Published online Jul 15, 2024. doi: 10.4251/wjgo.v16.i7.3350
Revised: May 6, 2024
Accepted: May 21, 2024
Published online: July 15, 2024
Processing time: 103 Days and 3.3 Hours
The incidence of multiple primary carcinomas (MPC) varies greatly, ranging from 0.73% to 11.70% in foreign countries, with duo-duplex carcinoma being the most common, trio-duplex carcinoma and above being rare, and simultaneous multigenic carcinoma being even rarer, accounting for 18.4% to 25.3% of the incidence of MPC. However, there is no report regarding patients presenting with simultaneous dual-origin carcinoma of the liver and colon and heterochronous pancreatic cancer.
We report a special case of multifocal carcinoma, in which one patient had a medical condition of primary liver and colon cancer and pancreatic cystadenocarcinoma 2 years after surgery. Through aggressive advanced fluorescent laparoscopic techniques, standardized immunotherapy, targeting, and chemotherapy, a better prognosis and a desirable survival period were achieved for the patient.
There is a need to clarify the nature of MPC through advanced surgical means to ensure better diagnosis and treatment.
Core Tip: This study describes an uncommon case of simultaneous dual-origin carcinoma of the liver and colon and heterochronous pancreatic cancer, which was verified through histopathological and immunohistochemical analyses. Our findings suggest that patients can benefit from comprehensive diagnosis and treatment.
- Citation: Wan DD, Li XJ, Wang XR, Liu TX. Metachronous multifocal carcinoma: A case report. World J Gastrointest Oncol 2024; 16(7): 3350-3356
- URL: https://www.wjgnet.com/1948-5204/full/v16/i7/3350.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i7.3350
Multiple primary carcinomas (MPC) were refer to the occurrence of two or more primary malignant tumors in the same patient. Currently, the diagnostic criteria proposed by Warren and Gates[1] are primarily used. The incidence of MPC varies greatly, ranging from 0.73% to 11.70% in foreign countries[2], with duo-duplex carcinoma being the most common, trio-duplex carcinoma and above being rare[3-5], and simultaneous multigenic carcinoma being even rarer, accounting for 18.4% to 25.3% of the incidence of MPC[6,7]. Accurate diagnosis prior to surgery poses challenges, necessitating postoperative immunohistochemistry of the specimen for a definitive diagnosis. As of reporting this case, there is no report regarding patients presenting with simultaneous dual-origin carcinoma of the liver and colon and heterochronous pancreatic cancer. Herein, we report the clinical case of a 60-year-old male patient who was diagnosed with meta
The patient was a 60-year-old male. He was admitted to the hospital due to right-sided abdominal pain that had lasted for a week.
The patient report abdominal pain, and there were changes in bowel habits. But, there were no signs of hematemesis or melena.
He had a history of hepatitis B, hypertension, diabetes, and sequelae of cerebral infarction.
He also had a family history of colon cancer.
The physical examination of the patient showed some abnormality that right abdominal tenderness, no rebound pain and muscle tension, not touched the mass.
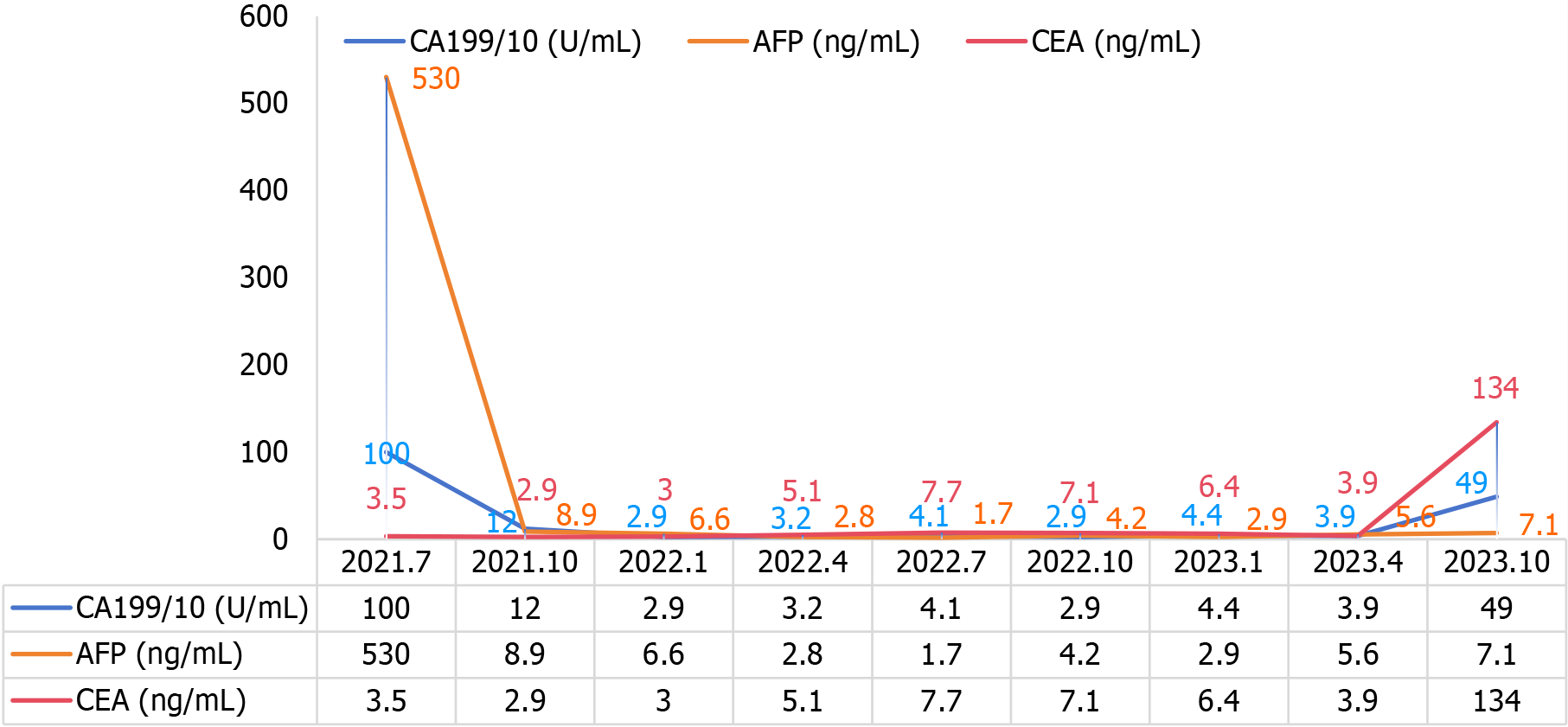
The post-hospitalization laboratory results were summarized as follows: The count of white blood cell, red blood cell and platelet are all normal, alpha-fetoprotein level of 530 ng/mL, cancer antigen 199 level of 100 U/mL, and carcinoembryonic antigen level of 3.5 ng/mL. Abnormal prothrombin level of 54.46 μg/L.
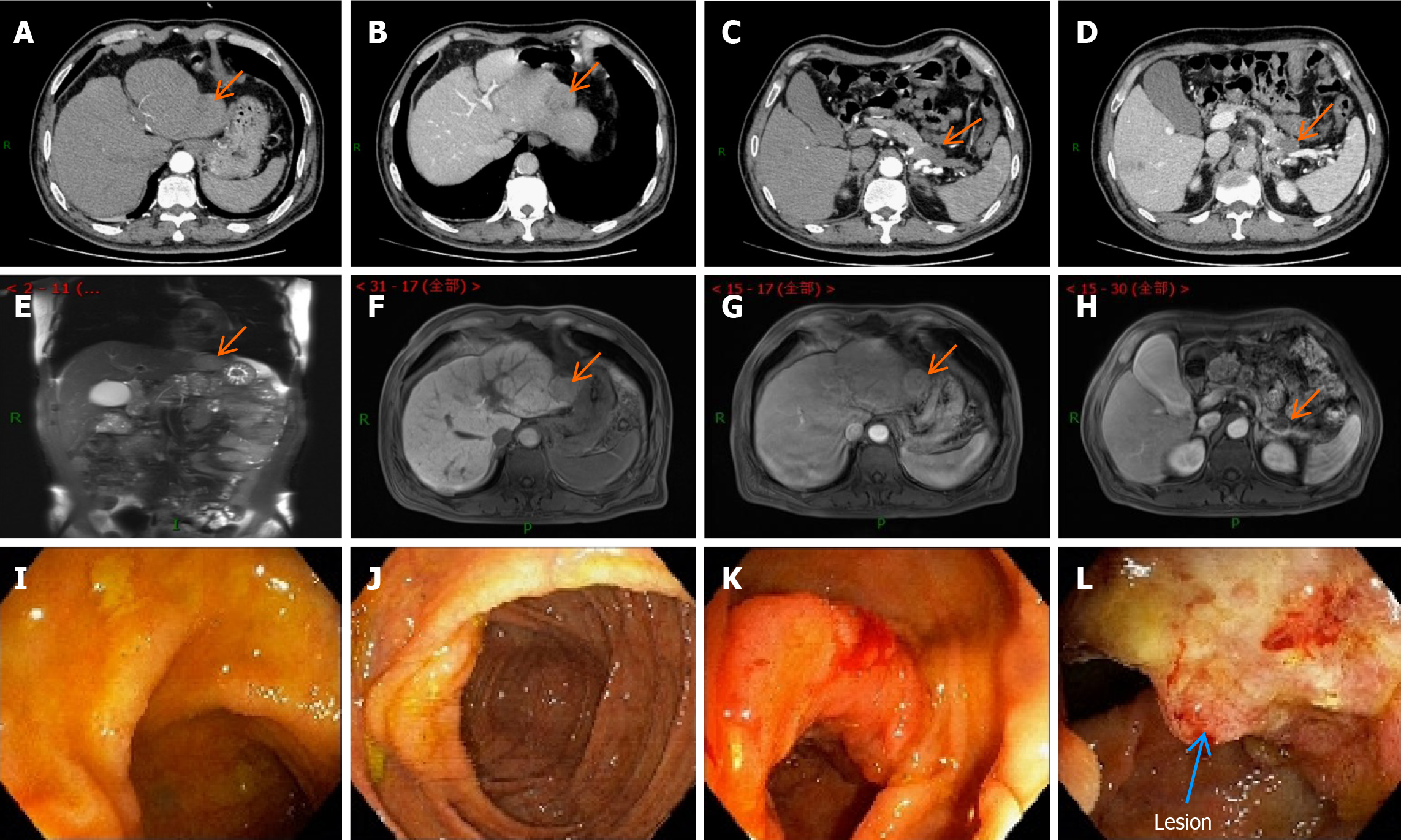
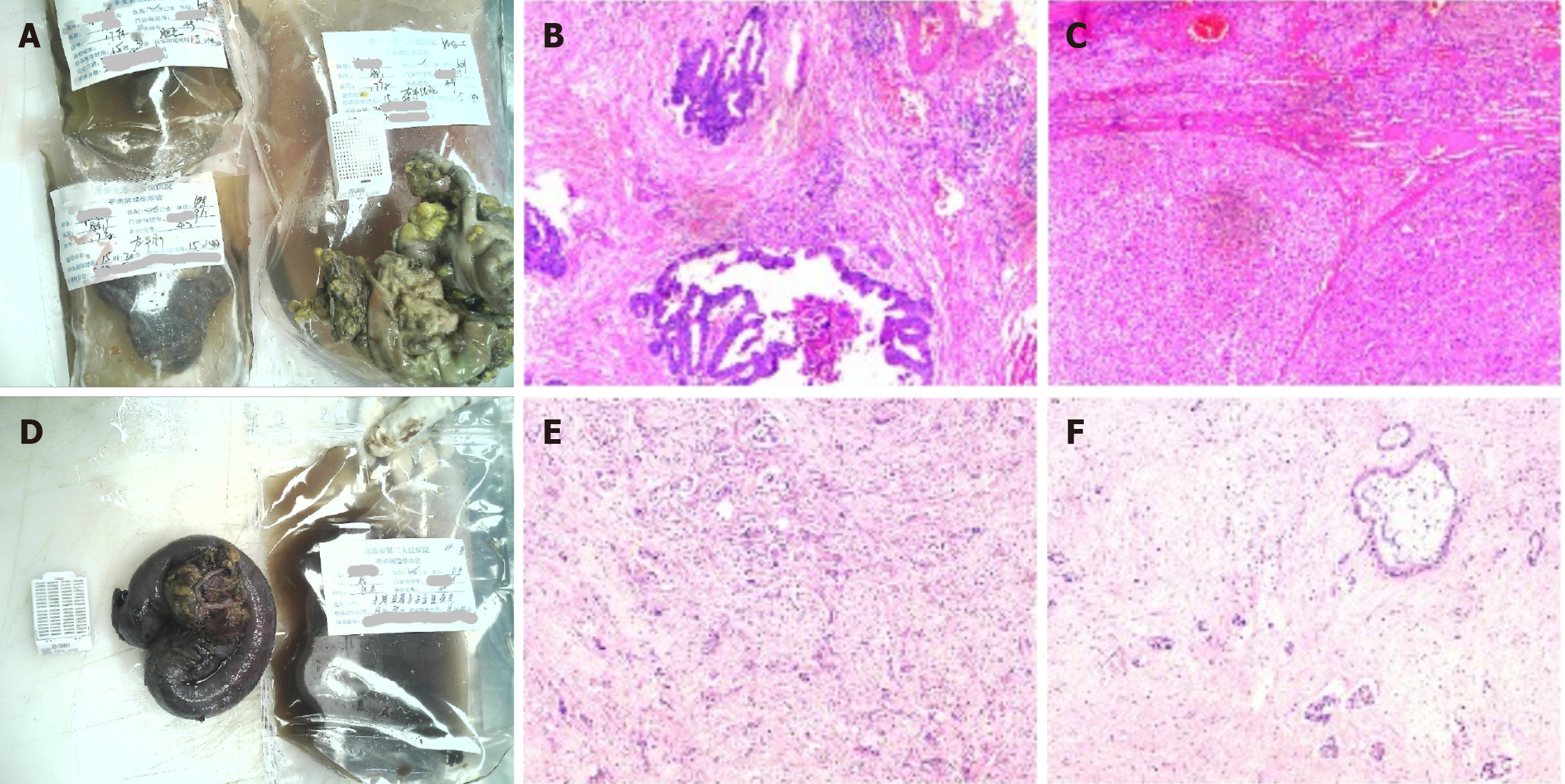
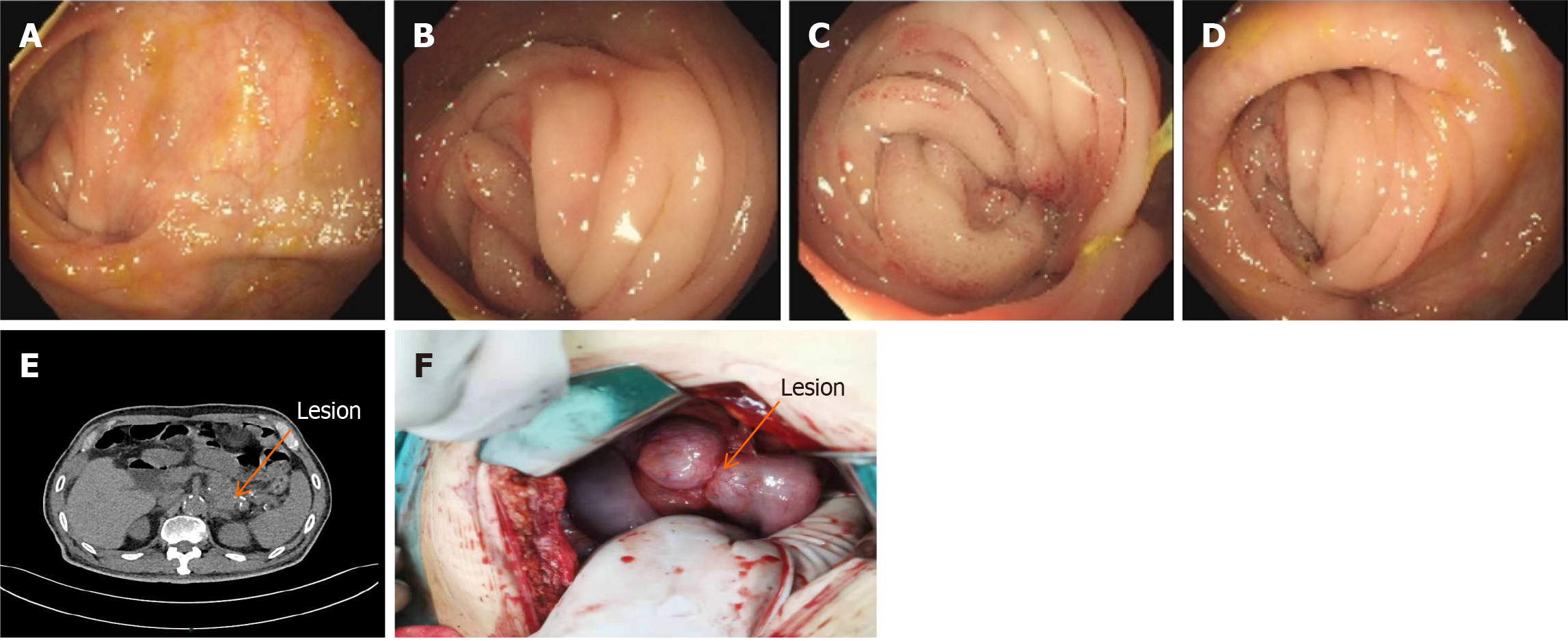
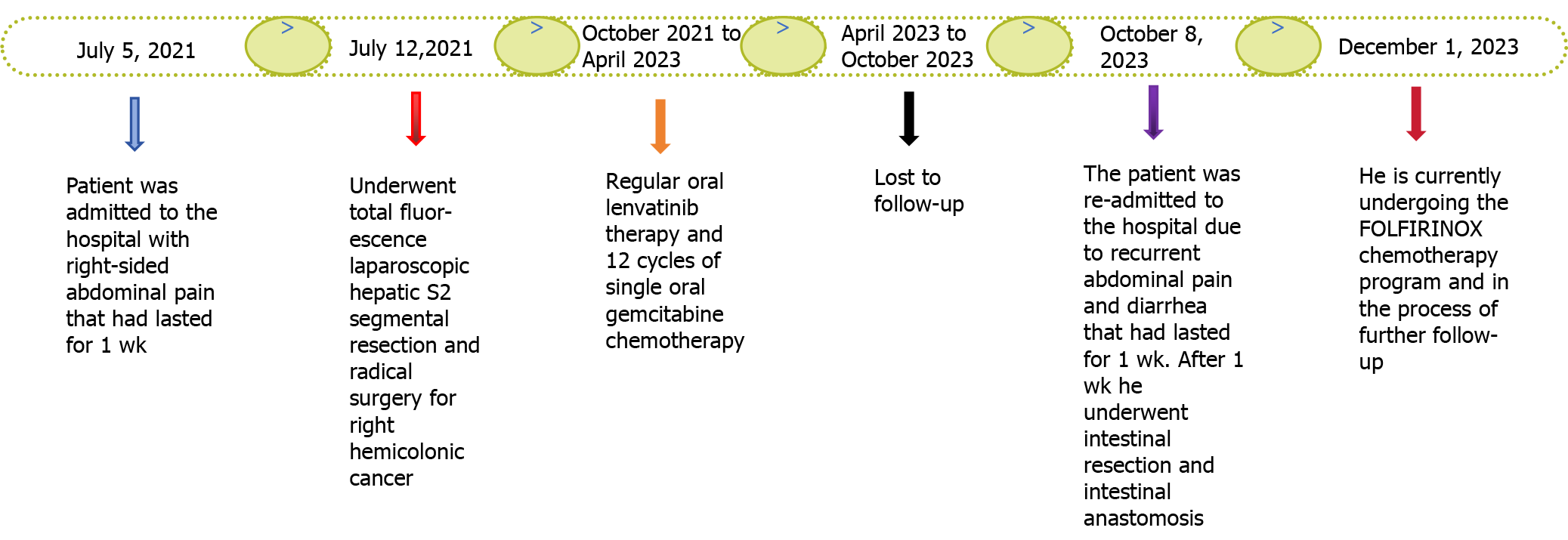
He was admitted to the hospital for a complete examination, including abdominal-enhanced magnetic resonance imaging, abdominal-enhanced computed tomography (CT), and gastrointestinal scintigraphy (Figure 1). Postoperative examination and immunohistochemical results confirmed that the colon lesion was a low-to-moderately differentiated adenocarcinoma, and the liver lesion was a moderately differentiated hepatocellular carcinoma (Figure 2). Two years post-surgery, the patient was re-admitted to the hospital due to recurrent abdominal pain and diarrhea that had lasted for 1 wk. After abdominal CT and colonoscopy (Figure 3A-E), intestinal obstruction and pancreatic cystadenoma were considered.
He was diagnosed with cystadenoma of the pancreas and double-origin cancer of the liver and colon.
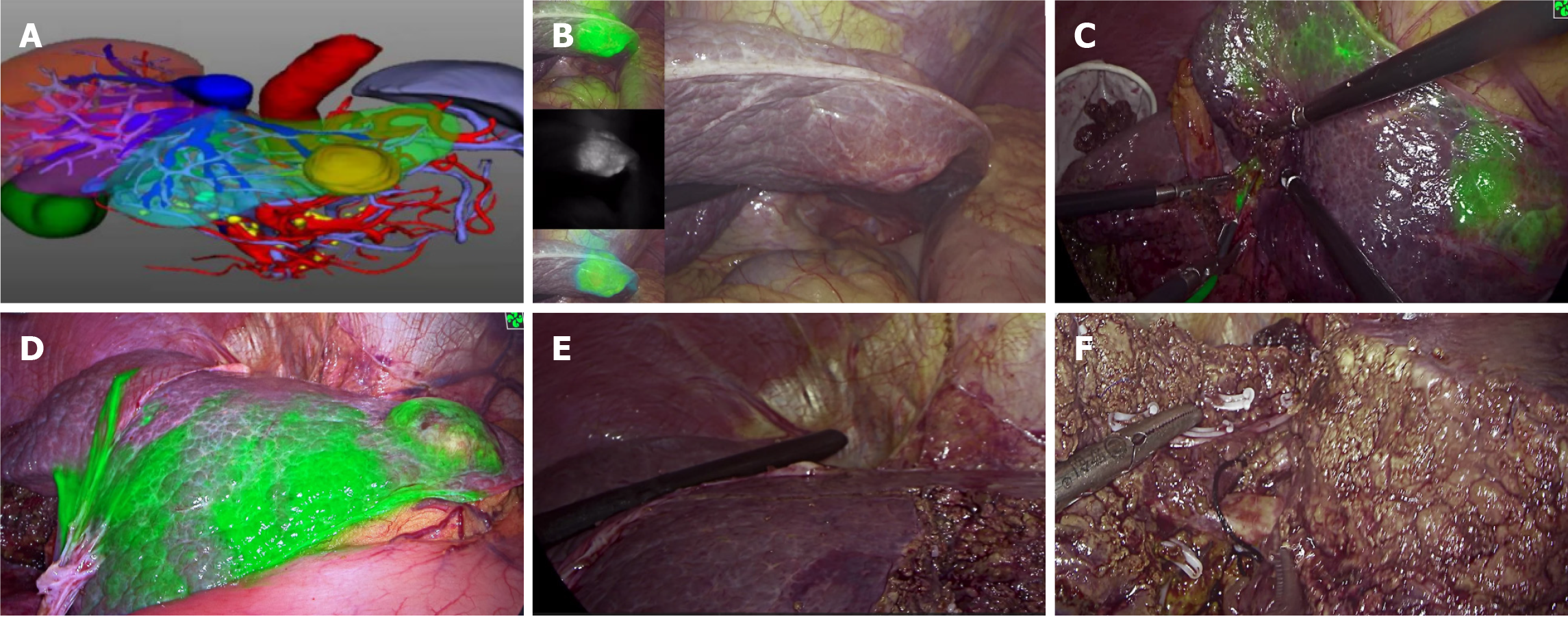
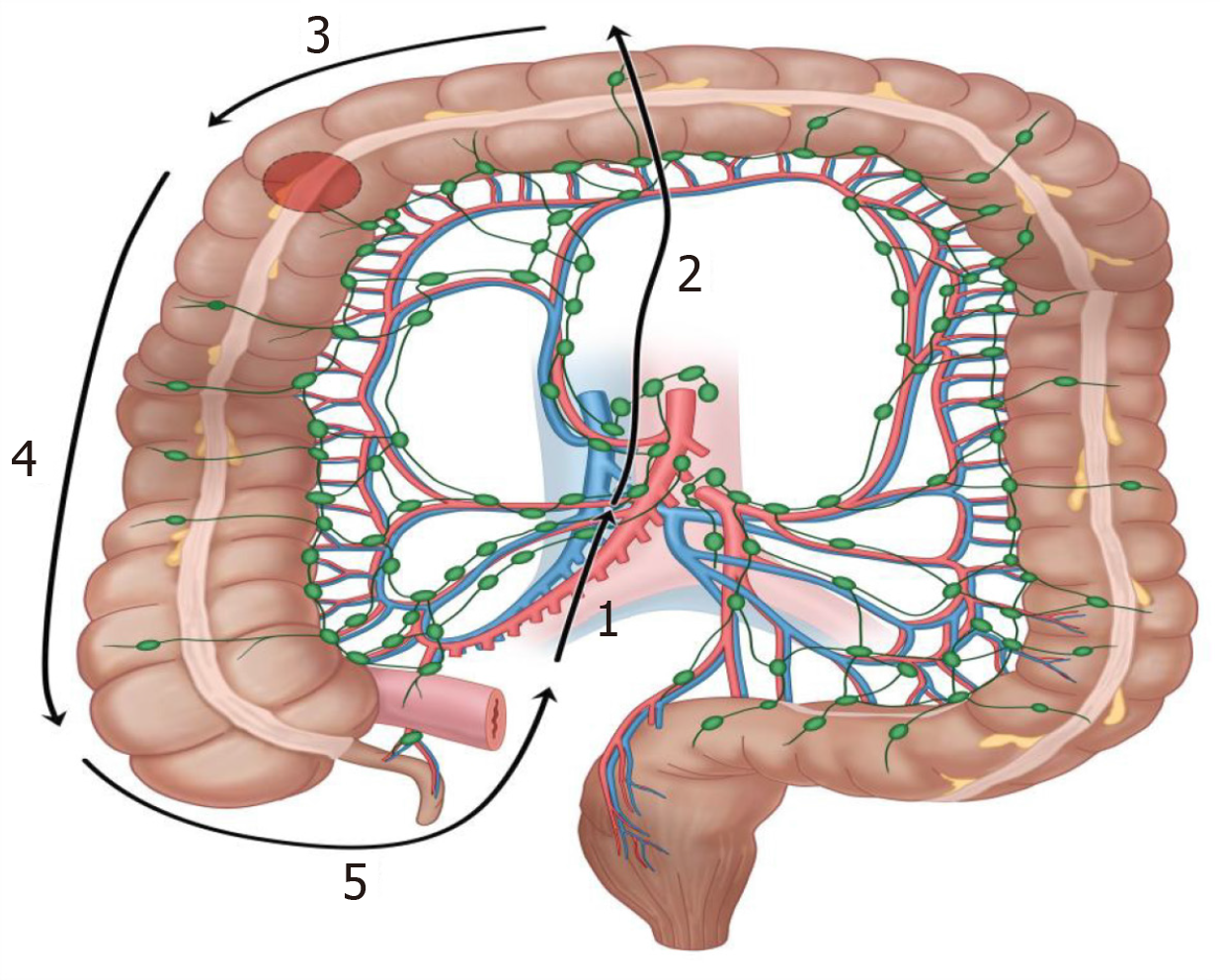
He underwent total fluorescence laparoscopic hepatic segmental 2 resection and radical surgery for right hemicolonic cancer. His operation proceeded smoothly and lasted for 4 h. The volume of blood lost due to bleeding was approximately 100 mL, and he was discharged 12 d after the surgery. The intra-operative images and operation schematic diagrams are presented in Figures 4 and 5. The patient underwent regular postoperative follow-ups, regular oral lenvatinib therapy, and 12 cycles of single oral gemcitabine chemotherapy. Two years post-surgery, the patient was re-admitted to the hospital due to recurrent abdominal pain and diarrhea that had lasted for 1 wk. The patient was not suitable for conservative treatment because of his poor condition; therefore, intestinal resection was performed. The site of the obstruction was observed during surgery (Figure 3F).
The patient recovered well after the operation and underwent the FOLFIRINOX chemotherapy program 1 month after the surgery. Currently, his condition is stable, and he is being followed up further. Furthermore, we provided the key indicators during follow-up and the timeline of the disease progression in Figures 6 and 7.
Owing to its dual blood supply, the liver is a common metastatic organ for malignant tumors, accounting for approximately 40% of all malignant tumors, with colorectal cancer being the most common source. Although the vast majority of colon and liver tumors reported simultaneously in clinical settings are liver metastases from intestinal cancer sources, the incidence of multi-origin cancers has increased in recent years, and dual primary malignant tumors of the liver and colon also exist simultaneously[8]. The postoperative pathology and immunohistochemistry of our patient confirmed that the two tumors were primary tumors without a clear basis for metastasis. Moreover, the canceration of the patient’s original cystadenoma in the tail of the pancreas involved the original intestinal-intestinal anastomosis and led to intestinal obstruction after 2 years of follow-up. This has not been reported in the domestic and international literature. Data have shown that the prognosis of concurrent MPC is worse than that of heterochronous MPC and solitary carcinoma. Moreover, tumor treatment is an important independent prognostic factor.
First, in the face of multi-site tumor lesions, doctors should break through the inertia of diagnosis and treatment thinking, and target screening for multi-source cancer should be considered. They should also avoid thinking subjectively regarding metastatic cancer and conducting non-surgical interventions. Even when it is uncertain whether the patient’s systemic condition can tolerate simultaneous surgeries, active surgical interventions can be considered, and adjuvant treatments can be performed after the surgery. In our case, further exclusion of microscopic metastases and anatomical resection of the liver by fluorescent laparoscopy and three-dimensional reconstruction, intra-operative ultrasound, and fluorescent staining techniques were performed to achieve surgical refinement. Doctors should prioritize malignant lesions. Furthermore, the patient’s condition and malignant foci of the liver and colon can be assessed simultaneously. Pancreatic foci were considered to be benign and asymptomatic, which, on balance, could be temporarily left untreated.
Second, the standardization of multi-source cancer surgery is a key factor in determining patient prognosis. For each part of the tumor, with the help of advanced equipment and under the guarantee of patient safety, doctors can achieve refined R0 resection and carry out standardized lymph node dissection. In the presence of stenosis of the original anastomosis, it is important not to blindly assume that it is caused by the recurrence of the original lesion, which, in this case, was ultimately confirmed to be caused by pancreatic cancer invading the original anastomosis.
In addition, multigenic cancers require strict follow-up and subsequent postoperative treatment. This typical case suggests that after surgery for simultaneous dual-origin cancer, there is still the possibility of heterochronic multiple-origin cancer, which requires clinical attention. Moreover, individualized regimens of immunotherapy, targeting, and chemotherapy can be formulated based on the results of genetic testing. This case suggests that irregular postoperative follow-up and missed visits may prevent physicians from noting the optimal treatment time for heterochronic multigenic cancers.
There is an urgent need to learn more about MPC and clarify the nature of the tumor through advanced surgical means. This can help ensure better diagnosis and treatment, which will benefit patients with MPC by allowing them to receive a more rigorous diagnostic and treatment plan, improving the probability of survival. However, data on the influence of comprehensive treatment after simultaneous multiple primary carcinoma surgeries on the occurrence of metachronous multifocal carcinoma are still lacking.
We would like to extend our appreciation to Xing-Ru Wang and Tian-Xi Liu for their significant contributions to the completion of this study through their encouragement, support, and research assistance.
| 1. | Warren S, Gates O. Multiple Primary Malignant Tumors: A Survey of the Literature and Statistical Study. Am J Cancer. 1932;16:1358-1414. |
| 2. | Izmajłowicz B, Kornafel J, Błaszczyk J. Multiple neoplasms among cervical cancer patients in the material of the lower Silesian cancer registry. Adv Clin Exp Med. 2014;23:433-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Salem A, Abu-Hijlih R, Abdelrahman F, Turfa R, Amarin R, Farah N, Sughayer M, Almousa A, Khader J. Multiple primary malignancies: analysis of 23 patients with at least three tumors. J Gastrointest Cancer. 2012;43:437-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Rosso S, De Angelis R, Ciccolallo L, Carrani E, Soerjomataram I, Grande E, Zigon G, Brenner H; EUROCARE Working Group. Multiple tumours in survival estimates. Eur J Cancer. 2009;45:1080-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 98] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Bittorf B, Kessler H, Merkel S, Brückl W, Wein A, Ballhausen WG, Hohenberger W, Günther K. Multiple primary malignancies: An epidemiological and pedigree analysis of 57 patients with at least three tumours. Eur J Surg Oncol. 2001;27:302-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Powell S, Tarchand G, Rector T, Klein M. Synchronous and metachronous malignancies: analysis of the Minneapolis Veterans Affairs (VA) tumor registry. Cancer Causes Control. 2013;24:1565-1573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Arpaci E, Tokluoglu S, Yetigyigit T, Alkis N. Multiple primary malignancies--a retrospective analysis at a single center in Turkey. Asian Pac J Cancer Prev. 2013;14:769-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Ma L, Chua MS, Andrisani O, So S. Epigenetics in hepatocellular carcinoma: an update and future therapy perspectives. World J Gastroenterol. 2014;20:333-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 77] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |