Published online Oct 15, 2024. doi: 10.4251/wjgo.v16.i10.4138
Revised: August 18, 2024
Accepted: August 26, 2024
Published online: October 15, 2024
Processing time: 70 Days and 1.9 Hours
The metastatic tumors in the small intestine secondary to extra-abdominal/extra-pelvic malignancy are extremely rare. However, the small intestine metastases are extremely prone to misdiagnosis and missed diagnosis due to the lack of specific clinical manifestations and examination methods, thus delaying its treatment. Therefore, in order to improve clinical diagnosis and treatment capabilities, it is necessary to summarize its clinical pathological characteristics and prognosis.
To summarize the clinicopathological characteristics of patients with small inte
The clinical data of patients with small intestinal metastases from extra-abdominal/extra-pelvic malignancy were retrieved and summarized, who admitted to and treated in the Air Force Medical Center, Chinese People’s Liberation Army. Then descriptive statistics were performed on the general conditions, primary tumors, secondary tumors in the small intestine, diagnosis and treatment processes, and prognosis.
Totally 11 patients (9 males and 2 females) were enrolled in this study, including 8 cases (72.3%) of primary lung cancer, 1 case (9.1%) of malignant lymphoma of the thyroid, 1 case (9.1%) of cutaneous malignant melanoma, and 1 case (9.1%) of testicular cancer. The median age at the diagnosis of primary tumors was 57.9 years old, the median age at the diagnosis of metastatic tumors in the small intestine was 58.81 years old, and the average duration from initial diagnosis of primary tumors to definite diagnosis of small intestinal metastases was 9 months (0-36 months). Moreover, small intestinal metastases was identified at the diagnosis of primary tumors in 4 cases. The small intestinal metastases were distributed in the jejunum and ileum, with such clinical manifestations as hematochezia (5, 45.4%) and abdominal pain, vomiting and other obstruction (4, 36.4%). In addition, 2 patients had no obvious symptoms at the diagnosis of small intestinal metastases, and 5 patients underwent radical resection of small intestinal malignancies and recovered well after surgery. A total of 3 patients did not receive subsequent treatment due to advanced conditions.
Small intestinal metastases of extra-abdominal/extra-pelvic malignancy is rare with high malignancy and great difficulty in diagnosis and treatment. Clinically, patients with extra-abdominal/extra-pelvic malignancy should be alert to the occurrence of this disease, and their prognosis may be improved through active surgery combined with standard targeted therapy.
Core Tip: The metastatic tumors in the small intestine secondary to extra-abdominal/extra-pelvic malignancy are extremely rare. This study intends to identify the clinicopathological characteristics of small intestinal metastases from extra-abdominal/extra-pelvic malignancy. Eleven patients with small intestinal metastases from extra-abdominal/extra-pelvic malignancy diagnosed and treated in the Air Force Medical Center from 2005 to 2024 were enrolled. The results showed that small intestinal metastases from extra-abdominal/extra-pelvic malignancy is rare in clinic, with high malignancy and great difficulty in diagnosis and treatment. Clinically, patients with extra-abdominal/extra-pelvic malignancy should be alert to the occurrence of this disease, and their prognosis may be improved through active surgery combined with standard targeted therapy.
- Citation: Zhang Z, Liu J, Yu PF, Yang HR, Li JY, Dong ZW, Shi W, Gu GL. Clinicopathological analysis of small intestinal metastasis from extra-abdominal/extra-pelvic malignancy. World J Gastrointest Oncol 2024; 16(10): 4138-4145
- URL: https://www.wjgnet.com/1948-5204/full/v16/i10/4138.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i10.4138
The small intestine is the longest part of the digestive tract but rich in lymphoid tissues and highly proliferative epithelial cells, so the primary malignant tumors in the small intestine have a prominently lower incidence rate than other digestive tract tumors, merely accounting for 5% of gastrointestinal tract tumors[1]. The metastatic tumors in the small intestine secondary to extra-abdominal/extra-pelvic malignancy are extremely rare in clinic. However, metastatic tumors in the small intestine are extremely prone to misdiagnosis and missed diagnosis due to the lack of specific clinical manifestations and examination methods, thus delaying its treatment[2]. A retrospective study was conducted on the clinical data of patients with small intestinal metastasis of extra-abdominal/extra-pelvic malignancy, who were diagnosed and treated in the Air Force Medical Center, People’s Liberation Army, a military-wide diagnosis and treatment center of small intestinal diseases, in the last two decades, and their clinicopathological characteristics were summarized and analyzed in combination with the literature, in the hope of deepening clinical understanding of the rare small intestinal metastasis of extra-abdominal/extra-pelvic malignancy and improving the diagnosis and treatment ability.
The cases diagnosed with “secondary malignant tumor in the small intestine” or “small intestinal malignancy” or “small intestinal cancer” from 2005 to 2024 in the hospital were screened from the EMRS clinician workstation system operated by the Air Force Medical Center, Chinese People’s Liberation Army (PLA). Through the review of their medical records and auxiliary examination results, the cases of “primary malignant tumor in the small intestine” and metastasis of primary abdominal/pelvic malignancy to the small intestine were excluded. As a result, totally 11 patients were enrolled. Subsequently, the clinical data of these patients were retrospectively researched, and descriptive statistics were conducted on their general conditions, primary tumors, secondary tumors in the small intestine, diagnosis and treatment processes, and prognosis.
In the past 20 years, 193 patients with small intestinal malignancies have been treated in the Air Force Medical Center, Chinese PLA; of which 11 patients (5.7%) were pathologically diagnosed with small intestinal metastasis from extra-abdominal and pelvic malignancies. There were 9 males and 2 females, including 8 cases (72.3%) of primary lung cancer, 1 case (9.1%) of malignant lymphoma of the thyroid, 1 case (9.1%) of cutaneous malignant melanoma, and 1 case (9.1%) of testicular cancer. The median age at the diagnosis of primary tumors was 57.9 years old. Except for one patient who was diagnosed with small cell lung cancer concomitant with metastases to the small intestine, mediastinal lymph node, chest wall, abdominal cavity and retroperitoneum and received no treatment, the remaining 10 patients underwent stan
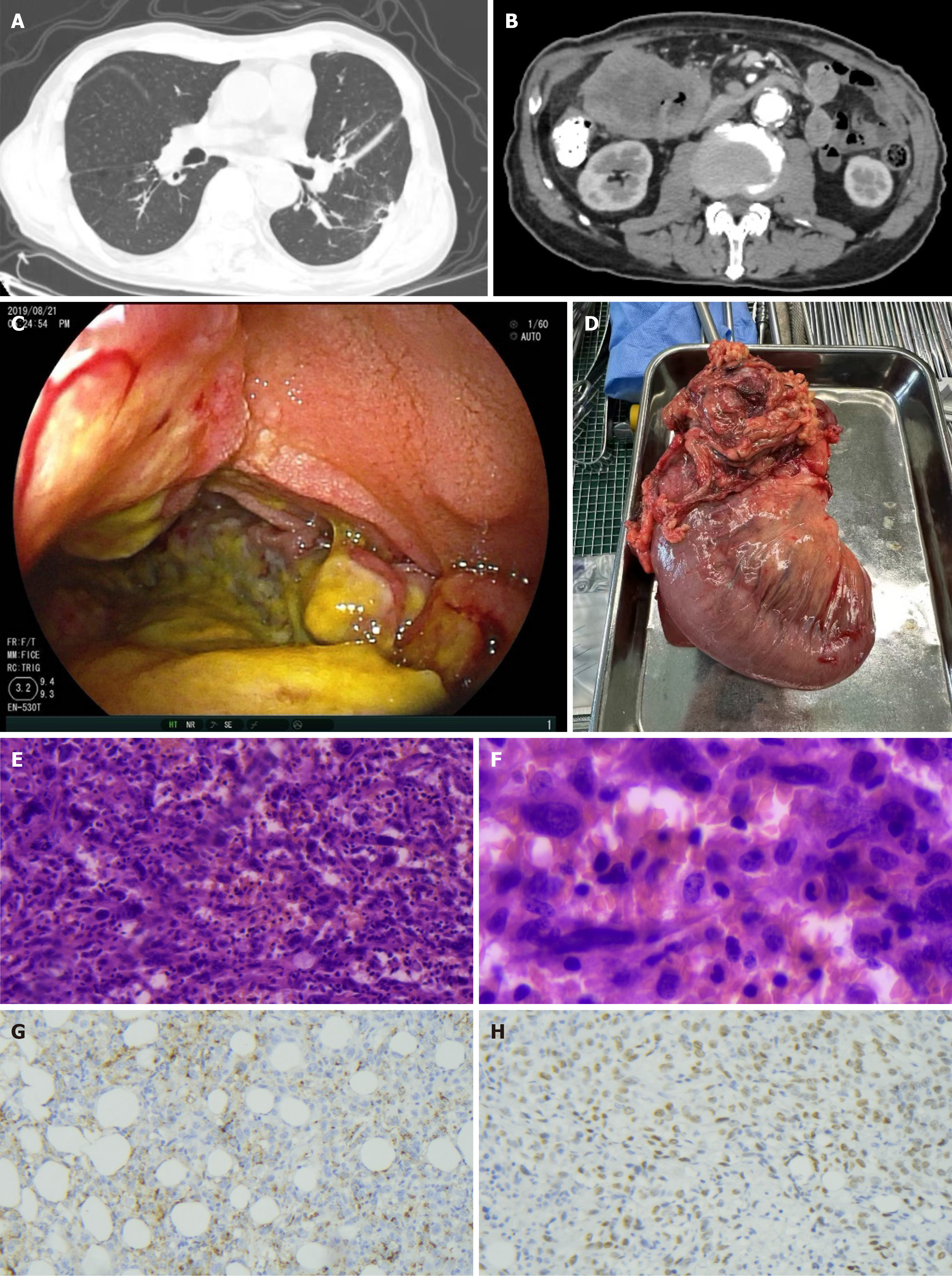
Averagely, the small intestinal metastases were distributed in the jejunum and ileum, without an obvious tendency of concentration, and the main clinical manifestations included gastrointestinal bleeding [5 (45.4%)], abdominal pain, vomiting and other obstruction [4 (36.4%)], and no obvious symptoms were observed in 2 cases at the diagnosis of small intestinal metastasis. Additionally, direct resection of small intestinal metastases was performed for 6 cases. Totally 3 cases underwent small intestinal endoscopy and tissue biopsy under the endoscope, 2 of which received resection of small intestinal metastases after definite pathological diagnosis. Targeted therapy was adopted for 1 case. The patient untreated with surgery died of gastrointestinal bleeding. No perioperative death occurred among the 10 surgically treated patients, with the therapeutic goal of relieving gastrointestinal symptoms achieved (Figure 1 and Table 1). All patients were followed up as of June 2024, and three of them are currently alive, with an overall survival of 5-42 months and oncologically assessed stable disease. The median survival of the 8 dead patients was 16.5 months (10 days to 38 months) from the time of diagnosis of primary tumors.
| Patient | Sex | Primary tumor | Treatment method for primary tumor | Age at diagnosis of primary tumor (year) | Complication of metastasis to other systems | History of other tumors | Family history | Age at diagnosis of small intestinal metastasis (year) | Duration (months) | Clinical symptom | Site of small intestinal metastasis | Nature of metastatic cancer in the small intestine | Management of secondary small intestinal lesions | Follow-up | Overall survival (months) |
| 1 | Male | Lung cancer (poorly differentiated non-small cell cancer) | Surgery + chemotherapy | 72 | No | Gingival squamous cell carcinoma in 2006 | No | 73 | 7 | Hematochezia | Jejunum (about 20 cm from Treitz ligament) | Intestinal metastasis of lung adenocarcinoma | Surgery | Death | 11 |
| 2 | Male | Lung cancer (poorly to moderately differentiated squamous cell carcinoma) | Chemotherapy + immunotherapy | 65 | No | No | No | 65 | 0 | Abdominal pain and obstruction | Ileum | Metastatic squamous cell carcinoma | Surgery | Survival | 9 |
| 3 | Male | Non-Hodgkin’s follicular lymphoma of the thyroid | Surgery + chemotherapy | 59 | No | No | Bladder cancer of his father | 59 | 0 | No obvious symptoms | Ileum | Metastasis of non-Hodgkin’s lymphoma | Surgery | Survival | 42 |
| 4 | Male | Malignant melanoma of the lumbar region | Surgery + chemotherapy | 54 | No | No | No | 57 | 36 | Abdominal pain and obstruction | Jejunum (100 cm from pylorus) | Metastatic malignant melanoma | Tissue biopsy under the endoscope + chemotherapy | Death | 38 |
| 5 | Male | Testicular cancer (chorionic epithelioma) | Chemotherapy | 49 | No | No | No | 49 | 0 | Hematochezia | Jejunum (120 cm from pylorus) | Metastasis of choriocarcinoma in germ cell tumors | Surgery | Survival | 5 |
| 6 | Male | Lung cancer (squamous cell carcinoma) | Radiotherapy + chemotherapy | 50 | Mediastinal lymph node metastasis of lung cancer | No | No | 53 | 26 | Hematochezia | Jejunum (60 cm from Treitz ligament) | Metastasis of lung squamous cell carcinoma | Surgery | Death | 32 |
| 7 | Male | Lung cancer (poorly to moderately differentiated small cell cancer) | Untreated | 56 | Metastasis to mediastinal lymph node, chest wall, abdominal cavity, and retroperitoneum | No | No | 56 | 0 | Hematochezia | Jejunum-ileum junction | / | Untreated | Death | 0.3 |
| 8 | Male | Lung cancer (poorly differentiated non-small cell cancer) | Radiotherapy | 75 | No | No | No | 75 | 4 | Abdominal pain and obstruction | Terminal ileum | Long metastasis of lung adenocarcinoma | Tissue biopsy under the endoscope | Death | 4 |
| 9 | Male | Lung cancer (neuroendocrine cancer) | Surgery | 71 | Abdominal cavity, retroperitoneum, and mediastinum | No | No | 73 | 14 | Abdominal pain and obstruction | Terminal ileum | Metastasis of cell neuroendocrine cancer | Surgery | Death | 18 |
| 10 | Female | Lung cancer (large cell cancer) | Targeted therapy + radiotherapy | 49 | No | No | No | 50 | 13 | Abdominal pain and hematochezia | Jejunum (180 cm from pylorus) | Metastasis of lung cell cancer | Tissue biopsy under the endoscope + surgery | Death | 21 |
| 11 | Female | Lung cancer (poorly differentiated non-small cell cancer) | Targeted therapy | 37 | Metastasis to bone, mediastinum, and abdominal wall | No | No | 37 | 9 | No obvious symptoms | Jejunum (120 cm from pylorus) | Metastasis of lung adenocarcinoma | Targeted therapy | Death | 15 |
Primary small intestinal tumors rarely occur in clinic[3], whose incidence rate is 50 times lower than that of colorectal cancer[4]. Due to the lack of specific clinical manifestations and typical early symptoms, as well as the difficult operation of small intestinal endoscopy, small intestinal malignancy has generally developed into an advanced stage at diagnosis, and its prognosis is worse than that of other related malignancies (e.g., colorectal cancer) on average[5,6]. The metastasis from extra-abdominal/extra-pelvic malignancy to the small intestine is even rarer, with greater difficulty in diagnosis and treatment, and poorer prognosis. In this study, the overall prognosis was unsatisfactory despite aggressive treatment. Only 3 out of the 11 cases have survived so far, with a median survival of 13 months.
It was uncovered through a study[7] that squamous cell carcinoma is the most common histologic type of lung cancer with gastrointestinal metastasis, and the esophagus and the small intestine are the top two common sites for metastasis. According to a retrospective analysis[8], the small intestine (59.6%) and the colon and rectum (25.6%) are the two most vulnerable organs to gastrointestinal metastasis from lung cancer. It was also concluded that more than half of the patients died within 3 months after the diagnosis of gastrointestinal metastasis, with a median survival of merely 2.8 months. A literature review was conducted by incorporating 57 case reports and 3 retrospective studies from the PubMed database[9], indicating that the prevalence of small intestinal metastases from lung cancer is 2.6% to 10.7%, the duration from the diagnosis of the primary tumors to the manifestation of intestinal metastasis ranges from 2 weeks to 4 years, and that the median survival of the followed up 79 patients is 2.3 months. Only 1 survived during the follow-up period, but the remaining 7 patients had a median survival of up to 13 months among 8 patients who suffered from primary lung cancer, significantly longer than that previously reported in the literature. It suggests that although the overall prognosis of these patients is poor, some are still likely to benefit from aggressive treatment.
As denoted in a study[10], among the extra-abdominal/extra-pelvic malignancies, lung cancer, breast cancer, and melanoma metastasize to the small intestine most frequently. Dwivedi et al[11] reported a case of small intestinal metastases from breast cancer in an elderly female patient, and the metastatic tumors in the small intestine were surgically resected after definite diagnosis, relieving the symptoms of gastrointestinal obstruction and providing an opportunity for subsequent chemotherapy. Gakuhara et al[12] reported that a patient with testicular seminoma ac
As a medical center for small intestinal diseases in China that took the lead in applying electronic small intestinal endoscopy, Air Force Medical Center, Chinese PLA has spent 20 years accumulating 11 cases of small intestinal meta
There are few cases of small intestinal metastasis of extra-abdominal/extra-pelvic malignancy in clinic, which is characterized by high malignancy and great difficulty in diagnosis and treatment. Clinically, the sufferers of extra-abdominal/extra-pelvic malignancy should be alerted to the occurrence of this disease and actively undergo surgery to eliminate gastrointestinal obstruction, bleeding, perforation and other serious complications, and their survival can be extended in combination with other targeted treatments.
| 1. | Mousavi SE, Ilaghi M, Mahdavizadeh V, Ebrahimi R, Aslani A, Yekta Z, Nejadghaderi SA. A population-based study on incidence trends of small intestine cancer in the United States from 2000 to 2020. PLoS One. 2024;19:e0307019. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Takeda H, Yamamoto H, Oikawa R, Umemoto K, Arai H, Mizukami T, Ogawa K, Uchida Y, Nagata Y, Kubota Y, Doi A, Horie Y, Ogura T, Izawa N, Moore JA, Sokol ES, Sunakawa Y. Genomic Profiling of Small Intestine Cancers From a Real-World Data Set Identifies Subgroups With Actionable Alterations. JCO Precis Oncol. 2024;8:e2300425. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Assumpção P, Khayat A, Araújo T, Barra W, Ishak G, Cruz A, Santos S, Santos Â, Demachki S, Assumpção P, Calcagno D, Santos N, Assumpção M, Moreira F, Santos A, Assumpção C, Riggins G, Burbano R. The Small Bowel Cancer Incidence Enigma. Pathol Oncol Res. 2020;26:635-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Bozhkov V, Magjov R, Chernopolsky P, Arnaudov P, Plachkov I, Ivanov T. Small intestinal tumors. Khirurgiia (Sofiia). 2015;81:4-8. [PubMed] |
| 5. | de Bree E, Rovers KP, Stamatiou D, Souglakos J, Michelakis D, de Hingh IH. The evolving management of small bowel adenocarcinoma. Acta Oncol. 2018;57:712-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, Cohen SA, Cooper HS, Deming DA, Garrido-Laguna I, Grem JL, Hoffe SE, Hubbard J, Hunt S, Kamel A, Kirilcuk N, Krishnamurthi S, Messersmith WA, Meyerhardt J, Miller ED, Mulcahy MF, Nurkin S, Overman MJ, Parikh A, Patel H, Pedersen KS, Saltz LB, Schneider C, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Johnson-Chilla A, Gregory KM, Gurski LA. Small Bowel Adenocarcinoma, Version 1.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2019;17:1109-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 113] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 7. | Dong XY, Li YL, Yao JN, Zhang LF. [The clinical characteristics of metastatic tumors in small intestine]. Zhonghua Yi Xue Za Zhi. 2024;104:2003-2006. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Antler AS, Ough Y, Pitchumoni CS, Davidian M, Thelmo W. Gastrointestinal metastases from malignant tumors of the lung. Cancer. 1982;49:170-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Hu Y, Feit N, Huang Y, Xu W, Zheng S, Li X. Gastrointestinal metastasis of primary lung cancer: An analysis of 366 cases. Oncol Lett. 2018;15:9766-9776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Di JZ, Peng JY, Wang ZG. Prevalence, clinicopathological characteristics, treatment, and prognosis of intestinal metastasis of primary lung cancer: a comprehensive review. Surg Oncol. 2014;23:72-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Dwivedi RC, Kazi R, Agrawal N, Chisholm E, St Rose S, Elmiyeh B, Rennie C, Pepper C, Clarke PM, Kerawala CJ, Rhys-Evans PH, Harrington KJ, Nutting CM. Comprehensive review of small bowel metastasis from head and neck squamous cell carcinoma. Oral Oncol. 2010;46:330-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Gakuhara A, Kitani K, Terashita D, Tomihara H, Fukuda S, Ota K, Hashimoto K, Ishikawa H, Hida J, Wakasa T, Kimura Y. [Small Bowel Metastasis of Breast Cancer-A Case Report]. Gan To Kagaku Ryoho. 2021;48:1737-1739. [PubMed] |
| 13. | Higashi D, Ishibashi Y, Tamura T, Nii K, Egawa Y, Koga M, Tomiyasu T, Harimura T, Tanaka R, Futatsuki R, Noda S, Futami K, Maekawa T, Takaki Y, Hirai F, Matsui T. Clinical features of and chemotherapy for cancer of the small intestine. Anticancer Res. 2010;30:3193-3197. [PubMed] |
| 14. | Wang M, Chen G, Luo J, Fan Z, Liu Y, Xie C, Gong Y. Case Report: Genetic profiling of small intestine metastasis from poorly differentiated non-small cell lung cancer: report of 2 cases and literature review of the past 5 years. Front Oncol. 2023;13:1265749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Green J, Schlieve CR, Friedrich AK, Baratta K, Ma DH, Min M, Patel K, Stein D, Cave DR, Litwin DE, Cahan MA. Approach to the Diagnostic Workup and Management of Small Bowel Lesions at a Tertiary Care Center. J Gastrointest Surg. 2018;22:1034-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Niiya F, Tamai N, Yamawaki M, Noda J, Azami T, Takano Y, Nishimoto F, Nagahama M. Efficacy and safety of uncovered self-expandable metal stents for distal malignant biliary obstruction in unresectable non-pancreatic cancer. DEN Open. 2025;5:e383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 17. | Stewart CL, Warner S, Ito K, Raoof M, Wu GX, Kessler J, Kim JY, Fong Y. Cytoreduction for colorectal metastases: liver, lung, peritoneum, lymph nodes, bone, brain. When does it palliate, prolong survival, and potentially cure? Curr Probl Surg. 2018;55:330-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 169] [Article Influence: 24.1] [Reference Citation Analysis (0)] |