Published online Sep 27, 2022. doi: 10.4240/wjgs.v14.i9.1060
Peer-review started: April 21, 2022
First decision: July 14, 2022
Revised: July 22, 2022
Accepted: August 19, 2022
Article in press: August 19, 2022
Published online: September 27, 2022
Processing time: 153 Days and 18.4 Hours
Acute appendicitis (AA) is one of the main indications for urgent surgery. Laparoscopic appendectomy (LA) has shown advantages in terms of clinical results and cost-effectiveness, even if there is still controversy about different devices to utilize, especially with regards to the endoloop (EL) vs endostapler (ES) when it comes to stump closure.
To compare safety and cost-effectiveness of EL vs ES.
From a prospectively maintained database, data of 996 consecutive patients treated by LA with a 3 years-follow up in the department of Emergency General Surgery - St Orsola University Hospital, Bologna (Italy) were retrieved. A meta-analysis was performed in terms of surgical complications, in comparison to the international literature published from 1995 to 2021.
The meta-analysis showed no evidence regarding wound infections, abdominal abscesses, and total post-operative complications, in terms of superiority of a surgical technique for the stump closure in LA.
Even when AA is complicated, the routine use of EL is safe in most patients.
Core Tip: Stump closure in the acute appendectomy setting could be performed via endoloop (EL) or endostapler use. The present meta-analysis assesses the experience of 996 patients consecutively treated in the department of Emergency General Surgery - St Orsola University Hospital, Bologna (Italy) and the evidence published in literature, confirming there is no superiority of a surgical method on how to perform the stump closure, with regards to wound infections, abdominal abscess, and total post-operative complications. Even when acute appendicitis is complicated, the routine use of EL is safe in most patients.
- Citation: Zorzetti N, Lauro A, Bellini MI, Vaccari S, Dalla Via B, Cervellera M, Cirocchi R, Sorrenti S, D’Andrea V, Tonini V. Laparoscopic appendectomy, stump closure and endoloops: A meta-analysis. World J Gastrointest Surg 2022; 14(9): 1060-1071
- URL: https://www.wjgnet.com/1948-9366/full/v14/i9/1060.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i9.1060
Acute appendicitis (AA) is one of the most frequent causes of acute abdominal pain and access to emergency care department. The lifetime chance of developing AA is lower in women, and the risk of being subject to surgery is higher in males[1], representing in fact one of the main indications for an urgent operation. Surgery is generally performed via a laparoscopic approach, and given the high volume of AA procedures worldwide, it represents a training operation as well[2].
Laparoscopic appendectomy (LA)[3,4] is demonstrated to be superior in terms of clinical results[5-9] and cost-effectiveness[10-14], even if there is still controversy[15-19] about the use of different devices during the operation[20-24]. Currently, it is still debated the use of endostapler (ES) vs endoloop (EL) in appendiceal stump closure[25-28]. The routine use of EL is safe in most patients affected by AA, also when it is complicated[29-32], representing a cost-effective device when taking into consideration the additional costs of potential post-operative complications, too[33-37]. We have previously shown money saving as well as the safety of the routine use of ELs[38]. The aim of this study is to meta-analyze the international literature, to compare the outcome of the patients laparoscopically treated in Bologna via EL to the data from the international literature.
Between November 2011 and January 2018, a total of 1045 LAs were performed in the department of Emergency General Surgery - St Orsola University Hospital, Bologna (Italy). Patients who undergone LA until January 2018 were identified retrospectively from a prospectively maintained database, so that a 3-year follow-up was achieved[39,40]. All grades of post-operative complications were collected and examined. Institutional review board for this study was not required, as this is a meta-analysis of already previous published data. At Bologna centre, patients were initially evaluated by a general surgeon, then underwent laboratory tests, and Alvarado or appendicitis inflammatory response (AIR) score (Table 1) were calculated in females and in males respectively[41,42].
| Alvarado score | AIR score | |
| Likely appendicitis | 7-10 | 9-12 |
| Probably appendicitis | 5-6 | 5-8 |
| Unlikely appendicitis | 0-4 | 0-4 |
Surgical procedures were performed by attendants or supervised trainees. Written informed consent was signed by all the patients before the procedures. Antibiotic prophylaxis was always administered. A supraumbilical 12 mm-Hasson trocar with an open approach was adopted to induce pneumoperitoneum and initiate laparoscopy. Then, 2 other operative trocars were placed in the left flank (10 mm) and suprapubic position (5 mm), with identification of the appendix, cut and coagulation of the mesoappendix.
The choice of EL vs ES to close the base of the appendiceal stump was made by the operating surgeon, after evaluating the inflammatory infiltration of the appendicular base[43]. If an EL was used, the appendicular stump was cut 3-5 mm away from cecum. The surgical specimen was then removed in an endobag through the 12 mm trocar.
Patients were divided in two groups (EL and ES) and in three categories (edematous, phlegmonous and gangrenous appendicitis) based on the severity of the histological examination. Cases requiring conversion to open appendectomy were excluded, while 996 LA (95.3%) were included in the meta-analysis.
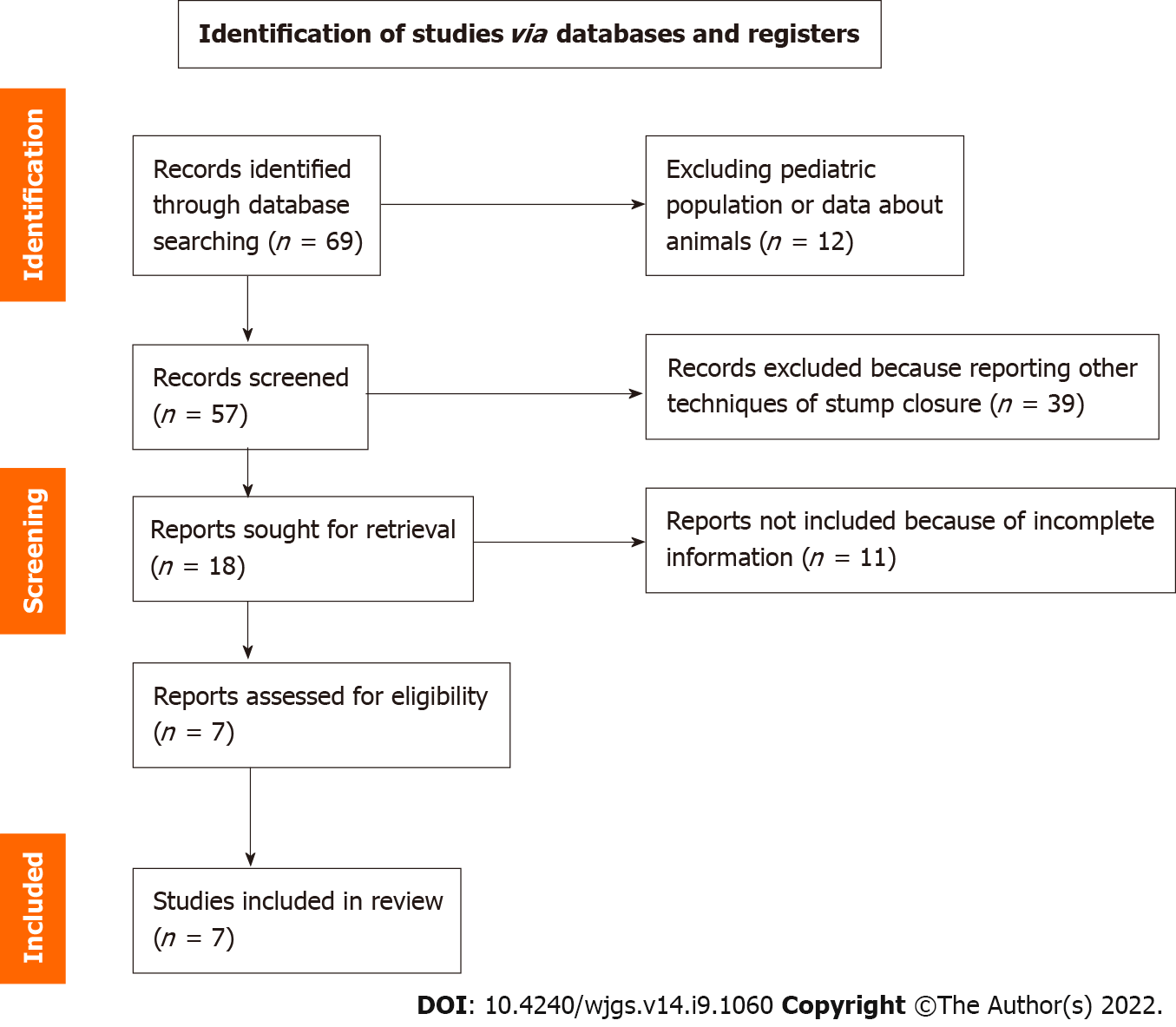
A meta-analysis was performed in terms of surgical complications, comparing the clinical data of the EL group (821 patients) to the international literature retrieved by Pubmed (Figure 1), according to the PRISMA principles[44].
Manuscripts were excluded from the analysis if they dealt with pediatric patients (< 15 years of age) or were published before 1995.
Data were collected and analyzed with MedCalc software. Statistical expertise was available to the authors. MedCalc 13.0.6.0 (MedCalc Software bvba, Østend, Belgium) was used for the meta-analysis. MedCalc uses a Freeman-Tukey transformation (arcsine square root transformation) to calculate the weighted summary proportion under the fixed and random effects model. The program lists the proportions (expressed as a percentage), with their 95% confidence interval (CI), found in the individual studies included in the meta-analysis. The heterogeneity was evaluated by means of statistics Cohran’s Q and I2. The results of the different studies, with 95%CI, and the pooled proportions with 95%CI are shown in a forest plot. Bias was detected using a funnel plot. Publication bias results in asymmetry of the funnel plot. P < 0.05 was considered statistically significant.
The sample of our study consisted of all our patients treated with EL for a total of eight hundred twenty-one patients (Table 2), corresponding to the 78.5% of all LAs. Post-operative complications in this group of interest were collected (Table 3) and reported according to the Clavien-Dindo classification[45,46] (Table 4). These data were then compared to those retrieved from the manuscripts finally considered in the analysis[9,19,26,29-31,47] (Table 5), in fact other four papers that were initially assessed and that were from the last 3 years[48-51], were not included, because of the lack of information and partial numbers and percentages of patients with wound infections, abdominal abscesses and total post-operative complications.
| EL (n = 821) | ES (n = 175) | P values | |
| Age (yr) | 35 (14-94) ± 18 | 36 (14-91) ± 17 | 0.50 |
| Male:Female | 425:396 | 111:64 | < 0.05 |
| BMI | 23.85 (14-44) ± 4.4 | 24 (17-42) ± 4.5 | 0.68 |
| CV comorbidities | 7.6% | 24% | < 0.05 |
| Other comorbidities | 13.9% | 31.4% | < 0.05 |
| Edematous AA | 251 | 5 | 0.18 |
| Phlegmonous AA | 410 | 59 | 0.05 |
| Gangrenous AA | 160 | 111 | 0.05 |
| EL (n = 821) | |
| Wound infections | 2 (0.3%) |
| Abdominal abscesses | 12 (1.5%) |
| Post-op complications IIIa/IIIb Clavien-Dindo | 17 (2%) |
| Total post-op complications | 35 (4.3%) |
| Clavien-Dindo | Number of patients (% of total cohort) |
| I | 3 (0.3) |
| II | 24 (2.4) |
| IIIa | 7 (0.7) |
| IIIb | 16 (1.6) |
| IVa | 0 (0) |
| IVb | 0 (0) |
| V | 0 (0) |
| Total | 50 (5) |
| Ref. | Number of patients (% of EL) | Wound infection | Abdominal abscesses | Post-op complications |
| Bologna experience | 821 (78.5) | 2 (0.3%) | 12 (1.5%) | 26 (3.2%) |
| Ortega et al[9], 1995 | 89 | 4 (4.5%) | 4 (4.5%) | 14 (15.7%) |
| Sadat-Safavi et al[19], 2016 | 38 (50) | 1 (2.6%) | 0 (0%) | 0 (0%) |
| Beldi et al[26], 2006 | 2565 (39.5) | 12 (0.5%) | 41 (1.6%) | 37 (1.4%) |
| Sahm et al[29], 2011 | 1670 (97.3) | 34 (2%) | 27 (1.6%) | 48 (2.9%) |
| Van Rossem et al[30], 2017 | 1050 (76.7) | 16 (1.5%) | 48 (4.5%) | 20 (1.9%) |
| Swank et al[31], 2014 | 465 (44.9) | 7 (1.5%) | 20 (4.3%) | 14 (3.1%) |
| Klima et al[47], 1998 | 100 | 3 (3%) | 4 (4%) | 4 (4%) |
Examination of the seven papers involved in the meta-analysis[9,19,26,29-31,47] showed that only Beldi et al[26] were in favor of application of an ES for transection and closure of the appendiceal stump in patients with AA. In their report it lowered the risk of postoperative intra-abdominal surgical-site infection and the need for readmission to hospital. All the other 6 papers didn’t find a statistically significant difference for intra or postsurgical complications, length of stay (LOS), wound infections, and abdominal abscesses among different groups of patients. Sahm et al[29] and Van Rossem et al[30] clearly stated that infectious complication rate is not influenced by the type of appendicular stump closure, either if performed by EL or ES, and routine stump closure using an EL is an easy, safe, and cost-effective procedure. Finally, it is important to mention the retrospective cohort study conducted by Swank et al[31] that compares the two strategies for closure of the appendiceal stump. The routine use of the ES showed no clinical advantages over the use of ELs.
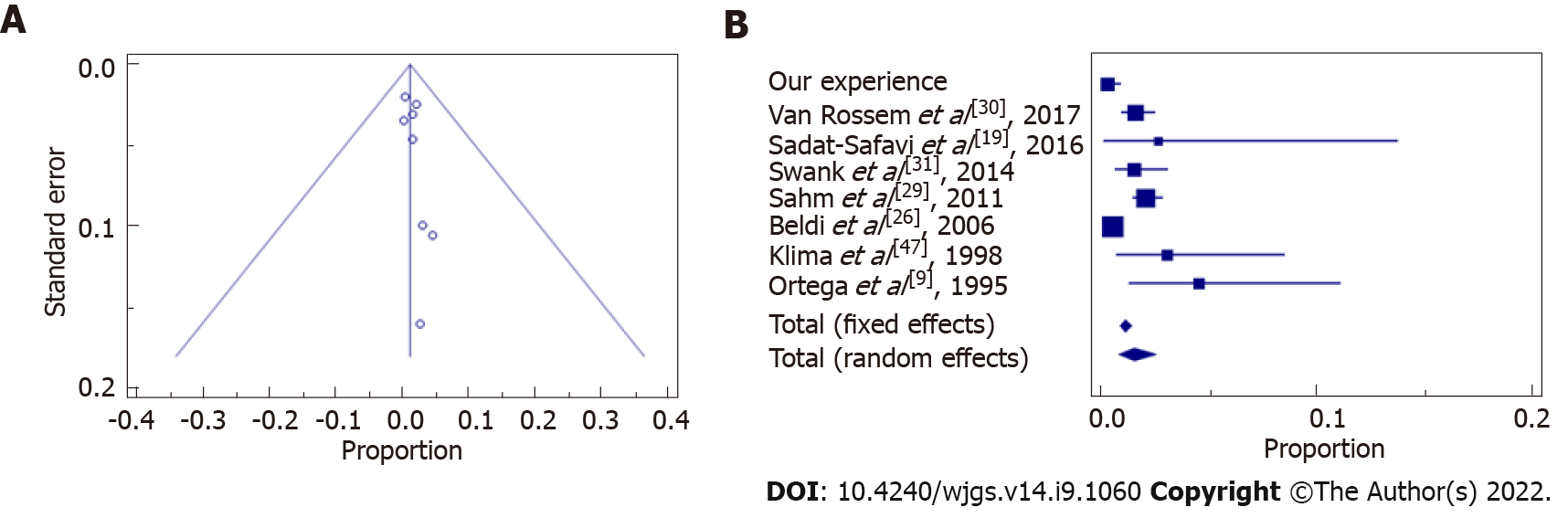
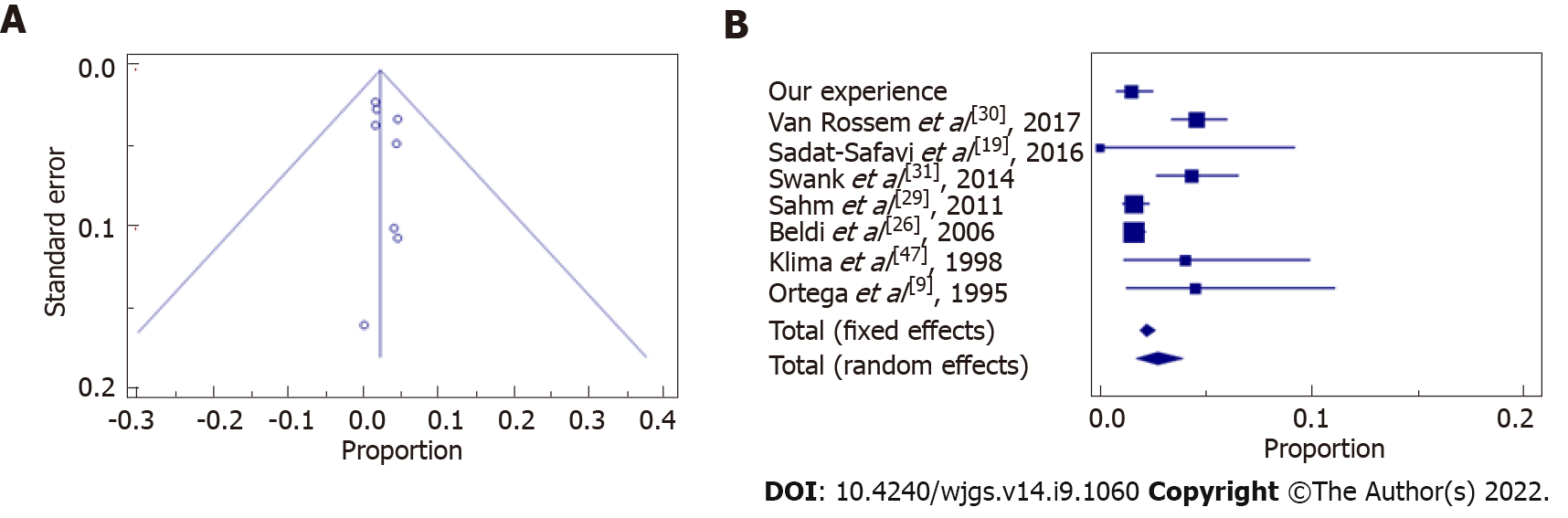
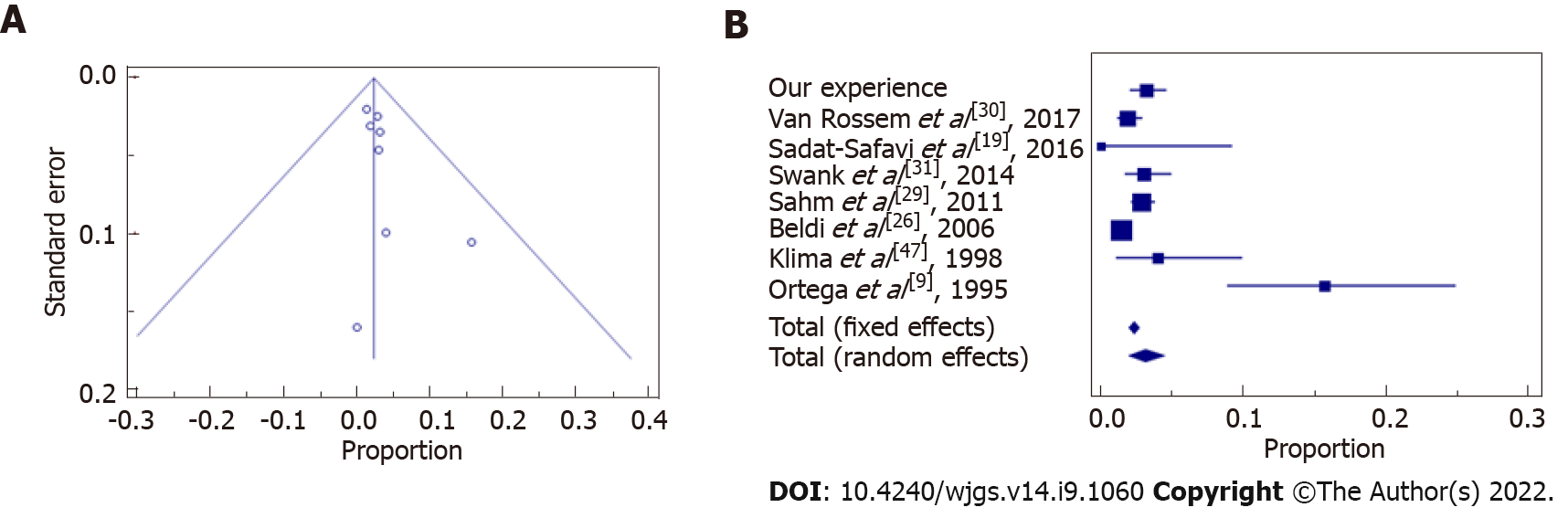
Statistical data and results showed that our experience followed the trend of the evidence in literature in terms of wound infections (Figure 2 and Table 6), abdominal abscesses (Figure 3 and Table 7) and total post-operative complications (Figure 4 and Table 8). The meta-analysis proved a wide heterogeneity among analyzed groups, as the funnel plots and the forest plots confirmed. Tables 6-8 report data related to the standard deviation of wound infection, abdominal abscesses, and post-operative complications, respectively. Figures 2A, 3A and 4A are Funnel Plots showing an asymmetrical distribution of the articles (dot) among both sides indicating that bias can be present. In Figures 2A and 4A, few papers are near the middle solid line, indicating the overall effect from the meta-analysis, possibly in relation to the limited size of the samples. Figures 2B, 3B and 4B Forrest Plots prove there is no statistically significant result in favor of ES or EL for the overall incidence of wound infections, abdominal abscess, or post-operative complications.
| Ref. | Standard deviation | Proportion (%) | 95%CI |
| Our experience | 821 | 0.244 | 0.0295-0.877 |
| Van Rossem et al[30], 2017 | 1050 | 1.524 | 0.873-2.463 |
| Sadat-Safavi et al[19], 2016 | 38 | 2.632 | 0.0666-13.810 |
| Swank et al[31], 2014 | 465 | 1.505 | 0.607-3.077 |
| Sahm et al[29], 2011 | 1670 | 2.036 | 1.414-2.833 |
| Beldi et al[26], 2006 | 2565 | 0.468 | 0.242-0.816 |
| Klima et al[47], 1998 | 100 | 3.000 | 0.623-8.518 |
| Ortega et al[9], 1995 | 89 | 4.494 | 1.238-11.109 |
| Total (fixed effects) | 6798 | 1.064 | 0.834-1.337 |
| Total (random effects) | 6798 | 1.496 | 0.759-2.475 |
| Ref. | Standard deviation | Proportion (%) | 95%CI |
| Our experience | 821 | 1.462 | 0.757-2.539 |
| Van Rossem et al[30], 2017 | 1050 | 4.571 | 3.390-6.016 |
| Sadat-Safavi et al[19], 2016 | 38 | 0.000 | 0.000-9.251 |
| Swank et al[31], 2014 | 465 | 4.301 | 2.647-6.565 |
| Sahm et al[29], 2011 | 1670 | 1.617 | 1.068-2.344 |
| Beldi et al[26], 2006 | 2565 | 1.598 | 1.149-2.162 |
| Klima et al[47], 1998 | 100 | 4.000 | 1.100-9.926 |
| Ortega et al[9], 1995 | 89 | 4.494 | 1.238-11.109 |
| Total (fixed effects) | 6798 | 2.206 | 1.870-2.583 |
| Total (random effects) | 6798 | 2.699 | 1.697-3.924 |
| Ref. | Standard deviation | Proportion (%) | 95%CI |
| Our experience | 821 | 3.167 | 2.079-4.606 |
| Van Rossem et al[30], 2017 | 1050 | 1.905 | 1.167-2.926 |
| Sadat-Safavi et al[19], 2016 | 38 | 0.000 | 0.000-9.251 |
| Swank et al[31], 2014 | 465 | 3.011 | 1.656-5.000 |
| Sahm et al[29], 2011 | 1670 | 2.874 | 2.127-3.793 |
| Beldi et al[26], 2006 | 2565 | 1.442 | 1.018-1.983 |
| Klima et al[47], 1998 | 100 | 4.000 | 1.100-9.926 |
| Ortega et al[9], 1995 | 89 | 15.730 | 8.875-24.982 |
| Total (fixed effects) | 6798 | 2.304 | 1.961-2.689 |
| Total (random effects) | 6798 | 3.089 | 1.979-4.437 |
Appendectomy is one of the most performed emergency surgery procedures. The laparoscopic approach is recognized and recommended internationally, but a matter of debate during the operation is the choice of the different available devices to close the appendicular stump, in consideration of the possible consequent leak leading to infection and postoperative complications.
Already previously[38], we evidenced that the routine use of EL is safe in most patients affected by AA, including cases with signs of complications. Furthermore, it is a cost-effective device, even when possible additional costs secondary to the occurrence of adverse events in the post-operative course are included. Conversely, Lasek et al[48] assessed via a multicenter observational study the stump closure only in patients affected by complicated AA. Their results highlighted some clinical benefits of ES use, but EL was superior in terms of overall morbidity and LOS, with no statistically significant difference in major complication rates and postoperative intra-abdominal abscess formation.
In literature, two papers systematically analyzed the techniques for appendiceal stump closure during LA[49,50]. Ceresoli et al[49] meta-analysed randomized trials and cohort studies comparing ES with endoscopic loop ties for the closure of the appendicular stump in LA, including pediatric patients and complicated AA, such as gangrenous/necrotic appendix or the perforated ones. In their analysis, ES was associated with a similar intra-abdominal abscess rate, but a lower incidence of wound infection, while LOS, readmission and reoperation rates were similar. In a subgroup analysis ES significantly reduced the wound infection rate in pediatric patients, while no difference in the main outcomes was observed in patients with complicated AA.
Makaram et al[50] performed a systematic review evaluating all methods of stump closure (ELs, polymeric endoclips, metallic endoclips, endosuture and ES). In this study[50], no difference in complication rate, LOS or cost was found. According to their analysis, endoclips provide the most time-efficient method of closure, although not statistically significant; closure by endosuture, represents the cheapest method, but it is hindered by a high complication rate. Current evidence suggests endosuture should then be avoided. ESs appear very safe and effective for stump closure, however they seem to be associated with high postoperative complication rates; furthermore, the consequent cost limits their use to the most severe cases of appendicitis, while instead EL provides a valuable alternative for closure, with a risk of intraoperative complications of 4.61%.
Another recent retrospective cohort study[51], whose subject was to determine the safety and efficiency of the use of EL and ES in complicated and uncomplicated AA, concluded that the systematic use of EL could reduce costs in uncomplicated appendicitis, while in complicated cases both options (loop and stapler) are valid. Also a prospective randomized clinical trial[52] and a retrospective study[53] recently analyzed the technical aspects of appendix stump closure: Ihnát et al[52] reported similar postoperative morbidity and safety following the use of EL, ES or hem-o-lok and even White et al[53] demonstrated non univocal superiority of one technique over the others, too.
Another point indeed to be considered is LA availability together with the fact that the different devices rely upon the resources of the hospital and the country where surgery is performed, pending possible spending reviews carried out by the government. It has been demonstrated that LA is performed more frequently in high-income countries in comparison to low-income countries (67.7% vs 8.1%), with better postoperative outcomes[54]. The difference in the costs of the used surgical devices (above all stapler) represented a principal determinant for the overall economic impact of the surgical procedure in some recent reports[33,36,38,50,51], to highlight how important is the cost-effectiveness in the measured outcomes. The medium saving reported in the present paper is relevant, varying from around approximately 300 € to more than 500 € just for the device, which then must be multiplied for the many LA conducted worldwide; further cost-analysis including operative time and LOS could reach major savings.
Our study presents some limitations: The design is a retrospective analysis to investigate the safety of ELs, then the results are pooled with other reports; the comparison between studies is difficult due to heterogenous patient selection and outcomes measured. However, EL seems to have the potential for being a safe and cost-effective device.
In conclusion, there is no evidence clearly illustrating a superior surgical method for performing stump closure in LA. Given that comparison between studies is difficult due to heterogeneous patient selection and measured outcomes, our meta-analysis shows that the data of our sample, related to wound infections, post-operative abdominal abscesses, and total post-operative complications, mirror current literature trend. The routine use of EL is safe in most patients affected by AA, even when complicated, and these findings could have above all more relevance in lower resource environments that may not have easy access to ES. Prospective studies are needed to analyze a greater number of patients and taking into account an accurate grading system for AA severity such as Disease Severity Score[55], Alvarado Score[41], AIR Score[42] or imaging severity scoring, such as the CT-Determined Severity Score[56]. Their aim should be first to stratify preoperatively the grade of AA and secondly to observe differences in postoperative complications. Finally, studies aiming at an accurate cost analysis are required, ideally in the form of randomized controlled trials comparing EL to polymeric clips, as both techniques are safe and effective, with favorable outcomes[50,52].
Laparoscopic appendectomy (LA) has shown advantages in terms of clinical results and cost-effectiveness, even if there is still controversy about which surgical device should be preferred to perform it.
To evaluate the safety cost-effectiveness of surgical devices in LA stump closure.
Incidence of wound infections, abdominal abscesses and total post-operative complications according to the Dindo-Clavien classification in LA stump closure with endoloop (EL) or endostapler.
A meta-analysis was performed in terms of surgical complications, comparing the clinical data of the EL group (821 patients) to the international literature retrieved by Pubmed, according to the PRISMA principles.
There is no superiority of one or another technique in terms of surgical complications for LA stump closure.
Routine use of EL is safe in most patients affected by acute appendectomy, even when complicated.
Studies of EL performing accurate cost analysis are required, in addition to randomized controlled trials comparing this method to polymeric clips, as both techniques have been proved to have to be safe and effective with favorable outcomes.
Provenance and peer review: Invited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Hori T, Japan; Li J, China; Ni X, China; Saif U, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000;215:337-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 343] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 2. | Ussia A, Vaccari S, Gallo G, Grossi U, Ussia R, Sartarelli L, Minghetti M, Lauro A, Barbieri P, Di Saverio S, Cervellera M, Tonini V. Laparoscopic appendectomy as an index procedure for surgical trainees: clinical outcomes and learning curve. Updates Surg. 2021;73:187-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Costa-Navarro D, Jiménez-Fuertes M, Illán-Riquelme A. Laparoscopic appendectomy: quality care and cost-effectiveness for today's economy. World J Emerg Surg. 2013;8:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT, Stamos MJ. Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the Nationwide Inpatient Sample (NIS), 2006-2008. J Gastrointest Surg. 2011;15:2226-2231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Sajid MS, Rimple J, Cheek E, Baig MK. Use of endo-GIA versus endo-loop for securing the appendicular stump in laparoscopic appendicectomy: a systematic review. Surg Laparosc Endosc Percutan Tech. 2009;19:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Coşkun H, Hasbahçeci M, Bozkurt S, Çipe G, Malya FÜ, Memmi N, Karatepe O, Akçakaya A, Müslümanoğlu M. Is concomitant cholecystectomy with laparoscopic sleeve gastrectomy safe? Turk J Gastroenterol. 2014;25:624-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Sohn M, Agha A, Bremer S, Lehmann KS, Bormann M, Hochrein A. Surgical management of acute appendicitis in adults: A review of current techniques. Int J Surg. 2017;48:232-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Di Saverio S, Mandrioli M, Sibilio A, Smerieri N, Lombardi R, Catena F, Ansaloni L, Tugnoli G, Masetti M, Jovine E. A cost-effective technique for laparoscopic appendectomy: outcomes and costs of a case-control prospective single-operator study of 112 unselected consecutive cases of complicated acute appendicitis. J Am Coll Surg. 2014;218:e51-e65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Ortega AE, Hunter JG, Peters JH, Swanstrom LL, Schirmer B. A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy. Laparoscopic Appendectomy Study Group. Am J Surg. 1995;169:208-12; discussion 212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 217] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 10. | Lucchi A, Berti P, Grassia M, Siani LM, Gabbianelli C, Garulli G. Laparoscopic appendectomy: Hem-o-lok versus Endoloop in stump closure. Updates Surg. 2017;69:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Takami T, Yamaguchi T, Yoshitake H, Hatano K, Kataoka N, Tomita M, Makimoto S. A clinical comparison of laparoscopic versus open appendectomy for the treatment of complicated appendicitis: historical cohort study. Eur J Trauma Emerg Surg. 2020;46:847-851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Shimoda M, Maruyama T, Nishida K, Suzuki K, Tago T, Shimazaki J, Suzuki S. Comparison of clinical outcome of laparoscopic versus open appendectomy, single center experience. Heliyon. 2018;4:e00635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Guadagni S, Cengeli I, Galatioto C, Furbetta N, Piero VL, Zocco G, Seccia M. Laparoscopic repair of perforated peptic ulcer: single-center results. Surg Endosc. 2014;28:2302-2308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Gorter RR, Heij HA, Eker HH, Kazemier G. Laparoscopic appendectomy: State of the art. Tailored approach to the application of laparoscopic appendectomy? Best Pract Res Clin Gastroenterol. 2014;28:211-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Antoniou SA, Mavridis D, Hajibandeh S, Antoniou GA, Gorter R, Tenhagen M, Koutras C, Pointner R, Chalkiadakis GE, Granderath FA, Fragiadakis GF, Philalithis AE, Bonjer HJ. Optimal stump management in laparoscopic appendectomy: A network meta-analysis by the Minimally Invasive Surgery Synthesis of Interventions and Outcomes Network. Surgery. 2017;162:994-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Aziret M, Çetinkünar S, Erdem H, Kahramanca Ş, Bozkurt H, Dülgeroğlu O, Yıldırım AC, İrkörücü O, Gölboyu EB. Comparison of open appendectomy and laparoscopic appendectomy with laparoscopic intracorporeal knotting and glove endobag techniques: A prospective observational study. Turk J Surg. 2017;33:258-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Partecke LI, Kessler W, von Bernstorff W, Diedrich S, Heidecke CD, Patrzyk M. Laparoscopic appendectomy using a single polymeric clip to close the appendicular stump. Langenbecks Arch Surg. 2010;395:1077-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Al-Temimi MH, Berglin MA, Kim EG, Tessier DJ, Johna SD. Discussion of: "Endostapler versus Hem-O-Lok clip to secure the appendiceal stump and mesoappendix during laparoscopic appendectomy". Am J Surg. 2017;214:1149-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Sadat-Safavi SA, Nasiri S, Shojaiefard A, Jafari M, Abdehgah AG, Notash AY Jr, Soroush A. Comparison the effect of stump closure by endoclips versus endoloop on the duration of surgery and complications in patients under laparoscopic appendectomy: A randomized clinical trial. J Res Med Sci. 2016;21:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Delibegović S. The use of a single Hem-o-lok clip in securing the base of the appendix during laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A. 2012;22:85-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Bali İ, Karateke F, Özyazıcı S, Kuvvetli A, Oruç C, Menekşe E, Emir S, Özdoğan M. Comparison of intracorporeal knotting and endoloop for stump closure in laparoscopic appendectomy. Ulus Travma Acil Cerrahi Derg. 2015;21:446-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Mayir B, Ensari CÖ, Bilecik T, Aslaner A, Oruç MT. Methods for closure of appendix stump during laparoscopic appendectomy procedure. Ulus Cerrahi Derg. 2015;31:229-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Yıldız I, Koca S. Is There An Ideal Stump Closure Technique In Laparoscopic Appendectomy? Surg Technol Int. 2016;28:117-120. [PubMed] |
| 24. | Delibegović S, Mehmedovic Z. The influence of the different forms of appendix base closure on patient outcome in laparoscopic appendectomy: a randomized trial. Surg Endosc. 2018;32:2295-2299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 25. | Kazemier G, in't Hof KH, Saad S, Bonjer HJ, Sauerland S. Securing the appendiceal stump in laparoscopic appendectomy: evidence for routine stapling? Surg Endosc. 2006;20:1473-1476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 26. | Beldi G, Vorburger SA, Bruegger LE, Kocher T, Inderbitzin D, Candinas D. Analysis of stapling versus endoloops in appendiceal stump closure. Br J Surg. 2006;93:1390-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 82] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 27. | Caglià P, Tracia A, Borzì L, Amodeo L, Tracia L, Veroux M, Amodeo C. Incisional hernia in the elderly: risk factors and clinical considerations. Int J Surg. 2014;12 Suppl 2:S164-S169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 28. | Sohn M, Hoffmann M, Pohlen U, Lauscher JC, Zurbuchen U, Holmer C, Buhr HJ, Lehmann KS. [Stump closure in laparoscopic appendectomy. Influence of endoloop or linear stapler on patient outcome]. Chirurg. 2014;85:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Sahm M, Kube R, Schmidt S, Ritter C, Pross M, Lippert H. Current analysis of endoloops in appendiceal stump closure. Surg Endosc. 2011;25:124-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 30. | van Rossem CC, van Geloven AA, Schreinemacher MH, Bemelman WA; snapshot appendicitis collaborative study group. Endoloops or endostapler use in laparoscopic appendectomy for acute uncomplicated and complicated appendicitis : No difference in infectious complications. Surg Endosc. 2017;31:178-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | Swank HA, van Rossem CC, van Geloven AA, in't Hof KH, Kazemier G, Meijerink WJ, Lange JF, Bemelman WA. Endostapler or endoloops for securing the appendiceal stump in laparoscopic appendectomy: a retrospective cohort study. Surg Endosc. 2014;28:576-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 32. | Beldi G, Muggli K, Helbling C, Schlumpf R. Laparoscopic appendectomy using endoloops: a prospective, randomized clinical trial. Surg Endosc. 2004;18:749-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 51] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Mehdorn M, Schürmann O, Mehdorn HM, Gockel I. Intended cost reduction in laparoscopic appendectomy by introducing the endoloop: a single center experience. BMC Surg. 2017;17:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Rakić M, Jukić M, Pogorelić Z, Mrklić I, Kliček R, Družijanić N, Perko Z, Patrlj L. Analysis of endoloops and endostaples for closing the appendiceal stump during laparoscopic appendectomy. Surg Today. 2014;44:1716-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Kryspin M, Wyrzykowsk D. Outcomes of Open and Laparoscopic Appendectomy With Single Endoloop Stump Closure. JSLS. 2018;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Kim S, Weireter L. Cost Effectiveness of Different Methods of Appendiceal Stump Closure during Laparoscopic Appendectomy. Am Surg. 2018;84:1329-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Granados-Romero JJ, Valderrama-Treviño AI, Barrera-Mera B, Uriarte-Ruíz K, Banegas-Ruiz R, Ceballos-Villalva JC. [Comparación entre ligadura con lazo hemostático y engrapadora mecánica lineal para el cierre de base apendicular]. Cir Cir. 2018;86:428-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Zorzetti N, Lauro A, Vaccari S, Ussia A, Brighi M, D'andrea V, Cervellera M, Tonini V. A systematic review on the cost evaluation of two different laparoscopic surgical techniques among 996 appendectomies from a single center. Updates Surg. 2020;72:1167-1174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 39. | Antonacci N, Ricci C, Taffurelli G, Monari F, Del Governatore M, Caira A, Leone A, Cervellera M, Minni F, Cola B. Laparoscopic appendectomy: Which factors are predictors of conversion? Int J Surg. 2015;21:103-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 40. | Finnerty BM, Wu X, Giambrone GP, Gaber-Baylis LK, Zabih R, Bhat A, Zarnegar R, Pomp A, Fleischut P, Afaneh C. Conversion-to-open in laparoscopic appendectomy: A cohort analysis of risk factors and outcomes. Int J Surg. 2017;40:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 41. | Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15:557-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 838] [Cited by in RCA: 814] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 42. | Kollár D, McCartan DP, Bourke M, Cross KS, Dowdall J. Predicting acute appendicitis? World J Surg. 2015;39:104-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 43. | Chu T, Chandhoke RA, Smith PC, Schwaitzberg SD. The impact of surgeon choice on the cost of performing laparoscopic appendectomy. Surg Endosc. 2011;25:1187-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 44. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 39933] [Article Influence: 9983.3] [Reference Citation Analysis (2)] |
| 45. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24754] [Article Influence: 1178.8] [Reference Citation Analysis (0)] |
| 46. | Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6210] [Cited by in RCA: 8582] [Article Influence: 536.4] [Reference Citation Analysis (0)] |
| 47. | Klima S. [Importance of appendix stump management in laparoscopic appendectomy]. Zentralbl Chir. 1998;123 Suppl 4:90-93. [PubMed] |
| 48. | Lasek A, Wysocki M, Mavrikis J, Myśliwiec P, Bobowicz M, Dowgiałło-Wnukiewicz N, Kenig J, Stefura T, Walędziak M, Pędziwiatr M; Pol-LA (Polish Laparoscopic Appendectomy) Collaborative Study Group. Comparison of stump closure techniques during laparoscopic appendectomies for complicated appendicitis - results from Pol-LA (Polish laparoscopic appendectomy) multicenter large cohort study. Acta Chir Belg. 2020;120:116-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 49. | Ceresoli M, Tamini N, Gianotti L, Braga M, Nespoli L. Are endoscopic loop ties safe even in complicated acute appendicitis? Int J Surg. 2019;68:40-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 50. | Makaram N, Knight SR, Ibrahim A, Patil P, Wilson MSJ. Closure of the appendiceal stump in laparoscopic appendectomy: A systematic review of the literature. Ann Med Surg (Lond). 2020;57:228-235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 51. | Durán Muñoz-Cruzado V, Anguiano-Diaz G, Tallón Aguilar L, Tinoco González J, Sánchez Arteaga A, Aparicio Sánchez D, Pareja Ciuró F, Padillo Ruiz J. Is the use of endoloops safe and efficient for the closure of the appendicular stump in complicated and uncomplicated acute appendicitis? Langenbecks Arch Surg. 2021;406:1581-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 52. | Ihnát P, Tesař M, Tulinský L, Ihnát Rudinská L, Okantey O, Durdík Š. A randomized clinical trial of technical modifications of appendix stump closure during laparoscopic appendectomy for uncomplicated acute appendicitis. BMC Surg. 2021;21:272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 53. | White C, Hardman C, Parikh P, Ekeh AP. Endostapler vs Endoloop closure of the appendiceal stump in laparoscopic appendectomy: Which has better outcomes? Am J Surg. 2021;222:413-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 54. | GlobalSurg Collaborative. Laparoscopy in management of appendicitis in high-, middle-, and low-income countries: a multicenter, prospective, cohort study. Surg Endosc. 2018;32:3450-3466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 55. | Garst GC, Moore EE, Banerjee MN, Leopold DK, Burlew CC, Bensard DD, Biffl WL, Barnett CC, Johnson JL, Sauaia A. Acute appendicitis: a disease severity score for the acute care surgeon. J Trauma Acute Care Surg. 2013;74:32-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 56. | Kim HC, Yang DM, Lee CM, Jin W, Nam DH, Song JY, Kim JY. Acute appendicitis: relationships between CT-determined severities and serum white blood cell counts and C-reactive protein levels. Br J Radiol. 2011;84:1115-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |