Published online Feb 15, 2024. doi: 10.4251/wjgo.v16.i2.364
Peer-review started: September 7, 2023
First decision: September 26, 2023
Revised: November 11, 2023
Accepted: December 25, 2023
Article in press: December 25, 2023
Published online: February 15, 2024
Processing time: 148 Days and 6.3 Hours
According to clinical data, a significant percentage of patients experience pain after surgery, highlighting the importance of alleviating postoperative pain. The current approach involves intravenous self-control analgesia, often utilizing opioid analgesics such as morphine, sufentanil, and fentanyl. Surgery for colo
To explore the effects of different anesthesia methods coupled with multi-mode analgesia on postoperative pain in patients with colorectal cancer.
Following the inclusion criteria and exclusion criteria, a total of 126 patients with colorectal cancer admitted to our hospital from January 2020 to December 2022 were included, of which 63 received general anesthesia coupled with multi-mode labor pain and were set as the control group, and 63 received general anesthesia associated with epidural anesthesia coupled with multi-mode labor pain and were set as the research group. After data collection, the effects of postoperative analgesia, sedation, and recovery were compared.
Compared to the control group, the research group had shorter recovery times for orientation, extubation, eye-opening, and spontaneous respiration (P < 0.05). The research group also showed lower Visual analog scale scores at 24 h and 48 h, higher Ramany scores at 6 h and 12 h, and improved cognitive function at 24 h, 48 h, and 72 h (P < 0.05). Additionally, interleukin-6 and interleukin-10 levels were significantly reduced at various time points in the research group compared to the control group (P < 0.05). Levels of CD3+, CD4+, and CD4+/CD8+ were also lower in the research group at multiple time points (P < 0.05).
For patients with colorectal cancer, general anesthesia coupled with epidural anesthesia and multi-mode analgesia can achieve better postoperative analgesia and sedation effects, promote postoperative rehabilitation of patients, improve inflammatory stress and immune status, and have higher safety.
Core Tip: The use of general anesthesia coupled with epidural anesthesia and multimodal analgesia in patients with colorectal cancer can effectively reduce postoperative pain, improve recovery, and enhance immune function. This approach provides superior analgesic and sedative effects, as well as improved inflammatory stress and immune status, ensuring patient safety and promoting postoperative rehabilitation.
- Citation: Tang JC, Ma JW, Jian JJ, Shen J, Cao LL. Effect of different anesthetic modalities with multimodal analgesia on postoperative pain level in colorectal tumor patients. World J Gastrointest Oncol 2024; 16(2): 364-371
- URL: https://www.wjgnet.com/1948-5204/full/v16/i2/364.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i2.364
Analysis of clinical data revealed that approximately 70% of patients experience postoperative pain, and about 40% of patients experience significant pain while in the recovery room[1]. Effective management of postoperative pain is crucial for anesthesiologists. Currently, intravenous patient-controlled analgesia is the primary approach used in postoperative acute pain clinics, with opioids, such as morphine, sufentanil, and fentanyl, being the usual choices[2]. Colorectal cancer is a prevalent malignant tumor that is typically treated surgically. General anesthesia is commonly used for colorectal cancer surgery[3]. Therefore, improving anesthetic management and postoperative pain management programs for colorectal cancer patients can help alleviate perioperative stress and promote postoperative recovery[4].
In this study, we selected patients receiving radical treatment for colorectal cancer at our hospital to analyze the effects of different anesthesia modalities with multimodal analgesia on postoperative pain. The innovation of this research lies in exploring the impact of different anesthesia methods and the combination of multimodal analgesia on postoperative pain in colorectal cancer patients. By comparing the control group with the study group, which received general anesthesia combined with epidural anesthesia and multimodal analgesia, we found that the study group demonstrated better outcomes in terms of postoperative recovery time, pain scores, cognitive function, and inflammation markers. This study not only introduces new methods for postoperative pain management in colorectal cancer patients but also positively impacts postoperative recovery and the inflammatory stress response, thus enhancing safety levels.
In accordance with the inclusion and exclusion criteria, 126 patients with colorectal cancer enrolled in our hospital from January 2020 to December 2022 were included, of which 63 cases received general anesthesia coupled with multimodal paroxysm, set as the control group, and 63 cases treated with general anesthesia coupled with epidural anesthesia in combination with multimodal bouts of pain, selected as the research group. The control group was 45-78 years old, with an average age of 62.12 ± 4.21 years; 38 cases were male, and 25 cases were female; American Society of Anesthesiologists (ASA) classification: 18 cases of grade I, 38 cases of grade II, and 7 cases of grade III. The research group was 46-79 years old, with a mean age of 62.35 ± 4.16 years; 36 males and 27 females; ASA classification: 17 cases of grade I, 38 cases of grade II, and 8 cases of grade III. The comparison of the primary data of the two groups of patients was comparable (P > 0.05).
Inclusion criteria: (1) Patients who received either general anesthesia combined with multimodal analgesia, or general anesthesia combined with epidural anesthesia and multimodal analgesia; (2) Patients diagnosed preoperatively by colonoscopy and cytological testing; (3) Patients who met the indications for surgery and underwent surgical resection; (4) Patients aged between 40 and 80 years; (5) Patients with TNM clinical stage 1-2; (6) Patients who were informed about the study and agreed to participate; and (7) Patients with complete information in the electronic medical record system.
Exclusion criteria: (1) Patients with atrioventricular block; (2) Patients with other malignant tumors or metastases; (3) Patients with severe functional lesions of major organs; (4) Patients with evident manifestations of stoma; and (5) Patients with missing data in the electronic medical record system.
Anesthesia program: Atropine was given 0.5 m before surgery, intravenous access was established for the patient after admission, and a monitor was connected to monitor the patient's heart rate, blood oxygen saturation, electrocardiogram, and non-invasive arterial blood pressure in real-time. The postoperative labor pain was performed with a self-controlled intravenous analgesia pump. The formula was 0.02 μg/kg/mL sufentanil, 2 mg/2 mL tropisetron added into 0.9% sodium chloride injection 100 mL at the background dose of 2 mL per hour, the self-controlled amount was 2 mL each time, and the locking time was 15 min each time. The load was 0.1 μg/kg intravenous sufentanil, plus 2 mg troisetron. After the operation, the multimodal infusion was performed by intravenous analgesia pump with 20 mL of ropivacaine injected into the incision.
Research group: Patients in the research group plan were given general anesthesia and epidural anesthesia, and on this basis, the multi-mode labor pain was performed, the epidural puncture was conducted in the intervertebral space, and 4.5 mg/kg of 2% lidocaine was injected, the patient's reaction was observed, and sufentanil, midazolam, vecuronium and propofol were administered for anesthesia induction after determining that the patient had no abnormal response. After reaching the standard, intubation was performed, and mechanical ventilation was connected after the position was determined and satisfied. Sufentanil and propofol were selected for anesthesia maintenance.
Control group: Patients received general anesthesia coupled with multimodal labor pain, anesthesia induction, and multimodal labor pain in the same research group.
Others: Patients in both groups were given intermittent intravenous injections of vecuronium bromide and fentanyl during operation to maintain muscle relaxation and intraoperative fluid supplementation in accordance with patients' needs. The analgesic pump was connected following the procedure.
General characteristics: Postoperative recovery of patients in the two groups was included, including extubation time, spontaneous breathing recovery time, eye-opening time upon exhalation, and orientation recovery time.
Pain during the perioperative period: Visual analog scale (VAS)[5] was applied for evaluation, and the evaluation time was preoperative, postoperative 6 h, 12 h, 24 h, and 48 h, respectively. The score was 0-10 points; 7-10 was classified as unbearable pain, 4-6 as moderate pain, 1-3 as mild pain, and 0 as no pain.
Sedation effect: Ramsay score[6] was applied for evaluation, divided into 1-6 grades, and assigned 1-6 points, respe
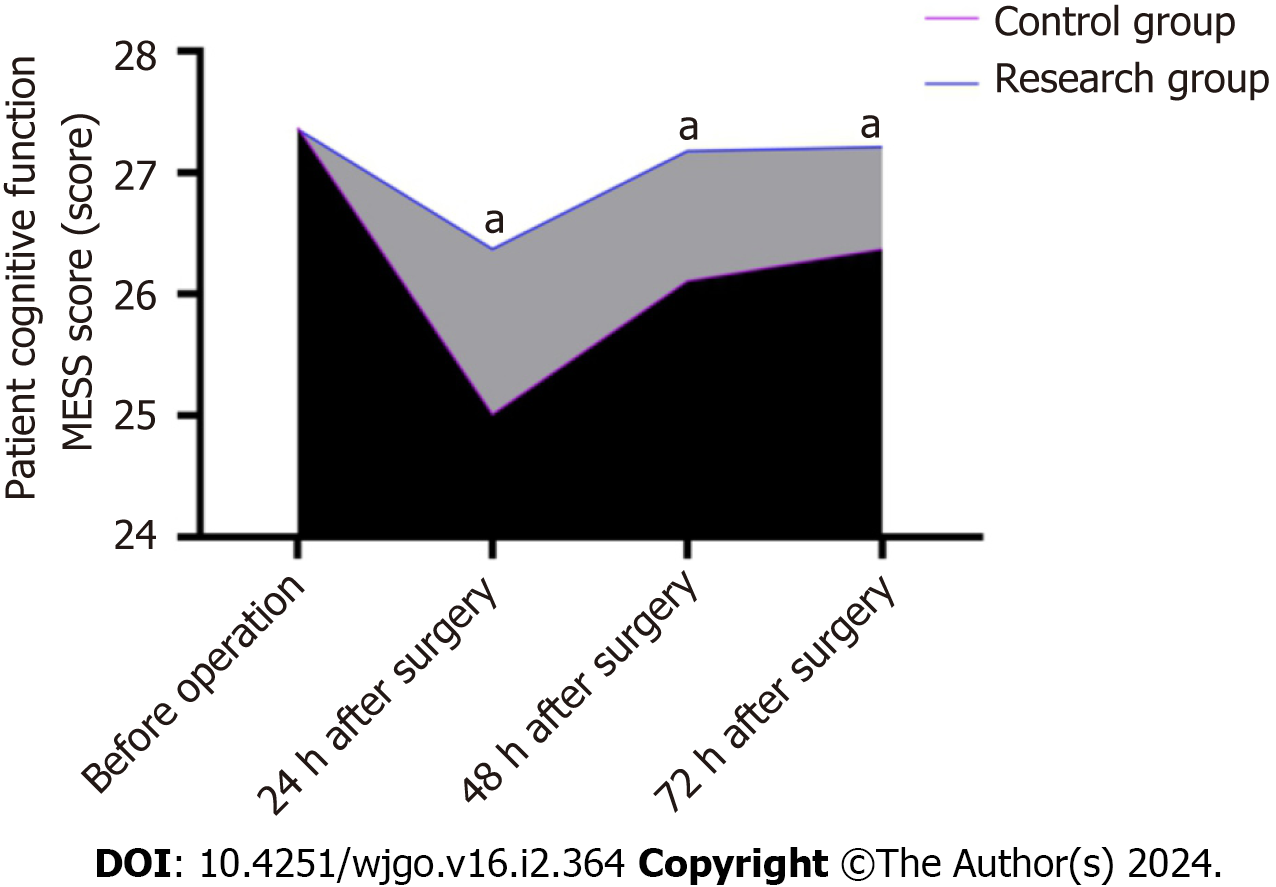
Cognitive function: Mangled Extremity Severity Score (MESS) score[7] was applied for cognitive function assessment, scoring 30. The higher the patient score, the more the postoperative cognitive function recovery. The evaluation time was pre-operation, 24 h, 48 h, and 72 h, respectively.
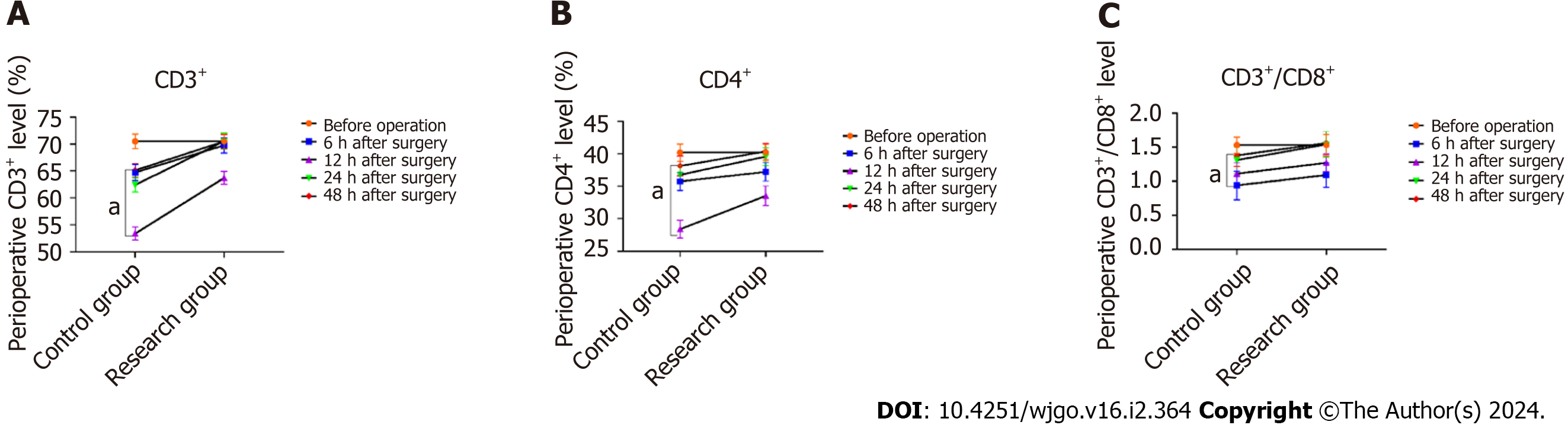
Laboratory index detection: Venous blood of the upper limb of the patient was collected before surgery, 6, 12, 24, 48 h following the procedure, and the level of T lymphocyte subsets (CD3+, CD4+, CD4+/CD8+) of the patient was detected by automatic cell analyzer. Part of the blood pressure was centrifugally separated, and serum was obtained. Tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6) and interleukin-10 (IL-10) were detected by ELISA.
SPSS22.0 software was applied for data analysis, and the count data were expressed as n (%); the χ2 test was used for comparison between groups; the measurement data obeying normal distribution were marked as (mean ± SD), and the SNK-q test was used for two-way comparison between groups. P < 0.05 represents statistical significance.
After comparison, there were no statistical differences in age, ASA grade, blood pressure, gender, and body mass index between the control group and the research group (P > 0.05; Table 1, Supplementary material).
| Item | Control group (n = 63) | Research group (n = 63) | X2/F | P value | |
| Age (yr) | 62.12 ± 4.21 | 62.35 ± 4.16 | 0.308 | 0.758 | |
| Gender (example) | Male | 38 (60.32) | 36 (57.15) | 0.043 | 0.835 |
| Female | 25 (39.69) | 27 (42.86) | |||
| Body mass index (kg/m2) | 25.34 ± 2.53 | 25.41 ± 2.73 | 0.149 | 0.882 | |
| Systolic pressure (mmHg) | 146.23 ± 21.25 | 144.98 ± 19.45 | 0.344 | 0.731 | |
| Diastolic blood pressure (mmHg) | 94.25 ± 21.91 | 94.89 ± 18.94 | 0.175 | 0.861 | |
| ASA classification (example) | Level I | 18 (28.58) | 17 (26.99) | 0.095 | 0.953 |
| Level II | 38 (60.32) | 38 (60.32) | |||
| Level III | 7 (11.12) | 8 (12.70) |
In comparison to the control group, orientation restoration time, extubation time, eye-opening time after exhalation, and spontaneous respiration recovery time were remarkably shortened (P < 0.05; Table 2).
| Group | Number of cases | Directional recovery time | Extubation time | Call eye opening time | Recovery time for spontaneous breathing |
| Research group | 63 | 25.34 ± 4.13 | 25.23 ± 2.32 | 15.82 ± 2.15 | 16.74 ± 2.17 |
| Control group | 63 | 27.67 ± 4.91 | 29.23 ± 3.15 | 19.82 ± 2.41 | 17.59 ± 2.17 |
| t value | / | 2.883 | 8.116 | 9.831 | 2.198 |
| P value | / | 0.005 | < 0.001 | < 0.001 | 0.030 |
In comparison to the control group, VAS scores of patients in the research group were remarkably decreased at 24 h and 48 h following the procedure; the difference was statistically significant (P < 0.05); Ramany scores of patients in the research group were remarkably increased at 6 h and 12 h following the procedure (P < 0.05; Figure 1).
In comparison to the control group, the cognitive MESS score of patients in the research group increased remarkably at 24 h, 48 h, and 72 h following the procedure, and the cognitive function of patients in the research group was more stable (P < 0.05; Figure 2).
In comparison to the control, IL-6 Levels of patients in the research group were remarkably decreased at 6, 12, 24, 48 h following the procedure (P < 0.05); In comparison to the control, the IL-10 Level in the research group was remarkably decreased at 12 h, 24 h, and 48 h following the procedure (P < 0.05). There was no significant change in TNF-α level at different times (P > 0.05; Figure 3).
In comparison to the research group, the level of CD3+ in the control group was remarkably decreased at 6, 12, 24, 48 h following the procedure (P < 0.05). In comparison to the research group, CD4+ levels in the research group were remarkably decreased at 6, 12, 24, 48 h following the procedure (P < 0.05). In comparison to the research group, the levels of CD4+/CD8+ in the research group were remarkably decreased at 6, 12, 24, 48 h following the procedure (P < 0.05).
Postoperative pain is a common complication after surgery and can cause discomfort, hinder patients' recovery, and increase the risk of complications such as lung infection[8]. Various factors contribute to postoperative pain, including surgical trauma and stress reactions[9]. Previous studies have shown that a single mechanism alone cannot explain the occurrence of pain[10]. Therefore, adopting a single analgesic program may not achieve the desired pain relief.
To address this issue, implementing a multi-mode analgesia program has been shown to effectively improve postoperative pain and target pain caused by different mechanisms and factors[11]. This approach involves using a combination of drugs or drug regimens to ensure adequate pain relief while minimizing the use of opioids. By targeting different pain pathways and mechanisms, a multimodal analgesia program can enhance patients' rehabilitation and overall postoperative outcomes.
Combining effective intraoperative and postoperative analgesia programs can achieve better analgesia effects, which is critical to promoting the postoperative rehabilitation of surgical patients[11]. Patients in the research group were coupled with epidural anesthesia based on general anesthesia and coupled with multi-mode analgesia. The results showed that spontaneous breathing and extubation time following the procedure were remarkably shortened compared to patients who only underwent general anesthesia coupled with multi-mode analgesia. This result may be because the combination of epidural anesthesia and multi-mode analgesic intervention based on general anesthesia remarkably reduced the amount of propofol in patients, which encouraged patients to resume spontaneous breathing as soon as possible and shortened the intubation time[12]. Epidural anesthesia can effectively reduce the occurrence of intercostal muscle paralysis and inhibit the major nerve damage caused by intraoperative incision and extubation stimulation[13]. This study analyzed the postoperative analgesia and sedation effects of the two groups of patients, and the results showed that the postoperative analgesia and sedation effects of the patients in the research group were better, which further confirmed that general anesthesia coupled with epidural anesthesia coupled with multi-mode analgesia could achieve better postoperative analgesia and sedation effects.
Anesthesia and surgical treatment cause the body to release various inflammatory factors, and inflammatory factors enter the blood, cause systemic inflammation, affect postoperative rehabilitation of patients, and are common factors leading to postoperative pain[14]. The body's immune status is a crucial factor in evaluating the postoperative rehabilitation ability of patients. The vital core cells in the immune response process are T lymphocytes, and their level is closely related to the disease's severity and the body's immune status[15]. This study analyzed the levels of IL-6, IL-10, TNF-α, and immune factors CD3+, CD4+, and CD4+/CD8+ in the two groups. The results showed that inflammatory factors were generally reduced in the research group, while the levels of immune factors were higher than those in the control group. It is suggested that the postoperative recovery of general anesthesia coupled with epidural anesthesia is more ideal than that of general anesthesia. MESS score is a commonly used scale for the cognitive function of patients. This study compared the MMSE scores of patients in the two groups, and the results showed that patients in the research group had a higher MESS score, suggesting that anesthesia and analgesia programs for patients in the research group could protect cognitive function and have more increased safety.
The limitations of this study are mainly as follows: (1) Limited sample size: This study only included 126 colorectal cancer patients who received treatment in the hospital from January 2020 to December 2022. The research findings may not be generalizable to other populations; (2) Single-center study: This study was conducted only at one hospital, which may limit the representativeness and generalizability of the research results; (3) Non-randomized grouping: The grouping of the study and control groups was not randomized, which may introduce potential bias and affect the accuracy of the research results; (4) Retrospective study design: This study used a retrospective study design, and the research results are susceptible to recall bias and information retrieval bias, leading to potential issues such as memory and information retrieval errors; (5) Specific to colorectal cancer patients: This study focused only on colorectal cancer patients, and the findings may not be applicable to other types of surgeries and diseases; and (6) Subjective assessment of outcomes: Some outcomes, such as VAS scores, Ramany scores, and cognitive function improvement, are based on self-reports by patients or subjective evaluations by doctors, which may be subjective and influenced by individual differences.
For patients with colorectal cancer, general anesthesia coupled with epidural anesthesia coupled with multi-mode analgesia can achieve better postoperative analgesia and sedation effects, promote postoperative rehabilitation of patients, improve the inflammatory stress and immune state of the body, and have higher safety.
Postoperative pain management is crucial in patient care, as a significant number of patients experience pain after surgery. The current approach involves intravenous self-control analgesia using opioid analgesics. Surgery for colorectal cancer typically involves general anesthesia, and optimizing anesthesia management and postoperative analgesic programs can reduce stress and enhance recovery.
The study aims to assess the impact of different anesthesia modalities with multimodal analgesia on postoperative pain in patients with colorectal cancer. Understanding the effects of these combinations can help improve pain management strategies and patient outcomes.
The objective is to explore the effects of different anesthesia methods coupled with multi-mode analgesia on post
A total of 126 patients with colorectal cancer were included, with 63 in the control group receiving general anesthesia coupled with multi-mode labor pain, and 63 in the research group receiving general anesthesia associated with epidural anesthesia coupled with multi-mode labor pain. Data on postoperative analgesia, sedation, and recovery were collected and compared between the two groups.
The research group had significantly shorter recovery times for orientation, extubation, eye-opening, and spontaneous respiration compared to the control group. They also reported lower pain intensity scores and reduced opioid consum
Results suggest that combining epidural anesthesia with multi-mode analgesia may lead to improved postoperative pain management in patients with colorectal cancer compared to general anesthesia alone. This finding emphasizes the importance of optimizing anesthesia modalities to enhance patient comfort and recovery.
Future research could investigate the long-term effects and potential complications associated with different anesthesia modalities coupled with multi-mode analgesia. Additionally, exploring the impact of these techniques on other surgical procedures could provide valuable insights into pain management strategies.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jeronimo C, Portugal; Liu J, China S-Editor: Lin C L-Editor: A P-Editor: Zhang YL
| 1. | Aliev VA, Bashankaev BN, Loria IZ, Glabay VP, Yavorovsky AG, Shavgulidze KB, Yunusov BT. Non-opioid multimodal anesthesia in the surgical treatment of colorectal cancer. Khirurgiia (Mosk). 2019;54-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 2. | Ashouri M, Karvandian K, Ataie-Ashtiani Z, Mohammadzadeh N. Continuous epidural catheter for anaesthesia management and post-op pain relief in colorectal surgery, complicated by epidural haematoma and bilateral paraplegia: A case report. Int J Surg Case Rep. 2021;83:106039. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 3. | Kay A, Marjon N, Guerra R, Alvarez E, Chapman J, Swanson M, Chen L, Ueda S. Surgeon placed transverse abdominis plane (TAP) blocks as an alternative to thoracic epidurals. Gynecol Oncol. 2022;164:9. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Carli F, Trudel JL, Belliveau P. The effect of intraoperative thoracic epidural anesthesia and postoperative analgesia on bowel function after colorectal surgery: a prospective, randomized trial. Dis Colon Rectum. 2001;44:1083-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 142] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Khashan AS. Labor epidural anesthesia associated with autism. J Pediatr. 2021;232:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Chen WK, Ren L, Wei Y, Zhu DX, Miao CH, Xu JM. General anesthesia combined with epidural anesthesia ameliorates the effect of fast-track surgery by mitigating immunosuppression and facilitating intestinal functional recovery in colon cancer patients. Int J Colorectal Dis. 2015;30:475-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Faisal M, Schäfer CN, Myrelid P, Winberg ME, Söderholm JD, Keita ÅV, Eintrei C. Effects of analgesic and surgical modality on immune response in colorectal cancer surgery. Surg Oncol. 2021;38:101602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Schmid F, Dahlmann M, Röhrich H, Kobelt D, Hoffmann J, Burock S, Walther W, Stein U. Calcium-binding protein S100P is a new target gene of MACC1, drives colorectal cancer metastasis and serves as a prognostic biomarker. Br J Cancer. 2022;127:675-685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Falk W, Magnuson A, Eintrei C, Henningsson R, Myrelid P, Matthiessen P, Gupta A. Comparison between epidural and intravenous analgesia effects on disease-free survival after colorectal cancer surgery: a randomised multicentre controlled trial. Br J Anaesth. 2021;127:65-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 10. | Berlin C, Cottard F, Willmann D, Urban S, Tirier SM, Marx L, Rippe K, Schmitt M, Petrocelli V, Greten FR, Fichtner-Feigl S, Kesselring R, Metzger E, Schüle R. KMT9 Controls Stemness and Growth of Colorectal Cancer. Cancer Res. 2022;82:210-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 11. | Zorzi M, Battagello J, Selby K, Capodaglio G, Baracco S, Rizzato S, Chinellato E, Guzzinati S, Rugge M. Non-compliance with colonoscopy after a positive faecal immunochemical test doubles the risk of dying from colorectal cancer. Gut. 2022;71:561-567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 55] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 12. | Hasselager RP, Hallas J, Gögenur I. Epidural Analgesia and Recurrence after Colorectal Cancer Surgery: A Danish Retrospective Registry-based Cohort Study. Anesthesiology. 2022;136:459-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 13. | Jaloun HE, Lee IK, Kim MK, Sung NY, Turkistani SAA, Park SM, Won DY, Hong SH, Kye BH, Lee YS, Jeon HM. Influence of the Enhanced Recovery After Surgery Protocol on Postoperative Inflammation and Short-term Postoperative Surgical Outcomes After Colorectal Cancer Surgery. Ann Coloproctol. 2020;36:264-272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Lederman D, Easwar J, Feldman J, Shapiro V. Anesthetic considerations for lung resection: preoperative assessment, intraoperative challenges and postoperative analgesia. Ann Transl Med. 2019;7:356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Liu Q, Lin JY, Zhang YF, Zhu N, Wang GQ, Wang S, Gao PF. Effects of epidural combined with general anesthesia vs general anesthesia on quality of recovery of elderly patients undergoing laparoscopic radical resection of colorectal cancer: A prospective randomized trial. J Clin Anesth. 2020;62:109742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |