Published online Apr 15, 2025. doi: 10.4251/wjgo.v17.i4.100526
Revised: December 16, 2024
Accepted: January 23, 2025
Published online: April 15, 2025
Processing time: 218 Days and 13.6 Hours
Appendiceal signet-ring cell carcinoma (SRCC) with terminal ileum metastasis is extremely rare. There have been no reported cases in domestic and foreign literature.
In this case report, we present an 88-year-old man with appendiceal SRCC with terminal ileum metastasis. The tumour stage was stage pT4bN2M1bG3 IVB, and the Tumour, Node, Metastasis staging system was used. The patient was admitted to our hospital on 12 July, 2022 and underwent laparoscopic appendectomy under general anaesthesia after the examination. The pathological examination that took place 1 week after the operation showed that SRCC of the appendix invaded the whole layer, vessels and nerves of the appendix wall. It was suggested that the primary appendix should be considered after excluding metastasis. Based on the postoperative pathology findings, the patient underwent a secondary surgery on 2 August, 2022. The second pathological examination showed residual SRCC in the appendiceal area of the ileocecal region, which infiltrated the serosal fibres and adipose tissue of the ileocecal region to the surface mesothelium. The tumour infiltrated the whole layer of the ileum wall, serosa fibres, adipose tissue and the surface mesothelium. Postoperative follow-up showed no signs of tumour recurrence or metastasis.
In clinical practice, a heightened awareness of rare diseases, coupled with thorough intraoperative exploration and rapid pathological examination, enables more accurate judgments, potentially sparing patients from unnecessary secondary surgery and ensuring optimal treatment.
Core Tip: Signet ring cell carcinoma (SRCC) of the appendix is a rare malignant tumor, which accounts for only about 2.3% of all malignant tumors of the digestive system and 0.42% of all malignant tumors. Because of the rarity of SRCC, it is important to study its clinicopathologic features, diagnosis, and treatment methods in depth to improve patient outcomes. This case report reports an extremely rare case of SRCC of the appendix with metastases in the terminal ileum. It demonstrates the diagnosis and treatment process of this rare disease, emphasizes the importance of improving alertness to rare diseases in clinical practice, and the necessity of thorough intraoperative exploration and rapid pathological examination, which helps to more accurately determine the condition, avoid unnecessary secondary surgeries, and ensure that patients are optimally treated.
- Citation: Tang XW, Zhou Y. Signet ring cell carcinoma of the appendix and terminal ileum: A case report. World J Gastrointest Oncol 2025; 17(4): 100526
- URL: https://www.wjgnet.com/1948-5204/full/v17/i4/100526.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i4.100526
The incidence of appendiceal signet-ring cell carcinoma (SRCC) is extremely low, representing a rare malignant tumour of the appendix[1]. Clinical manifestations of appendiceal SRCC are often nonspecific, with the potential absence of symptoms or only mild presentations resembling acute or chronic appendicitis. This condition can be easily misdiagnosed as appendicitis, leading to appendectomy and subsequent secondary surgery[2]. Additionally, some clinicians may lack awareness of malignant tumours in the appendix, contributing to a higher rate of misdiagnosis and missed diagnoses. Currently, surgical intervention remains the primary approach in the clinical management of appendiceal SRCC, with right hemicolectomy still considered the optimal surgical procedure for the majority of histological types of primary appendiceal cancer. There are very few cases of appendiceal SRCC with ileum metastasis. This study reports a case of appendiceal SRCC with terminal ileum metastasis. The patient underwent secondary surgery and combined chemotherapy, and postoperative follow-up revealed no signs of tumour recurrence or metastasis. This may provide valuable insights for the diagnosis and treatment of appendiceal SRCC.
The patient was an 88-year-old man. This study has been approved by Shanghai Jiading Hospital of Traditional Chinese Medicine Ethics Committee (Expedited Ethical Review No. 16). On 12 July, 2022, he came to the hospital due to abdominal distention and discomfort lasting for half a month, which was aggravated for 3 days. Half a month before admission, the patient developed abdominal distension and discomfort without obvious causes, accompanied by difficult defecation, but without obvious abdominal pain, nausea or vomiting. Three days before admission, the patient’s abdominal distension worsened, and he went to another hospital for treatment. Abdominal computed tomography (CT) scan showed signs of acute appendicitis and a small amount of pelvic effusion. A routine blood test showed the following: White blood cell count of 13.1 × 109/L, 86.5% neutrophils, C-reactive protein of 5.8 mg/L and normal coagulation function. Acute appendicitis was diagnosed, and surgical treatment was recommended. The patient was transferred to our hospital for further surgical treatment.
July 12, 2022: The patient came to the hospital due to abdominal distension and discomfort for half a month, aggravated for 3 days. The patient was diagnosed with acute appendicitis and surgical treatment was recommended. The patient was transferred to Shanghai Jiading Hospital for further surgical treatment. The patient underwent laparoscopic appendectomy under general anesthesia.
July 18, 2022: The patient was discharged from the hospital after recovery of bowel ventilation and diet.
July 20, 2022: The first postoperative pathology report was obtained and showed SRCC in the appendix, which invaded all layers of the appendiceal wall as well as vessels and nerves. Primary appendiceal cancer is recommended to be considered after excluding metastases.
July 25, 2022: The patient was readmitted to the hospital and additional surgical treatment was planned.
August 02, 2022: The patient underwent laparoscopic radical resection of right colon cancer after surgical contraindication was excluded. Because the procedure was difficult, it was converted to laparotomy. Right hemicolectomy and partial sigmoid/descending colectomy were performed.
August 10, 2022: A second postoperative pathology report was obtained and showed residual SRCC in the ileocecal appendix area invading the serosal fibers and adipose tissue to the superficial mesothelial layer.
August 19, 2022: The patient recovered well after treatment of postoperative symptoms and was discharged.
November 2022: The patient started oral capecitabine.
November 2023 (1 year post-operative follow-up): The patient remains in outpatient follow-up and no signs of tumor recurrence or metastasis have been observed.
The patient had a history of hypertension and lacunar cerebral infarction, both well-controlled, with no history of abdominal surgery.
Physical examination on admission showed a body temperature of 37.5 °C, heart rate of 100 beats/min, blood pressure of 135/70 mmHg, clear mentation, a flat abdomen, slight fullness in the lower abdomen, no visible gastrointestinal peristalsis waves, tenderness in the right lower abdomen, accompanied by rebound pain and muscle guarding and normal bowel sounds. The patient immediately underwent laparoscopic appendectomy under general anaesthesia. Intraoperatively, the appendix was located in the pelvic area, with a diameter of 1.5 cm, a length of about 5 cm and a thickened, swollen and hard texture. It was adherent to the cecum and peritoneum, with a small amount of pale yellow exudate around the appendix and pelvic cavity. The appendix was removed after separating the adhesions.
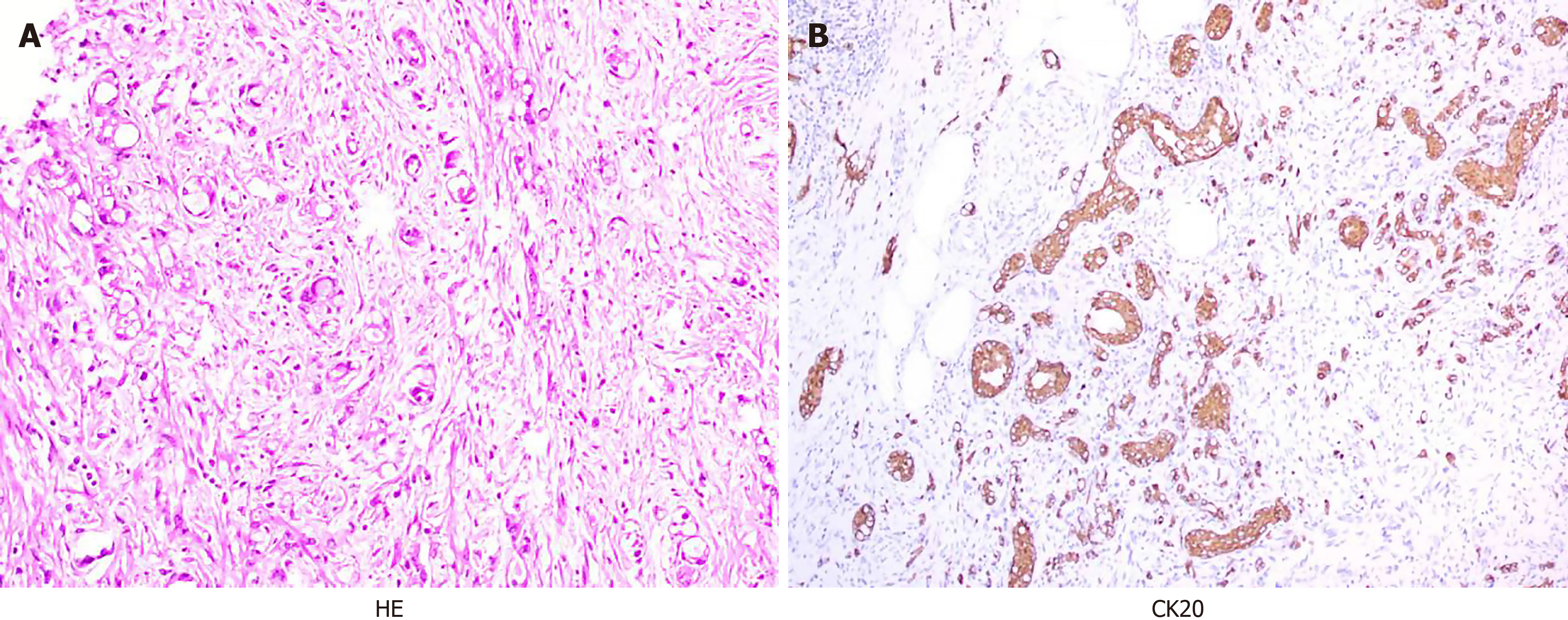
The first postoperative pathology report was obtained on 20 July, 2022. The report showed the following: The appendix exhibited SRCC that invaded all layers, as well as the vessels and nerves of the appendix wall. It was suggested that primary appendiceal carcinoma should be considered after excluding metastasis. Immunohistochemical and special staining results showed the following: MLH1 (+), MSH2 (+), MSH6 (+), PMS2 (+), Ki-67 (+, 30%), Syn (-), CgA (focally positive), the CD56 (-), CK7 (-), CK8/18 (+), CK20 (+), SATB2 (+), AB/PAS AB (+) /PAS (-), mucin-4 (nuclear positive), MUC-5AC (-), villin (+), CDX2 (+) and paired box-8 (-; Figure 1). Based on the postoperative pathological examination, secondary surgery was required.
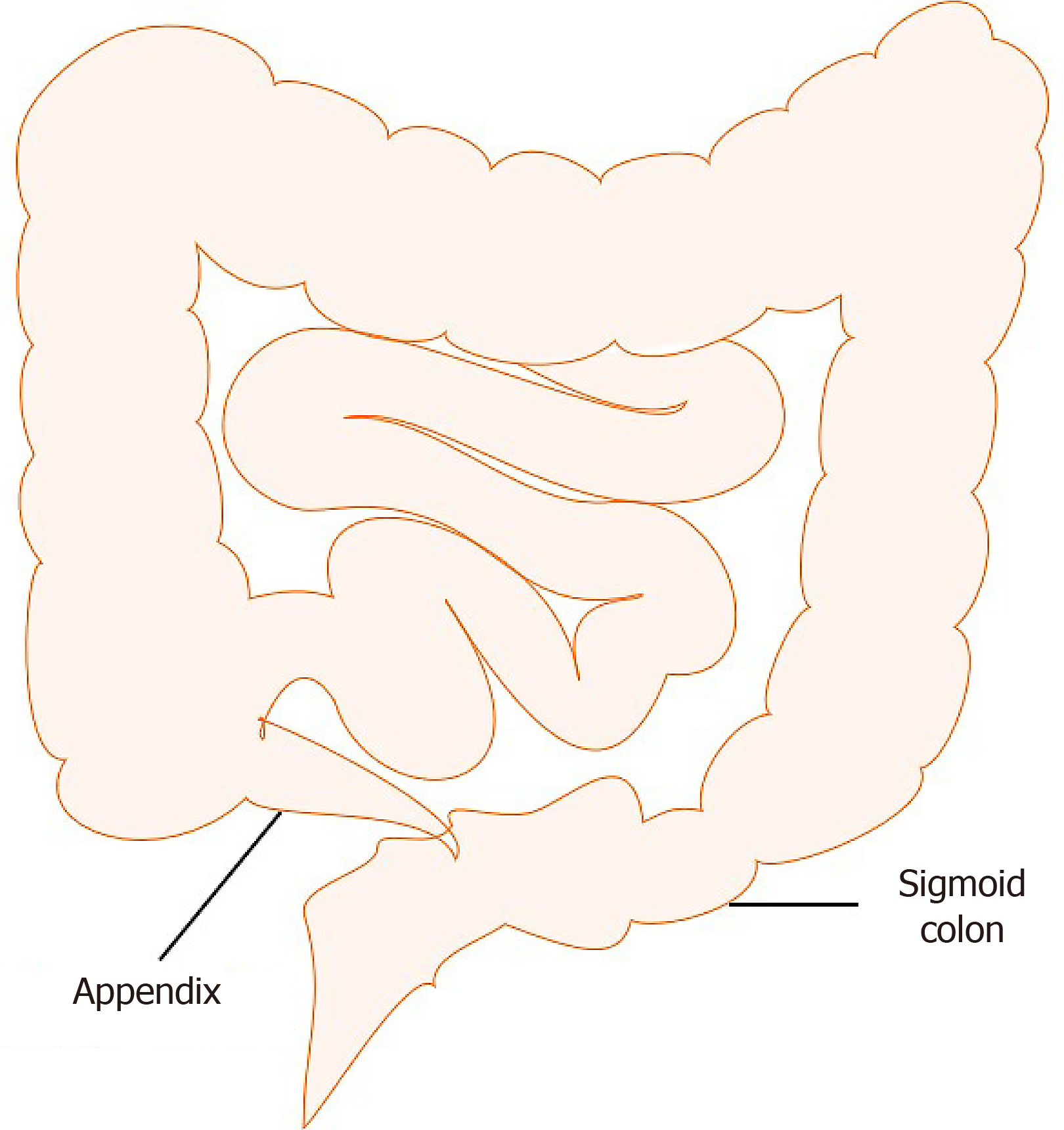
On 2 August, 2022, laparoscopic radical resection of right colon cancer was performed under general anaesthesia after excluding surgical contraindications. During the operation, the greater omentum moved inferiorly to encapsulate the ileocecal junction, and the omental tissue showed oedema and hyperplasia. After dissecting the greater omentum, oedema and hyperplasia of the ileocecal junction of the ascending colon were observed. The distal ileum was slightly dilated, and the sigmoid colon was elongated, and it accumulated in the right lower abdomen, forming dense adhesions with the ileocecal junction and terminal ileum, which could not be separated. Laparoscopic surgery was difficult, so a laparotomy was performed. During the operation, we found that the appendix was only adherent to the sigmoid colon and not to the terminal ileum. According to the intraoperative findings, right hemicolectomy and partial sigmoid/descending colectomy were performed. The resected segment was 26 cm from the ileal resection margin and 19 cm from the ileocecal junction, indicating that ileal metastasis did not result from adhesion to the appendix (Figure 2). After postoperative symptomatic treatment, the patient recovered well and was discharged on 19 August, 2022.
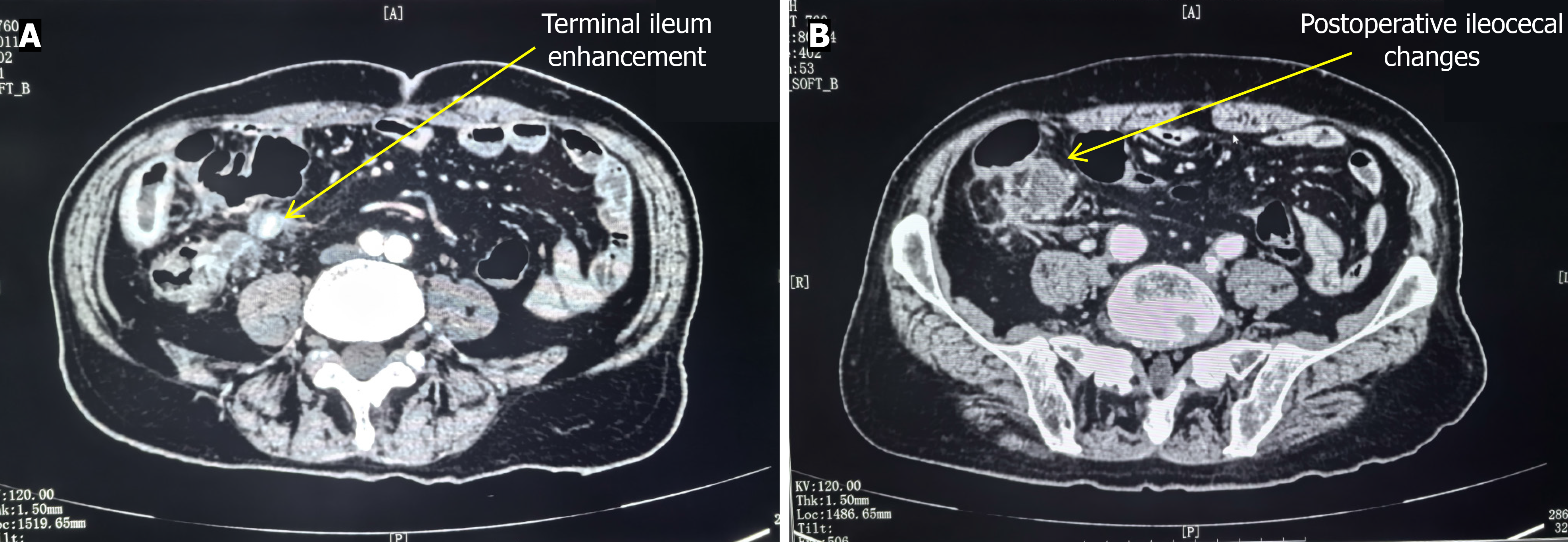
The patient was hospitalised again on 25 July, 2022 and was planned to undergo additional surgical treatment. Colonoscopy did not reveal any space-occupying lesions. Preoperative contrast-enhanced CT of the lower abdomen showed a nodular soft tissue density shadow in the ileocecal region and thickening of the small intestine in the right lower abdomen, which showed enhanced uptake (Figure 3). The second pathological examination was obtained on 10 August, 2022. It showed residual SRCC in the appendiceal area of the ileocecal region, infiltrating serosal fibres and adipose tissue to the surface mesothelial layer of the ileocecal region. The appendiceal area showed postoperative pathological changes, including abundant foreign bodies, inflammatory cell infiltration, foreign body giant cell reaction, abundant foamy tissue cell reaction and focal fat necrosis. The sigmoid colon adhered to the ileocecal region, and the serosal layer and mesentery of the sigmoid colon were infiltrated by carcinoma. The maximum diameter of the tumour was approximately 4 cm. The tumour infiltrated the entire wall of the ileum, serosal fibres, adipose tissue and the surface mesothelium. There was no tumour involvement in the distal and proximal resection margins of the sigmoid colon or the distal and proximal resection margins of the right colon. One out of two mesenteric lymph nodes showed cancer metastasis, and five cancer nodules were found. Two out of two lymph nodes beside the sigmoid colon and four out of fifteen mesenteric lymph nodes near the ascending colon showed cancer metastasis, with cancer infiltration observed in the surrounding fat of two lymph nodes. No cancer involvement was found in one out of one lymph node sent from the cecum. Moreover, two lymph nodes sent from the mesentery showed no cancer metastasis. Immunohistochemistry and special staining results were as follows: MLH1 (+), MSH2 (+), MSH6 (+), PMS2 (+), Syn (-), CgA (-), CD56 (-), tumour-suppressor protein 53 (+), Ki-67 (+, 40%), SATB2 (+), AB/PAS AB (+)/PAS (sporadic positive), CK7 (-), CK20 (+) and CK8/18 (+).
The patient was hospitalised again on 25 July, 2022 and was planned to undergo additional surgical treatment. Colonoscopy did not reveal any space-occupying lesions. Preoperative contrast-enhanced CT of the lower abdomen showed a nodular soft tissue density shadow in the ileocecal region and thickening of the small intestine in the right lower abdomen, which showed enhanced uptake (Figure 3).
The patient had signet ring cell carcinoma of the appendix and lymph node metastasis.
Combined with the postoperative pathological examination reports, it was suggested that the patient should undergo postoperative chemotherapy and tumour genetic testing. The preferred chemotherapy regimen was mFOLFOX6, but considering the patient’s advanced age, the possibility of receiving the CapeOx regimen chemotherapy was also considered after a discussion with the family. After four courses of CapeOx chemotherapy, due to the coronavirus disease 2019 pandemic and despite the patient not being infected, the family requested to discontinue chemotherapy. After multiple communications, the patient received two courses of oral capecitabine. Subsequently, the family declined further chemotherapy.
The patient is currently under outpatient follow-up (the last contact was in early November 2023; follow-up time was 1 year, and magnetic resonance imaging was performed), and no signs of tumour recurrence or metastasis have been observed during the postoperative follow-up.
SRCC is a rare subtype of adenocarcinoma. It is named for its signet-ring appearance under the microscope due to abundant mucin in the cells, rich cytoplasm and nuclei pushed to one side of the cell[3]. In this case, the initial pathology of the appendix showed that the patient had SRCC of the appendix, and the secondary pathology indicated a lesion in the terminal ileum with a diameter of approximately 4 cm. Therefore, the primary focus could either be adenocarcinoma of the terminal ileum with tumour cells implanting in the appendix or an appendiceal tumour that has formed metastatic lesions in the terminal ileum through lymphatic or blood flow[4]. Immunohistochemical analysis shows that distal small intestinal adenocarcinoma exhibits similar immunohistochemical characteristics to colon cancer, and, as appendix adenocarcinoma, it can express positivity for various proteins such as CK18, CK20, MUC-5AC, villin and CDX2. However, SATB2 protein is typically not expressed in the small intestinal mucosal epithelium, yet it has high sensitivity and specificity in appendiceal and colorectal adenocarcinoma. Literature also suggests that the expression of SATB2 protein can be used as a biological marker for the origin of appendiceal tumours[5]. Based on this, it was concluded that the patient’s case was one of SRCCA, with a high likelihood that the lesion in the terminal ileum was metastatic. When distinguishing primary appendiceal tumours from metastatic tumours, immunohistochemical features and pathological findings can be used. The expression of SATB2 protein is an important biomarker that helps identify the primary site of appendiceal tumours[5]. Because SATB2 protein can also be positively expressed in some small intestinal adenocarcinomas[6], in order to exclude small intestinal adenocarcinomas as primary tumors in this study, we detected CK7, which was not expressed in tumor tissues, so we considered the appendix as the primary tissue of tumors. In this study, using only SATB2 positivity to suggest that the tumor was a primary appendiceal is a limitation of this study, and at that time we should use more markers to examine. In addition, the pathological report of the primary appendiceal tumour did not mention an orthotopic component or precursor lesion in the appendix, whereas metastatic tumours may not show these features at the primary site. By considering the pathological features, immunohistochemical findings and clinical manifestations, the primary site of the tumour can be more accurately determined.
In this study, resection was selected as the treatment method, which was consistent with previous literature reports[7,8]. SRCC is highly invasive, with a median survival period of about 24 months. The treatment and management of this condition follow the guidelines for colon cancer[9]. Patients diagnosed with SRCCA typically undergo standard right hemicolectomy and receive perioperative chemotherapy regimens, such as FOLFOX and CapeOx, involving fluo
During the early treatment of this patient, the best surgical approach was not selected promptly. The causes are summarised as follows: (1) SRCC of the appendix has a low incidence and is rare in clinical practice; (2) The clinical presentation was similar to that of acute appendicitis, but during the collection of the medical history, it was noted that the patient had complained of abdominal distension and constipation for some time before surgery; and (3) During the operation, the appendix was found to be adherent to the sigmoid colon and the adhesions were distinct from inflammatory adhesions. Inflammatory adhesions usually form as a result of an inflammatory reaction in the abdominal cavity, such as infection or postoperative inflammation, and they may be extensive and involve multiple organs. Inflammatory adhesions tend to result from fibrin exudation and organization as a result of an inflammatory reaction in the peritoneum, resulting in thin and fragile adhesion bands[14]. Adhesions caused by tumors may be due to invasive tumor growth and local inflammatory response, and adhesion bands may be thick and tough and difficult to separate[15].
In summary, this patient had appendiceal SRCC with ileal metastasis. In the clinical management process, although secondary surgery for malignant tumours of the appendix is not uncommon, if the physician is aware of the possibility of rare diseases and conducts necessary and comprehensive intraoperative exploration along with rapid pathological examination, a more accurate judgment can be made. This approach allows the patient to avoid unnecessary secondary surgery and receive more appropriate treatment.
| 1. | Roy SP, Al Zhahrani N, Barat S, Morris DL. Case series on high grade appendiceal cancer with peritoneal and liver carcinomatosis undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC). Int J Surg Case Rep. 2022;94:107027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Pickhardt PJ, Levy AD, Rohrmann CA Jr, Kende AI. Primary neoplasms of the appendix manifesting as acute appendicitis: CT findings with pathologic comparison. Radiology. 2002;224:775-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 88] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Wang G, Li Q, Chen W. Chemotherapy in the treatment of different histological types of appendiceal cancers: a SEER based study. BMC Cancer. 2021;21:778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Chen F, Harvey SE, Young ED, Liang TZ, Larman T, Voltaggio L. Extra-appendiceal mucinous neoplasms: A tumour with clinicopathologic similarities to low- and high-grade appendiceal counterpart. Hum Pathol. 2024;148:23-31. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Mikaeel RR, Young JP, Tapia Rico G, Hewett PJ, Hardingham JE, Uylaki W, Horsnell M, Price TJ. Immunohistochemistry features and molecular pathology of appendiceal neoplasms. Crit Rev Clin Lab Sci. 2021;58:369-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Neri G, Arpa G, Guerini C, Grillo F, Lenti MV, Giuffrida P, Furlan D, Sessa F, Quaquarini E, Viglio A, Ubezio C, Pasini A, Ferrero S, Sampietro G, Ardizzone S, Latella G, Mescoli C, Rugge M, Zingone F, Barresi V, Ciccocioppo R, Pedrazzoli P, Corazza GR, Luinetti O, Solcia E, Paulli M, Di Sabatino A, Vanoli A. Small Bowel Adenocarcinomas Featuring Special AT-Rich Sequence-Binding Protein 2 (SATB2) Expression and a Colorectal Cancer-Like Immunophenotype: A Potential Diagnostic Pitfall. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Suzuki T, Yamamoto Y, Torigoe T, Mizukami S, Shigehara K. Primary Appendiceal Adenocarcinoma Presenting with Hematochezia due to the Invading Tumor in the Sigmoid Colon. Case Rep Surg. 2020;2020:8833573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Stein S, Raymond D O B. Appendiceal Adenocarcinoma Presenting As Perforated Appendicitis. Cureus. 2021;13:e13578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Sato A, Sato Y, Hiruta N, Oshiro T, Yoshida Y, Urita T, Kitahara T, Kadoya K, Nabekura T, Moriyama Y, Okazumi S. Signet-ring cell carcinoma of the appendix with ganglioneuromatosis: a case report. Surg Case Rep. 2022;8:151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Ang CS, Shen JP, Hardy-Abeloos CJ, Huang JK, Ross JS, Miller VA, Jacobs MT, Chen IL, Xu D, Ali SM, Baumgartner J, Lowy A, Fanta P, Ideker T, Millis SZ, Harismendy O. Genomic Landscape of Appendiceal Neoplasms. JCO Precis Oncol. 2018;2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Choe JH, Overman MJ, Fournier KF, Royal RE, Ohinata A, Rafeeq S, Beaty K, Phillips JK, Wolff RA, Mansfield PF, Eng C. Improved Survival with Anti-VEGF Therapy in the Treatment of Unresectable Appendiceal Epithelial Neoplasms. Ann Surg Oncol. 2015;22:2578-2584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Hirose S, Enami C, Kawamatsu N, Ito Y, Onoda T, Sugiyama Y, Suzuki H, Nagafuchi M, Ikeda T, Niisato Y, Yamada T, Yamamoto Y, Moriwaki T, Suzuki H. Systemic chemotherapy combined with anti-epidermal growth factor receptor antibody therapy for RAS wild-type appendiceal signet-ring cell carcinoma: a series of three cases. Int Cancer Conf J. 2022;11:17-22. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Strach MC, Sutherland S, Horvath LG, Mahon K. The role of chemotherapy in the treatment of advanced appendiceal cancers: summary of the literature and future directions. Ther Adv Med Oncol. 2022;14:17588359221112478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 14. | Tian X, Zhang Y, Gong H, Bai M, Sun C, Jia Y, Duan C, Wang X. Knockdown of ANO1 decreases TGF-β- and IL-6-induced adhesion and migration of cardiac fibroblasts by inhibiting the expression of integrin and focal adhesion kinase. Exp Cell Res. 2024;443:114321. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Dimitrov J, Maddalena M, Terlizzi C, Altobelli GG, Pellegrino S, Mehmood T, De Rosa V, Iommelli F, Del Vecchio S. Dynamic roles of neutrophil extracellular traps in cancer cell adhesion and activation of Notch 1-mediated epithelial-to-mesenchymal transition in EGFR-driven lung cancer cells. Front Immunol. 2024;15:1470620. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |