10 (Cr) | 0.46 | 1.58 | 0.20-12.50 | 0.67 | ||||
| Log10 (Tbil) | 2.95 | 19.16 | 4.87-75.41 | < 0.001 | 2.24 | 9.38 | 2.16-40.82 | 0.002b |
| Log10 (WBC) | -0.43 | 0.65 | 0.21-1.99 | 0.45 | ||||
| Log10 (PLT) | -1.17 | 0.31 | 0.12-0.78 | 0.01 | ||||
| Log10 (HGB) | 1.94 | 6.98 | 0.52-92.97 | 0.14 | ||||
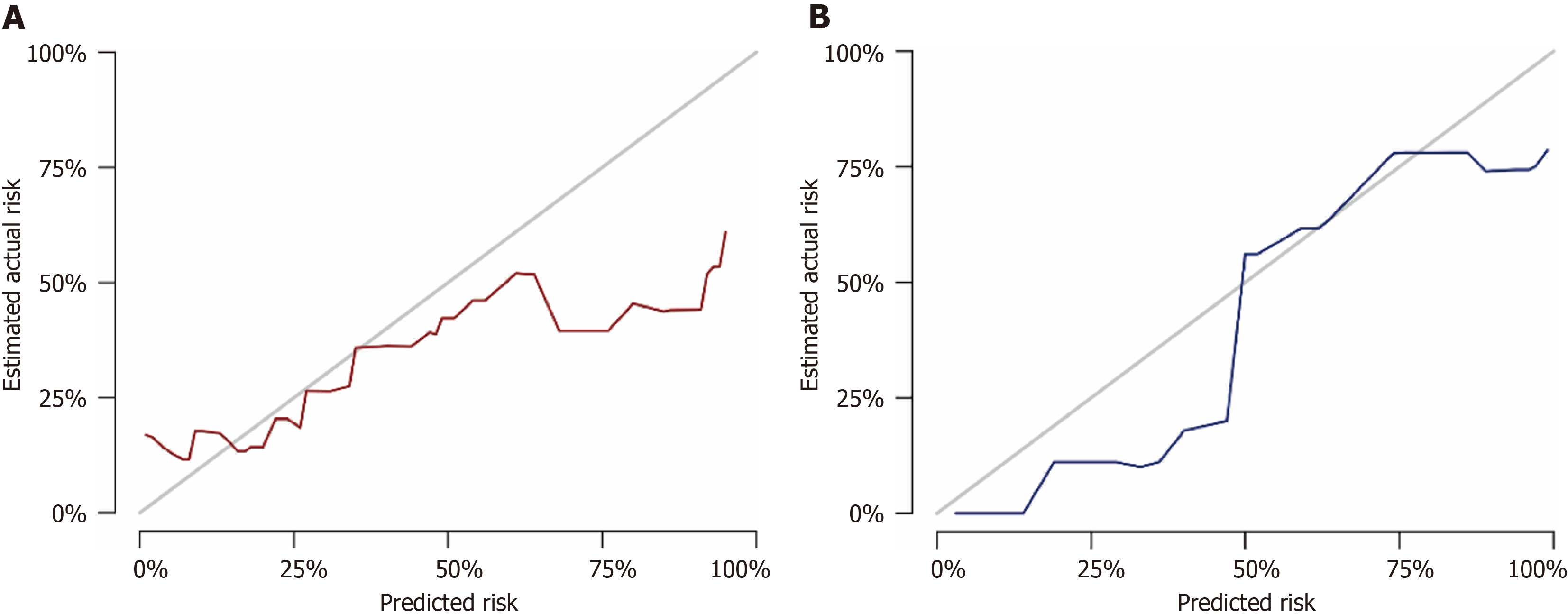
The discrimination of the NDC score was assessed by calculating the AUCs for predicting 6-year survival compared to the Child-Pugh, MELD, MELD-Na, and FIPS scores (Table 3, Figure 4). The NDC score predicted 6-year survival with AUCs of 0.906 in the training set and 0.956 in the validation set, which were distinctly better than those of the Child-Pugh score [0.689 (P = 0.002) and 0.670 (P = 0.007)], the MELD score [0.649 (P = 0.001) and 0.661 (P = 0.007)], the MELD-Na score [0.666 (P = 0.001) and 0.748 (P = 0.02)], and the FIPS score [0.583 (P < 0.001) and 0.691 (P = 0.02)]. The excellent calibration of the nomogram was observed in the calibration plots (Figure 5), which were used to analyze the consistency between the observed and predicted probabilities.
| NDC | Child-Pugh | MELD | MELD-Na | FIPS | |
| Training cohort | |||||
| 6-yr AUC | 0.906 | 0.689 | 0.649 | 0.666 | 0.583 |
| 95%CI | 0.791-1.000 | 0.546-0.833 | 0.493-0.805 | 0.515-0.817 | 0.420-0.747 |
| P value vs NDC | 0.002b | 0.001b | 0.001b | < 0.001b | |
| Validation cohort | |||||
| 6-yr AUC | 0.956 | 0.670 | 0.661 | 0.748 | 0.691 |
| 95%CI | 0.868-1.000 | 0.460-0.879 | 0.400-0.921 | 0.541-0.955 | 0.439-0.943 |
| P value vs NDC | 0.007b | 0.007b | 0.02a | 0.02a |
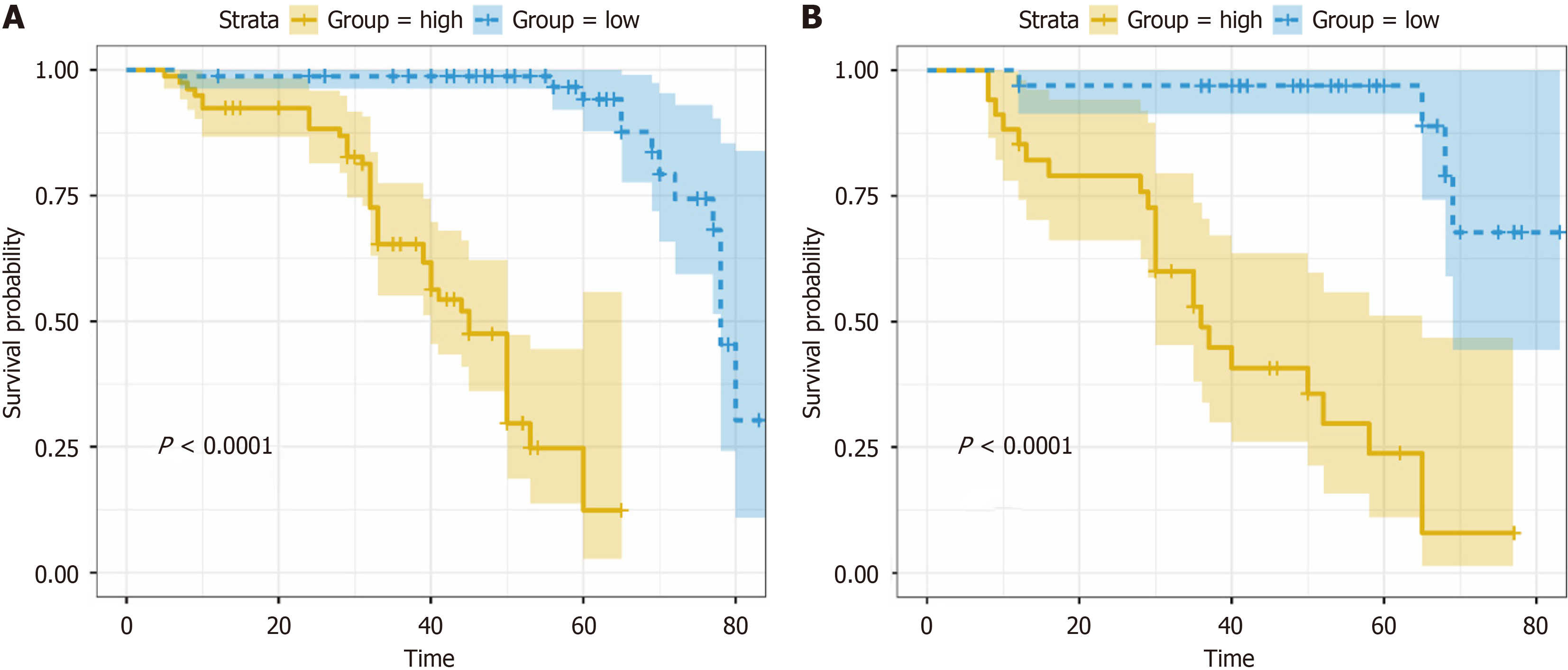
According to the median risk score of the training set (3.85), the training set and the test set were divided into a high-risk group and a low-risk group (patients with a risk score of 3.85 were classified as the low-risk group, and patients with a risk score > 3.85 were classified as the high-risk group). K-M survival analysis was performed for the high- and low-risk groups in the training set and validation set, and the results showed that the survival prognosis was worse in the high-risk group than in the low-risk group (P < 0.001; Figure 6).
It has been widely accepted that TIPS placement can be an important treatment for the complications of portal hy
In the present study, we revealed that the indications for TIPS, shunt reasonability, post-PPG, PVP%, ICGR15 and Tbil were independent long-term prognostic factors in hepatitis cirrhosis patients. Ascites is associated with a higher mortality rate than variceal bleeding is, suggesting that it is a better indicator of advanced cirrhosis. Standards for shunt reasonability have been introduced previously. Importantly, the quality of the shunt tract is influenced by numerous factors, including portal vein pressure, stent selection, shunt location, stent extension into the IVC, portal vein length, blood flow, shunt angle, diameter, morphology, and other related variables. The post-PPG and PVP percentages reflect hemodynamic changes after TIPS placement and can be used to assess the effectiveness of surgery. The ICGR15 and total bilirubin concentration are both used to assess liver function. The NDC model containing the above indicators performed better than did the Child-Pugh, MELD, MELD-Na and FIPS scores in predicting long-term survival. Our study used the median score as a cutoff to stratify patients into two groups according to prognostic risk. K-M analysis revealed that the diffe
This study has several limitations. The patients included in this study were mainly those with hepatitis cirrhosis, and the other four scoring models were mainly based on Western populations with alcoholic cirrhosis. The inconsistency of the characteristics, occurrence, and development of liver injury in patients with cirrhosis of various etiologies may contribute to potential bias in model accuracy. Moreover, in this study, the patients’ renal function was basically normal, and their serum Cr and urea nitrogen levels were basically within the normal ranges, which may reduce the overall predictive performance of models containing the serum Cr concentration as a scoring factor. Additionally, it needs to be confirmed whether Cr can be used as an index for long-term survival in patients with cirrhosis in China following TIPS surgery. This study is also limited by the fact that it was a single-center retrospective analysis with a certain number of participants who were lost to follow-up, potentially resulting in a statistically significant reduction in the mortality rate.
In conclusion, we developed a new prognostic model to predict long-term survival in patients with hepatitis cirrhosis after TIPS placement, which can help identify high-risk patients and guide follow-up management after TIPS implan
The NDC model can accurately predict long-term survival after the TIPS procedure in patients with hepatitis cirrhosis, help identify high-risk patients and guide follow-up management after TIPS implantation. Notably, the development of the NDC model offers a robust tool for predicting long-term survival post-TIPS, surpassing traditional models such as the Child-Pugh, MELD, MELD-Na, and FIPS in terms of accuracy and reliability. However, there is still a need for more comprehensive prediction models leveraging large-sample, multicenter datasets to improve the assessment of long-term survival in patients undergoing TIPS placement in the future.
The transjugular intrahepatic portosystemic shunt (TIPS) represents a therapeutic modality for addressing complications associated with portal hypertension. This technique involves the creation of shunt pathways within the hepatic pa
The pressing need for a more accurate model for assessing long-term survival rates to guide treatment decisions in patients with chronic liver disease is emphasized. Therefore, we are committed to developing a model to predict the long-term survival of patients with hepatitis cirrhosis after TIPS.
The aim of our study was to establish a model to predict long-term survival in patients with hepatitis cirrhosis after the TIPS procedure.
We conducted a retrospective study of 224 patients with PHT who received elective therapy and randomized them into training and validation sets. Continuous variables are presented as the mean with standard deviation, and categorical variables are presented as absolute and relative frequencies [n (%)]. Student’s t test or the Mann-Whitney U test was used to assess the differences in quantitative variables between the groups. The chi-square test was used for analyzing un
We devised a newly developed Cox (NDC) model for predicting long-term survival after TIPS in patients with hepatitis cirrhosis, which outperformed existing scoring models, such as the Child-Pugh, model for end-stage liver disease (MELD), MELD-sodium (MELD-Na) and the Freiburg index of post-TIPS survival (FIPS) scores, for predicting long-term survival.
The NDC model can accurately predict long-term survival after the TIPS procedure in patients with hepatitis cirrhosis, help identify high-risk patients and guide follow-up management after TIPS implantation. Notably, the development of the NDC model offers a robust tool for predicting long-term survival post-TIPS, surpassing traditional models such as the Child-Pugh, MELD, MELD-Na and FIPS in terms of accuracy and reliability.
We can learn from this study that the NDC model can predict long-term survival after TIPS, and its performance was better than that of other scores, such as Child-Pugh, MELD, MELD-Na and FIPS. Future studies should focus on de
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang M, China S-Editor: Zhang H L-Editor: A P-Editor: Xu ZH
| 1. | Lapenna L, Di Cola S, Gazda J, De Felice I, Gioia S, Merli M. New Indications for TIPSs: What Do We Know So Far? J Clin Exp Hepatol. 2023;13:794-803. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 2. | Rössle M, Richter GM, Nöldge G, Palmaz JC, Wenz W, Gerok W. New non-operative treatment for variceal haemorrhage. Lancet. 1989;2:153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Tripathi D, Stanley AJ, Hayes PC, Travis S, Armstrong MJ, Tsochatzis EA, Rowe IA, Roslund N, Ireland H, Lomax M, Leithead JA, Mehrzad H, Aspinall RJ, McDonagh J, Patch D. Transjugular intrahepatic portosystemic stent-shunt in the management of portal hypertension. Gut. 2020;69:1173-1192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 235] [Cited by in RCA: 215] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 4. | Boike JR, Thornburg BG, Asrani SK, Fallon MB, Fortune BE, Izzy MJ, Verna EC, Abraldes JG, Allegretti AS, Bajaj JS, Biggins SW, Darcy MD, Farr MA, Farsad K, Garcia-Tsao G, Hall SA, Jadlowiec CC, Krowka MJ, Laberge J, Lee EW, Mulligan DC, Nadim MK, Northup PG, Salem R, Shatzel JJ, Shaw CJ, Simonetto DA, Susman J, Kolli KP, VanWagner LB; Advancing Liver Therapeutic Approaches (ALTA) Consortium. North American Practice-Based Recommendations for Transjugular Intrahepatic Portosystemic Shunts in Portal Hypertension. Clin Gastroenterol Hepatol. 2022;20:1636-1662.e36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 137] [Article Influence: 45.7] [Reference Citation Analysis (0)] |
| 5. | Abraldes JG, Caraceni P, Ghabril M, Garcia-Tsao G. Update in the Treatment of the Complications of Cirrhosis. Clin Gastroenterol Hepatol. 2023;21:2100-2109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 33] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 6. | Bettinger D, Schultheiss M, Boettler T, Muljono M, Thimme R, Rössle M. Procedural and shunt-related complications and mortality of the transjugular intrahepatic portosystemic shunt (TIPSS). Aliment Pharmacol Ther. 2016;44:1051-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Burgos AC, Thornburg B. Transjugular Intrahepatic Portosystemic Shunt Placement for Refractory Ascites: Review and Update of the Literature. Semin Intervent Radiol. 2018;35:165-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Allegretti AS, Frenk NE, Li DK, Seethapathy H, Vela Parada XF, Long J, Endres P, Pratt DS, Chung RT, Ganguli S, Irani Z, Yamada K. Evaluation of model performance to predict survival after transjugular intrahepatic portosystemic shunt placement. PLoS One. 2019;14:e0217442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Huo TI, Lee SD, Lin HC. Selecting an optimal prognostic system for liver cirrhosis: the model for end-stage liver disease and beyond. Liver Int. 2008;28:606-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Machicao VI. Model for End-Stage Liver Disease-Sodium Score: The Evolution in the Prioritization of Liver Transplantation. Clin Liver Dis. 2017;21:275-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Ascha M, Abuqayyas S, Hanouneh I, Alkukhun L, Sands M, Dweik RA, Tonelli AR. Predictors of mortality after transjugular portosystemic shunt. World J Hepatol. 2016;8:520-529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Bettinger D, Sturm L, Pfaff L, Hahn F, Kloeckner R, Volkwein L, Praktiknjo M, Lv Y, Han G, Huber JP, Boettler T, Reincke M, Klinger C, Caca K, Heinzow H, Seifert LL, Weiss KH, Rupp C, Piecha F, Kluwe J, Zipprich A, Luxenburger H, Neumann-Haefelin C, Schmidt A, Jansen C, Meyer C, Uschner FE, Brol MJ, Trebicka J, Rössle M, Thimme R, Schultheiss M. Refining prediction of survival after TIPS with the novel Freiburg index of post-TIPS survival. J Hepatol. 2021;74:1362-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 101] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 13. | Henry Z, Patel K, Patton H, Saad W. AGA Clinical Practice Update on Management of Bleeding Gastric Varices: Expert Review. Clin Gastroenterol Hepatol. 2021;19:1098-1107.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 14. | European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1125] [Cited by in RCA: 1129] [Article Influence: 75.3] [Reference Citation Analysis (0)] |
| 15. | de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2011] [Cited by in RCA: 2278] [Article Influence: 227.8] [Reference Citation Analysis (3)] |
| 16. | Lee HL, Lee SW. The role of transjugular intrahepatic portosystemic shunt in patients with portal hypertension: Advantages and pitfalls. Clin Mol Hepatol. 2022;28:121-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Bosch J. Small diameter shunts should lead to safe expansion of the use of TIPS. J Hepatol. 2021;74:230-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 18. | Rössle M, Haag K, Ochs A, Sellinger M, Nöldge G, Perarnau JM, Berger E, Blum U, Gabelmann A, Hauenstein K. The transjugular intrahepatic portosystemic stent-shunt procedure for variceal bleeding. N Engl J Med. 1994;330:165-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 474] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 19. | Molodianovitch K, Faraggi D, Reiser B. Comparing the areas under two correlated ROC curves: parametric and non-parametric approaches. Biom J. 2006;48:745-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Vizzutti F, Celsa C, Calvaruso V, Enea M, Battaglia S, Turco L, Senzolo M, Nardelli S, Miraglia R, Roccarina D, Campani C, Saltini D, Caporali C, Indulti F, Gitto S, Zanetto A, Di Maria G, Bianchini M, Pecchini M, Aspite S, Di Bonaventura C, Citone M, Guasconi T, Di Benedetto F, Arena U, Fanelli F, Maruzzelli L, Riggio O, Burra P, Colecchia A, Villa E, Marra F, Cammà C, Schepis F. Mortality after transjugular intrahepatic portosystemic shunt in older adult patients with cirrhosis: A validated prediction model. Hepatology. 2023;77:476-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 21. | Song J, Wang X, Yan Y, Xiang T, Luo X. Validating the prognostic value of Freiburg index of posttransjugular intrahepatic portosystemic shunt survival score and classic scores in Chinese patients with implantation of transjugular intrahepatic portosystemic shunt. Eur J Gastroenterol Hepatol. 2022;34:1074-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Gotthardt D, Weiss KH, Baumgärtner M, Zahn A, Stremmel W, Schmidt J, Bruckner T, Sauer P. Limitations of the MELD score in predicting mortality or need for removal from waiting list in patients awaiting liver transplantation. BMC Gastroenterol. 2009;9:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Krishnan A, Woreta TA, Vaidya D, Liu Y, Hamilton JP, Hong K, Dadabhai A, Ma M. MELD or MELD-Na as a Predictive Model for Mortality Following Transjugular Intrahepatic Portosystemic Shunt Placement. J Clin Transl Hepatol. 2023;11:38-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 24. | El-Khateeb E, Darwich AS, Achour B, Athwal V, Rostami-Hodjegan A. Review article: time to revisit Child-Pugh score as the basis for predicting drug clearance in hepatic impairment. Aliment Pharmacol Ther. 2021;54:388-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 25. | Yang C, Chen Q, Zhou C, Liu J, Huang S, Wang Y, Wang C, Ju S, Chen Y, Li T, Bai Y, Yao W, Xiong B. FIPS Score for Prediction of Survival After TIPS Placement: External Validation and Comparison With Traditional Risk Scores in a Cohort of Chinese Patients With Cirrhosis. AJR Am J Roentgenol. 2022;219:255-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |