Published online Jan 15, 2022. doi: 10.4251/wjgo.v14.i1.153
Peer-review started: February 25, 2021
First decision: May 3, 2021
Revised: May 16, 2021
Accepted: December 9, 2021
Article in press: December 9, 2021
Published online: January 15, 2022
Processing time: 319 Days and 13.8 Hours
Approximately 8% of all non-Hodgkin lymphomas are extranodal marginal zone B cell lymphomas of mucosa-associated lymphoid tissue (MALT), also known as MALT lymphomas. These arise at a wide range of different extranodal sites, with most cases affecting the stomach, the lung, the ocular adnexa and the thyroid. The small intestine is involved in a lower percentage of cases. Lymphoma growth in the early stages is associated with long-lasting chronic inflammation provoked by bacterial infections (e.g., Helicobacter pylori or Chlamydia psittaci infections) or autoimmune conditions (e.g., Sjögren’s syndrome or Hashimoto thyroiditis). While these inflammatory processes trigger lymphoma cell proliferation and/or survival, they also shape the microenvironment. Thus, activated immune cells are actively recruited to the lymphoma, resulting in either direct lymphoma cell stimulation via surface receptor interactions and/or indirect lymphoma cell stimulation via secretion of soluble factors like cytokines. In addition, chronic inflammatory conditions cause the acquisition of genetic alterations resulting in autonomous lymphoma cell growth. Recently, novel agents targeting the microenvironment have been developed and clinically tested in MALT lymphomas as well as other lymphoid malignancies. In this review, we aim to describe the composition of the microenvironment of MALT lymphoma, the interaction of activated immune cells with lymphoma cells and novel therapeutic approaches in MALT lymphomas using immunomodulatory and/or microenvironment-targeting agents.
Core Tip: This review summarizes and discusses the major findings in extranodal mucosa-associated lymphoid tissue lymphomas with a focus on the microenvironment. It describes how long-lasting chronic inflammatory processes promote the growth of malignant cells, which can be directly mediated by bacteria and/or interaction with activated immune cells. In addition, major genetic alterations are summarized, and models of how these might be acquired are discussed. Finally, novel therapies targeting the microenvironment are described.
- Citation: Uhl B, Prochazka KT, Fechter K, Pansy K, Greinix HT, Neumeister P, Deutsch AJ. Impact of the microenvironment on the pathogenesis of mucosa-associated lymphoid tissue lymphomas. World J Gastrointest Oncol 2022; 14(1): 153-162
- URL: https://www.wjgnet.com/1948-5204/full/v14/i1/153.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i1.153
Extranodal mucosa-associated lymphoid tissue (MALT) lymphomas account for 5%-8% of all non-Hodgkin lymphomas (NHLs) and were first described in 1983 by Isaacson and Wright[1-3]. MALT lymphomas arise at a wide range of extranodal sites, most frequently occurring in the stomach, followed by the lung, ocular adnexa, thyroid and small intestine[4]. The cells of this type of lymphoma have the same cytological and immunophenotypical (CD20+, CD21+, CD35+, IgM+, and IgD-) features as marginal zone B cells, prompting the World Health Organization to designate this lymphoma “extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma)”[5]. The cell of origin of MALT lymphomas is the marginal zone (MZ) B cell. These B cells are a first line of defense against infectious agents and build up an innate-like antibody response in a T cell-independent and T cell-dependent manner[6,7]. MALT lymphomagenesis is highly dependent on microenvironmental factors and therefore often associated with chronic inflammation induced either by Helicobacter pylori (H. pylori), the most common pathogen in gastric MALT lymphomas, or by chronic inflammation as a result of autoimmune disease. These are known risk factors for the development of MZ lymphomas[8]. In addition to the antigenic drive, oncogenic events are important in the process of malignant transformation[8]. MALT lymphoma cell proliferation is driven by T cell signaling, chronic (auto) antigen stimulation of MZ B cells, and activation of the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB pathway)[9].
In MALT lymphomas, recurrent chromosomal aberrations, such as trisomies, amplifications and deletions, chromosomal translocations, somatic point mutations, and promotor hypermethylation, have been described.
The most common cytogenetic alterations are trisomies 3, 12, and/or 18, which are present in 20%-35% of cases, and they are often associated with one of the four main translocations[10-13]. Trisomies 3 and 18 and losses at 6q23 occur in MALT lym
The most common chromosomal translocations associated with the pathogenesis of MALT lymphomas are t(1;14)(p22,q32) (involving the IGHV and BCL10 genes), t(11;18)(q21,q21) (involving BIRC3/MALT1), t(14;18)(q32,q21) (involving IGH/BCL2) and t(3;14)(p14.1,q32) (involving IGHV-FOXP1)[8,10,16]. The frequency of genetic aberrations is dependent on the primary site of disease[10,17]. At least three translocations, t(11;18), t(14;18) and t(1;14), involve the BCL10 and MALT1 genes and lead to activation of the NF-кB pathway in lymphocytes, thus indicating that these aberrations are oncogenic events[18,19].
We observed somatic missense mutations in PIM1 and cMYC in 46% of gastric and 30% of extragastric MALT lymphomas[20]. In addition, missense and frameshift mutations in p53 were described in 20.8% of MALT lymphomas (mainly of gastric origin)[10]. Moreover, whole exome sequencing of extragastric MALT lymphomas identified recurrent novel somatic mutations in PIK3CD, TET2, and TNFRSF14 and in two G protein-coupled receptors (GPR34 and CCR6), which have not been reported to be somatically mutated in human tumors thus far. In addition, recurrent mutations were found in two genes (TBL1XR1 and NOTCH1), for which somatic mutations were already reported in ocular adnexal MALT lymphomas. The mutation frequencies of these genes were remarkably variable among MALT lymphomas affecting different sites[21]. Sequencing of NF-κB signaling pathway-related genes — A20, Card11,
Finally, promoter hypermethylation of the tumor suppressor genes p16 and p57 has been reported in low-grade MALT lymphoma cases[24]. CpG hypermethylation of A20 has been detected in 26% of investigated MALT lymphomas, including ocular adnexal cases and lymphomas located in the salivary and thyroid glands[10].
Aberrant somatic hypermutation (ASHM) has been identified to be crucial for the development of lymphoid neoplasms. ASHM occurs commonly in diffuse large B cell lymphomas but is rare in indolent lymphomas[10,25,26]. The pathogenesis of most lymphomas is associated with distinct genetic lesions arising from mistakes during class switch recombination (CSR) and somatic hypermutation (SHM)[10,27]. Acti
It is well known that MALT lymphomas are commonly associated with long-lasting chronic inflammation caused by microbial pathogens and/or autoimmune diseases that trigger sustained lymphoid proliferation. The low activation threshold of MZ B cells may predispose them to neoplastic transformation[29].
Gastric MALT lymphomas show a strong association with chronic H. pylori infection[30]. Other infectious associations have been reported for Borrelia burgdorferi (skin)[31], Campylobacter jejuni (intestine)[32], Achromobacter xylosoxidans (lung)[33], Chlamydia psittaci (ocular, nongastrointestinal MALT lymphomas)[34-36] and hepatitis C virus (splenic marginal zone lymphoma)[37]. The strength of these associations shows vast geographical discrepancies[38-40]. In addition, an association of MALT lymphomas with chronic inflammation induced by autoimmune disease is found in primary Sjögren’s syndrome (pSS)[41-43] and Hashimoto thyroiditis[44].
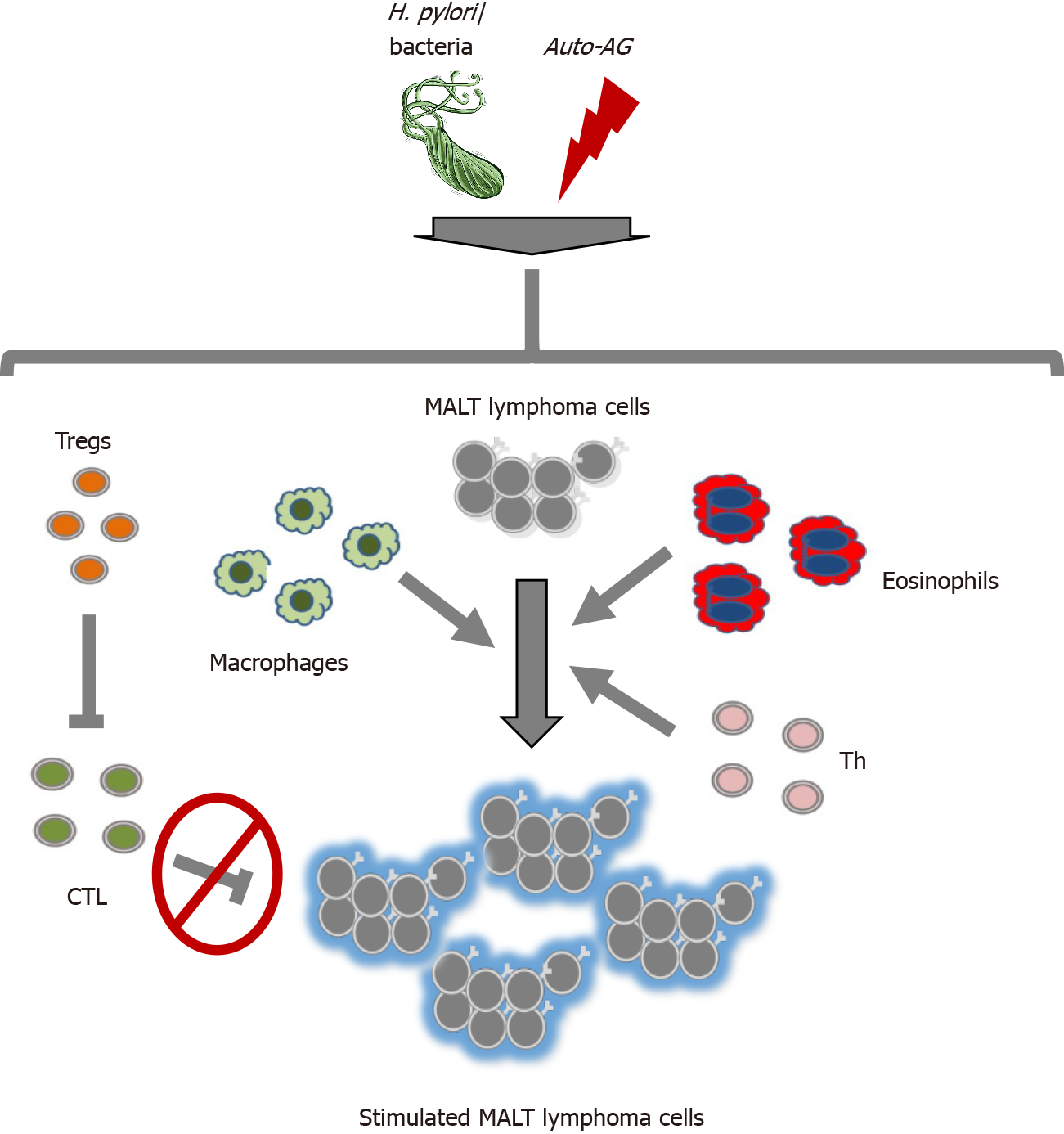
Long-lasting chronic inflammation, e.g., induced by H. pylori infection or pSS, is the trigger for a multistage process in the evolution of MALT lymphomas due direct effects on B cell proliferation and/or survival and/or indirect effects on the activation of innate and adaptive immune cells[9,43,45] as shown in Figure 1.
H. pylori strains expressing cytotoxin-associated gene A (CagA) are associated with the lymphomagenesis of gastric MALT lymphoma[46,47]. CagA is involved in the promotion of proliferation and the inhibition of apoptosis of B lymphocytes through activation of extracellular signal-regulated kinase (ERK) and p38 mitogen-activated protein kinase (MAPK) and upregulation of BCL-2 and BCL-xL[47]. Second, the CagA tyrosine phosphorylation-independent pathway impairs p53 via AKT serine/threonine kinase 1 (AKT1) and human homolog of double minute 2 (HDM2)[9,45]. In general, cell wall lipopolysaccharide has been shown to be responsible for triggering a pattern of mucosal inflammation via Toll-like receptor signaling, resulting in activation of MAPK, phosphoinositide 3-kinase (PI3K) and NF-κB pathways in H. pylori infection[48,49].
As already mentioned, long-lasting chronic inflammatory processes might also influence MALT lymphomagenesis through the direct (auto) antigen-mediated interaction of lymphoma cells with immune cells and/or the secretion of soluble factors like cytokines. In this case, a direct immune cell-lymphoma cell interaction and subsequent activation result. Activated T cells targeting H. pylori represent cells targeting autoantigens in the case of pSS, and these T cells are present in MALT lymphomas and are able to promote lymphoma cell growth via CD40-mediated signaling and T helper (Th) type-2 cytokine (IL-4, IL-5, and IL-10) effects[50,51]. Examples of two cytokines are a proliferation-inducing ligand (APRIL) and B cell-activating factor (BAFF), which are members of the tumor necrosis factor family and play a key role in B cells and autoimmunity. Both cytokines are secreted by eosinophils and/or macrophages and stimulate MALT lymphoma cells[52-54]. Both the CD40/CD40L interaction and APRIL and/or BAFF signaling cause the activation of important downstream signaling pathways, e.g., NF-κB and/or MAPK[55,56], and thereby have an important impact on MALT lymphomagenesis.
Chronic inflammatory processes in MALT lymphomas not only promote B cell growth/proliferation but also actively induce immunosuppressive conditions, which also play a major role in the development and progression of this B cell malignancy. These effects are partially mediated by recruited regulatory T cells (Tregs)[57,58], which suppress anticancer immunity by secreting anti-inflammatory cytokines and/or expressing immune inhibitory surface receptors[59,60]. Furthermore, activated tumor-infiltrating T cells have dysfunctional cytolytic capacity in MALT lymphomas[61,62].
It has been demonstrated that T cells, macrophages and neutrophils recruited during long-lasting chronic inflammation contribute to the formation of genetic aberrations, DNA damage and genetic instability in B cells, leading to antigen-independent lymphoma cell growth. These effects are mediated by activation of ASHM and class-switching recombination in MALT lymphomas[63] and are associated with epigenetic and genetic changes in p57KIP[24], p16INK4A[24,64] and p53[10] as well as chromosomal translocation of cMYC and BCL6[10,65].
As already described, MALT lymphomas with long-lasting chronic infections cause B cell proliferation and/or survival either directly and/or indirectly via activation of immune cells[9,43,45,66]. Therefore, these interactions provide multiple potential targets for new immunomodulatory treatments beyond the established treatment options for H. pylori eradication by antibiotics, radiation, chemotherapy and treatment with the anti-CD20 antibody therapy rituximab[67].
Immunomodulatory drugs (IMiDs) represent a novel therapeutic approach to target the tumor microenvironment of MALT lymphomas. IMiDs, consisting of thalidomide, lenalidomide and pomalidomide, are approved for the treatment of multiple myeloma, and lenalidomide is approved for the treatment of relapsed follicular lymphoma[53,68-70]. IMiDs exert anti-inflammatory effects, such as decreased production of cytokines and increased production of Th1 type cytokines; furthermore, they decrease vascular endothelial growth factor (VEGF) levels and show modulating effects on basic cellular mechanisms (T cell costimulation and alteration of FOXP3+ Tregs and natural killer cells)[68,69]. The efficacy of lenalidomide in MALT lym
Further therapeutic targets are related to Tregs, which are recruited into the microenvironment of MALT lymphoma[58,72] and suppress antitumoral immune reactions[58,60,73,74]. It has been shown that the Bruton’s kinase inhibitor ibrutinib reduces the number of Tregs in the early course of treatment in chronic lymphocytic leukemia (CLL), in addition to inhibiting the BCR pathway[75]. Ibrutinib has been tested in relapsed/refractory marginal zone B cell lymphoma (MZL) and possesses a remarkable response rate with tolerable toxicity[53]. However, no data are available thus far for the treatment of MALT lymphoma.
As reported in section 3, in MALT lymphoma cells, the NF-κB pathway is strongly activated by genetic alterations[18,76,77] or by interaction with activated immune cells via the CD40/CD40L[52-54,56] and/or APRIL axes[77-79].
Bortezomib, a proteasome inhibitor with inhibitory effects on the NF-κB signaling pathway[10], showed promising response rates in MALT lymphoma patients in phase II trials[80]. Furthermore, bortezomib was reported to reverses the tumor-induced dysfunction of CD8+ T cells by increasing the expression of Notch cascade genes[81]. Moreover, bortezomib enacts immunostimulatory effects by activating tumor-infiltrating CD8+ T cells[61,62]. Taken together, these findings suggest that the anti-lymphoma effects of bortezomib are mediated by NF-κB inhibition and by reversal of the observed T cell malfunction[52-54].
Another possibility to suppress NF-κB activation in MALT lymphoma cells is the disruption of the APRIL axis[82] with use of an anti-APRIL antibody; one such antibody was developed by Guadagnoli et al[82] and has shown promising results in CLL in a preclinical setting[83-89]. However, this strategy has not been tested in MALT lymphoma patients thus far.
It has also been demonstrated that macrolides, which are used for eradication of bacterial infection in MALT lymphomas, have certain immunomodulatory effects, e.g., they decrease the number and inhibit the function of neutrophils as well as eosinophils and inhibit Th2 cell functions[83-89]. Thus, it is likely that the immunomodulatory effects significantly impact the response rates of MALT lymphomas when these antimicrobial drugs are used.
MALT lymphomas represent a heterogeneous group of lymphoid neoplasms arising at different extranodal sites and are associated with a variety of long-lasting chronic infections. In the current pathogenic model, (auto) antigen stimuli trigger lymphoma cell growth, survival, and recruitment of immune cells to the microenvironment, which in turn stimulate lymphoma cells directly via surface receptor interactions and/or indirectly via cytokine secretion. Moreover, it has been shown that inflammatory processes may lead to the acquisition of further genetic alterations resulting in lymphoma cell growth independent of (auto) antigen stimuli. Many agents targe
We thank Waha JE for reviewing the manuscript for clarity in English as a native speaker.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Austria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Asano N S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983;52:1410-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 2. | A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. The Non-Hodgkin's Lymphoma Classification Project. Blood. 1997;89:3909-3918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1957] [Cited by in RCA: 1796] [Article Influence: 64.1] [Reference Citation Analysis (0)] |
| 3. | Olszewski AJ, Castillo JJ. Survival of patients with marginal zone lymphoma: analysis of the Surveillance, Epidemiology, and End Results database. Cancer. 2013;119:629-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 162] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 4. | Isaacson PG, Du MQ. MALT lymphoma: from morphology to molecules. Nat Rev Cancer. 2004;4:644-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 364] [Cited by in RCA: 321] [Article Influence: 15.3] [Reference Citation Analysis (1)] |
| 5. | Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H. Weltgesundheitsorganisation. WHO classification of tumours of haematopoietic and lymphoid tissues. [cited 12 January 2021]. In: International Agency for Research on Cancer [Internet]. Available from: https://publications.iarc.fr/Book-And-Report-Series/Who-Classification-Of-Tumours/WHO-Classification-Of-Tumours-Of-Haematopoietic-And-Lymphoid-Tissues-2017. |
| 6. | Efremov DG, Turkalj S, Laurenti L. Mechanisms of B Cell Receptor Activation and Responses to B Cell Receptor Inhibitors in B Cell Malignancies. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 7. | Cerutti A, Cols M, Puga I. Marginal zone B cells: virtues of innate-like antibody-producing lymphocytes. Nat Rev Immunol. 2013;13:118-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 554] [Article Influence: 46.2] [Reference Citation Analysis (0)] |
| 8. | Zucca E, Bertoni F, Vannata B, Cavalli F. Emerging role of infectious etiologies in the pathogenesis of marginal zone B-cell lymphomas. Clin Cancer Res. 2014;20:5207-5216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 9. | Kiesewetter B, Raderer M. Immunomodulatory treatment for mucosa-associated lymphoid tissue lymphoma (MALT lymphoma). Hematol Oncol. 2020;38:417-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Troppan K, Wenzl K, Neumeister P, Deutsch A. Molecular Pathogenesis of MALT Lymphoma. Gastroenterol Res Pract. 2015;2015:102656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 11. | Krugmann J, Tzankov A, Dirnhofer S, Fend F, Wolf D, Siebert R, Probst P, Erdel M. Complete or partial trisomy 3 in gastro-intestinal MALT lymphomas co-occurs with aberrations at 18q21 and correlates with advanced disease stage: a study on 25 cases. World J Gastroenterol. 2005;11:7384-7385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Taji S, Nomura K, Matsumoto Y, Sakabe H, Yoshida N, Mitsufuji S, Nishida K, Horiike S, Nakamura S, Morita M, Taniwaki M. Trisomy 3 may predict a poor response of gastric MALT lymphoma to Helicobacter pylori eradication therapy. World J Gastroenterol. 2005;11:89-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Kwee I, Rancoita PM, Rinaldi A, Ferreri AJ, Bhagat G, Gascoyne RD, Canzonieri V, Gaidano G, Doglioni C, Zucca E, Ponzoni M, Bertoni F. Genomic profiles of MALT lymphomas: variability across anatomical sites. Haematologica. 2011;96:1064-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Dierlamm J, Wlodarska I, Michaux L, Stefanova M, Hinz K, Van Den Berghe H, Hagemeijer A, Hossfeld DK. Genetic abnormalities in marginal zone B-cell lymphoma. Hematol Oncol. 2000;18:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Deutsch AJ, Aigelsreiter A, Steinbauer E, Frühwirth M, Kerl H, Beham-Schmid C, Schaider H, Neumeister P. Distinct signatures of B-cell homeostatic and activation-dependent chemokine receptors in the development and progression of extragastric MALT lymphomas. J Pathol. 2008;215:431-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Willis TG, Jadayel DM, Du MQ, Peng H, Perry AR, Abdul-Rauf M, Price H, Karran L, Majekodunmi O, Wlodarska I, Pan L, Crook T, Hamoudi R, Isaacson PG, Dyer MJ. Bcl10 is involved in t(1;14)(p22;q32) of MALT B cell lymphoma and mutated in multiple tumor types. Cell. 1999;96:35-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 531] [Cited by in RCA: 491] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 17. | Bertoni F, Zucca E. Delving deeper into MALT lymphoma biology. J Clin Invest. 2006;116:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Lucas PC, Yonezumi M, Inohara N, McAllister-Lucas LM, Abazeed ME, Chen FF, Yamaoka S, Seto M, Nunez G. Bcl10 and MALT1, independent targets of chromosomal translocation in malt lymphoma, cooperate in a novel NF-kappa B signaling pathway. J Biol Chem. 2001;276:19012-19019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 314] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 19. | Uren AG, O'Rourke K, Aravind LA, Pisabarro MT, Seshagiri S, Koonin EV, Dixit VM. Identification of paracaspases and metacaspases: two ancient families of caspase-like proteins, one of which plays a key role in MALT lymphoma. Mol Cell. 2000;6:961-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 350] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 20. | Deutsch AJ, Frühwirth M, Aigelsreiter A, Cerroni L, Neumeister P. Primary cutaneous marginal zone B-cell lymphomas are targeted by aberrant somatic hypermutation. J Invest Dermatol. 2009;129:476-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Moody S, Thompson JS, Chuang SS, Liu H, Raderer M, Vassiliou G, Wlodarska I, Wu F, Cogliatti S, Robson A, Ashton-Key M, Bi Y, Goodlad J, Du MQ. Novel GPR34 and CCR6 mutation and distinct genetic profiles in MALT lymphomas of different sites. Haematologica. 2018;103:1329-1336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 22. | Lenz G, Davis RE, Ngo VN, Lam L, George TC, Wright GW, Dave SS, Zhao H, Xu W, Rosenwald A, Ott G, Muller-Hermelink HK, Gascoyne RD, Connors JM, Rimsza LM, Campo E, Jaffe ES, Delabie J, Smeland EB, Fisher RI, Chan WC, Staudt LM. Oncogenic CARD11 mutations in human diffuse large B cell lymphoma. Science. 2008;319:1676-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 649] [Cited by in RCA: 685] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 23. | Li ZM, Rinaldi A, Cavalli A, Mensah AA, Ponzoni M, Gascoyne RD, Bhagat G, Zucca E, Bertoni F. MYD88 somatic mutations in MALT lymphomas. Br J Haematol. 2012;158:662-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Min KO, Seo EJ, Kwon HJ, Lee EJ, Kim WI, Kang CS, Kim KM. Methylation of p16(INK4A) and p57(KIP2) are involved in the development and progression of gastric MALT lymphomas. Mod Pathol. 2006;19:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Deutsch AJ, Aigelsreiter A, Staber PB, Beham A, Linkesch W, Guelly C, Brezinschek RI, Fruhwirth M, Emberger W, Buettner M, Beham-Schmid C, Neumeister P. MALT lymphoma and extranodal diffuse large B-cell lymphoma are targeted by aberrant somatic hypermutation. Blood. 2007;109:3500-3504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Bödör C, Bognár A, Reiniger L, Szepesi A, Tóth E, Kopper L, Matolcsy A. Aberrant somatic hypermutation and expression of activation-induced cytidine deaminase mRNA in mediastinal large B-cell lymphoma. Br J Haematol. 2005;129:373-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Küppers R, Dalla-Favera R. Mechanisms of chromosomal translocations in B cell lymphomas. Oncogene. 2001;20:5580-5594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 463] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 28. | Matsumoto Y, Marusawa H, Kinoshita K, Endo Y, Kou T, Morisawa T, Azuma T, Okazaki IM, Honjo T, Chiba T. Helicobacter pylori infection triggers aberrant expression of activation-induced cytidine deaminase in gastric epithelium. Nat Med. 2007;13:470-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 379] [Cited by in RCA: 382] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 29. | Isaacson PG, Spencer J. The biology of low grade MALT lymphoma. J Clin Pathol. 1995;48:395-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 52] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Wotherspoon AC, Ortiz-Hidalgo C, Falzon MR, Isaacson PG. Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet. 1991;338:1175-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1293] [Cited by in RCA: 1201] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 31. | Cerroni L, Zöchling N, Pütz B, Kerl H. Infection by Borrelia burgdorferi and cutaneous B-cell lymphoma. J Cutan Pathol. 1997;24:457-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 268] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 32. | Parsonnet J, Isaacson PG. Bacterial infection and MALT lymphoma. N Engl J Med. 2004;350:213-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 97] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 33. | Adam P, Czapiewski P, Colak S, Kosmidis P, Tousseyn T, Sagaert X, Boudova L, Okoń K, Morresi-Hauf A, Agostinelli C, Pileri S, Pruneri G, Martinelli G, Du MQ, Fend F. Prevalence of Achromobacter xylosoxidans in pulmonary mucosa-associated lymphoid tissue lymphoma in different regions of Europe. Br J Haematol. 2014;164:804-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 34. | Ferreri AJ, Guidoboni M, Ponzoni M, De Conciliis C, Dell'Oro S, Fleischhauer K, Caggiari L, Lettini AA, Dal Cin E, Ieri R, Freschi M, Villa E, Boiocchi M, Dolcetti R. Evidence for an association between Chlamydia psittaci and ocular adnexal lymphomas. J Natl Cancer Inst. 2004;96:586-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 376] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 35. | Chanudet E, Adam P, Nicholson AG, Wotherspoon AC, Ranaldi R, Goteri G, Pileri SA, Ye H, Müller-Hermelink HK, Du MQ. Chlamydiae and Mycoplasma infections in pulmonary MALT lymphoma. Br J Cancer. 2007;97:949-951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 36. | Aigelsreiter A, Gerlza T, Deutsch AJ, Leitner E, Beham-Schmid C, Beham A, Popper H, Borel N, Pospischil A, Raderer M, Kessler HH, Neumeister P. Chlamydia psittaci Infection in nongastrointestinal extranodal MALT lymphomas and their precursor lesions. Am J Clin Pathol. 2011;135:70-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 37. | Negri E, Little D, Boiocchi M, La Vecchia C, Franceschi S. B-cell non-Hodgkin's lymphoma and hepatitis C virus infection: a systematic review. Int J Cancer. 2004;111:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 122] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 38. | Aoyama S, Masaki A, Sakamoto Y, Takino H, Murase T, Ohshima K, Yoshino T, Kato S, Inagaki H. Achromobacter Infection Is Rare in Japanese Patients with Pulmonary B-cell Lymphoma. Intern Med. 2018;57:789-794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 39. | Carugi A, Onnis A, Antonicelli G, Rossi B, Mannucci S, Luzzi A, Lazzi S, Bellan C, Tosi GM, Sayed S, De Falco G, Leoncini L. Geographic variation and environmental conditions as cofactors in Chlamydia psittaci association with ocular adnexal lymphomas: a comparison between Italian and African samples. Hematol Oncol. 2010;28:20-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | Chanudet E, Zhou Y, Bacon CM, Wotherspoon AC, Müller-Hermelink HK, Adam P, Dong HY, de Jong D, Li Y, Wei R, Gong X, Wu Q, Ranaldi R, Goteri G, Pileri SA, Ye H, Hamoudi RA, Liu H, Radford J, Du MQ. Chlamydia psittaci is variably associated with ocular adnexal MALT lymphoma in different geographical regions. J Pathol. 2006;209:344-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 181] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 41. | Wöhrer S, Troch M, Streubel B, Zwerina J, Skrabs C, Formanek M, Hauff W, Hoffmann M, Müllauer L, Chott A, Raderer M. MALT lymphoma in patients with autoimmune diseases: a comparative analysis of characteristics and clinical course. Leukemia. 2007;21:1812-1818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 42. | Ferraccioli GF, Sorrentino D, De Vita S, Casatta L, Labombarda A, Avellini C, Dolcetti R, Di Luca D, Beltrami CA, Boiocchi M, Bartoli E. B cell clonality in gastric lymphoid tissues of patients with Sjögren's syndrome. Ann Rheum Dis. 1996;55:311-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | Nocturne G, Mariette X. Sjögren Syndrome-associated lymphomas: an update on pathogenesis and management. Br J Haematol. 2015;168:317-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 199] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 44. | Troch M, Woehrer S, Streubel B, Weissel M, Hoffmann M, Müllauer L, Chott A, Raderer M. Chronic autoimmune thyroiditis (Hashimoto's thyroiditis) in patients with MALT lymphoma. Ann Oncol. 2008;19:1336-1339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 45. | Umehara S, Higashi H, Ohnishi N, Asaka M, Hatakeyama M. Effects of Helicobacter pylori CagA protein on the growth and survival of B lymphocytes, the origin of MALT lymphoma. Oncogene. 2003;22:8337-8342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 46. | Kuo SH, Wu MS, Yeh KH, Lin CW, Hsu PN, Chen LT, Cheng AL. Novel Insights of Lymphomagenesis of Helicobacter pylori-Dependent Gastric Mucosa-Associated Lymphoid Tissue Lymphoma. Cancers (Basel). 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 47. | Lin WC, Tsai HF, Kuo SH, Wu MS, Lin CW, Hsu PI, Cheng AL, Hsu PN. Translocation of Helicobacter pylori CagA into Human B lymphocytes, the origin of mucosa-associated lymphoid tissue lymphoma. Cancer Res. 2010;70:5740-5748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 48. | Slomiany BL, Slomiany A. Syk: a new target for attenuation of Helicobacter pylori-induced gastric mucosal inflammatory responses. Inflammopharmacology. 2019;27:203-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 49. | Slomiany BL, Slomiany A. Role of LPS-elicited signaling in triggering gastric mucosal inflammatory responses to H. pylori: modulatory effect of ghrelin. Inflammopharmacology. 2017;25:415-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 50. | Clark EA, Ledbetter JA. How B and T cells talk to each other. Nature. 1994;367:425-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 454] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 51. | Nakamura H, Kawakami A, Tominaga M, Migita K, Kawabe Y, Nakamura T, Eguchi K. Expression of CD40/CD40 Ligand and Bcl-2 family proteins in labial salivary glands of patients with Sjögren's syndrome. Lab Invest. 1999;79:261-269. [PubMed] |
| 52. | Blosse A, Peru S, Levy M, Marteyn B, Floch P, Sifré E, Giese A, Prochazkova-Carlotti M, Azzi Martin L, Dubus P, Mégraud F, Ruskone Fournestraux A, Fabiani B, Copie Bergman C, Robe C, Hahne M, Huard B, Lehours P. APRIL-producing eosinophils are involved in gastric MALT lymphomagenesis induced by Helicobacter sp infection. Sci Rep. 2020;10:14858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 53. | Raderer M, Kiesewetter B. What you always wanted to know about gastric MALT-lymphoma: a focus on recent developments. Ther Adv Med Oncol. 2021;13:17588359211033825. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 54. | Stergiou IE, Poulaki A, Voulgarelis M. Pathogenetic Mechanisms Implicated in Sjögren's Syndrome Lymphomagenesis: A Review of the Literature. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 55. | Elgueta R, Benson MJ, de Vries VC, Wasiuk A, Guo Y, Noelle RJ. Molecular mechanism and function of CD40/CD40L engagement in the immune system. Immunol Rev. 2009;229:152-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 836] [Cited by in RCA: 1142] [Article Influence: 71.4] [Reference Citation Analysis (0)] |
| 56. | Bossen C, Schneider P. BAFF, APRIL and their receptors: structure, function and signaling. Semin Immunol. 2006;18:263-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 387] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 57. | Craig VJ, Cogliatti SB, Arnold I, Gerke C, Balandat JE, Wündisch T, Müller A. B-cell receptor signaling and CD40 Ligand-independent T cell help cooperate in Helicobacter-induced MALT lymphomagenesis. Leukemia. 2010;24:1186-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 58. | García M, Bellosillo B, Sánchez-González B, García-Payarols F, Seoane A, Ferrer AM, Gimeno E, Barranco LE, Torner A, Solé F, Besses C, Serrano S, Salar A. Study of regulatory T-cells in patients with gastric malt lymphoma: influence on treatment response and outcome. PLoS One. 2012;7:e51681. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 59. | Curiel TJ. Regulatory T cells and treatment of cancer. Curr Opin Immunol. 2008;20:241-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 200] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 60. | Togashi Y, Shitara K, Nishikawa H. Regulatory T cells in cancer immunosuppression - implications for anticancer therapy. Nat Rev Clin Oncol. 2019;16:356-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 497] [Cited by in RCA: 1030] [Article Influence: 171.7] [Reference Citation Analysis (0)] |
| 61. | D'Elios MM, Amedei A, Manghetti M, Costa F, Baldari CT, Quazi AS, Telford JL, Romagnani S, Del Prete G. Impaired T-cell regulation of B-cell growth in Helicobacter pylori--related gastric low-grade MALT lymphoma. Gastroenterology. 1999;117:1105-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 75] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 62. | Bergman MP, D'Elios MM. Cytotoxic T cells in H. pylori-related gastric autoimmunity and gastric lymphoma. J Biomed Biotechnol. 2010;2010:104918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 63. | Thieblemont C, Bertoni F, Copie-Bergman C, Ferreri AJ, Ponzoni M. Chronic inflammation and extra-nodal marginal-zone lymphomas of MALT-type. Semin Cancer Biol. 2014;24:33-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 64. | Neumeister P, Hoefler G, Beham-Schmid C, Schmidt H, Apfelbeck U, Schaider H, Linkesch W, Sill H. Deletion analysis of the p16 tumor suppressor gene in gastrointestinal mucosa-associated lymphoid tissue lymphomas. Gastroenterology. 1997;112:1871-1875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 65. | Liang R, Chan WP, Kwong YL, Xu WS, Srivastava G, Ho FC. High incidence of BCL-6 gene rearrangement in diffuse large B-cell lymphoma of primary gastric origin. Cancer Genet Cytogenet. 1997;97:114-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 66. | Hussell T, Isaacson PG, Crabtree JE, Spencer J. Helicobacter pylori-specific tumour-infiltrating T cells provide contact dependent help for the growth of malignant B cells in low-grade gastric lymphoma of mucosa-associated lymphoid tissue. J Pathol. 1996;178:122-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 67. | Zucca E, Arcaini L, Buske C, Johnson PW, Ponzoni M, Raderer M, Ricardi U, Salar A, Stamatopoulos K, Thieblemont C, Wotherspoon A, Ladetto M; ESMO Guidelines Committee. Marginal zone lymphomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:17-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 219] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 68. | Kotla V, Goel S, Nischal S, Heuck C, Vivek K, Das B, Verma A. Mechanism of action of lenalidomide in hematological malignancies. J Hematol Oncol. 2009;2:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 286] [Cited by in RCA: 340] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 69. | Quach H, Ritchie D, Stewart AK, Neeson P, Harrison S, Smyth MJ, Prince HM. Mechanism of action of immunomodulatory drugs (IMiDS) in multiple myeloma. Leukemia. 2010;24:22-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 395] [Cited by in RCA: 465] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 70. | Leonard JP, Trneny M, Izutsu K, Fowler NH, Hong X, Zhu J, Zhang H, Offner F, Scheliga A, Nowakowski GS, Pinto A, Re F, Fogliatto LM, Scheinberg P, Flinn IW, Moreira C, Cabeçadas J, Liu D, Kalambakas S, Fustier P, Wu C, Gribben JG; AUGMENT Trial Investigators. AUGMENT: A Phase III Study of Lenalidomide Plus Rituximab Versus Placebo Plus Rituximab in Relapsed or Refractory Indolent Lymphoma. J Clin Oncol. 2019;37:1188-1199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 179] [Cited by in RCA: 293] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 71. | Kiesewetter B, Troch M, Mayerhoefer ME, Dolak W, Simonitsch-Klupp I, Raderer M. Delayed Efficacy After Treatment With Lenalidomide or Thalidomide in Patients With Mucosa-Associated Lymphoid Tissue Lymphoma. Oncologist. 2016;21:72-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 72. | Bagheri N, Azadegan-Dehkordi F, Rahimian G, Rafieian-Kopaei M, Shirzad H. Role of Regulatory T-cells in Different Clinical Expressions of Helicobacter pylori Infection. Arch Med Res. 2016;47:245-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 73. | Laur AM, Floch P, Chambonnier L, Benejat L, Korolik V, Giese A, Dubus P, Mégraud F, Bandeira A, Lehours P. Regulatory T cells may participate in Helicobacter pylori persistence in gastric MALT lymphoma: lessons from an animal model. Oncotarget. 2016;7:3394-3402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 74. | Iwaya Y, Kobayashi M, Momose M, Hiraoka N, Sakai Y, Akamatsu T, Tanaka E, Ohtani H, Fukuda M, Nakayama J. High levels of FOXP3⁺ regulatory T cells in gastric MALT lymphoma predict responsiveness to Helicobacter pylori eradication. Helicobacter. 2013;18:356-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 75. | Podhorecka M, Goracy A, Szymczyk A, Kowal M, Ibanez B, Jankowska-Lecka O, Macheta A, Nowaczynska A, Drab-Urbanek E, Chocholska S, Jawniak D, Hus M. Changes in T-cell subpopulations and cytokine network during early period of ibrutinib therapy in chronic lymphocytic leukemia patients: the significant decrease in T regulatory cells number. Oncotarget. 2017;8:34661-34669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 76. | Liu F, Karube K, Kato H, Arita K, Yoshida N, Yamamoto K, Tsuzuki S, Kim W, Ko YH, Seto M. Mutation analysis of NF-κB signal pathway-related genes in ocular MALT lymphoma. Int J Clin Exp Pathol. 2012;5:436-441. [PubMed] |
| 77. | McAllister-Lucas LM, Inohara N, Lucas PC, Ruland J, Benito A, Li Q, Chen S, Chen FF, Yamaoka S, Verma IM, Mak TW, Núñez G. Bimp1, a MAGUK family member linking protein kinase C activation to Bcl10-mediated NF-kappaB induction. J Biol Chem. 2001;276:30589-30597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 145] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 78. | Hozak RR, Manji GA, Friesen PD. The BIR motifs mediate dominant interference and oligomerization of inhibitor of apoptosis Op-IAP. Mol Cell Biol. 2000;20:1877-1885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 79. | Panwalkar A, Verstovsek S, Giles F. Nuclear factor-kappaB modulation as a therapeutic approach in hematologic malignancies. Cancer. 2004;100:1578-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 78] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 80. | Thounaojam MC, Dudimah DF, Pellom ST Jr, Uzhachenko RV, Carbone DP, Dikov MM, Shanker A. Bortezomib enhances expression of effector molecules in anti-tumor CD8+ T lymphocytes by promoting Notch-nuclear factor-κB crosstalk. Oncotarget. 2015;6:32439-32455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 81. | Pellom ST Jr, Dudimah DF, Thounaojam MC, Uzhachenko RV, Singhal A, Richmond A, Shanker A. Bortezomib augments lymphocyte stimulatory cytokine signaling in the tumor microenvironment to sustain CD8+T cell antitumor function. Oncotarget. 2017;8:8604-8621. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 82. | Guadagnoli M, Kimberley FC, Phan U, Cameron K, Vink PM, Rodermond H, Eldering E, Kater AP, van Eenennaam H, Medema JP. Development and characterization of APRIL antagonistic monoclonal antibodies for treatment of B-cell lymphomas. Blood. 2011;117:6856-6865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 83. | Zimmermann P, Ziesenitz VC, Curtis N, Ritz N. The Immunomodulatory Effects of Macrolides-A Systematic Review of the Underlying Mechanisms. Front Immunol. 2018;9:302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 188] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 84. | Ghosh N, Tucker N, Zahurak M, Wozney J, Borrello I, Huff CA. Clarithromycin overcomes resistance to lenalidomide and dexamethasone in multiple myeloma. Am J Hematol. 2014;89:E116-E120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 85. | Van Nuffel AM, Sukhatme V, Pantziarka P, Meheus L, Sukhatme VP, Bouche G. Repurposing Drugs in Oncology (ReDO)-clarithromycin as an anti-cancer agent. Ecancermedicalscience. 2015;9:513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 86. | Li L, Sun R, Miao Y, Tran T, Adams L, Roscoe N, Xu B, Manyam GC, Tan X, Zhang H, Xiao M, Tzankov A, Visco C, Dybkaer K, Bhagat G, Tam W, Hsi ED, van Krieken JH, You H, Huh J, Ponzoni M, Ferreri AJM, Møller MB, Piris MA, Zhang M, Winter JN, Medeiros LJ, Rassidakis GZ, Vaupel CA, Li Y, Dakappagari N, Xu-Monette ZY, Young KH. PD-1/PD-L1 expression and interaction by automated quantitative immunofluorescent analysis show adverse prognostic impact in patients with diffuse large B-cell lymphoma having T-cell infiltration: a study from the International DLBCL Consortium Program. Mod Pathol. 2019;32:741-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 87. | Ferreri AJ, Sassone M, Kiesewetter B, Govi S, Scarfò L, Donadoni G, Raderer M. High-dose clarithromycin is an active monotherapy for patients with relapsed/refractory extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT): the HD-K phase II trial. Ann Oncol. 2015;26:1760-1765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 88. | Ferreri AJM, Cecchetti C, Kiesewetter B, Sassone M, Calimeri T, Perrone S, Ponzoni M, Raderer M. Clarithromycin as a "repurposing drug" against MALT lymphoma. Br J Haematol. 2018;182:913-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 89. | Govi S, Dognini GP, Licata G, Crocchiolo R, Resti AG, Ponzoni M, Ferreri AJ. Six-month oral clarithromycin regimen is safe and active in extranodal marginal zone B-cell lymphomas: final results of a single-centre phase II trial. Br J Haematol. 2010;150:226-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |