Published online Jan 15, 2024. doi: 10.4251/wjgo.v16.i1.244
Peer-review started: November 4, 2023
First decision: November 22, 2023
Revised: December 6, 2023
Accepted: December 18, 2023
Article in press: December 18, 2023
Published online: January 15, 2024
Processing time: 67 Days and 17.1 Hours
Schwannomas are uncommon tumors originating from Schwann cells, forming the neural sheath. They account for approximately 2%-6% of all mesenchymal tumors and are most commonly identified in peripheral nerve trunks, with rarity in the gastrointestinal tract. Among gastrointestinal locations, the stomach harbors the majority of nerve sheath tumors, while such occurrences in the sigmoid colon are exceptionally infrequent.
This study presented a clinical case involving a 60-year-old female patient who, during colonoscopy, was diagnosed with a submucosal lesion that was later identified as a nerve sheath tumor. The patient underwent surgical resection, and the diagnosis was confirmed through immunohistochemistry. This study highlighted an exceptionally uncommon occurrence of a nerve sheath tumor in the sigmoid colon, which was effectively managed within our department. Additionally, a comprehensive review of relevant studies was conducted.
The preoperative diagnosis of nerve sheath tumors poses challenges, as the definitive diagnosis still relies on pathology and immunohistochemistry. Alth
Core Tip: This study describes an uncommon nerve sheath tumor occurrence in the sigmoid colon, which was initially identified as a submucosal lesion and subsequently verified through histopathological and immunohistochemical analyses. The findings suggest that immunohistochemistry is the preferred diagnostic approach for this condition, and endoscopic surgery stands out as the optimal treatment modality.
- Citation: Li JY, Gao XZ, Zhang J, Meng XZ, Cao YX, Zhao K. Comprehensive evaluation of rare case: From diagnosis to treatment of a sigmoid Schwannoma: A case report. World J Gastrointest Oncol 2024; 16(1): 244-250
- URL: https://www.wjgnet.com/1948-5204/full/v16/i1/244.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i1.244
Schwannomas are uncommon tumors originating from Schwann cells that form the neural sheath. Accounting for approximately 2%-6% of all mesenchymal tumors[1], they predominantly occur in peripheral nerve trunks and are infrequently found in the gastrointestinal tract. The stomach hosts the majority of nerve sheath tumors within the gastrointestinal tract, whereas such tumors in the sigmoid colon are exceptionally rare[2]. The majority of colonic nerve sheath tumors are typically discovered as submucosal tumors during routine colonoscopy, and their accurate diagnosis prior to surgery poses challenges, necessitating postoperative immunohistochemistry of the specimen for definitive diagnosis[3]. The present study aimed to report a clinical case involving a 60-year-old female patient who was diagnosed with sigmoid nerve sheath tumor during colonoscopy. The patient subsequently underwent surgical resection, and histological diagnosis was made.
A 60-year-old female patient was admitted to our hospital for further diagnostic assessment and treatment regarding a submucosal bulge in the colon. This anomaly was identified during a colonoscopy performed at a nearby clinic two months earlier.
The patient did not report any abdominal pain, diarrhea, or bloating, and there were no changes in bowel habits. Furthermore, there were no signs of gastrointestinal symptoms, such as hematemesis or melena.
The patient had a documented medical history of hypertension, characterized by blood pressure readings as high as 18.67/13.33 kPa. However, this condition was effectively managed by administering plain oral medications, namely valsartan and amlodipine, normalizing blood pressure level. Additionally, it is noteworthy that the patient had undergone radical mastectomy to treat breast cancer approximately 12 years before her admission to our hospital.
The patient did not disclose any family genetic or aggregation diseases. There was no evident cancer history among her other relatives.
The physical examination of the patient showed no abnormality.
The post-hospitalization laboratory results were summarized as follows: White blood cell count of 4.99 × 109/L, red blood cell count of 4.31 × 1012/L, platelet count of 215 × 109/L, alpha-fetoprotein level of 7.11 ng/mL, cancer antigen 199 level less than 2.00 U/mL, and carcinoembryonic antigen level of 1.50 ng/mL.
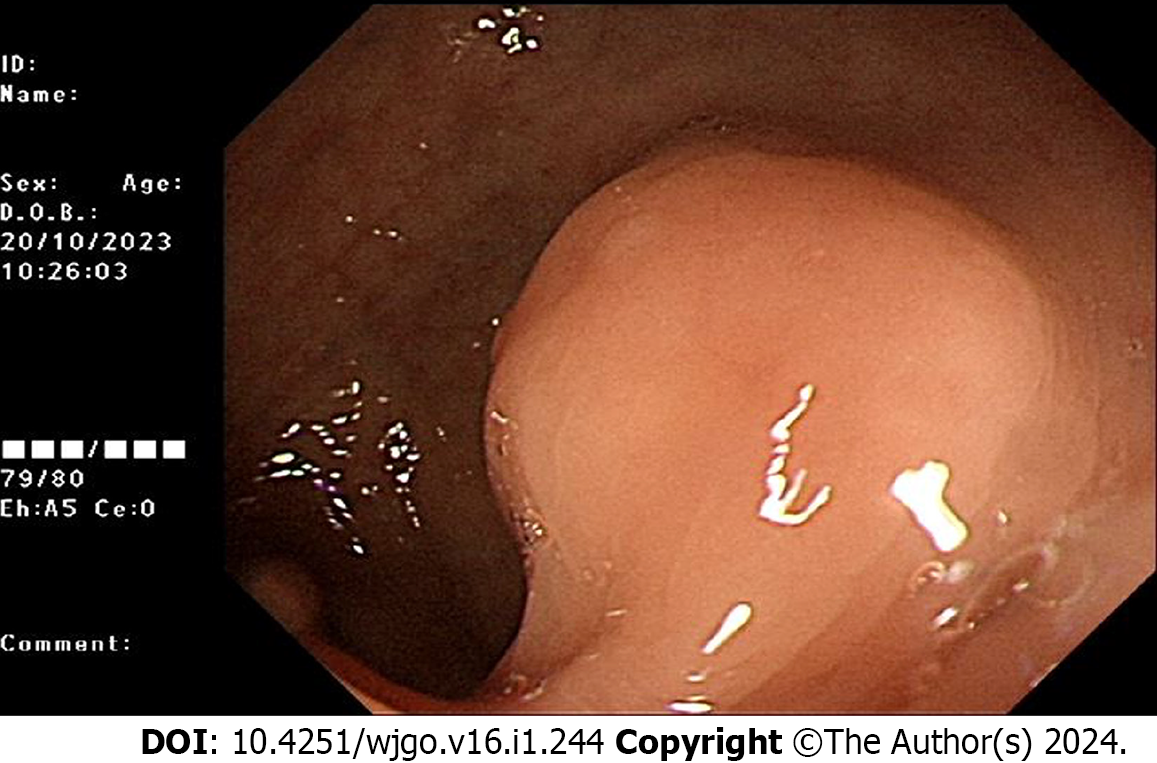
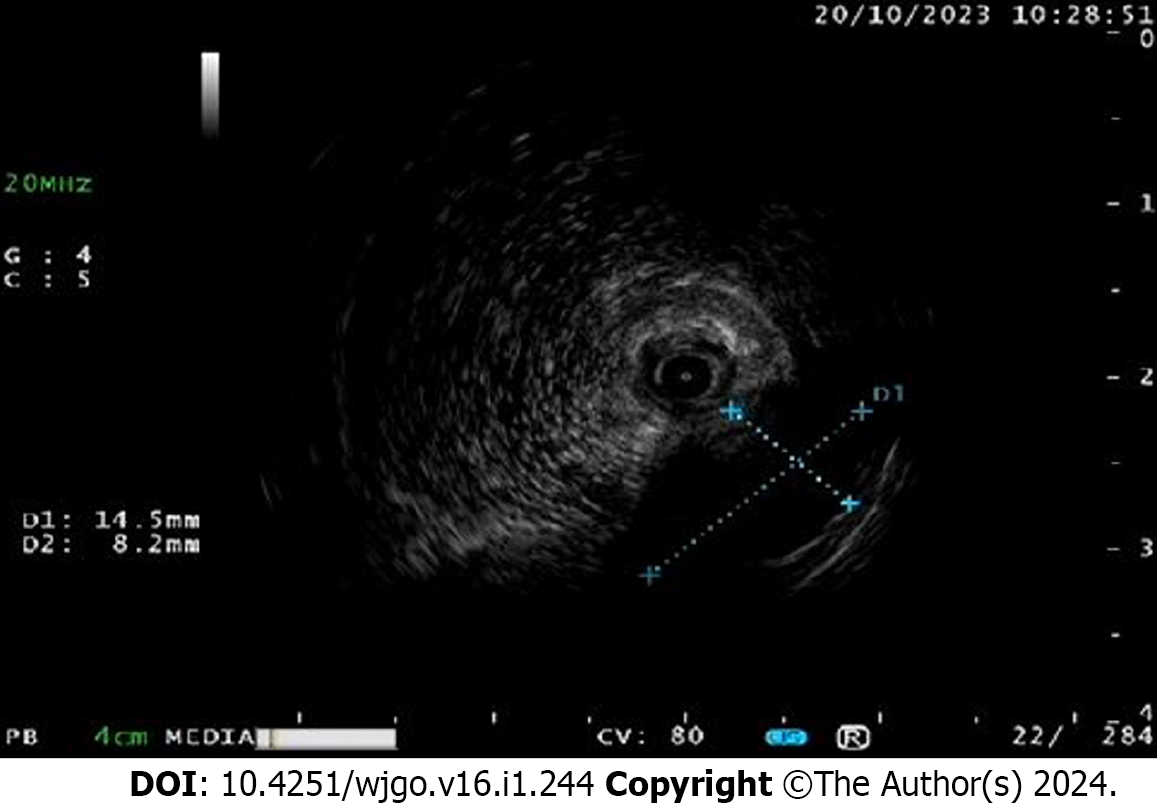
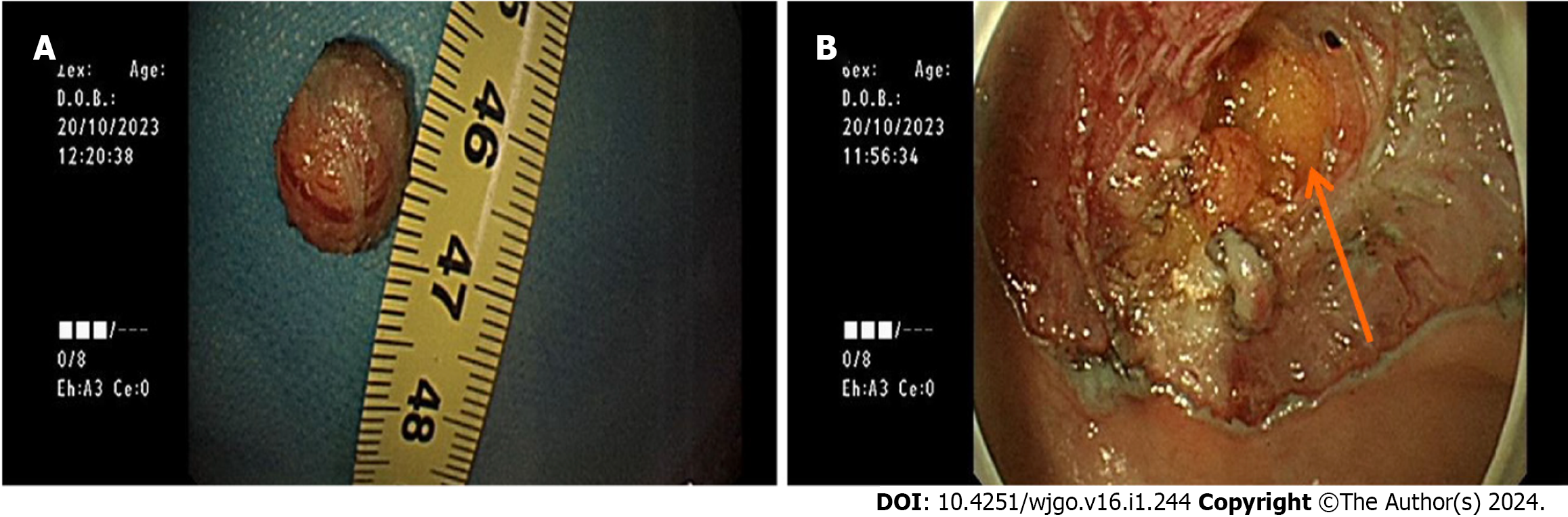
Abdominal computed tomography (CT) displayed no abnormality. The colonoscopy of the patient revealed the presence of a submucosal bulge located 15 cm proximal to the anus, as depicted in Figure 1. The ultrasound endoscopy showed the presence of a hypoechoic mass in the lamina propria, exhibiting heterogeneous echogenicity and measuring approximately 1.0 cm in size (Figure 2).
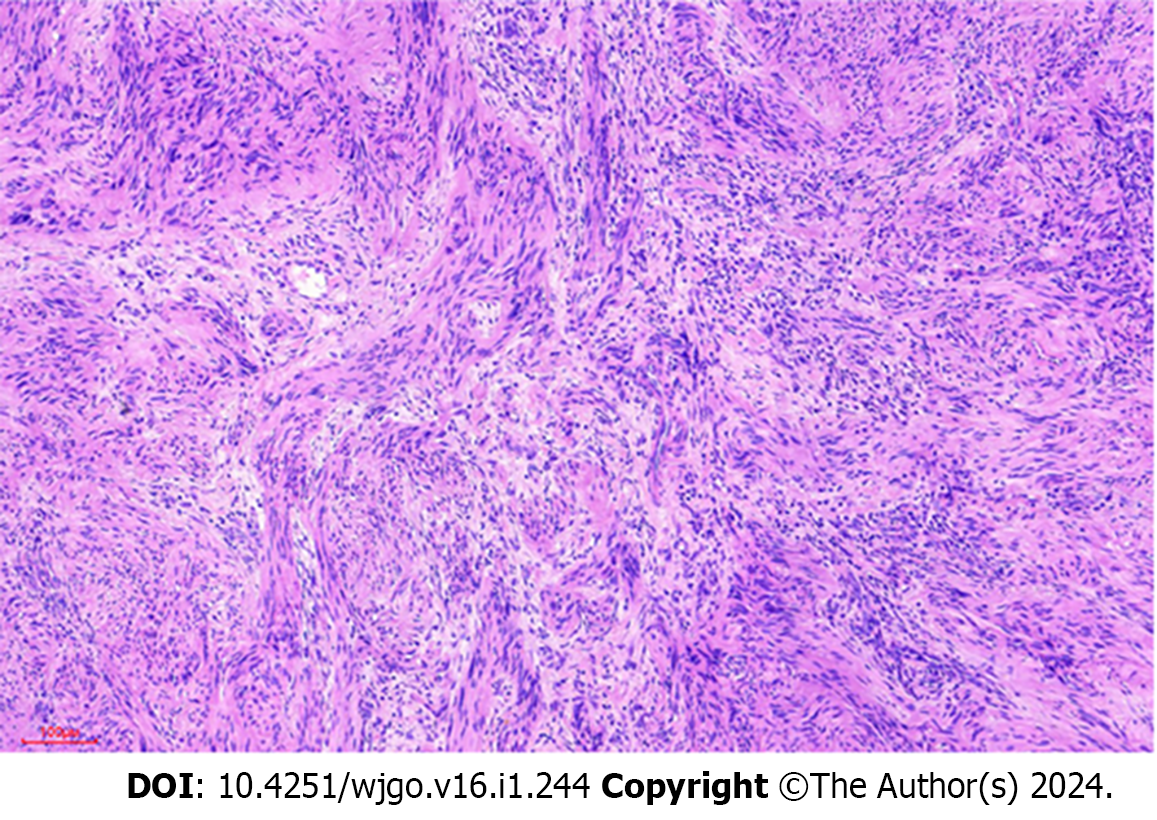
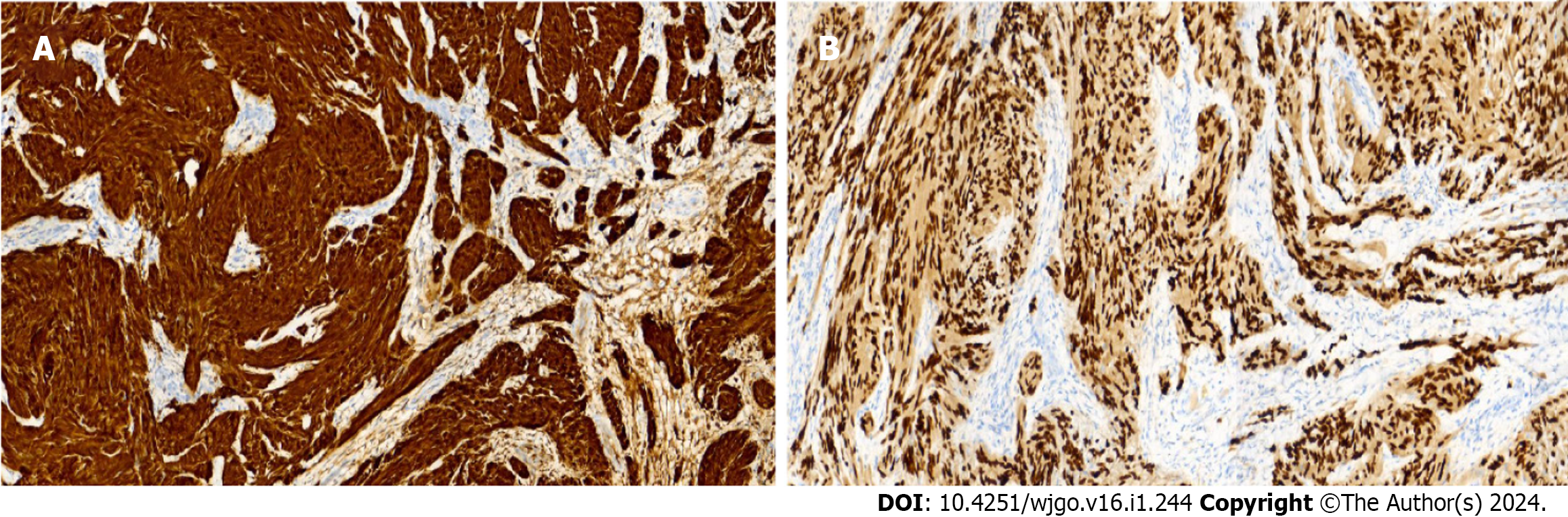
Following the thorough exfoliation of the tumor, samples were procured and subsequently dispatched for pathological examination. Hematoxylin and eosin staining was conducted, revealing the presence of spindle cells exhibiting minimal nuclear heterogeneity (Figure 3).
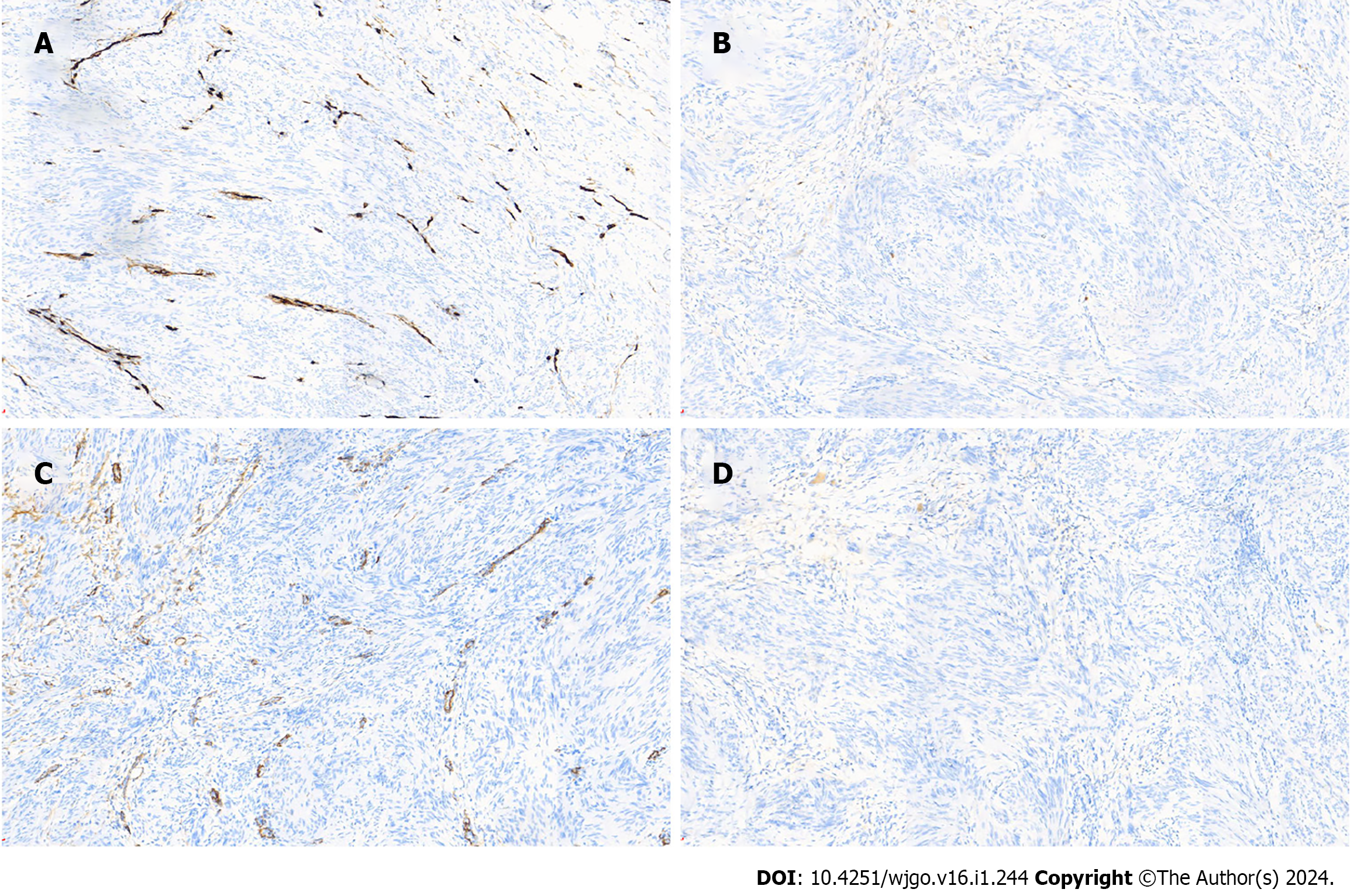
To enhance the precision of the tumor diagnosis, immunohistochemical staining was conducted. The tumor cells exhibited negative results for CD117, CD34, Desmin, SMA, and Dog-1 (Figure 4), in which Ki-67 (+, 2%), SOX-10, S-100, and SDHB were all strongly positive (Figure 5). The immunohistochemical results aligned with the diagnosis of a nerve sheath tumor. The presence of a Ki-67 index, measuring 2%, additionally substantiates the classification of the tumor as benign.
According to the above-mentioned results, the patient was diagnosed with a nerve sheath tumor of the sigmoid colon.
The patient underwent endoscopic submucosal dissection (ESD) to augment the sigmoid colon submucosally. A saline solution containing 1:10,000 epinephrine was injected post-mucosally. The positive lifting sign was noted, and a trapdoor was created to resect the surface mucosal layer. This procedure facilitated the exposure of the tumor, involving the removal of a segment of the muscular layer (Figure 6). The excision of the lesion was carried out utilizing a DUAL knife, employing repeated stripping with loopers and subsequent blunt separation. The trauma exhibited small perforations, which were adequately managed through hemostasis using hemostatic clips. A total of 11 hemostatic clips were applied to close the trauma.
The patient’s postoperative vital signs were stable, and the patient remained in satisfactory condition two months after the surgery.
Schwannomas are benign mesenchymal tumors derived from Schwann cells that form the neural sheath[4]. When situated within the gastrointestinal tract, gastrointestinal stromal tumors encompass smooth muscle tumors, smooth muscle histiocytomas, smooth muscle sarcomas, and gastrointestinal nerve sheath tumors. Gastrointestinal nerve sheath tumors are most frequently identified in the stomach and small intestine, with occurrences in the colon and rectum being exceptionally rare. While nerve sheath tumors can manifest at any life stage, their prevalence is notably higher in cases aged 60 years and older, with similar occurrence rates observed in both genders[5].
The majority of patients typically do not exhibit symptoms, while a minority may manifest symptoms, such as intestinal obstruction, abdominal pain, constipation, or melena[6]. Most patients are clinically detected by colonoscopy. The preoperative diagnosis of colorectal nerve sheath tumors has consistently posed challenges and necessitates differentiation from other mesenchymal tumors within the digestive system, particularly colorectal mesenchymal tumors. In clinical evaluations, magnetic resonance imaging and CT scan are frequently utilized to aid in diagnostic procedures. Nerve sheath tumors mainly present as clearly delineated homogeneous wall masses on abdominal CT scan and appear as well-defined transmural hypoechoic masses during ultrasound endoscopy[1]. However, their current utility in clinical practice is constrained due to the shortage of specificity[7]. A colorectal nerve sheath tumor can manifest as a submucosal mass or yellowish polypoid alterations during colonoscopy and as a hypoechoic mass originating from the lamina propria during ultrasonography. This poses a challenge in distinguishing it from other mesenchymal tumors[2,5-7]. In Inagawa et al’s study, only 15% of the colon schwannomas were diagnosed on preoperative endoscopic biopsy[8]. In Bohlok et al’s research, a preoperative diagnosis was made in 24% of cases with colorectal schwannomas[1].
Consequently, the definitive diagnosis still relies on pathology and immunohistochemistry. Nerve sheath tumors typically show positive staining for S-100 and SOX-10, with occasional instances of Vimentin staining. Conversely, immunohistochemical analysis typically yields negative results for DOG1, SMA, Desmin, CD117, p53, CD34, and c-kit[9-13].
On a macroscopic level, nerve sheath tumors typically exhibit lobulated and well-defined tumor characteristics, mainly displaying a cystic pattern[14,15]. Nerve sheath tumors frequently display microscopic features characterized by spindle-shaped cells with light nuclear staining and a low mitotic rate. Apart from morphology and immunohistochemical staining, pathologists contribute to the diagnosis by classifying nerve sheath tumors into Antoni A and Antoni B, representing the two histological growth patterns. The primary histological characteristic of Antoni A is the notable existence of Verocay bodies, wherein spindle cells are tightly arranged within fenestrated structures. Conversely, the principal histological attribute of Antoni B entails elongated or circular nucleated spindle cells that are sparsely distributed amidst yellow verrucous histiocytes and myxoid stroma[5,14]. The tumor observed in this case study is likely to be classified as Antoni type A, as evidenced by the histological presence of densely arranged spindle cells.
Despite being classified as benign, nerve sheath tumors have the potential to exhibit malignancy, with the Ki-67 index and the mitotic index serving as the primary diagnostic criteria for identifying such cases. A Ki-67 index exceeding 5% potentially indicates the presence of malignancy, while surpassing 10% tends to be indicative of malignancy. Additionally, the observation of more than 5 nuclear schizophrenic phases per high power field of view also suggests the likelihood of malignancy. A previous study revealed that out of 93 colorectal nerve sheath tumors, only 3 tumors were malignant[2]. Therefore, the most appropriate treatment option is complete surgical removal of the tumor with no lesions at the margins[14,16]. Refraining from radical resection is recommended once the clinical diagnosis is confirmed[5,17]. Radiotherapy and adjuvant chemotherapy are not recommended due to the benign nature of the tumor. The selection of a surgical procedure is contingent upon factors, such as the tumor’s size, location, and pathological characteristics. In the context of treating colorectal nerve sheath tumors, endoscopic resection has emerged as a routine treatment modality alongside traditional surgical techniques, owing to advancements in endoscopic techniques. In the present case, the patient underwent ESD in the sigmoid colon, resulting in successful resection of the tumor. The patient exhibited favorable postoperative recovery and remained recurrence-free throughout the follow-up period.
In conclusion, a sigmoid colon nerve sheath tumor is exceedingly infrequent. Owing to its uncommon nature, there remains a lack of consensus regarding the appropriate diagnostic and therapeutic approaches, rendering it particularly prone to misdiagnosis during clinical evaluation. Immunohistochemistry is widely regarded as the definitive method for diagnosing colorectal nerve sheath tumors within the academic community. By conducting a thorough examination of clinical features, laboratory tests, imaging and pathological manifestations, as well as the treatment and prognosis of the case, the objective of this research was to provide a valuable framework for the diagnosis and management of this specific disease.
We express gratitude to Hong-Hao Zhang, Kun Zhao, Xiao-Yu Jiang, Long-Qing Yu, and Guang-Yi Qu for their valuable comments on drafts of this study. Additionally, we would like to extend our appreciation to Jian Zhang and Xi-Zhuang Gao for their significant contributions to the completion of this study through their encouragement, support, and research assistance.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dilek ON, Turkey; Vij M, India S-Editor: Fan JR L-Editor: A P-Editor: Zhang XD
| 1. | Bohlok A, El Khoury M, Bormans A, Galdon MG, Vouche M, El Nakadi I, Donckier V, Liberale G. Schwannoma of the colon and rectum: a systematic literature review. World J Surg Oncol. 2018;16:125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 49] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 2. | Kim G, Kim SI, Lee KY. Case Report: Schwannoma of the sigmoid colon: a case report of a rare colonic neoplasm and review of literature. F1000Res. 2019;8:652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Pansari M, Lodin D, Gupta AK, Genuit T, Moseson J. Rare Case of a Transverse Colon Schwannoma. Cureus. 2020;12:e7604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Trivedi A, Ligato S. Microcystic/reticular schwannoma of the proximal sigmoid colon: case report with review of literature. Arch Pathol Lab Med. 2013;137:284-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Fotiadis CI, Kouerinis IA, Papandreou I, Zografos GC, Agapitos G. Sigmoid schwannoma: a rare case. World J Gastroenterol. 2005;11:5079-5081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Kanneganti K, Patel H, Niazi M, Kumbum K, Balar B. Cecal schwannoma: a rare cause of gastrointestinal bleeding in a young woman with review of literature. Gastroenterol Res Pract. 2011;2011:142781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Qi Z, Yang N, Pi M, Yu W. Current status of the diagnosis and treatment of gastrointestinal schwannoma. Oncol Lett. 2021;21:384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (1)] |
| 8. | Inagawa S, Hori M, Shimazaki J, Matsumoto S, Ishii H, Itabashi M, Adachi S, Kawamoto T, Fukao K. Solitary schwannoma of the colon: report of two cases. Surg Today. 2001;31:833-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Brandimarte G, Festa V, Balsamo G, Dezi A, Marzano C, Tursi A. Incidental Schwannoma of the Sigmoid. J Gastrointestin Liver Dis. 2020;29:303. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Miettinen M, Virolainen M, Maarit-Sarlomo-Rikala. Gastrointestinal stromal tumors--value of CD34 antigen in their identification and separation from true leiomyomas and schwannomas. Am J Surg Pathol. 1995;19:207-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 292] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 11. | Zhang K, Qu S, Li J, Cheng Y, Shi J, Liu T. A case report of rectal schwannoma treated with laparoscopic proctectomy. Medicine (Baltimore). 2018;97:e9866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | González Ruiz Y, Reyes Delgado A, Gutiérrez Alonso C, Franco Rubio JI, González Herrero M. [Sigmoid intussusception as a clinical presentation of colonic schwannoma: Pediatric case]. Arch Argent Pediatr. 2019;117:e68-e71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Adlekha S, Chadha T. Cellular schwannoma arising from sigmoid mesocolon presenting as torsion. Ann Med Health Sci Res. 2013;3:S33-S34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Nonose R, Lahan AY, Santos Valenciano J, Martinez CA. Schwannoma of the Colon. Case Rep Gastroenterol. 2009;3:293-299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Çakır T, Aslaner A, Yaz M, Gündüz Ur. Schwannoma of the sigmoid colon. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Zibert K, Richards S, Darwin P. A Patient With Rectal Schwannoma. Clin Gastroenterol Hepatol. 2019;17:A25-A26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Mokhtari M, Iranpour P, Golbahar Haghighi A, Ghahramani L. Schwannoma of the Rectosigmoid Colon. Adv Biomed Res. 2022;11:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |