Published online Sep 15, 2010. doi: 10.4251/wjgo.v2.i9.360
Revised: March 5, 2010
Accepted: March 12, 2010
Published online: September 15, 2010
We report here on a case of duodenal metastasis from primary lung adenocarcinoma. A 69-year old man was diagnosed with primary lung adenocarcinoma. Four courses of combined chemotherapy with carboplatin and paclitaxel associated with irradiation of 60 Gy shrunk the lung tumor. However, soon after,the para-aortic lymph node became swollen. Esophagogastroduodenoscopy revealed three duodenal tumors. Differential diagnosis between malignant lymphoma and metastatic duodenal cancer was endoscopically difficult. The histology of biopsied specimens was poorly differentiated adenocarcinoma. Immunohistochemical analysis revealed a positive reaction for thyroid transcription factor-1 (TTF-1). Thus, we concluded that these were metastatic duodenal tumors from lung adenocarcinoma. Two courses of gemcitabine led to a complete remission in this duodenal metastasis and para-aortic lymph node swelling with only scarring remaining in computed tomography. He is now on the continuous generalized chemotherapy. In conclusion, duodenal metastasis from primary lung adenocarcinoma is rare and hard to diagnose. In such an instance, TTF-1 immunostaining is crucial to obtain the correct diagnosis.
- Citation: Miura T, Shimaoka Y, Nakamura J, Yamada S, Miura T, Yanagi M, Sato K, Usuda H, Emura I, Takahashi T. TTF-1 is useful for primary site determination in duodenal metastasis. World J Gastrointest Oncol 2010; 2(9): 360-363
- URL: https://www.wjgnet.com/1948-5204/full/v2/i9/360.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v2.i9.360
Common metastatic sites of lung cancer are the brain, liver, adrenal glands and bone[1]. Gastrointestinal metastasis is quite rare. On the other hand, thyroid transcription factor-1 (TTF-1) is a very useful immunohistochemical marker for determining thyroid cancer and lung cancer. We report on a case of duodenal metastasis, the primary site of which was determined correctly to be the lung by using TTF-1 immunostaining despite the total shrinkage of the primary lesion by chemotherapy.
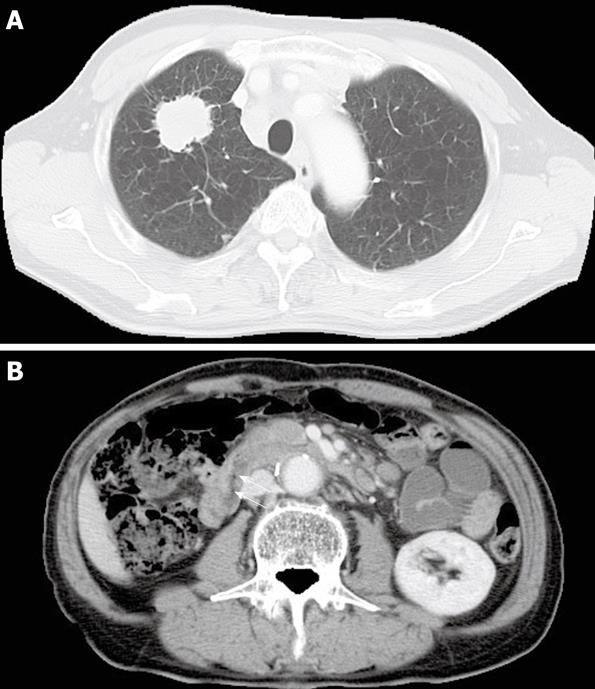
A 69-year old man was admitted to our hospital for cough and hoarseness. His past history was a right nephrectomy for renal pelvic cancer in July, 2006. Pathological examination of this cancer revealed ureteral transitional cell carcinoma, G2, pT1, lt-u0, ly0, v0. He was diagnosed as having right lung adenocarcinoma with lymph node metastasis (cT2N3M0, StageIIIb) in our respiratory unit (Figure 1A). Histology was poorly differentiated adenocarcinoma. He received combined chemotherapy with carboplatin and paclitaxel associated with the focused irradiation of 60Gy. After four courses of chemotherapy, primary lesion and lymph node metastasis were totally shrunk but, in turn, the para-aortic lymph node swelling and thickening of the duodenal walls (Figure 1B) appeared in computed tomography. Tumor markers of primary lung cancer such as CEA, SLX and CYFRA were under the normal upper limit. He had no clinical symptoms, including melena and abdominal pain.
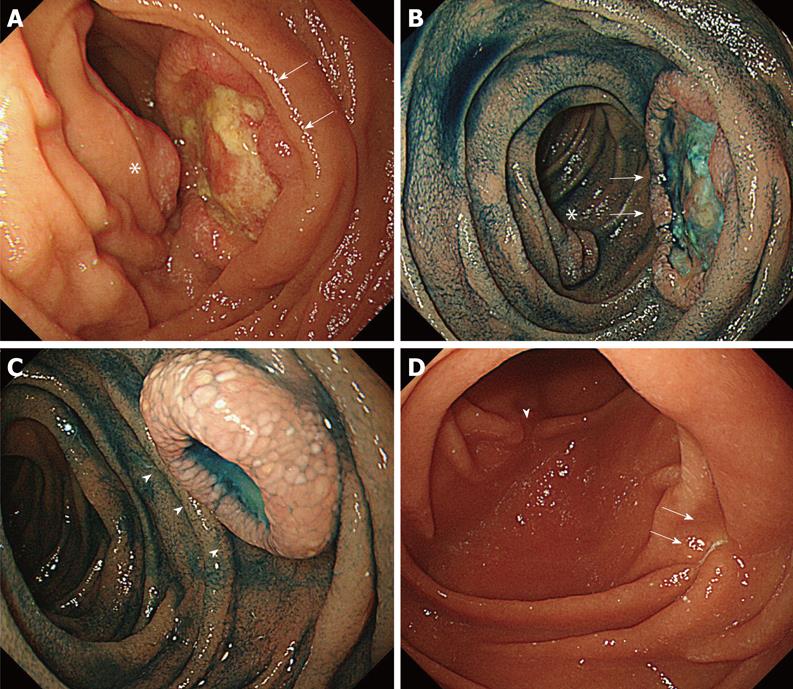
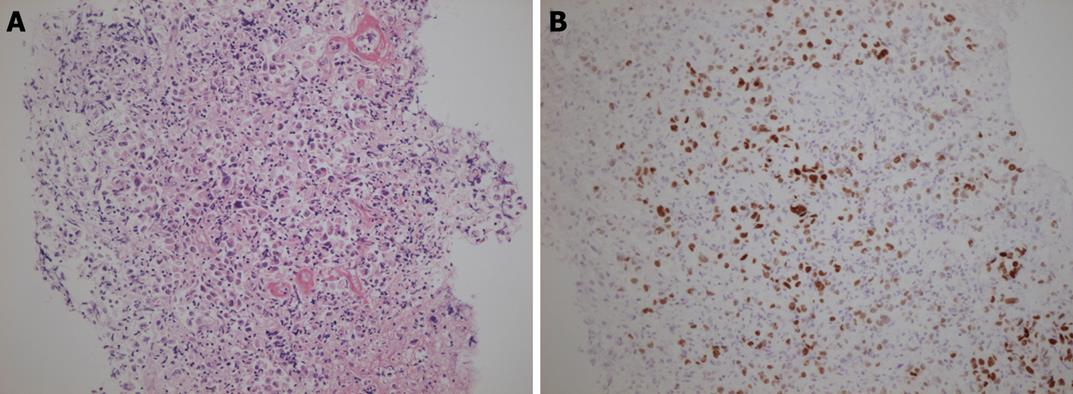
Esophagogastroduodenoscopy (EGD) was performed and three submucosal tumors were found located at the second portion of the duodenum. Endoscopic appearances varied among these 3 tumors. One showed a widely flat elevation with large central ulceration associated with a central tumorous protrusion (Figure 2A and B). Another one formed a tumorous protrusion with central ulceration (Figure 2C). The covering mucosa of the tumors looked normal with regular villi. Therefore, these lesions were thought to be non-epithelial tumors or tumors of submucosal origin. Based on these findings, malignant lymphoma or metastatic tumor to the duodenum was a possible diagnosis and primary duodenal carcinoma much less likely. The histopathological diagnosis of the biopsied specimens was poorly differentiated adenocarcinoma (Figure 3A). We thought metastasis from lung adenocarcinoma was less suspicious because the first-line therapy was very effective and the duodenal metastasis in lung adenocarcinoma was rare. To further characterize the nature of the tumor, we carried out immunostaining of TTF-1 and it was positive (Figure 3B). TTF-1 positivity is highly restricted to primary lung carcinoma and thyroid tumor[2,3]. Since CT revealed no thyroid tumor, we finally diagnosed this tumor as duodenal metastasis from primary lung adenocarcinoma. He received second-line generalized chemotherapy using gemcitabine. After 3 courses of gemcitabine, the para-aortic lymph node swelling and the thickening of the duodenal wall both disappeared in CT. The duodenal tumors disappeared and only scars remained in EGD (Figure 2D).
He is now receiving the additional courses of chemotherapy with gemcitabine.
Primary lung cancer often metastasizes to the brain, liver, adrenal glands and bone[1]. On the other hand, metastasis to the digestive tract is rare[4]. The site of metastasis to the digestive system is as follows: small intestine only (4.6%); large intestine only (2.0%); stomach only (1.6%); stomach and small intestine (0.6%); small and large intestine (0.6%); and stomach and large intestine (0.3%)[4]. Duodenal metastasis is very rare, even in autopsy[5].
Small bowel metastasis from primary lung cancer exhibits symptoms such as abdominal pain, vomiting, melena, weight loss, gastrointestinal perforation and obstruction, but most cases are asymptomatic[6].
Morphological features of duodenal metastasis are divided into four types: compression, protrusion, ulcer and stenosis[7]. Appearance of a metastatic lesion from extra-abdominal primary cancer is all protrusion type with central ulceration, so called ‘bull’s-eye’[7]. This type of metastatic lesion is probably hematogenous. The gross appearance of our case was protrusion type, widely elevated, having a central ulcer and resembling a submucosal tumor. Among all duodenal metastasis, the second portion (descending portion) is most frequent (58.7%)[7].
It is important to differentiate between primary and metastatic duodenal adenocarcinoma to make an appropriate choice of therapy, although it is difficult on occasion[1,2,8]. Recently, TTF-1 has become one of the best immunohistochemical markers to determine the lung or thyroid origin[2,8,9]. TTF-1 is tissue-specific for the thyroid gland and lung[2,3]. It is expressed in the type II alveolar cells and bronchial cells[10]. It is a transcription activator of the lung epithelial cell-specific surfactant protein B genes[11]. TTF-1 is expressed frequently in small cell carcinoma (85%-90%) and in adenocarcinoma (75%-80%)[9]. Sensitivity of TTF-1 for primary lung adenocarcinoma is 57.5 to 76% and the specificity is almost 100%[8]. Thus, TTF-1 is a very good marker to determine the lung origin in duodenal metastasis, as shown in our case.
The prognosis of lung cancer patients with metastasis to the digestive tract is poor[12]. Indication for emergency surgery is bleeding, perforation and obstruction[12]. There is a possible risk of gastrointestinal perforation due to chemotherapy[13]. In our case, duodenal tumors and lymph nodes shrank by systemic chemotherapy using gemcitabine without any serious adverse reaction.
In conclusion, duodenal metastasis from primary lung adenocarcinoma is rare and therefore difficult to diagnose. On such an occasion, TTF-1 can be a very useful immunohistochemical marker to determine the lung origin.
Peer reviewer: Cornelis FM Sier, PhD, Departments of Surgery and Gastroenterology, Leiden University Medical Center, Albinusdreef 2, Bldg 1, D6-18, 2333 ZA Leiden,The Netherlands
S- Editor Wang JL L- Editor Roemmele A E- Editor Yang C
| 1. | Steinhart AH, Cohen LB, Hegele R, Saibil FG. Upper gastrointestinal bleeding due to superior mesenteric artery to duodenum fistula: rare complication of metastatic lung carcinoma. Am J Gastroenterol. 1991;86:771-774. |
| 2. | Di Loreto C, Di Lauro V, Puglisi F, Damante G, Fabbro D, Beltrami CA. Immunocytochemical expression of tissue specific transcription factor-1 in lung carcinoma. J Clin Pathol. 1997;50:30-32. |
| 3. | Lau SK, Luthringer DJ, Eisen RN. Thyroid transcription factor-1: a review. Appl Immunohistochem Mol Morphol. 2002;10:97-102. |
| 4. | Ryo H, Sakai H, Ikeda T, Hibino S, Goto I, Yoneda S, Noguchi Y. [Gastrointestinal metastasis from lung cancer]. Nihon Kyobu Shikkan Gakkai Zasshi. 1996;34:968-972. |
| 5. | Richie RE, Reynolds VH, Sawyers JL. Tumor metastases to the small bowel from extra-abdominal sites. South Med J. 1973;66:1383-1387. |
| 6. | Mosier DM, Bloch RS, Cunningham PL, Dorman SA. Small bowel metastases from primary lung carcinoma: a rarity waiting to be found? Am Surg. 1992;58:677-682. |
| 7. | Miyakawa K, Sato N, Tateishi U, Inuma H, Moriyama N. Morphological features of metastasis: Duodenum (in Japanese with English abstract). Stomach and Intestine. 2003;38:1790-1798. |
| 8. | Reis-Filho JS, Carrilho C, Valenti C, Leitão D, Ribeiro CA, Ribeiro SG, Schmitt FC. Is TTF1 a good immunohistochemical marker to distinguish primary from metastatic lung adenocarcinomas? Pathol Res Pract. 2000;196:835-840. |
| 9. | Moldvay J, Jackel M, Bogos K, Soltész I, Agócs L, Kovács G, Schaff Z. The role of TTF-1 in differentiating primary and metastatic lung adenocarcinomas. Pathol Oncol Res. 2004;10:85-88. |
| 10. | Ikeda K, Clark JC, Shaw-White JR, Stahlman MT, Boutell CJ, Whitsett JA. Gene structure and expression of human thyroid transcription factor-1 in respiratory epithelial cells. J Biol Chem. 1995;270:8108-8114. |
| 11. | Bohinski RJ, Di Lauro R, Whitsett JA. The lung-specific surfactant protein B gene promoter is a target for thyroid transcription factor 1 and hepatocyte nuclear factor 3, indicating common factors for organ-specific gene expression along the foregut axis. Mol Cell Biol. 1994;14:5671-5681. |
| 12. | Woods JM 4th, Koretz MJ. Emergency abdominal surgery for complications of metastatic lung carcinoma. Arch Surg. 1990;125:583-585. |
| 13. | Suzaki N, Hiraki A, Ueoka H, Aoe M, Takigawa N, Kishino T, Kiura K, Kanehiro A, Tanimoto M, Harada M. Gastric perforation due to metastasis from adenocarcinoma of the lung. Anticancer Res. 2002;22:1209-1212. |