INTRODUCTION
Diabetes mellitus (DM) poses a substantial global health threat because of the high prevalence with different etiologies and increased risk of mortality[1]. This metabolic disorder’s hallmarks are chronic hyperglycemia, hyperlipidemia, and insulin resistance, contributing to macrovascular and microvascular events[2]. Atherosclerotic cardiovascular disease is a prominent global cause of morbidity and mortality, with approximately 70% to 80% of deaths in individuals with diabetes attributed to vascular disorders[3]. Other serious diabetic complications may damage many vital organs, which can result in more severe and irreversible pathological illnesses, including nephropathy, retinopathy, vasculopathy, neuropathy, cardiovascular diseases, and hepatopathy[4].
The hyperglycemic state leads to complications, especially atherosclerotic cardiovascular disease, by affecting lipoproteins, vascular matrix components, and cellular metabolism. This results in the excessive formation of free radicals due to glucose autoxidation and non-enzymatic protein glycation[5]. Over time, it damages cellular organelles and enzymes, leading to increased lipid peroxidation[6]. A complete understanding of the precise mechanisms underlying oxidative stress in diabetes requires further exploration, which may involve multiple pathways. In diabetes, antioxidant defenses are compromised, and free radical and reactive oxygen species (ROS) levels are elevated, suggesting the potential antioxidant supplements[7]. Various ROS, originating mainly from mitochondrial electron transport chains, cause damage to vascular endothelial cells, disrupt junctions, and increase permeability, which in turn accelerates microvascular disease progression[8].
Despite advances in DM research, insights into its etiology, effects, and progression, and developments in insulin and its analogs, optimal glycemic control remains challenging. For patients with type 2 DM (T2DM), lifestyle modifications like diet and exercise are important, yet they are challenging to follow consistently[9]. There are currently two existing primary treatment protocols for T2DM: Injections of insulin or insulin-like peptides and oral administration of hypoglycemic agents. Although these therapies are essential for the treatment of T2DM, they also bear adverse effects[10]. For instance, several prescribed medications, such as metformin (MET), sulfonylureas, GLP-1 receptor agonists, and SGLT2 inhibitors, are involved with gastrointestinal issues, risk of hypoglycemia, weight gain, and increased susceptibility to infection[11]. Aside from this, these medications can become less effective over time as the disease progresses, necessitating the need for dose adjustments or combination therapy, which complicates treatment regimens and, in turn, leads to poor adherence. Additionally, MET has been a standard treatment for T2DM due to its remarkable ability to lower plasma glucose levels[12]. Despite this, MET suffers from the lowest compliance of all oral antidiabetic medications due to minor to severe adverse effects that impair patient compliance. While MET controls diabetes and provides hepatoprotection, patients are still experiencing liver-related complications, necessitating a more effective therapeutic option[13].
Taurine (TAU), a semi-essential amino acid relatively abundant in the brain, the heart, and muscles, is active in several cellular processes and has anti-inflammatory and antioxidant properties[14,15]. Regarding health benefits, TAU controls glucose and lipid metabolism, promotes energy metabolism, and reduces inflammation while acting as an antioxidant by acting as a ROS scavenger[16]. TAU depletion causes numerous pathological changes, including severe cardiomyopathy, renal and pancreatic ailments, as well as loss of retinal photoreceptors. The use of TAU supplements has shown promise in preventing complications of diabetes, including endothelial dysfunction, nephropathy, retinopathy, and cardiomyopathy[17].
Earlier studies have demonstrated TAU's critical role in endocrine pancreas development and insulin production and secretion. A diet containing TAU was found to increase pancreatic islet mass while simultaneously reducing beta cell apoptosis, suggesting it protects beta cells from damage[18]. TAU also mitigates the effects of cytokine-induced apoptosis in pancreatic beta cells, which suggests it could be beneficial to the anti-inflammatory processes associated with autoimmune diabetes[19]. Considering TAU's potential for preventing or alleviating diabetes, particularly in early life stages, further research into its role in improving pancreatic function and mitigating diabetic complications is necessary. Taking into account the negative aspects, numerous studies have been conducted on the effects of high TAU intake but have not reported serious adverse effects[20,21]. There could be potential unwanted effects of TAU on the nervous system, cardiovascular system, and muscle emerging from its activity in regulating calcium release[22]. Despite that, TAU appears to be safe for humans at doses as high as 10 g/day for six months[23]. However, as with any dietary supplement, TAU should be consumed moderately. When TAU is overconsumed, side effects may arise as nausea, vomiting, diarrhea, dizziness, tremors, and headache[24]. Furthermore, caution must be exercised due to the potential interactions between TAU and cardiovascular and nervous system drugs, which may exacerbate the effects of such treatments and increase the risk of hypotension[25], altered heart rhythms, or neurological concerns[26].
In addition, cholecalciferol (CHO), the major form of vitamin D in humans, plays a significant role in bone health by increasing intestinal absorption of calcium, magnesium, and phosphate[27]. Aside from promoting bone health, research suggests that CHO also possesses anti-inflammatory and antioxidant properties[28]. This antioxidant role is relevant in insulin resistance and diabetes, where oxidative stress has been linked to their related complications[29]. Supplementation with CHO is unlikely to cause severe adverse reactions, even at high doses[30]. The excessive intake of this nutrient, on the other hand, may lead to hypercalcemia, which may cause calcium deposits in soft tissues or lead to kidney stones and cardiovascular complications[31,32]. Moreover, hypercalcemia can be exacerbated by CHO in individuals with high calcium levels, as well as hypertensive patients on thiazide diuretics[33]. In this regard, blood calcium levels are advised to be monitored to prevent CHO toxicity.
The current study aimed to determine if CHO and TAU supplements could enhance MET’s effectiveness in treating diabetes while minimizing the associated pathological risks, including hepatitis, dyslipidemia, and oxidative stress tissue damage. If so, it may be possible to anticipate improvements in patient compliance with MET.
MATERIALS AND METHODS
Chemicals
CHO (Vidrop®) was purchased from Medical Union Pharmaceuticals (MUP, Ismailia, Egypt). MET (Cidophage®) was obtained from Chemical Industries Development Co. (CID; Giza, Egypt). TAU powder was obtained from BDH Chemicals Ltd. (Poole, Dorset, United Kingdom). Streptozotocin (STZ) was purchased from Sigma-Aldrich Chemical Corporation (St Louis, MO, United States). Assay kits for antioxidant and oxidative biomarkers [superoxide dismutase (SOD), catalase (CAT), and malondialdehyde (MDA)] as well as low-density lipoprotein cholesterol (LDL-C) assay kit were purchased from Biodiagnostic Co. (Dokki, Giza, Egypt). Kit for serum glucose, triglyceride, and high-density lipoprotein cholesterol (HDL-C) were obtained from BioMed Diagnostics (EGY-CHEM for lab technology, Badr city, Egypt).
Animals and experimental design
The animal study was conducted under the guiding principle for the care and use of research animals reviewed and approved by the ZU-IACUC committee, with ethical sanction number ZU-IACUC/2/F/47/2022. Initially, the experiment started with 75 healthy male albino rats (Sprague Dawley) weighing approximately 200-250 gm. Rats were obtained from the animal house at the Faculty of Veterinary Medicine of Zagazig University, where animals were kept in cages under standard conditions of temperatures around 20-25 ℃ with proper ventilation during light and dark cycles. Rats were left to acclimatize for one week before the experiment, during which they were fed with rat normal pellet diet (kcal percentage from fat approximately 12%) and tap water before they were simply randomized into two main groups, namely:
Non-diabetic group (control): Ten healthy adult albino rats were intraperitoneally injected with a single dose of citrate buffer solution (0.1 mmol/L) and continued their normal diet.
Diabetic group: The rats were fed a high-fat diet containing an approximate kcal percentage of 58% fat, 25% protein, and 17% carbohydrates for four weeks before receiving a single intraperitoneal dose of STZ (45 mg/kg) dissolved in sodium citrate buffer as described in previous studies[34,35]. Rats were fed fructose solution 20% (w/v) directly after receiving STZ to prevent hypoglycemia. MET and the proposed supplements were administered to rats on the third day following T2DM induction. Prior to the onset of diabetes, blood glucose levels were assessed, and thereafter, weekly monitoring for six weeks was carried out using a glucometer (GlucoDrTM, All Medicus Co. Ltd, Gyeonggi, Korea). Induction of diabetes was confirmed two days following STZ administration. Fifty rats were deemed diabetic whose blood-glucose levels exceeded 250 mg/dL and were selected for further investigation. This group was further randomly subdivided into five subgroups of ten diabetic rats treated for six weeks each, as follows: (1) STZ group: Rats served as the non-treated diabetic group after experimental induction of diabetes; (2) MET-treated group: Diabetic rats received a daily dose of MET (250 mg/kg) for six weeks, administered orally using a metallic stomach tube[36]; (3) TAU + MET-treated group: A combination of TAU (100 mg/kg) and MET (250 mg/kg) was orally co-administered daily to diabetic rats[37]; (4) CHO + MET-treated group: A combination of CHO (7500 IU/kg) and (250 mg/ kg) of MET were orally co-administered daily to diabetic rats[38]; and (5) TAU + CHO + MET-treated group: A mixture of CHO (7500 IU/kg), TAU (100 mg/kg), and (250 mg/ kg) of MET was orally co-administered daily to diabetic rats.
Blood collection
Upon completing the ten-week experiment, rats were fasted for 12 hours and then sedated with ketamine-xylazine, and blood samples were collected by orbital puncture using heparinized microhematocrit capillary tubes. Two blood samples were taken from each rat to evaluate oxidative stress markers and biochemical parameters. The first was collected in a clean tube with anticoagulant (EDTA), then centrifuged to separate plasma for measuring glycated hemoglobin (HbA1c). The serum collected from the second sample was used for further biochemical analysis.
Biochemical analysis
As described by Ng et al[39], blood glycated hemoglobin (HbA1c%) levels were measured using an immunoassay kit (ELISA; Cusabio, Houston, TX, United States). Serum glucose levels were measured using the BioMed Diagnostic kits following the method described by Young et al[40]. In rat serum, insulin levels were measured using a radioimmunoassay kit (insulin-I125 kit, Radio Assay System Laboratories Inc., England) as outlined by Woodhead et al[41]. The obtained glucose and insulin data were used to calculate the Homeostasis Model Assessment of Insulin Resistance (HOMA-IR), a measure of insulin resistance and beta cell function, using the following equation[42].
HOMA-IR = Serum insulin (µIU/mL) × serum glucose (mg/dL)/405.
Serum HDL-C levels were determined following the method by Castelli et al[43] (1977) using the BioMed HDL-C-cholesterol kit. Moreover, LDL-C-cholesterol was measured using a perciptation assay kit according to the manufacturer’s (Biodiagnostics) instructions. Furthermore, serum triglyceride levels were determined by enzyme colorimetry using the BioMed kit, whereas the colorimetric kit (Spinreact, Santa Coloma, Girona, Spain) was used to assess serum cholesterol levels following the manufacturer's instructions. Consequently, very-low-density lipoprotein cholesterol (VLDL-C) was determined according to Friedewald equation: VLDL-C = TG/5.
Serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) activities were measured using the kinetic UV KIT (EliTech group Clinical Systems, Seppim SAS, Sées, France), while serum lactate dehydrogenase (LDH) activity was determined using the kinetic UV assay kit (Spectrum Diagnostics, Cairo, Egypt) according to Young[44]. Additionally, SOD activity was evaluated using the commercially available Biodiagnostic kit, following Nishikimi et al[45]. The analysis of CAT activity was performed using Aebi's method[46]. In addition, MDA levels were determined using the colorimetric end-point kit, following the Ohkawa method[47].
Tissue collection and histological study
Following blood collection, animals were euthanized by cervical dislocation directly after receiving a high anesthetic dose. Then, the animals were dissected, and the pancreas and liver were fixed in 10% formalin for histopathological and immunohistopathological studies. After ethanol dehydration, the samples were prepared as a paraffin block. A thin section of the paraffin block was stained with hematoxylin and eosin (H&E) and then observed under the microscope (Amscope) for detailed information about the tissue. Photomicrographs were captured at different magnifications 100 × and 400 ×.
Immunohistochemistry was conducted according to the standard procedures. Tissue sections were subjected to routine microwave treatment to distinguish antigen epitopes[48]. Immunostaining is a two-step process: Initially, the primary antibody binds to the related antigen, followed by interaction with a specific secondary antibody carrying an amplifying enzyme system to visualize this reaction. The Biotin-Streptavidin system was used to visualize the markers, whereas diaminobenzidine was used as a permanent chromogen[49]. Counterstaining was carried out with hematoxylin. Photomicrographs were captured at different magnifications 40 × and 400 ×. Fiji software was used to analyze the stain intensity, as well as number, and size of the stained islets per 40 × field[50]. In order to evaluate stain intensity, images of test groups were first deconvoluted, inverted, then analyzed, and compared with control measurements.
Statistical analysis
Data analyses were conducted using the SPSS for Windows, version 26 software. SPSS was used to perform the normality test, and parametric tests were conducted on the normally distributed data. Data were analyzed by ANOVA except for baseline-corrected blood glucose changes, which were analyzed by repeated-measures two-way analysis of variance and compared by Tukey’s test. The results’ significance was tested at a P value of ≤ 0.05, and the data were expressed as mean ± standard error. The graphs were created with the aid of GraphPad Prism 9.
RESULTS
Changes in blood glucose levels
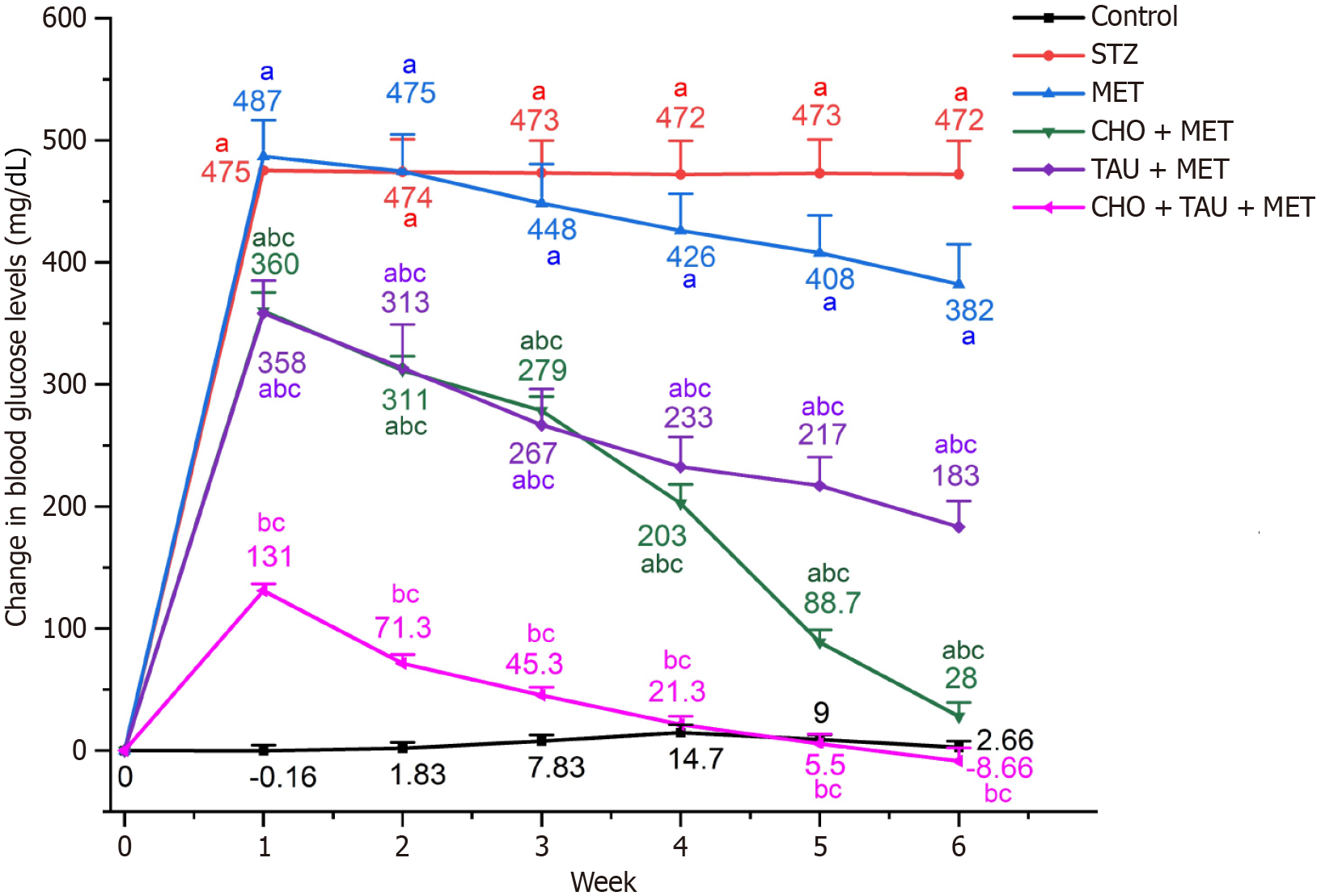
Blood glucose levels were sequentially recorded from the first to the sixth week of the experiment, and changes were then calculated by comparing them with the initial measurements. Changes in blood glucose levels among the STZ group were significantly greater than the control group. Compared to the STZ group, the MET-treated group showed no significant changes until the sixth week, when their glucose level decreased significantly. Meanwhile, glucose levels decreased significantly in the three treated groups, CHO + MET, TAU + MET, and CHO + TAU + MET, during the six-week experiment compared to STZ and MET groups. Eventually, the glucose level in the CHO + TAU + MET group decreased significantly, reaching a level close to normal.
Serum glucose, insulin, HOMA-IR levels, and HbA1c%
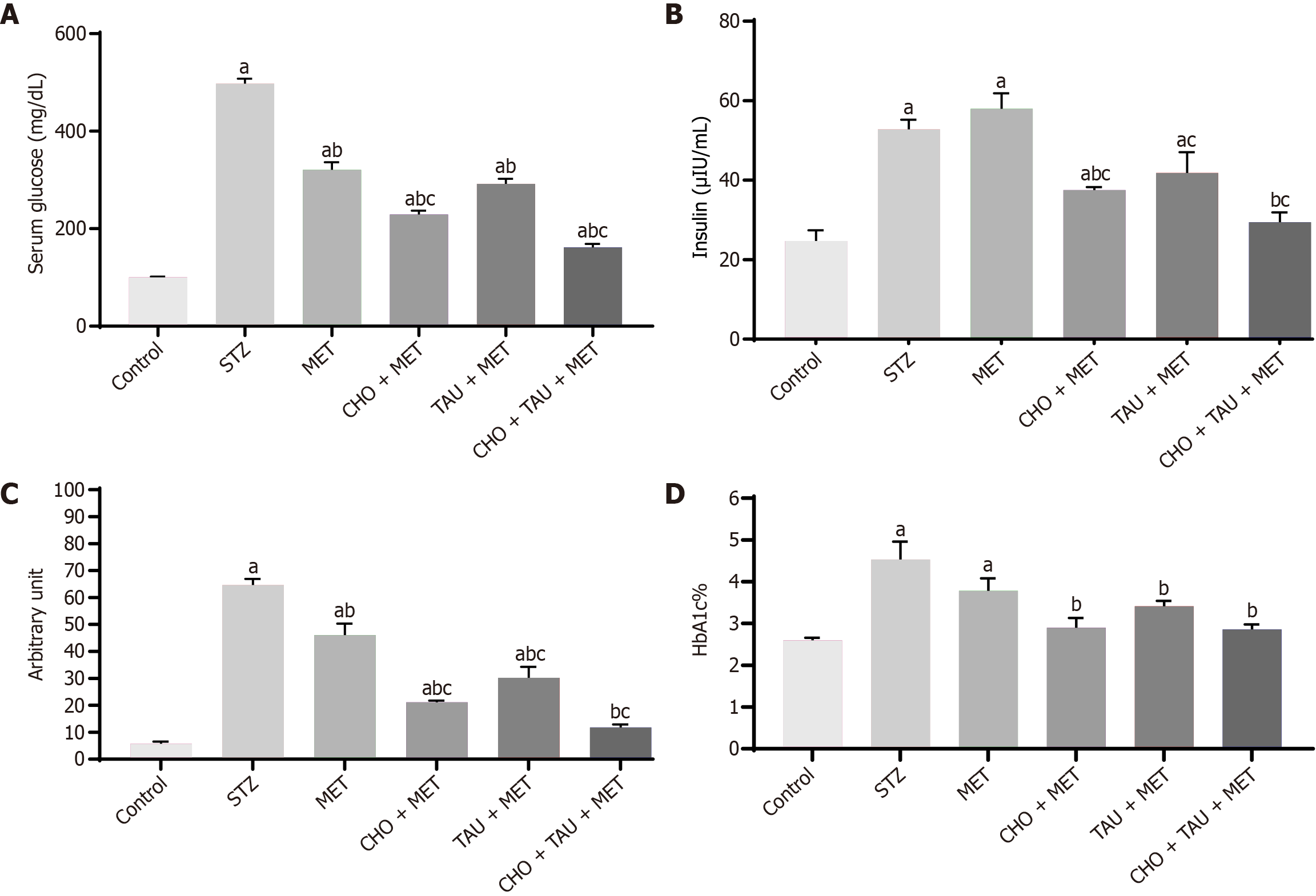
As shown in Figure 1, the STZ group showed significant increases in serum glucose, insulin, HOMA-IR, and HbA1c% compared with the control group. Yet, serum insulin levels in the MET group did not differ significantly from those in the STZ group, whereas serum glucose and HOMA-IR levels declined significantly. A pronounced reduction in serum glucose and insulin levels occurred in the CHO + MET-treated group compared with the STZ and MET groups. Although serum glucose and insulin levels were significantly lower in the TAU + MET-treated group than in the STZ group, they were comparable to the MET-treatment group. The combined treatment of CHO, TAU, and MET resulted in a significant 1.98-fold decrease in serum glucose levels compared to the MET-treated group. The HOMA-IR level receiving a single TAU or CHO-treated group supplement declined significantly compared to the STZ and MET groups. The combined use of CHO, TAU, and MET significantly reduced insulin and HOMA-IR levels by 1.97-fold and 3.91-fold, respectively, vs MET alone.
Figure 1 Changes in blood glucose levels in the control and experimental groups.
STZ: Streptozotocin; MET: Metformin; CHO: Cholecalciferol; TAU: Taurine. aSignificance compared to the control group. bSignificance compared to the Streptozotocin diabetic group. CSignificance compared to the metformin-treated group.
Moreover, the HOMA-IR level for this group was comparable to the control group. MET treatment did not exert any significant difference from the diabetic control. Compared to the STZ group, there was a significant difference in HbA1c% between the supplemented MET-treated groups. With the abovementioned combination, HbA1c% significantly declined by 1.58 times concerning STZ-induced diabetics.
Lipid profile
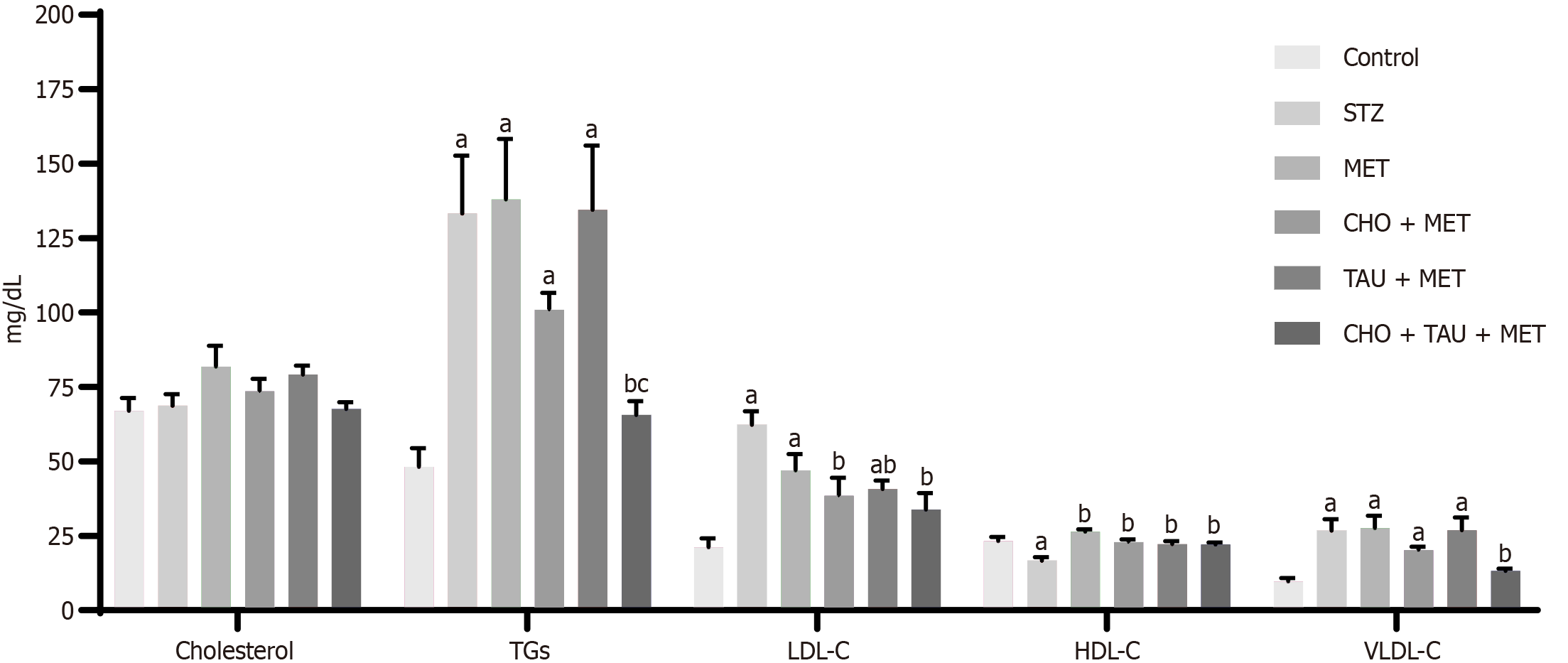
As can be observed in Figure 2, untreated diabetic rats did not demonstrate any significant differences in serum cholesterol levels compared to the control group. Similarly, none of the treated groups showed significant changes in serum cholesterol levels compared to the STZ group. In the meantime, the STZ group showed a significant increase in triglycerides (TGs), LDL-C, and VLDL-C levels and a significant decline in HDL-C levels compared with the control group. HDL-C levels increased significantly in all treated rats relative to STZ but failed to reveal significance compared to the MET-treated group.
Figure 2 Assessment of glycemic profiles.
A-D: Measurement of serum glucose level (A), insulin level (B), Homeostasis Model Assessment of Insulin Resistance levels (C), glycated hemoglobin% (D) in the control group and other experimental groups. The data, presented as means ± SE (n = 6), indicate significant differences at P < 0.05. STZ: Streptozotocin; MET: Metformin; CHO: Cholecalciferol; TAU: Taurine; HbA1c: Glycated hemoglobin. aSignificance compared to the control group. bSignificance compared to the Streptozotocin diabetic group. cSignificance compared to the metformin-treated group.
Neither TAU nor CHO alone nor their combination showed any significant difference in VLDL-C levels compared to MET-treated groups. Compared to the sole MET treatment, there were non-significant differences in TG levels except for TAU and CHO co-treatment, which showed a significant drop in TG levels. Also, neither the MET, CHO + MET, or TAU + MET-treated groups exhibited any significant differences in TGs or VLDL-C levels from the STZ group. However, compared to the STZ group, the CHO + TAU + MET group showed significant declines in TG and VLDL-C levels.
Although the MET-treated group alone failed to demonstrate a significant change in LDL-C levels compared with the STZ group when TAU or CHO were used alone or in combination, a significant reduction in LDL-C levels was observed. Meanwhile, comparing the three treated groups with the MET-treated group showed no significant differences in LDL-C levels.
Serum aminotransferase enzymes (AST, ALT) and LDH activities
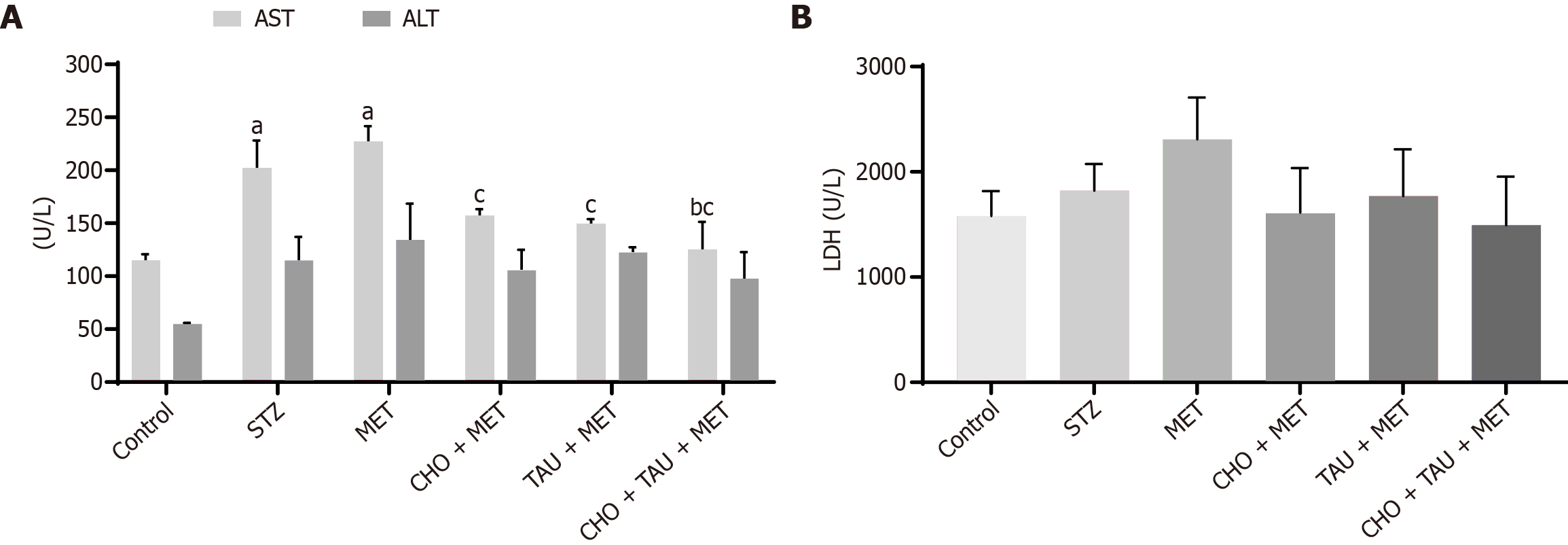
Figure 3 shows a significant increase in AST levels among the STZ group in comparison to the control group. Meanwhile, neither the MET, the CHO + MET, nor the TAU + MET groups showed significant differences in AST levels from the STZ group. Conversely, the AST level decreased significantly following the coadministration of CHO, TAU, and MET compared to both STZ and MET-treated groups. All experimental groups had no statistically significant changes in ALT and LDH levels.
Figure 3 Lipid markers measurements in the control group and other experimental groups.
The data, presented as means ± SE (n = 6), indicate significant differences at P < 0.05. STZ: Streptozotocin; MET: Metformin; CHO: Cholecalciferol; TAU: Taurine; TGs: Triglycerides; LDL-C: Low-density lipoprotein cholesterol; HDL-C: High-density lipoprotein cholesterol; VLVL-C: Very low-density lipoprotein cholesterol. aSignificance compared to the control group. bSignificance compared to the Streptozotocin diabetic group. cSignificance compared to the metformin-treated group.
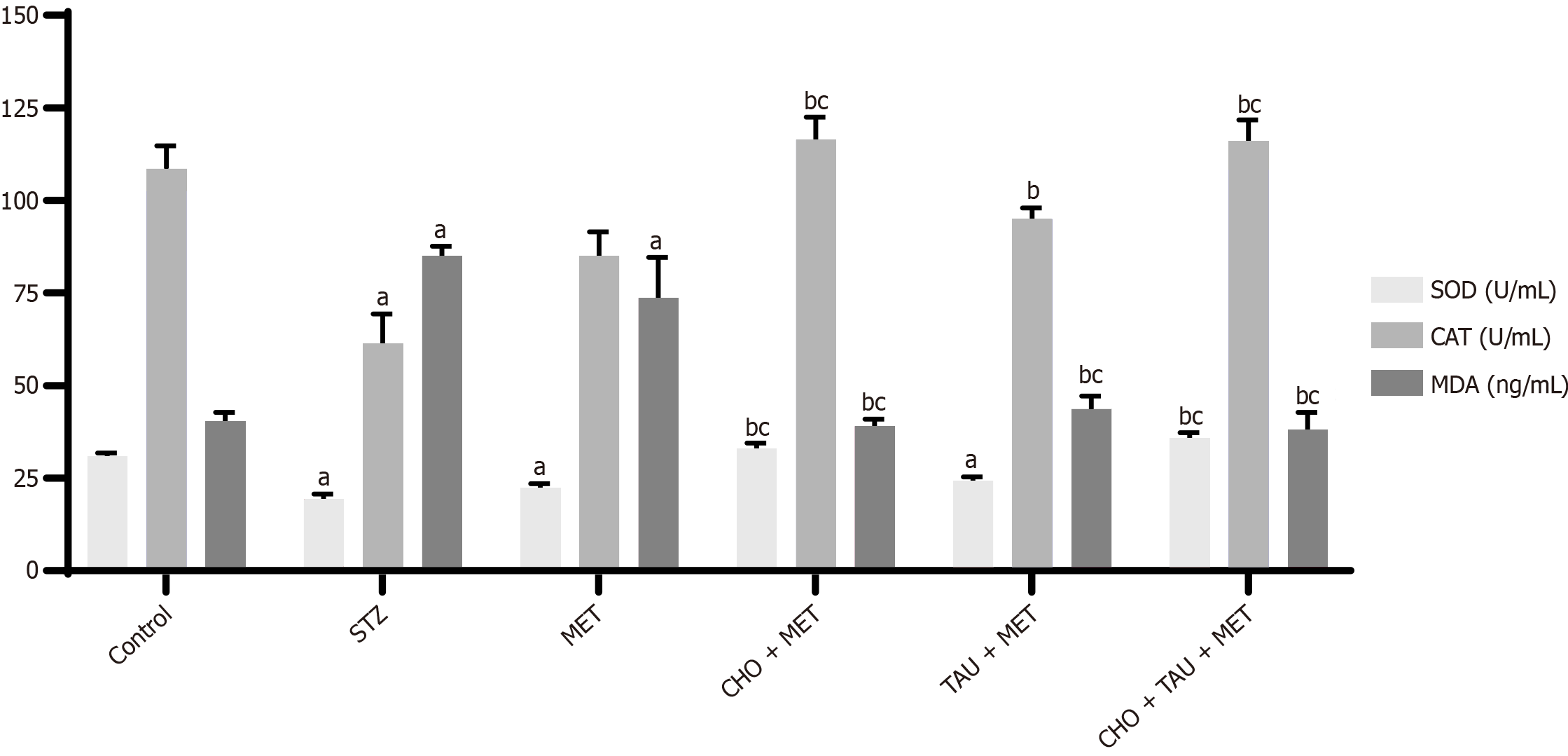
Antioxidants and oxidative stress markers
In the STZ group, the activity of antioxidant markers (SOD and CAT) was significantly decreased compared to the control group, as presented in Figure 4, whereas there was a significant increase in oxidative stress marker (MDA) level. In contrast, the MET-treated group did not exhibit significant differences in SOD, CAT, and MDA levels when compared to the STZ group. Meanwhile, the daily intake of CHO + MET and CHO + TAU + MET significantly ameliorated the reduction of SOD and CAT levels while increasing the MDA level as compared to the STZ group, reaching near to normal estimates and slightly better than the control group.
Figure 4 Measurement of liver enzymes.
A and B: Serum aminotransferase enzymes (aspartate aminotransferase, alanine aminotransferase; A) and Serum lactate dehydrogenase (LDH; B) levels in the control group and other experimental groups. The data, presented as means ± SE (n = 6), indicate significant differences at P < 0.05. STZ: Streptozotocin; MET: Metformin; CHO: Cholecalciferol; TAU: Taurine; TGs: Triglycerides; LDH: Lactate dehydrogenase; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase. aSignificance compared to the control group. bSignificance compared to the Streptozotocin diabetic group. cSignificance compared to the metformin-treated group.
Histopathology
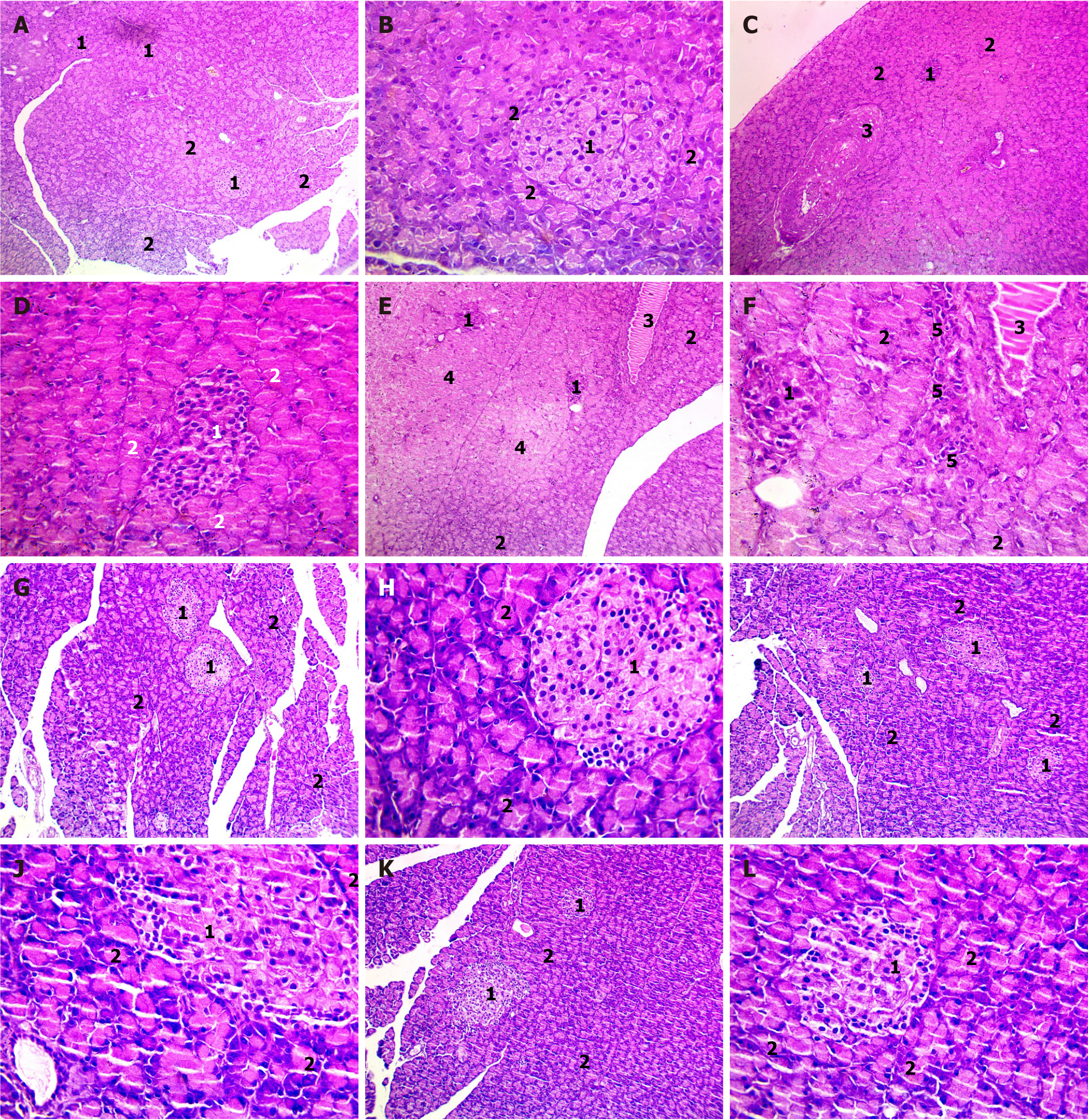
Histopathology of pancreatic sections: In the control group, the pancreatic tissue exhibited well-defined normal islets of Langerhans with granulated cytoplasm and a regular lining of acinar cells around the islets (Figure 5A and B). However, the untreated diabetic rats displayed a marked reduction in the sizes of islets, the irregular acinar cell lining around the islets, and a notably thickened blood vessel (Figure 5C and D). Treatment with MET in diabetic rats reduced islet size, degenerative changes in acinar cells, and perivascular inflammation (Figure 5E and F). Conversely, MET-treated diabetic rats that received CHO had restored islet structure (Figure 5G and H), while the combination of TAU showed a similar effect but without inflammation (Figure 5I and J). In the meantime, the coadministration of CHO and TAU to the MET-treated diabetic rats showed a slightly increased size of islets surrounded by acinar cells (Figure 5K and L).
Figure 5 Measurement of antioxidant biomarkers in the control group and other experimental animals.
The data, presented as means ± SE (n = 6), indicate significant differences at P < 0.05. STZ: Streptozotocin; MET: Metformin; CHO: Cholecalciferol; TAU: Taurine; SOD: Superoxide dismutase; CAT: Catalase; MDA: Malondialdehyde. aSignificance compared to the control group. bSignificance compared to the Streptozotocin diabetic group. cSignificance compared to the metformin-treated group.
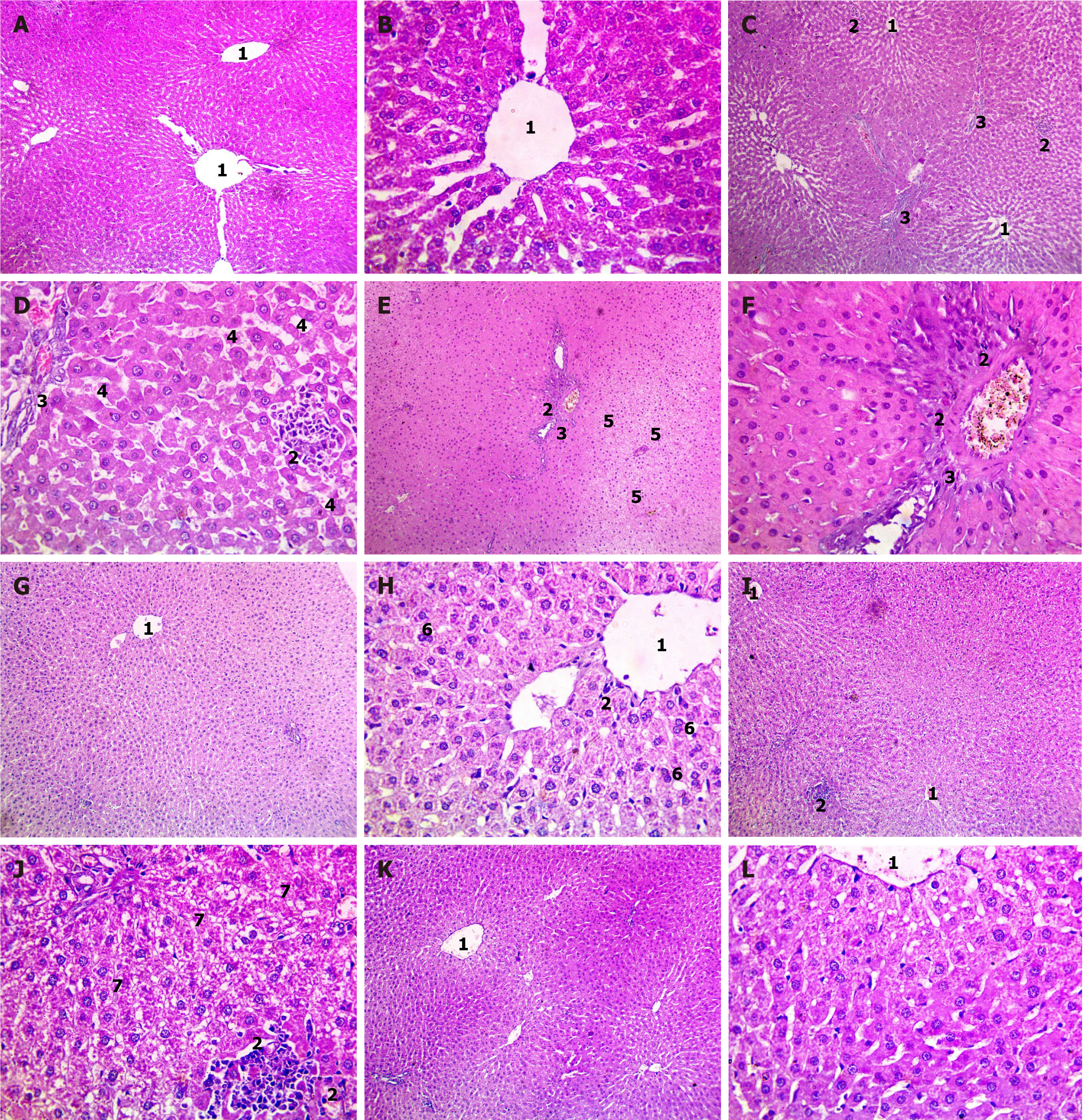
Histopathology of liver sections: The histopathological examination of rat liver sections stained with H&E revealed distinct features in each experimental group. In the control group, the liver exhibited normal morphology. In contrast, in the STZ group, there were signs of lobular inflammation (Figure 6A and B), fibrous portal expansion, sinusoidal dilatation, and hydropic degeneration of hepatocytes with areas of necrosis (Figure 6C and D). Treatment with MET partially mitigated these effects, showing hydropic degeneration of hepatocytes with necrotic regions (denoted by lost nuclei) with congested central veins and lobular inflammation but no fibrosis (Figure 6E and F). The CHO + MET-treated group displayed preserved hepatocyte arrangement with binucleation of some hepatocytes and mild lobular inflammation (Figure 6G and H). In contrast, TAU supplementation showed hydropic degeneration of hepatocytes with areas of necrosis with lobular inflammation (Figure 6I and J). The supplementation of CHO and TAU in the MET-treated group exhibited preserved hepatocyte arrangement with minimal signs of inflammation and fibrosis (Figure 6K and L).
Figure 6 Examination of histopathological changes in rat pancreatic sections using HandE staining.
A-I: Photomicrographs of different magnifications showing pancreatic sections of control group (A and B), Streptozotocin diabetic group (C and D), metformin (MET)-treated group (E and F), cholecalciferol (CHO) + MET-treated group (G and H), taurine (TAU) + MET-treated group (I and J), and TAU + CHO + MET-treated group (K and L). 1Normal structure of the islet of Langerhans. 2Normal structure of acinar cells. 3Normal structure of a thickened blood vessel. 4Normal structure of areas of degenerative changes in acinar cells. 5Normal structure of perivascular inflammation.
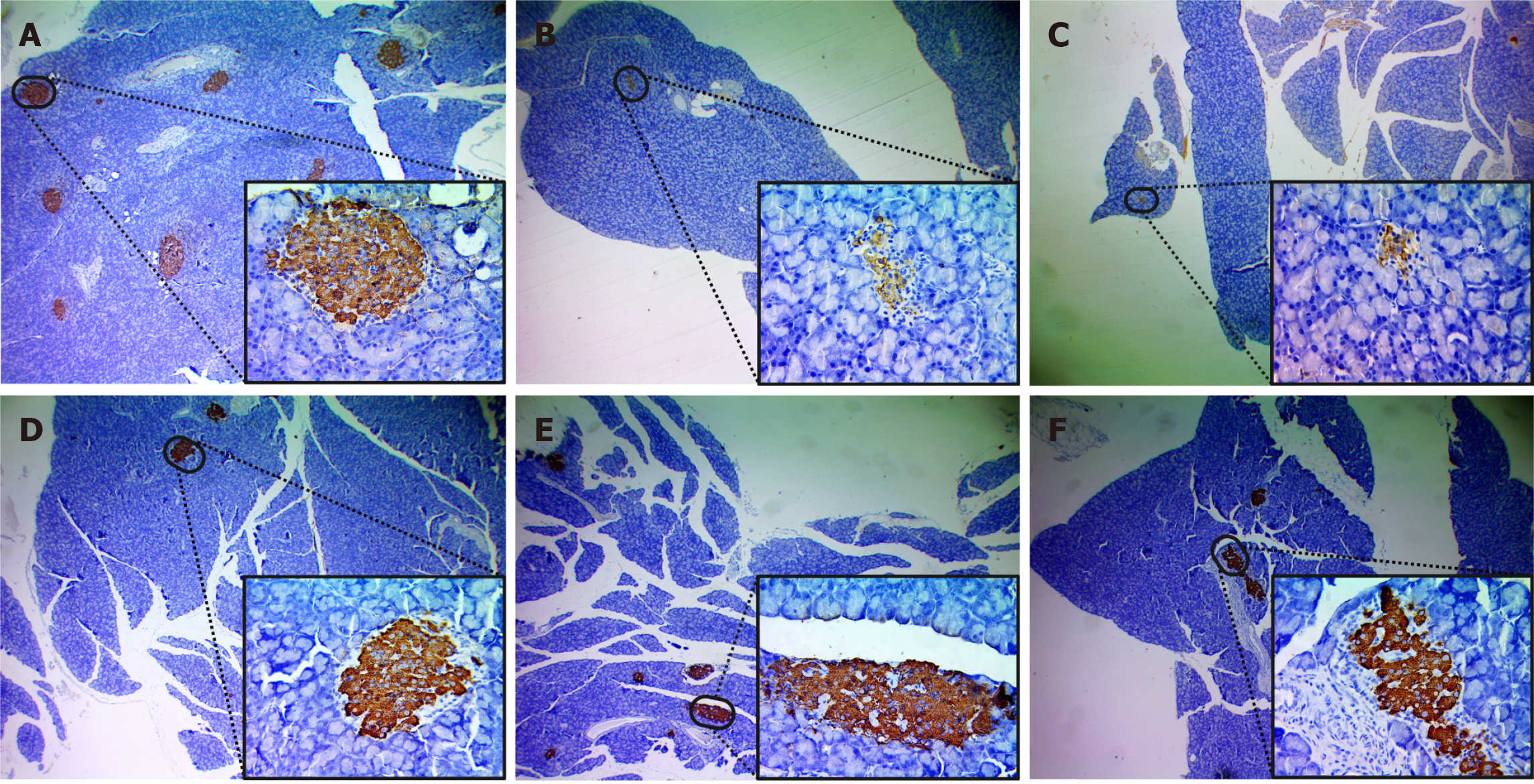
Immunohistochemical observations
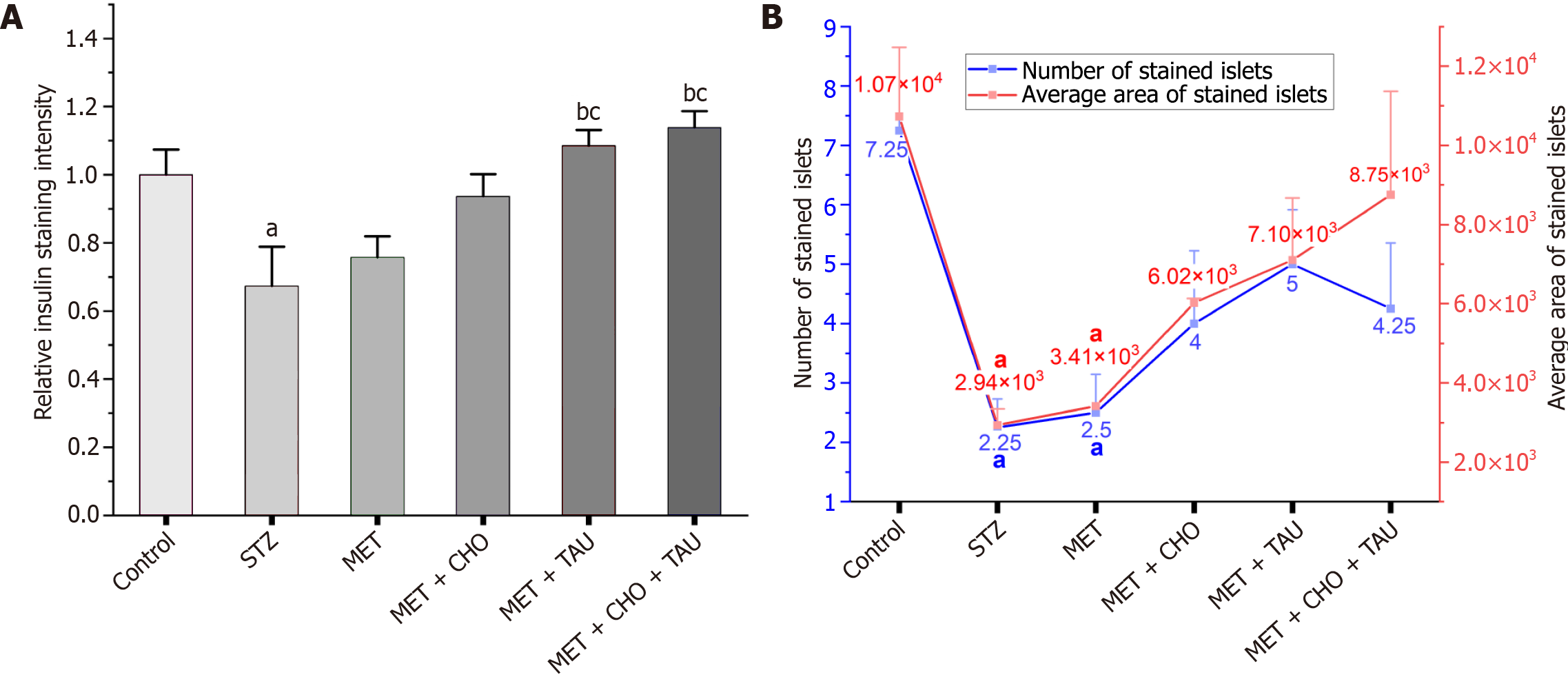
As can be seen in Figure 7A, the control group contains a well-defined typical Langerhans islet with positive insulin staining, surrounded by acinar cells with negative insulin staining. Comparatively, STZ diabetic rats showed decreased positive (brown) and very weak insulin staining in their islets and markedly decreased mass of their islets (Figure 7B). Also, in the MET-treated group, weak insulin staining of the islets with a marked decrease in islet mass was observed, which was relatively higher than in the STZ group (Figure 7C). The CHO + MET-treated group showed a significant restoration of insulin staining on the islet, whereas treatment with TAU and CHO + TAU groups (Figure 7D) exhibited a more substantial recovery of staining intensity with increased area and number of stained islets (Figure 7E and F).
Figure 7 Examination of histopathological changes in rat liver sections using HE staining.
Photomicrographs of different magnifications showing pancreatic sections of the control group (A and B), Streptozotocin diabetic group (C and D), metformin (MET)-treated group (E and F), cholecalciferol (CHO) + MET-treated group (G and H), taurine (TAU) + MET-treated group (I and J), and TAU + CHO + MET-treated group (K and L). 1The central vein. 2Lobular inflammation. 3Fibrous portal expansion. 4Sinusoidal dilatation. 5Hydropic degeneration. 6Preserved hepatocyte arrangement with binucleation of some hepatocytes. 7Hydropic degeneration of hepatocytes with areas of necrosis indicated by lost nuclei.
In comparison with the control, the relative stain intensity was reduced by 32.7 and 24.3% in the STZ and MET groups, respectively (Figure 8A). Also, the number and size of islets were significantly lower than those of the control group (Figure 8B). Meanwhile, TAU exerted prominent restoration of insulin staining of the islets with restored and enhanced islets staining intensity with regular outlining comparable to control (Figure 8A). Also, the number of stained islets was increased to 5 stained areas per field, whereas the area was increased to (7102 µm2). Eventually, rats supplemented with CHO and TAU experienced a significant rise in relative insulin stain intensity by 13.8% (Figure 8A), with greater stained islet size (8747 µm2; Figure 8B).
Figure 8 Photomicrographs from immunohistochemistry assays of insulin staining for the pancreas in the six study groups at a Magnification power of × 400.
A: Control group; B: Streptozotocin group; C: metformin (MET)-treated group; D: Cholecalciferol (CHO)+ MET- treated group; E: Taurine (TAU)+ MET- treated group; F: CHO + TAU + MET-treated group. The brown color indicates positive insulin staining (diaminobenzidine).
DISCUSSION
T2DM exhibits a progressive nature with evolving pathological implications over time. Initial monotherapy becomes less effective, thereby requiring combination therapy for efficient management[51]. While several studies have introduced the beneficial effects of dietary supplements (TAU, CHO)[18,29], our study specifically aimed to explore their synergistic effects in enhancing the effectiveness of MET for T2DM treatment.
To experimentally validate the induction of T2DM, the group treated with STZ demonstrated a notable and significant rise in the mean random blood glucose levels throughout the six-week experiment. This increase was observed in comparison to the control non-diabetic group. Further evidence supporting these findings comes from histological examination, through which T2DM was evident by the cytotoxic effects of STZ on pancreatic β-cells.
Nevertheless, the proposed treatment groups exhibited a significant reduction in mean random blood glucose compared to the STZ and MET-treated groups throughout the experimental period. As seen in Figure 9, both su-pplements exerted an effect alone in counteracting the STZ impact on the glycemic profile. The effect of CHO on blood glucose was prominent and was in alignment with a previous report by Santos and Vianna, who reported the administration of 12.5 μg/kg−1 of CHO to Wistar rats led to a reduction of 40% in blood glucose[52]. Also, Yousefi Rad et al[53] have reported the beneficial effect of CHO on the control of blood glucose levels as well as insulin resistance in T2DM patients. This could be attributed to the stimulating effect of CHO on insulin receptors in beta cells, leading to insulin gene expression, as well as its role in promoting intestinal transport of glucose molecules[54]. Aside from this, calcitriol, the active form of CHO, participates in calcium absorption, an essential step in insulin release from beta cells[55].
Figure 9 Analysis of immunohistochemical results.
A: The relative islet staining intensity of stained islets; B: The number and area of the stained islets. The data, presented as means ± SE (n = 6), indicate significant differences at P < 0.05. STZ: Streptozotocin; MET: Metformin; CHO: Cholecalciferol; aSignificance compared to the control group. bSignificance compared to the Streptozotocin diabetic group. cSignificance compared to the metformin-treated group.
Additionally, TAU also influenced blood glucose levels when combined with MET. This effect was also evident in earlier preclinical studies and clinical trials. For instance, in a trial by Maleki et al[14], TAU demonstrated a significant reduction in fasting blood glucose, insulin, and HOMA-IR. The cause of this may be linked to the reported effect it has on the liver, in which it reduces the phosphorylation of the insulin receptor β subunit (IRβ) and hepatic Akt, thereby reducing glucose production as well as glucagon activity[56,57]. Also, TAU was reported to improve beta-pancreatic cell function and insulin clearance while enhancing AMPK activity in muscles that help maintain glucose hemostasis[18,58]. Also, the immunohistochemical localization of insulin antibodies supported the microscopic H and E histopathological results of pancreas tissues (Figure 8). TAU treatment prominently restored insulin staining and islet size, with regular outlining comparable to the control. These findings were in line with those of Arany et al[18], who reported the increased pancreatic islet mass in TAU-supplemented rats, which could explain the augmented stain intensity for rats co-supplemented with CHO and TAU. Eventually, TAU and CHO held great potential on the glycemic profile, and as shown in Figures 1 and 9, the synergy resulted in a significant reduction in blood glucose levels, serum insulin, HOMA-IR, and HbA1C comparable to those of non-diabetic rats.
Considering the lipid profile evaluation, it can be concluded that MET intake contributes to ameliorating STZ effects on HDL levels (Figure 2). These effects stem from control over the hyperglycemia-induced ROS generation. As a result, the formation of advanced glycation end-products is reduced, and consequently, oxidative stress and inflammation[59]. The CHO supplement, on the other hand, was the primary supplement that affected the lipid profile in a positive way, specifically through reducing LDL-C and TG. However, CHO is thought to directly reduce lecithin-cholesterol acyltransferase activity, directly influencing TGs, total cholesterol, and LDL cholesterol. Also, as it enhances calcium absorption, CHO can be indirectly implicated by impacting cholesterol absorption and hepatic bile acid conversion by decreasing fat absorption[60].
MET treatment appears to be the contributor to the reversal of STZ effects on HDL levels (Figure 2). Treatment with CHO, TAU, MET, and their combination resulted in significant improvements in levels of lipid markers, supporting Malek et al[61] and Asemi et al[62], who revealed that CHO, TAU, and MET together have therapeutic roles in modification of lipid abnormalities via lipid peroxidation prevention and reduction of the atherosclerotic inflammatory process, which in turn may help to prevent the onset of plaque and all subsequent disorders.
Elevated levels of ALT and AST in the STZ group are related to insulin resistance and fatty liver, while elevated LDH levels interfere with glucose metabolism and insulin production and play a role in increasing cytosolic free ATP and Ca2 + levels within islet beta cells[63]. These effects were exacerbated by MET treatment, which is in line with previous hepatotoxicity reports[64]. It is clear from Figure 3 that the hepatocellular necrosis induced by STZ was reversed by CHO, as evidenced by the decline in AST, ALT, and LDH levels. The findings were in accordance with those reported by Lorvand Amiri et al[65], who found that vitamin D led to a significant reduction in liver aminotransferase levels. Additionally, histopathological examination of liver tissues in the STZ diabetic group revealed lobular inflammation, sinusoidal dilatation, and fibrous portal expansion. The combination therapy (CHO + TAU + MET) demonstrated preserved hepatocyte arrangement with no inflammation or fibrosis, surpassing the effects of MET alone.
A significant part of the protective action of CHO is to enhance the activities of key antioxidant enzymes, SOD, and CAT (Figure 4). Also, CHO exerted a significant negative effect on MDA levels, which were in alignment with a meta-analysis of clinical data[66]. This can be explained by the fact that the CHO supplement interacts with Vitamin D receptors, which in turn activates the Vitamin D Response Elements in the nucleus, leading to the transcription of antioxidant genes[66]. Moreover, CHO also stimulates antioxidant pathways such as nuclear factor erythroid-2-related factor 2 (Nrf2)/Keap1[67] and ROS-scavenging enzymes (Glucose-6-phosphate dehydrogenase)[68] while reducing ROS-generating enzymes (NADPH oxidase)[69], thus indirectly reducing the risk of oxidative damage.
Despite the significance of preclinical studies, animal models offer limited predictive power[70]. This is attributed to the biological and physiological differences due to the discrepancy in how disease manifests and how treatment responds between rodents and humans. In contrast to animal models, the high genetic variation in drug metabolism and immune activity between individuals potentially affects estimates of treatment efficacy and toxicity[71]. Even so, it may still be necessary to conduct animal studies of TAU interaction prior to clinical studies to detect any potential pharmacokinetic interactions between the suggested combination therapy. Also, more parameters can be included in future glucose-insulin dynamic studies to directly assess insulin sensitivity (hyperinsulinemic-euglycemic clamp) or indirectly (glucose tolerance tests). It will, therefore, be crucial to conduct dose-finding trials to identify effective and well-tolerated dosages of CHO and TAU to minimize MET's adverse effects and optimize therapeutic outcomes in patients with diabetes. Furthermore, conducting clinical trials on diabetic patients can offer insight into the long-term benefits, safety profiles, and complications associated with the proposed co-therapy.
CONCLUSION
The study highlighted hyperglycemia, oxidative stress, and insulin resistance as contributors to pathological tissue changes and abnormal biochemical parameters in diabetic rats. MET, while possessing mild antioxidant and anti-inflammatory properties, was deemed insufficient to prevent diabetic complications. The combined therapy involving MET, CHO, and TAU proved more effective in mitigating apoptosis and ameliorating the biochemical, histological, and immunohistochemical changes associated with diabetes. This supplementation approach effectively restored these parameters to normal levels. The current study findings demonstrate the importance of a synergistic therapeutic approach to alleviating diabetes-related complications through treating oxidative stress-induced tissue damage and achieving metabolic balance.
ACKNOWLEDGEMENTS
The authors acknowledge their research institutes for the technical support.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country of origin: Egypt
Peer-review report’s classification
Scientific Quality: Grade B, Grade B, Grade B, Grade B, Grade C
Novelty: Grade A, Grade B, Grade B, Grade B
Creativity or Innovation: Grade B, Grade B, Grade B, Grade B
Scientific Significance: Grade B, Grade B, Grade B, Grade B
P-Reviewer: Alsaidan A; Papazafiropoulou A; Srinivasan AR; Wu QN S-Editor: Lin C L-Editor: A P-Editor: Zhang L