Published online Nov 15, 2023. doi: 10.4251/wjgo.v15.i11.2041
Peer-review started: August 31, 2023
First decision: September 23, 2023
Revised: October 4, 2023
Accepted: October 23, 2023
Article in press: October 23, 2023
Published online: November 15, 2023
Processing time: 76 Days and 8 Hours
Pancreatic pseudoaneurysm is a rare vascular complication of chronic pancreatitis (CP) or necrotizing pancreatitis with an incidence of 4% to 17%, but it is potentially life-threatening. It is well known that most pancreatic pseudoaneurysms are clinically associated with pancreatic pseudocysts and are usually in the peripancreatic body-tail. A minority of intrapancreatic pseudoaneurysms occur in the absence of pseudocyst formation. Noninvasive computed tomogra
We report the case of a 67-year-old man who had been admitted to our hospital due to recurrent abdominal pain for 1 mo that was aggravated for 5 d. CT and MRI revealed a mass in the pancreatic head with significant expansion of the main pancreatic duct and mild atrophy of the pancreatic body-tail. He was admitted to the department of hepatobiliary and pancreatic surgery due to the possibility of a pancreatic tumor. The patient was then referred for endoscopic ultrasonography (EUS) with possible EUS-FNA. However, EUS showed a cystic lesion in the pancreatic head with wall thickness and enhancing nodules, which was doubtful because it was inconsistent with the imaging findings. Subsequently, color doppler flow imaging demonstrated turbulent arterial blood flow in the cystic lesion and connection with the surrounding vessel. Therefore, we highly suspected the possibility of CP complicated with intrapancreatic pseudoaneurysm, combined with the patient's long-term drinking history and the sonographic features of CP. Indeed, angiography revealed an oval area of contrast medium extravasation (size: 1.0 cm × 1.5 cm) at the far-end branch of the superior pancreaticoduodenal artery, and angiographic embolization was given imme
EUS is an important differential diagnostic tool when pancreatic pseudoaneurysm mimics the imaging appearance of a hypervascular pancreatic tumor.
Core Tip: Pancreatic pseudoaneurysm is a rare vascular complication of chronic pancreatitis, and the most commonly used clinical screening methods are computed tomography (CT) and magnetic resonance imaging (MRI). We report an even rarer case of an intrapancreatic pseudoaneurysm that mimicked a pancreatic neuroendocrine tumor on the axial view of contrast-enhanced CT and MRI. Finally, the diagnosis was confirmed by endoscopic ultrasonography; the patient was successfully treated with angiographic embolization. The imaging findings of pancreatic pseudoaneurysm mimicking pancreatic tumor is a concern.
- Citation: Yang Y, Liu XM, Li HP, Xie R, Tuo BG, Wu HC. Pancreatic pseudoaneurysm mimicking pancreatic tumor: A case report and review of literature. World J Gastrointest Oncol 2023; 15(11): 2041-2048
- URL: https://www.wjgnet.com/1948-5204/full/v15/i11/2041.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v15.i11.2041
Pancreatic pseudoaneurysm is an uncommon complication of chronic pancreatitis (CP). Life-threatening lastingly existing pseudoaneurysms lack a complete vascular wall structure and have a high risk of spontaneous rupture[1-3]. Hence, timely diagnosis and treatment are of great clinical significance.
Although angiography is the gold standard for diagnosing pancreatic pseudoaneurysms and can simultaneously provide management of therapy, given its invasive and expensive nature as well as the nonspecific clinical manifestations of pseudoaneurysm, can only be performed in cases of suspected pseudoaneurysm on computed tomography (CT) or magnetic resonance imaging (MRI)[4,5]. Most unruptured pancreatic pseudoaneurysms are incidentally diagnosed by CT or MRI. These relatively uncommon lesions are being incidentally detected with greater frequency as a result of the widespread use of high-resolution imaging techniques. The typical imaging appearance of a pancreatic pseudoaneurysm was described as a rapidly enhancing lesion with enhancement and attenuation similar to those of the aorta, which provide an accurate diagnosis of pancreatic pseudoaneurysm even in cases where the diagnosis is not suspected[6].
However, the diagnosis of pancreatic tumors also relies on CT and/or MRI. They are most often manifested as hypo
A 67-year-old male who complained of upper abdominal pain for 1 mo that was aggravated for 5 d was referred to our hospital.
One month previously, he had suffered dull abdominal pain that was around the epigastric area and radiated to the lower back without nausea, hematemesis, melena or fever. This discomfort worsened for 5 d. The patient was referred to our hospital.
The patient had no previous medical history.
He had a long-term drinking personal history for 43 years (liquor 250 g/d) and no family history of malignant tumors or genetic diseases.
His vital signs were stable. Abdominal examination revealed mild tenderness in the epigastric area and negative peritoneal irritation signs.
The serum tumor markers were within the normal range. Other laboratory examinations were normal except for a slight elevation in serum amylase (232 U/L).
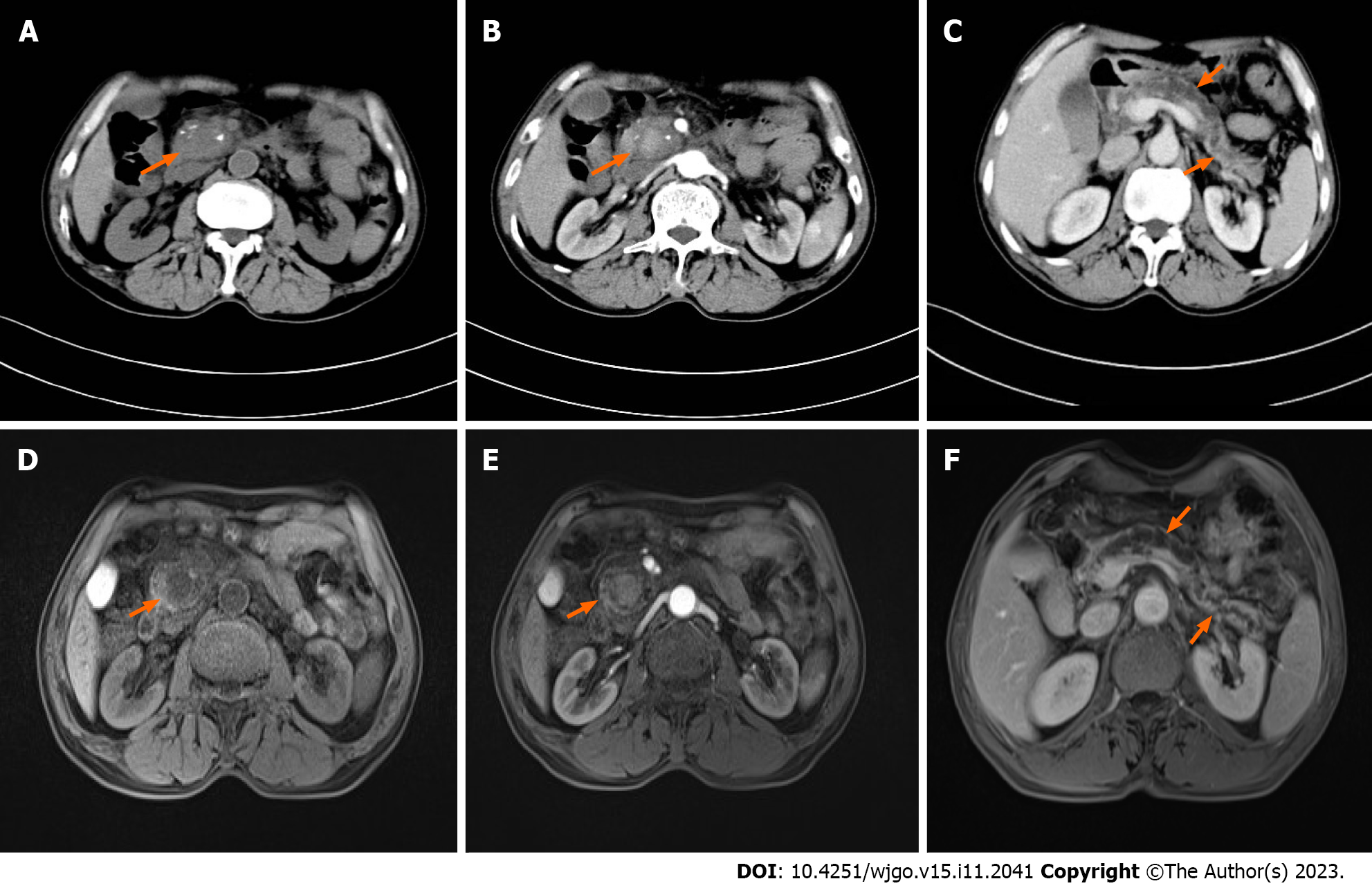
Abdominal CT showed enlargement of the pancreatic head with unclear borders and scattered irregular calcifications. The intrapancreatic lesion was slightly enhanced with uneven density on contrast-enhanced imaging (Figure 1A and B), and the main pancreatic duct was markedly dilated (Figure 1C), indicating a tumor in the pancreatic head with surrounding inflammation. MRI described the enlargement and deformation of the pancreatic head, and the contrast-enhanced scan showed uniformly mild enhancement within the lesion (Figure 1D and E). The pancreatic duct was generally dilated, and the pancreatic body and tail showed slight atrophy (Figure 1F). Neuroendocrine tumors of the pancreatic head with pancreatitis were considered.
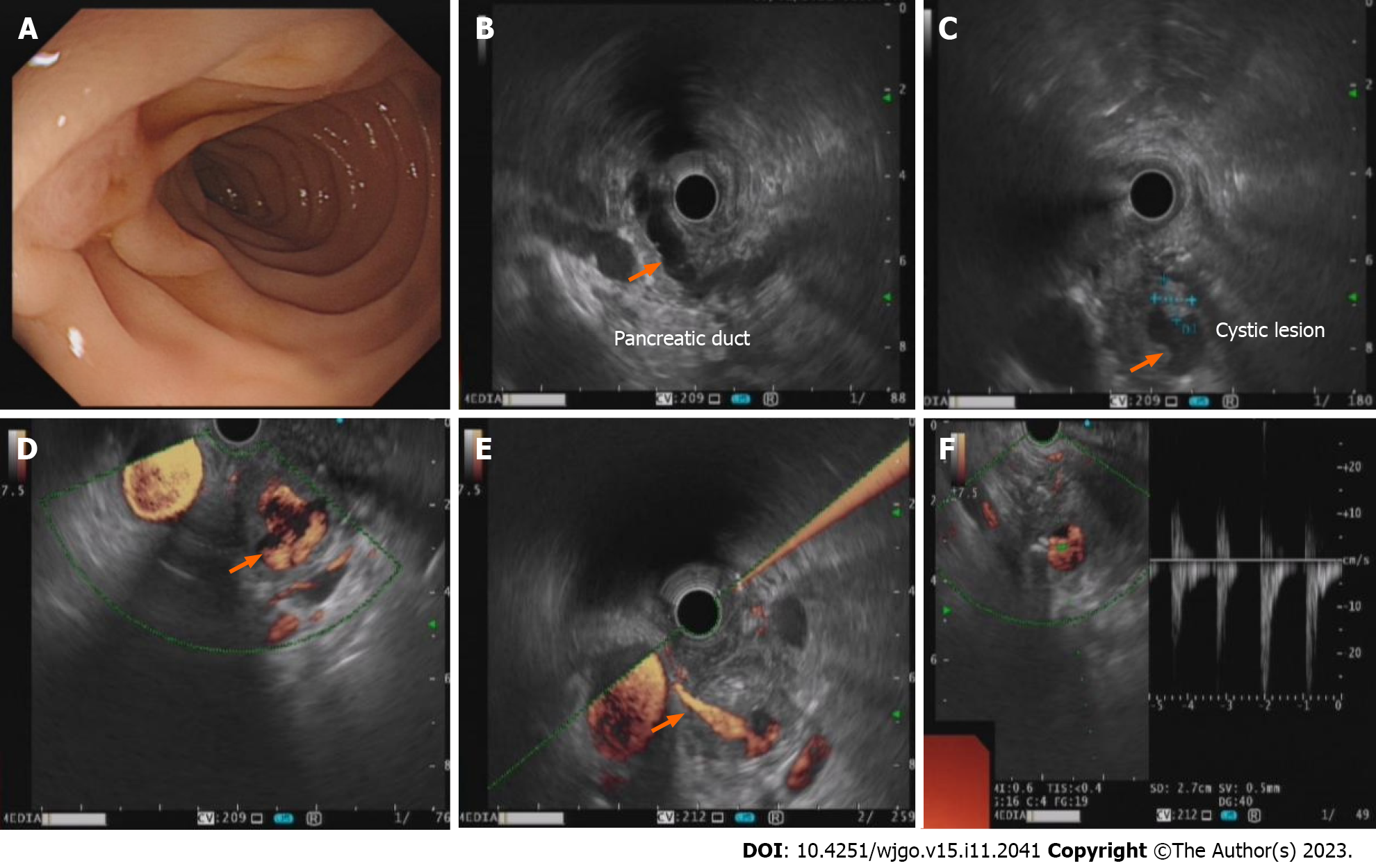
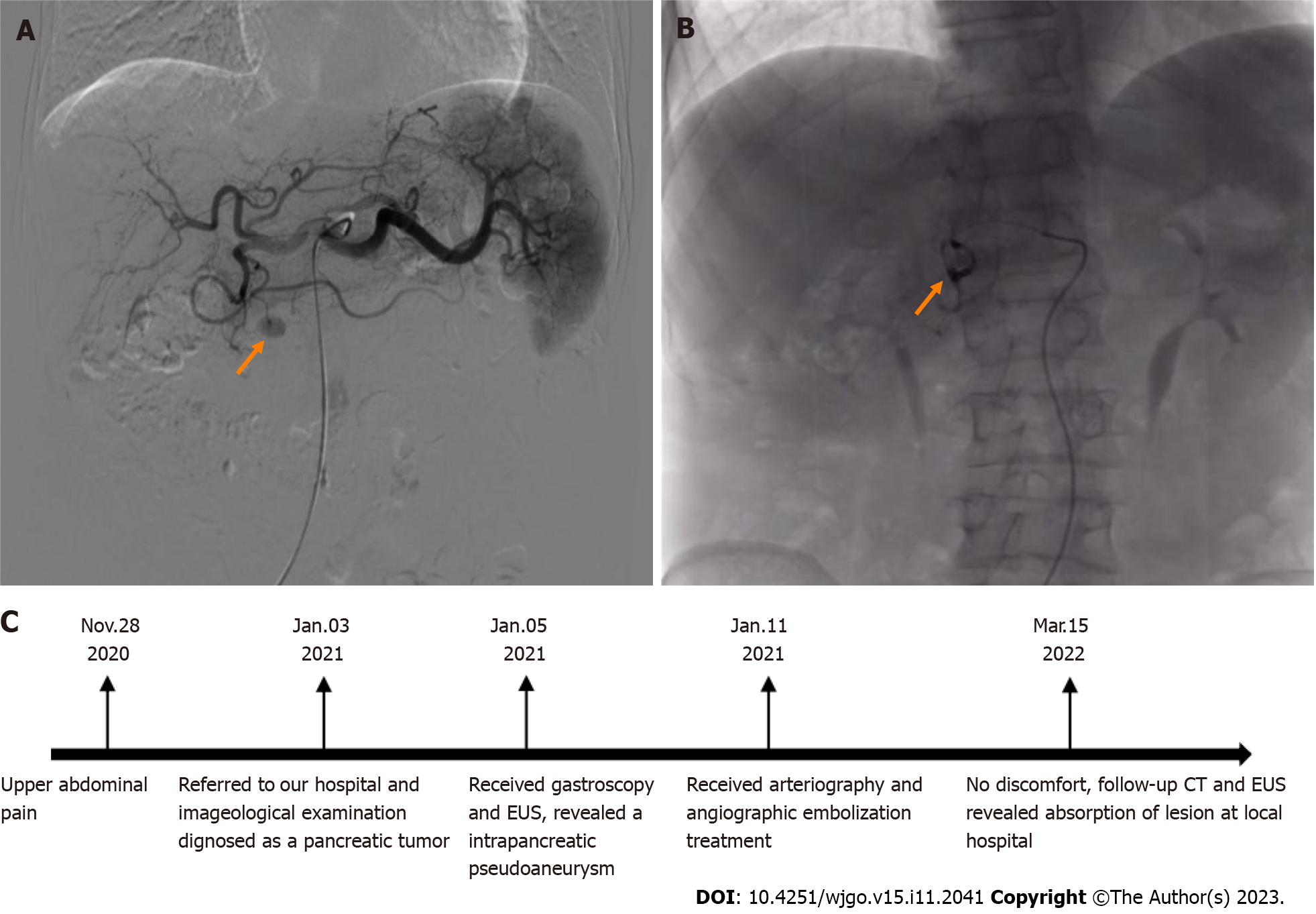
Gastroscopy showed that the shape of the duodenal papilla was normal, and there was no abnormal secretion (Figure 2A). Endoscopic ultrasonography (EUS) revealed mild atrophy of the pancreatic body and tail, obvious dilation of the main pancreatic duct that was 10 mm in diameter and no dilation of the bile duct. An irregular cystic lesion (size: 1.5 cm × 1.8 cm) was found in the central parenchyma of the pancreatic head with wall thickness and enhancing nodules (Figure 2B and C). Color doppler flow imaging (CDFI) indicated turbulent blood flow in the lesion with intense vascular flow and connection with the surrounding vessel (Figure 2D and E). Its blood flow filling frequency was consistent with that of the abdominal aorta, and the arterial blood flow signal was indicated by the doppler spectrum (Figure 2F). Arteriography was further preformed, and an oval area of contrast medium extravasation was finally discovered at the far-end branch of the superior pancreaticoduodenal artery after two injections of contrast medium (Figure 3A).
He was finally diagnosed with acute exacerbation of CP complicated with a pancreaticoduodenal artery pseudoaneurysm considering his personal history, EUS and arteriography examinations.
Angiographic embolization was immediately performed after the blood flow source of the pseudoaneurysm was confirmed, and no contrast medium spillage was found after embolization (Figure 3B). Comprehensive treatment with antibiotics, somatostatin, proton pump inhibitors and nutritional support was given during hospitalization.
He was discharged after undergoing the therapy for 10 d, and abstinence from liquor was strongly advised. He reported no discomfort by telephone follow-up and underwent follow-up CT and EUS at local hospital 1 year later, in which the diagnosis was CP, and absorption of the lesion and metal density shadow were revealed in the pancreatic head (Figure 3C).
Pseudoaneurysm associated with CP is a rare complication resulting from the erosion of pancreatic or nearby vessels by leaked pancreatic juice[9]. The arteries involved with the greatest frequency are the spleen artery (40%), followed by the gastroduodenal artery (30%), the superior and inferior pancreaticoduodenal artery (20%), the left gastric artery (5%), the hepatic artery and branches (2%)[10,11]. Clinically, most pseudoaneurysms associated with CP are formed in relation to longstanding pancreatic pseudocysts caused by vascular erosion from enzymes within the pseudocyst, direct compression, or ischemia, thereby converting the pseudocyst into a large pseudoaneurysm, as well as usually being in the peripancreatic body-tail[12,13]. However, intrapancreatic and small pseudoaneurysms unrelated to pancreatic pseu
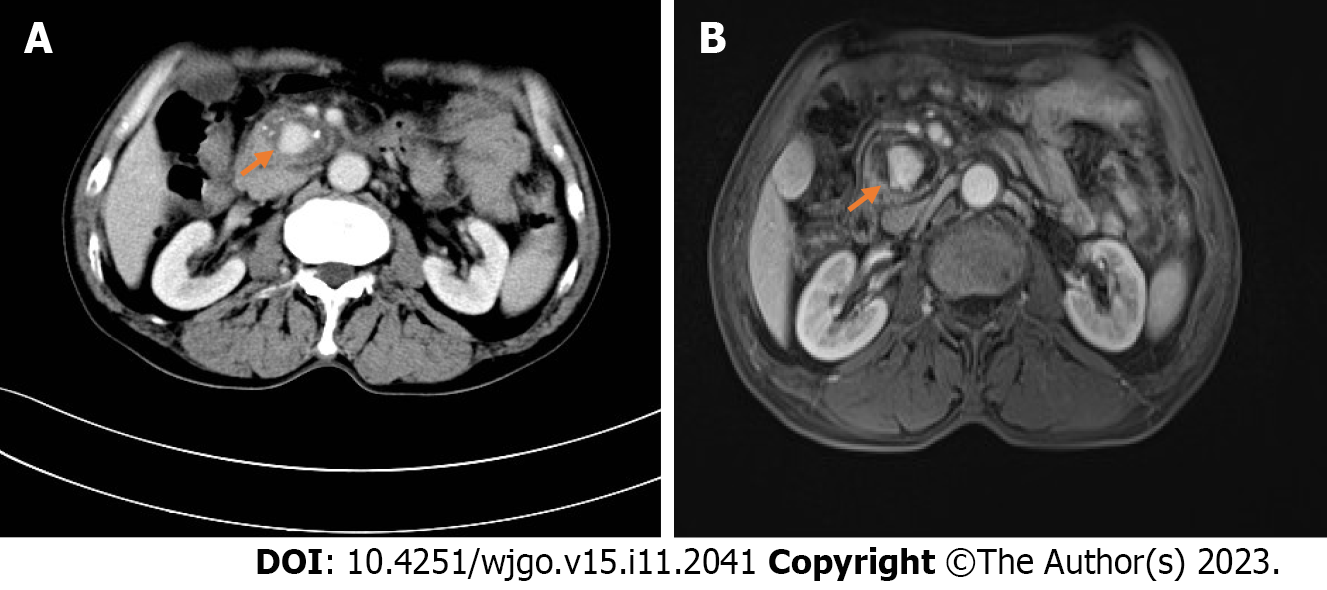
In our case, a hypoechoic mass in the head of the pancreas showed mild enhancement in the arterial phase (Figure 1B and E) and delayed enhancement in the venous phase (Figure 4). Due to the lack of pseudocyst formation and combined indirect signs of pancreatic head tumors, such as obvious dilation of the pancreatic duct and atrophy of the distal pancreas, it was more likely to be misdiagnosed as a pancreatic tumor, especially a neuroendocrine tumor, because it can be markedly hyperattenuating in the arterial or pancreatic phase[12,14]. In fact, the kind of indirect imaging signs are also in accordance with the diagnostic criteria of CP. Therefore, a diagnostic pitfall will be encountered when the lesion location is unusual and is a hypervascular solid mass.
Notably, these unusual imaging findings may be related to the formation mechanism of pseudoaneurysms. Pseudoaneurysms have no normal vessel wall structure, are merely composed of hematoma and surrounding fibrous tissue, are not continuous with the arterial lumen, and have a leaking hole on the artery wall[15-17]. Hence, we thought that when the diameter of the leaking hole on the arterial wall was extremely small and the access connected to the hematoma was narrow and twisted, hemodynamic alterations occurred in which the blood flow was slow in the arterial phase and stagnant in the venous phase, which gave rise to no significantly enhanced lesion on CT and MRI after injection of the contrast medium. Relevant literature also proposed that vascular endoleaks are usually evaluated with static multiphasic CT that includes noncontrast, arterial, and delayed phases. However, static CT may miss some endoleaks, particularly low-flow endoleaks that emerge in the late arterial phase[18]. This hypothesis was supported during angiography, as we did not find the lesion until two injections of contrast medium were performed. To our knowledge, this is a rare report describing the CT and MRI findings of CP with intrapancreatic pseudoaneurysm mimicking a pancreatic tumor.
As described above, CT and MRI are fast and noninvasive imaging modalities that provide an easy diagnosis of pan
It is well known that EUS has been extensively applied in the detection, diagnosis and treatment of pancreatic disease. The advantage of EUS with the auxiliary function of CDFI lies in dynamically reflecting the peripheral blood flow signal and clearly delineating the extent and size of the pseudoaneurysm[26]. Not only does EUS play an important role in the noninvasive detection of pancreatic pseudoaneurysms, but the convenience of monitoring and follow-up is also a significant advantage of EUS. In conclusion, even though the initial CT or MRI imaging was misunderstood, when EUS examination of suspected pancreatic cystic lesions in the background of CP is performed, we should remain clinically suspicious of a pseudoaneurysm regardless of the location and size, thereby effectively avoiding pitfalls in differential diagnosis.
So far, angiography embolization has been widely accepted in the management of pseudoaneurysms because of its higher rates of diagnosis and successful embolization in the meanwhile. Surgical treatment is merely suitable for patients in whom angiographic embolization has failed or who have active bleeding with unstable vital signs[27]; a few case reports and small case series have appeared in the literature showing the feasibility of EUS-guided obliteration of pancreatic pseudoaneurysm by means of glue or thrombin injection, alone or combined with coil deployment[28-30]. Some experts also have indicated that for patients with repeated angiography or embolization failure, the advent of thrombin instillation through EUS guidance has opened an altogether new arena for managing difficult pseudoaneurysms and thereby avoiding surgical risks, but it is essential to note that it relates to increased embolic risk. Studies are needed to provide more data on the efficacy of this method[31].
Although CT and MRI have a high diagnostic rate for pancreatic pseudoaneurysm, the rare location and unusual imaging findings still likely led to a misdiagnosis. EUS has an irreplaceable advantage in the noninvasive diagnosis of pancreatic pseudoaneurysms. Through continuous dynamic scanning, combined with color doppler flow and spectrum, it can efficiently make a correct diagnosis. We hope that this case report can provide more clinical experience for the diagnosis and differential diagnosis of pancreatic pseudoaneurysm.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shiryajev YN, Russia; Uhlmann D, Germany S-Editor: Qu XL L-Editor: A P-Editor: Wu RR
| 1. | Chiang KC, Chen TH, Hsu JT. Management of chronic pancreatitis complicated with a bleeding pseudoaneurysm. World J Gastroenterol. 2014;20:16132-16137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 2. | Peynircioğlu B, Karaosmanoğlu AD, İdilman İS, Akata D, Şimşek H. Intrapancreatic pseudoaneurysm causing massive gastrointestinal hemorrhage and chronic pancreatitis. Turk J Gastroenterol. 2015;26:270-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | El Hamel A, Parc R, Adda G, Bouteloup PY, Huguet C, Malafosse M. Bleeding pseudocysts and pseudoaneurysms in chronic pancreatitis. Br J Surg. 1991;78:1059-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 103] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Shuaib W, Tiwana MH, Vijayasarathi A, Sadiq MF, Anderson S, Amin N, Khosa F. Imaging of vascular pseudoaneurysms in the thorax and abdomen. Clin Imaging. 2015;39:352-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Múnera F, Soto JA, Palacio D, Velez SM, Medina E. Diagnosis of arterial injuries caused by penetrating trauma to the neck: comparison of helical CT angiography and conventional angiography. Radiology. 2000;216:356-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 164] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Shelar SS, Dhande R, Nagendra V, Suryadevara M, Shetty N. Giant Abdominal Pseudoaneurysm Secondary to Recurrent Pancreatitis: Imaging and Endovascular Intervention. Cureus. 2022;14:e32872. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Lee ES, Lee JM. Imaging diagnosis of pancreatic cancer: a state-of-the-art review. World J Gastroenterol. 2014;20:7864-7877. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 247] [Cited by in RCA: 249] [Article Influence: 22.6] [Reference Citation Analysis (4)] |
| 8. | Yoon SH, Lee JM, Cho JY, Lee KB, Kim JE, Moon SK, Kim SJ, Baek JH, Kim SH, Lee JY, Han JK, Choi BI. Small (≤ 20 mm) pancreatic adenocarcinomas: analysis of enhancement patterns and secondary signs with multiphasic multidetector CT. Radiology. 2011;259:442-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 180] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 9. | Hsu JT, Yeh CN, Hung CF, Chen HM, Hwang TL, Jan YY, Chen MF. Management and outcome of bleeding pseudoaneurysm associated with chronic pancreatitis. BMC Gastroenterol. 2006;6:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Balachandra S, Siriwardena AK. Systematic appraisal of the management of the major vascular complications of pancreatitis. Am J Surg. 2005;190:489-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Larrey Ruiz L, Luján Sanchis M, Peño Muñoz L, Barber Hueso C, Cors Ferrando R, Durá Ayet AB, Sempere García-Argüelles J. Pseudoaneurysm associated with complicated pancreatic pseudocysts. Rev Esp Enferm Dig. 2016;108:583-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Evans RP, Mourad MM, Pall G, Fisher SG, Bramhall SR. Pancreatitis: Preventing catastrophic haemorrhage. World J Gastroenterol. 2017;23:5460-5468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Flati G, Andrén-Sandberg A, La Pinta M, Porowska B, Carboni M. Potentially fatal bleeding in acute pancreatitis: pathophysiology, prevention, and treatment. Pancreas. 2003;26:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 148] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 14. | Horton KM, Hruban RH, Yeo C, Fishman EK. Multi-detector row CT of pancreatic islet cell tumors. Radiographics. 2006;26:453-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 83] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Bedioui H, Ayadi S, Daghfous A, Jouini M, Bakhtri M, Rajhi H, Chebbi F, Fteriche F, Ksantini R, Kacem MJ, Ben Safta Z. Pseudoaneurysm of the splenic artery presenting with gastrointestinal bleeding. J Emerg Med. 2010;38:317-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Udd M, Leppäniemi AK, Bidel S, Keto P, Roth WD, Haapiainen RK. Treatment of bleeding pseudoaneurysms in patients with chronic pancreatitis. World J Surg. 2007;31:504-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Pilleul F, Beuf O. Diagnosis of splanchnic artery aneurysms and pseudoaneurysms, with special reference to contrast enhanced 3D magnetic resonance angiography: a review. Acta Radiol. 2004;45:702-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Rajiah PS, Weber N, Loewen J, Kasten H, Williamson E, Moore A, Leng S. Dynamic CT Angiography in Vascular Imaging: Principles and Applications. Radiographics. 2022;42:E224-E225. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Burke JW, Erickson SJ, Kellum CD, Tegtmeyer CJ, Williamson BR, Hansen MF. Pseudoaneurysms complicating pancreatitis: detection by CT. Radiology. 1986;161:447-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Agrawal GA, Johnson PT, Fishman EK. Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. AJR Am J Roentgenol. 2007;188:992-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 142] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 21. | Lawler LP, Horton KM, Fishman EK. Peripancreatic masses that simulate pancreatic disease: spectrum of disease and role of CT. Radiographics. 2003;23:1117-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Saba L, Anzidei M, Lucatelli P, Mallarini G. The multidetector computed tomography angiography (MDCTA) in the diagnosis of splenic artery aneurysm and pseudoaneurysm. Acta Radiol. 2011;52:488-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Barral M, Sirol M, Malgras B, Boudiaf M, Kaci R, Pocard M, Soyer P. Pancreatic hematoma due to ruptured splenic pseudoaneurysm mimicking pancreatic malignancy. Diagn Interv Imaging. 2017;98:565-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Hashimoto M, Watanabe G, Matsuda M, Mori M. Intrapancreatic pseudoaneurysm associated with pancreatitis mimicking pancreatic tumor. J Gastroenterol Hepatol. 2005;20:159-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Palmucci S, Mauro LA, Milone P, Di Stefano F, Scolaro A, Di Cataldo A, Ettorre GC. Diagnosis of ruptured superior mesenteric artery aneurysm mimicking a pancreatic mass. World J Gastroenterol. 2010;16:2298-2301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Varadarajulu S, Eloubeidi MA. Diagnosis of an aneurysm masquerading as a pancreatic-cyst lesion at EUS. Gastrointest Endosc. 2007;65:721-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Bhasin DK, Rana SS, Sharma V, Rao C, Gupta V, Gupta R, Kang M, Singh K. Non-surgical management of pancreatic pseudocysts associated with arterial pseudoaneurysm. Pancreatology. 2013;13:250-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Roach H, Roberts SA, Salter R, Williams IM, Wood AM. Endoscopic ultrasound-guided thrombin injection for the treatment of pancreatic pseudoaneurysm. Endoscopy. 2005;37:876-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Jeffers K, Majumder S, Vege SS, Levy M. EUS-guided pancreatic pseudoaneurysm therapy: better to be lucky than good. Gastrointest Endosc. 2018;87:1155-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Rai P, Kc H, Goel A, Aggarwal R, Sharma M. Endoscopic ultrasound-guided coil and glue for treatment of splenic artery pseudo-aneurysm: new kid on the block! Endosc Int Open. 2018;6:E821-E825. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Gamanagatti S, Thingujam U, Garg P, Nongthombam S, Dash NR. Endoscopic ultrasound guided thrombin injection of angiographically occult pancreatitis associated visceral artery pseudoaneurysms: Case series. World J Gastrointest Endosc. 2015;7:1107-1113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |