Published online Apr 15, 2020. doi: 10.4251/wjgo.v12.i4.405
Peer-review started: September 19, 2019
First decision: October 18, 2019
Revised: December 10, 2019
Accepted: December 23, 2019
Article in press: December 23, 2019
Published online: April 15, 2020
Processing time: 209 Days and 8 Hours
Primary tumor location is a prognostic factor for metastatic colorectal cancer (mCRC). Post hoc analyses of mCRC clinical trials, including FIRE-3, CALGB/SWOG 80405, suggest that primary tumor location is also predictive of survival benefit with cetuximab or bevacizumab in combination with 5-fluorouracil-based chemotherapy.
Evaluate prognostic/predictive roles of primary tumor location in real-world mCRC patients treated with cetuximab or bevacizumab plus 5-fluorouracil-based chemotherapy.
This retrospective cohort study selected patients with KRAS wild-type mCRC who initiated first-line therapy with cetuximab or bevacizumab in combination with 5-fluorouracil/leucovorin/irinotecan (FOLFIRI) or 5-fluorouracil/ leucovorin/oxaliplatin (FOLFOX) between January 2013 and April 2017 from the Flatiron Health electronic health record-derived database of de-identified patient-level data in the United States. Primary tumor location was abstracted from patients’ charts. Left-sided primary tumor location (LPTL) was defined as tumors that originated in the splenic flexure, descending colon, sigmoid colon, or rectum; right-sided primary tumor location (RPTL) was defined as tumors that originated from the appendix, cecum, ascending colon, hepatic flexure, or transverse colon. Propensity score matching was used to balance the baseline demographic and clinical characteristics between patients treated with cetuximab and patients treated with bevacizumab. Kaplan-Meier and Cox regression methods were used for survival analyses.
A total of 1312 patients met the selection criteria. Of 248 cetuximab plus FOLFIRI or FOLFOX patients, 164 had LPTL and 84 had RPTL; of 1064 bevacizumab plus FOLFIRI or FOLFOX patients, 679 had LPTL and 385 had RPTL. Cetuximab LPTL and RPTL patients were more likely to receive FOLFIRI vs bevacizumab patients (LPTL: 64.0% vs 24.3%; RPTL: 76.2% vs 24.9%, P < 0.001). Stage at initial diagnosis was different between cetuximab RPTL vs bevacizumab RPTL patients (P < 0.001); cetuximab RPTL patients were more likely to have stage III disease (44.0% vs 22.6%), while bevacizumab RPTL patients were more likely to have stage IV disease (65.7% vs 48.8%). Cetuximab RPTL patients were more likely to have a documented history of adjuvant chemotherapy vs bevacizumab RPTL patients (47.6% vs 22.3%, P < 0.001). In the propensity score-matched sample, median overall survival (OS) was 29.7 mo (95%CI: 26.9-35.2) for LPTL patients vs 18.3 mo (95%CI: 15.8-21.3) for RPTL patients (P < 0.001). Median OS was 29.7 mo (95%CI: 27.4-NA) for cetuximab LPTL patients vs 29.1 mo (95%CI: 26.6-35.6) for bevacizumab LPTL patients (HR = 0.87; 95%CI: 0.63-1.19; P = 0.378) and 17.0 mo (95%CI: 12.0-32.6) for cetuximab RPTL patients vs 18.8 mo (95%CI: 15.8-22.3) for bevacizumab RPTL patients (HR = 1.00; 95%CI: 0.68-1.46; P = 0.996). The interaction of treatment and primary tumor location was not significant in the Cox regression.
In this real-world mCRC cohort, the prognostic role of primary tumor location was substantiated, but not the predictive role for treatment with cetuximab vs bevacizumab in combination with 5-fluorouracil-based chemotherapy.
Core tip: Primary tumor location is a prognostic factor for metastatic colorectal cancer. Post hoc analyses of randomized clinical trials, including FIRE-3 and CALGB/SWOG 80405, suggest that primary tumor location is also predictive of survival benefit with cetuximab and bevacizumab in metastatic colorectal cancer patients. This analysis of a large cohort of real-world patients with KRAS wild-type metastatic colorectal cancer who received first-line treatment with cetuximab or bevacizumab with 5-fluorouracil-based chemotherapy found a prognostic effect of primary tumor location but not a predictive effect, possibly due to differences between patients in real-world clinical practice vs clinical trial settings.
- Citation: Aggarwal H, Sheffield KM, Li L, Lenis D, Sorg R, Barzi A, Miksad R. Primary tumor location and survival in colorectal cancer: A retrospective cohort study. World J Gastrointest Oncol 2020; 12(4): 405-423
- URL: https://www.wjgnet.com/1948-5204/full/v12/i4/405.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v12.i4.405
Metastatic colorectal cancer (mCRC) is a heterogeneous disease with differing outcomes and clinical responses, in part due to differences in chromosomal and molecular profiles between primary tumors that arise from the left (distal) and right (proximal) sides of the colon[1]. During gastrulation, both the left (hindgut) and right (midgut) sides of the gut develop from the endoderm. The left side gives rise to the distal third of the transverse colon, splenic flexure, descending colon, sigmoid rectum and the upper part of the anal canal, whereas the right side gives rise to the duodenum distal to the ampulla, the entire small bowel, the cecum, appendix, ascending colon, and the proximal two-thirds of the transverse colon[2].
Right-sided primary tumor location (RPTL) has been shown to be associated with several adverse prognostic factors compared with left-sided primary tumor location (LPTL), including point mutations in codon 600 of BRAF; point mutations in codons 12 and 13 of KRAS and 61 of NRAS; point mutations in exons 9 and 20 of phosphoino-sitide 3-kinase; frameshift and nonsense mutations in transforming growth factor-β receptor-2; hypermutation; and microsatellite instability[3-6]. In contrast, LPTL is more likely than RPTL to be associated with overexpression of epidermal growth factor receptor (EGFR) or human epidermal growth factor receptor 2 (HER2) and vascular endothelial growth factor, high epiregulin, and chromosomal instability[3-5]. RPTL is more common in women than men and is associated with a higher median age at diagnosis than LPTL[7].
As a result of these clinical and molecular differences between the left and right sides of the colon, primary tumor location is a prognostic factor; a meta-analysis of 66 studies showed that patients with LPTL have significantly longer overall survival (OS) than patients with RPTL[8]. This meta-analysis, which included over 1.4 million patients with early and advanced colorectal cancer (CRC), showed that LPTL was associated with a significantly reduced risk of death compared with RPTL (HR = 0.82, P < 0.001), and that this was independent of adjuvant chemotherapy, year of study, race, stage, quality of included studies, and number of study participants[8].
Primary tumor location also appears to be a predictive factor of clinical outcomes of CRC treatment with EGFR inhibitors, most likely due to molecular differences between sides of the colon in tumor expression of proteins such as EGFR/HER2, BRAF, vascular endothelial growth factor receptor 2, and excision repair cross complement group 1[9]. In the first-line setting, a retrospective post hoc analysis of the CRYSTAL and FIRE-3 studies showed that cetuximab plus 5-fluorouracil/ leucovorin/irinotecan (FOLFIRI) significantly improved OS compared with FOLFIRI alone or bevacizumab plus FOLFIRI for patients with RAS wild-type (WT) mCRC LPTL (CRYSTAL: 28.7 mo vs 21.7 mo, HR = 0.65, P = 0.002; FIRE-3: 38.3 mo vs 28.0 mo, HR = 0.63, P = 0.002)[10]. Conversely, patients with RPTL derived little or no benefit from cetuximab plus FOLFIRI compared with FOLFIRI alone or bevacizumab plus FOLFIRI (CRYSTAL: 18.5 mo vs 15.0 mo, HR = 1.08, P = 0.76; FIRE-3: 18.3 mo vs 23.0 mo, HR = 1.31, P = 0.28)[10]. Furthermore, a post hoc analysis of the CALGB/SWOG 80405 study showed that cetuximab plus FOLFIRI or 5-fluorouracil/ leucovorin/oxaliplatin (FOLFOX) significantly improved OS compared with bevacizumab plus FOLFIRI or FOLFOX for mCRC patients with LPTL (37.5 mo vs 32.1 mo, P = 0.04)[11]. On the other hand, in patients with RPTL, bevacizumab plus FOLFIRI or FOLFOX significantly improved OS compared with cetuximab plus FOLFIRI or FOLFOX (24.5 mo vs 16.4 mo, P = 0.03)[11]. Results for progression-free survival (PFS) were similar to those for OS[11]. Collectively, these studies indicated that primary tumor location may be predictive of survival outcomes associated with first-line treatment of mCRC with EGFR inhibitors.
In the second-line setting, a retrospective analysis of the FIRE-3 study showed that OS was improved for patients with LPTL who received second-line cetuximab plus irinotecan (after first-line bevacizumab plus FOLFIRI on trial) compared with those who received second-line bevacizumab plus FOLFIRI (after first-line cetuximab plus FOLFIRI on trial) (OS: 17.6 mo vs 14.1 mo, HR = 0.65, P = 0.002), with similar results observed for PFS[12]. For patients with RPTL, there was no difference in efficacy between those who received bevacizumab and those who received cetuximab[12]. Furthermore, a post hoc analysis of the NCIC CO.17 study showed that, in KRAS WT patients, those with LPTL had significantly improved PFS when treated with cetuximab monotherapy compared with best supportive care (5.4 mo vs 1.8 mo, HR = 0.28, P < 0.0001)[13]. On the other hand, those with RPTL did not experience a benefit with cetuximab monotherapy (1.9 mo vs 1.9 mo, HR = 0.73, P = 0.26)[13]. These studies suggest that primary tumor location may also be predictive of survival outcomes following second-line treatment of mCRC with EGFR inhibitors.
Based on an overall assessment of these and other studies, the National Comprehensive Cancer Network recommends that only patients with LPTL RAS WT mCRC be offered cetuximab or panitumumab as first-line treatment for mCRC, whereas bevacizumab can be considered in the first-line setting for patients with RPTL RAS WT mCRC[14]. All patients with RAS WT tumors should be considered for treatment with cetuximab or panitumumab in subsequent lines of therapy if neither was previously given[14].
Most studies that investigated the effect of primary tumor location on biologic therapy efficacy were post hoc analyses of large randomized controlled trials not designed to answer questions about tumor sidedness, or were single institution analyses of small cohorts. Consequently, there is a lack of real-world evidence from large mCRC populations describing the association of primary tumor location with survival outcomes from biologic therapy. This study evaluated the prognostic and predictive role of primary tumor location and its association with survival benefit in real-world patients with KRAS WT mCRC who initiated first-line therapy with cetuximab plus FOLFIRI or FOLFOX vs with bevacizumab plus FOLFIRI or FOLFOX in the United States.
The patients in this retrospective cohort study were selected from Flatiron Health’s electronic health record (EHR)-derived longitudinal demographically and geographically diverse database, which comprises de-identified patient-level structured and unstructured data, curated via technology-enabled abstraction. At the time of this study, it included data from more than 265 community clinics and academic institutions at more than 800 sites of care in the United States. The database has been described in detail previously[15]. In brief, the database was created by aggregating, normalizing, and harmonizing patient-level data. Data were processed centrally and stored in a secure format. Structured data (e.g. treatments) were semantically mapped to standard reference terminologies, whereas unstructured data, including primary tumor location, were extracted from EHR-based digital documents (e.g. medical care notes) via technology-enabled abstraction. Every data point sourced from unstructured documents was manually reviewed by trained chart abstractors[15].
Quality control included duplicate chart abstraction of a sample of critical abstracted variables. Additional quality control was performed covering areas such as demographics and treatment length/dosage, and included both medical and data considerations. Any issues identified were logged, prioritized, investigated, and resolved[15].
Eligible patients aged at least 18 years had an International Statistical Classification of Diseases and Related Health Problems (ICD) code for CRC (ICD-9 153.x, 154.x, ICD-10 C18x, C19x, C20x, or C21x), at least 2 visits in the Flatiron database on or after January 1, 2013, a confirmed diagnosis of stage IV or recurrent metastatic disease on or after January 1, 2013, and documented KRAS WT biomarker status any time before or within 28 d of the start of first-line treatment with either cetuximab in combination with FOLFIRI or FOLFOX, or bevacizumab in combination with FOLFIRI or FOLFOX between January 1, 2013 and April 30, 2017. The enrollment end date of April 30, 2017 was selected to allow for 6 mo of follow-up before the data cutoff date of October 31, 2017. Eligible patients could have less than 6 mo of follow-up data due to death or loss to follow-up.
Exclusion criteria included a greater than 90-d gap between the metastatic diagnosis date and the first structured activity (visit, administration, or order) and receipt of both bevacizumab and cetuximab or FOLFIRI and FOLFOX, or any other drugs (e.g. panitumumab) as part of first-line therapy.
Primary tumor location was abstracted from patients’ charts. For the main analysis, LPTL was defined as tumors that originated in the splenic flexure, descending colon, sigmoid colon, or rectum and RPTL was defined as tumors that originated in the appendix, cecum, ascending colon, hepatic flexure, or transverse colon.
The index date was defined as the date on which first-line therapy containing cetuximab or bevacizumab was initiated, as determined by the first episode of the relevant drugs (i.e. administration or non-cancelled order). The start of first-line therapy was defined as the first episode of an eligible drug that was given after or up to 14 d before the metastatic diagnosis date. All eligible drugs given within 28 d of the start of first-line therapy (i.e. the first eligible drug episode) were considered part of the first-line therapy regimen.
The primary outcome was OS, defined as the time from the index date to the patient’s date of death. Patients without a date of death were censored at their last confirmed activity date (last structured visit or medication administration). The Flatiron Enhanced Mortality variable version 2.0[15] was used to amalgamate internal and external data sources to generate the best understanding of a patient’s vital status and date of death.
The baseline demographic and clinical variables were patients’ age at index date, sex, race, ethnicity, geographic region, practice type (community vs academic), site of disease, stage at initial diagnosis, Eastern Cooperative Oncology Group (ECOG) performance status, modified Charlson Comorbidity Index, NRAS and BRAF mutation status, first-line chemotherapy backbone (FOLFOX vs FOLFIRI), year of cetuximab or bevacizumab initiation, documented history of adjuvant chemotherapy (for patients initially diagnosed at an earlier stage disease who developed recurrent metastases), duration of follow-up time, and duration of first-line therapy. For duration of first-line therapy, patients were classified as having discontinued first-line therapy (i.e. an event) if any of the following occurred: (1) The patient started a subsequent line of therapy; (2) The patient died; or (3) There was a gap of more than 90 d between the patient’s last administration or non-cancelled order for first-line therapy and the last activity date. Patients were censored at the last administration or non-cancelled order for first-line therapy.
Institutional Review Board approval of the study protocol was obtained prior to conduct of the study and included a waiver of informed consent. Data were de-identified and provisions were in place to prevent re-identification in order to protect patient confidentiality. The study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and that are consistent with Good Pharmacoepidemiology Practices and applicable laws and regulations.
Descriptive statistics were generated by primary tumor location and treatment. Chi-square test (or Fisher's exact test if the expected frequency was less than five) for categorical variables or t-test or Wilcoxon rank sum test for means and Kruskall-Wallis test for medians of continuous variables were used to test for statistically significant differences in baseline patient characteristics between cetuximab and bevacizumab within primary tumor location.
Propensity score method using 1:4 matching (i.e. one cetuximab patient matched to up to four bevacizumab patients) was used to balance patients' baseline demographic and clinical characteristics between the cetuximab and bevacizumab cohorts. The probability of receiving first-line cetuximab vs bevacizumab (i.e. the propensity score) was modeled via a logistic regression model. The dependent variable was receipt of cetuximab (yes/no). Independent variables included age at index date, sex, race, stage at initial diagnosis, modified Charlson Comorbidity Index, ethnicity, year of cetuximab or bevacizumab initiation, history of adjuvant chemotherapy, geographic region, side of colon, indicator variable for rectum/rectosigmoid, NRAS and BRAF mutation status, and first-line chemotherapy backbone (FOLFIRI/ FOLFOX). Patients were matched based on the logit of propensity scores using the nearest neighbor algorithm to find matches, and a caliper of 0.20 was used, which represents the number of standard deviations of the distance measure (i.e. logit of the propensity score) within which matches were acceptable. Covariate balance was assessed in the matched sample via visual inspection, computation of mean standardized differences and t-tests of difference-in-means.
Kaplan-Meier and Cox regression methods were used for OS analyses in the matched population. The prognostic effect of primary tumor location was evaluated by comparing OS in patients with LPTL vs RPTL KRAS WT mCRC by treatment. The predictive effect of primary tumor location on OS benefit with cetuximab or bevacizumab was investigated by evaluating the significance (P < 0.05) of the interaction term between primary tumor location (i.e. left vs right) and treatment (i.e. cetuximab vs bevacizumab) in a Cox regression model that included treatment, primary tumor location, and an interaction term between primary tumor location and treatment. Consistent with the methods of Austin et al[16], a stratified (by each matched set) log-rank test was used to compare survival curves, given that the matched patients were not independent. Cox regressions were estimated using clusters defined by each matched set. Several sensitivity analyses were conducted to evaluate the robustness of the findings of the main analysis. Specifically, different propensity score matching procedures, such as: (1) 1:1 matching without a caliper; (2) 1:2 matching (i.e. one cetuximab patient matched to up to 2 bevacizumab patients); and (3) Inverse probability of treatment weighting (IPTW), were implemented. Additionally, an alternative definition for the index date and different definitions for left and right side of colon were also considered. Lastly, different subgroups of patients were considered in order to evaluate whether conclusions obtained in the main analysis held for different patient subgroups. These subgroups included: (1) LPTL mCRC patients only; (2) RPTL mCRC patients only; (3) NRAS mutation-negative patients only; (4) Stage IV at initial diagnosis patients only; (5) Patients with a first-line chemotherapy backbone of FOLFIRI; and (6) Patients with a first-line chemotherapy backbone of FOLFOX.
A two-sided significance level of α = 0.05 was used, whereby P < α was considered statistically significant.
The statistical methods of this study were reviewed by Yajun Emily Zhu from Eli Lilly and Company.
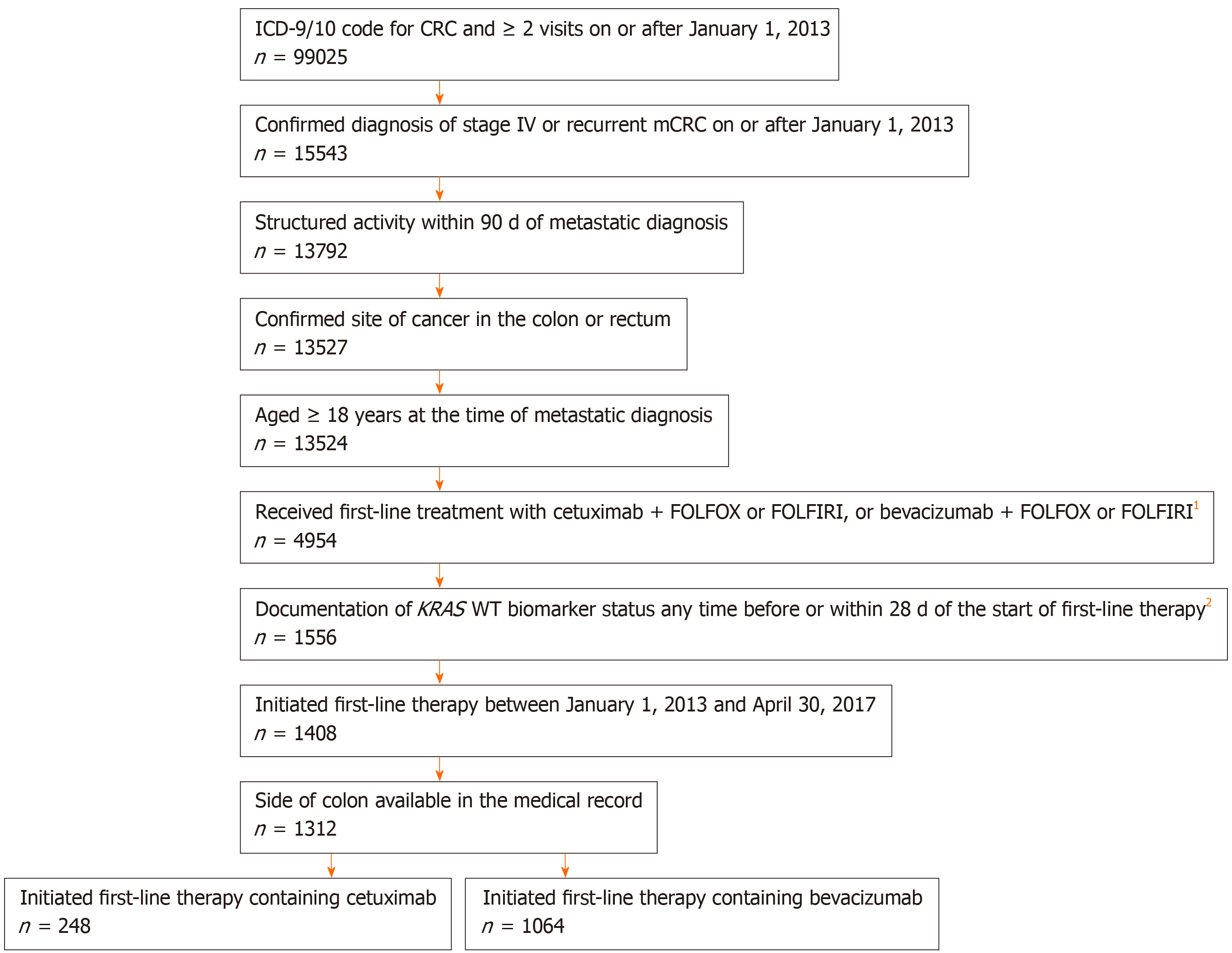
Of the 1312 patients who met the study inclusion and exclusion criteria, 248 received first-line cetuximab plus FOLFIRI or FOLFOX, and 1064 received first-line bevacizumab plus FOLFIRI or FOLFOX. The study profile is shown in Figure 1.
There were notable differences between patients who received cetuximab (n = 248) vs patients who received bevacizumab (n = 1064) (data not shown). Patients who received cetuximab were more likely to be stage III at initial diagnosis and less likely to be stages I, II, and IV than patients who received bevacizumab (stage I: cetuximab 1.2% vs bevacizumab 2.9%; stage II: cetuximab 7.3% vs bevacizumab 10.6%; stage III: cetuximab 32.7% vs bevacizumab 21.8%; stage IV: cetuximab 57.3% vs bevacizumab 62.4%; P = 0.003 for the overall comparison) and were less likely to be tested for NRAS and BRAF mutations (tested for NRAS mutations: cetuximab 31.9% vs bevacizumab 41.4%, P = 0.007; tested for BRAF mutations: cetuximab 32.7% vs bevacizumab 46.0%, P < 0.001). Furthermore, patients who received cetuximab were more likely to receive FOLFIRI as the chemotherapy backbone and less likely to receive FOLFOX as the chemotherapy backbone vs patients who received bevacizumab (FOLFIRI: cetuximab 68.1% vs bevacizumab 24.5%; FOLFOX: cetuximab 31.9% vs bevacizumab 75.5%; P < 0.001), and more likely to have a documented history of adjuvant chemotherapy (cetuximab 36.3% vs bevacizumab 24.0%, P < 0.001) (data not shown).
Of the 248 cetuximab plus FOLFIRI or FOLFOX patients, 164 had LPTL and 84 had RPTL, and of the 1064 bevacizumab plus FOLFIRI or FOLFOX patients, 679 had LPTL and 385 had RPTL. Table 1 compares patient characteristics for those receiving first-line cetuximab vs first-line bevacizumab stratified by primary tumor location before propensity score matching. Patients who received cetuximab were more likely to receive a backbone of FOLFIRI compared with patients who received bevacizumab (LPTL: 64.0% vs 24.3%, P < 0.001; RPTL: 76.2% vs 24.9%, P < 0.001). Patients with RPTL who received cetuximab were more likely to be stage III at initial diagnosis (44.0% vs 22.6%) and less likely to be stage IV (48.8% vs 65.7%) at initial diagnosis compared with RPTL patients who received bevacizumab (P = 0.001). Patients with RPTL who received cetuximab were more likely to have a documented history of adjuvant chemotherapy compared with patients with RPTL who received bevacizumab (47.6% vs 22.3%, P < 0.001). Patients with LPTL who received cetuximab were less likely to be tested for NRAS mutations (LPTL: 31.1% vs 41.4%, P = 0.020) and BRAF mutations (LPTL: 28.0% vs 46.1%, P < 0.001), compared with patients with LPTL who received bevacizumab. There was no significant difference between groups in NRAS status among those tested.
| LPTL1 | RPTL1 | |||||
| Cetuximab (n = 164) | Bevacizumab (n = 679) | P value | Cetuximab (n = 84) | Bevacizumab (n = 385) | P value | |
| Age at index date2, years | 0.727 | 0.801 | ||||
| Median | 61.0 | 61.0 | 66.5 | 67.0 | ||
| Sex, n (%) | 0.749 | 0.296 | ||||
| Female | 59 (36.0) | 256 (37.7) | 36 (42.9) | 192 (49.9) | ||
| Male | 105 (64.0) | 423 (62.3) | 48 (57.1) | 193 (50.1) | ||
| Race, n (%) | 0.042 | 0.506 | ||||
| Black or African American | 17 (10.4) | 61 (9.0) | 7 (8.3) | 43 (11.2) | ||
| White | 114 (69.5) | 435 (64.1) | 57 (67.9) | 264 (68.6) | ||
| Other race | 27 (16.5) | 109 (16.1) | 9 (10.7) | 46 (11.9) | ||
| Missing | 6 (3.7) | 74 (10.9) | 11 (13.1) | 32 (8.3) | ||
| Region, n (%) | 0.001 | 0.008 | ||||
| Northeast | 38 (23.2) | 144 (21.2) | 20 (23.8) | 73 (19.0) | ||
| Midwest | 14 (8.5) | 133 (19.6) | 12 (14.3) | 99 (25.7) | ||
| South | 54 (32.9) | 246 (36.2) | 24 (28.6) | 140 (36.4) | ||
| West | 40 (24.4) | 105 (15.5) | 15 (17.9) | 47 (12.2) | ||
| Unknown | 18 (11.0) | 51 (7.5) | 13 (15.5) | 26 (6.8) | ||
| Practice type, n (%) | 0.079 | 0.052 | ||||
| Academic | 2 (1.2) | 31 (4.6) | 0 | 17 (4.4) | ||
| Community | 162 (98.8) | 648 (95.4) | 84 (100) | 368 (95.6) | ||
| Site of disease, n (%) | 1.000 | NA | ||||
| Colon | 111 (67.7) | 460 (67.7) | 84 (100) | 385 (100) | ||
| Rectum | 53 (32.3) | 219 (32.3) | 0 | 0 | ||
| Side of colon, n (%) | 0.973 | 0.745 | ||||
| Left side | 86 (52.4) | 364 (53.6) | 0 | 0 | ||
| Rectosigmoid | 18 (11.0) | 79 (11.6) | 0 | 0 | ||
| Rectum | 52 (31.7) | 206 (30.3) | 0 | 0 | ||
| Splenic flexure | 8 (4.9) | 30 (4.4) | 0 | 0 | ||
| Right side | 0 | 0 | 70 (83.3) | 329 (85.5) | ||
| Transverse colon | 0 | 0 | 14 (16.7) | 56 (14.5) | ||
| Group stage at initial diagnosis, n (%) | 0.199 | 0.001 | ||||
| Stage I | 2 (1.2) | 26 (3.8) | 1 (1.2) | 5 (1.3) | ||
| Stage II | 13 (7.9) | 73 (10.8) | 5 (6.0) | 40 (10.4) | ||
| Stage III | 44 (26.8) | 145 (21.4) | 37 (44.0) | 87 (22.6) | ||
| Stage IV | 101 (61.6) | 411 (60.5) | 41 (48.8) | 253 (65.7) | ||
| Unknown | 4 (2.4) | 24 (3.5) | 0 | 0 | ||
| ECOG PS at index date2, 3, n (%) | 0.176 | 0.026 | ||||
| 0 | 39 (23.8) | 192 (28.3) | 27 (32.1) | 80 (20.8) | ||
| 1 | 22 (13.4) | 117 (17.2) | 9 (10.7) | 83 (21.6) | ||
| 2+ | 5 (3.0) | 29 (4.3) | 3 (3.6) | 26 (6.8) | ||
| Missing | 98 (59.8) | 341 (50.2) | 45 (53.6) | 196 (50.9) | ||
| Modified CCI at index date2, 4, n (%) | 0.526 | 0.339 | ||||
| 0 | 136 (82.9) | 557 (82.0) | 64 (76.2) | 293 (76.1) | ||
| 1 | 20 (12.2) | 86 (12.7) | 17 (20.2) | 59 (15.3) | ||
| 2 | 7 (4.3) | 21 (3.1) | 3 (3.6) | 24 (6.2) | ||
| 3+ | 1 (0.6) | 15 (2.2) | 0 | 9 (2.3) | ||
| NRAS tested, n (%) | 51 (31.1) | 281 (41.4) | 0.020 | 28 (33.3) | 160 (41.6) | 0.204 |
| NRAS status among those tested5, n (%) | 0.112 | 0.373 | ||||
| Mutation negative | 49 (96.1) | 256 (91.1) | 28 (100) | 144 (90.0) | ||
| Mutation positive | 0 | 19 (6.8) | 0 | 14 (8.8) | ||
| Results pending | 0 | 1 (0.4) | 0 | 1 (0.6) | ||
| Unknown | 1 (2.0) | 1 (0.4) | 0 | 0 | ||
| Unsuccessful/indeterminate | 1 (2.0) | 4 (1.4) | 0 | 1 (0.6) | ||
| BRAF tested, n (%) | 46 (28.0) | 313 (46.1) | < 0.001 | 35 (41.7) | 176 (45.7) | 0.579 |
| BRAF status among those tested5, n (%) | 0.075 | 0.072 | ||||
| Mutation negative | 45 (97.8) | 288 (92.0) | 24 (68.6) | 103 (58.5) | ||
| Mutation positive | 0 | 23 (7.3) | 10 (28.6) | 73 (41.5) | ||
| Results pending | 0 | 1 (0.3) | 0 | 0 | ||
| Unknown | 1 (2.2) | 1 (0.3) | 0 | 0 | ||
| Unsuccessful/indeterminate | 0 | 0 | 1 (2.9) | 0 | ||
| First-line chemotherapy backbone, n (%) | < 0.001 | < 0.001 | ||||
| FOLFIRI | 105 (64.0) | 165 (24.3) | 64 (76.2) | 96 (24.9) | ||
| FOLFOX | 59 (36.0) | 514 (75.7) | 20 (23.8) | 289 (75.1) | ||
| History of adjuvant chemotherapy6, n (%) | 0.171 | < 0.001 | ||||
| No/not documented | 114 (69.5) | 510 (75.1) | 44 (52.4) | 299 (77.7) | ||
| Yes | 50 (30.5) | 169 (24.9) | 40 (47.6) | 86 (22.3) | ||
| First-line therapy duration7, days | 0.076 | 0.969 | ||||
| Median | 197.0 | 183.0 | 156.0 | 162.0 | ||
| Length of follow-up8, days | 0.019 | 0.345 | ||||
| Median | 501.5 | 442.0 | 323.5 | 350.0 | ||
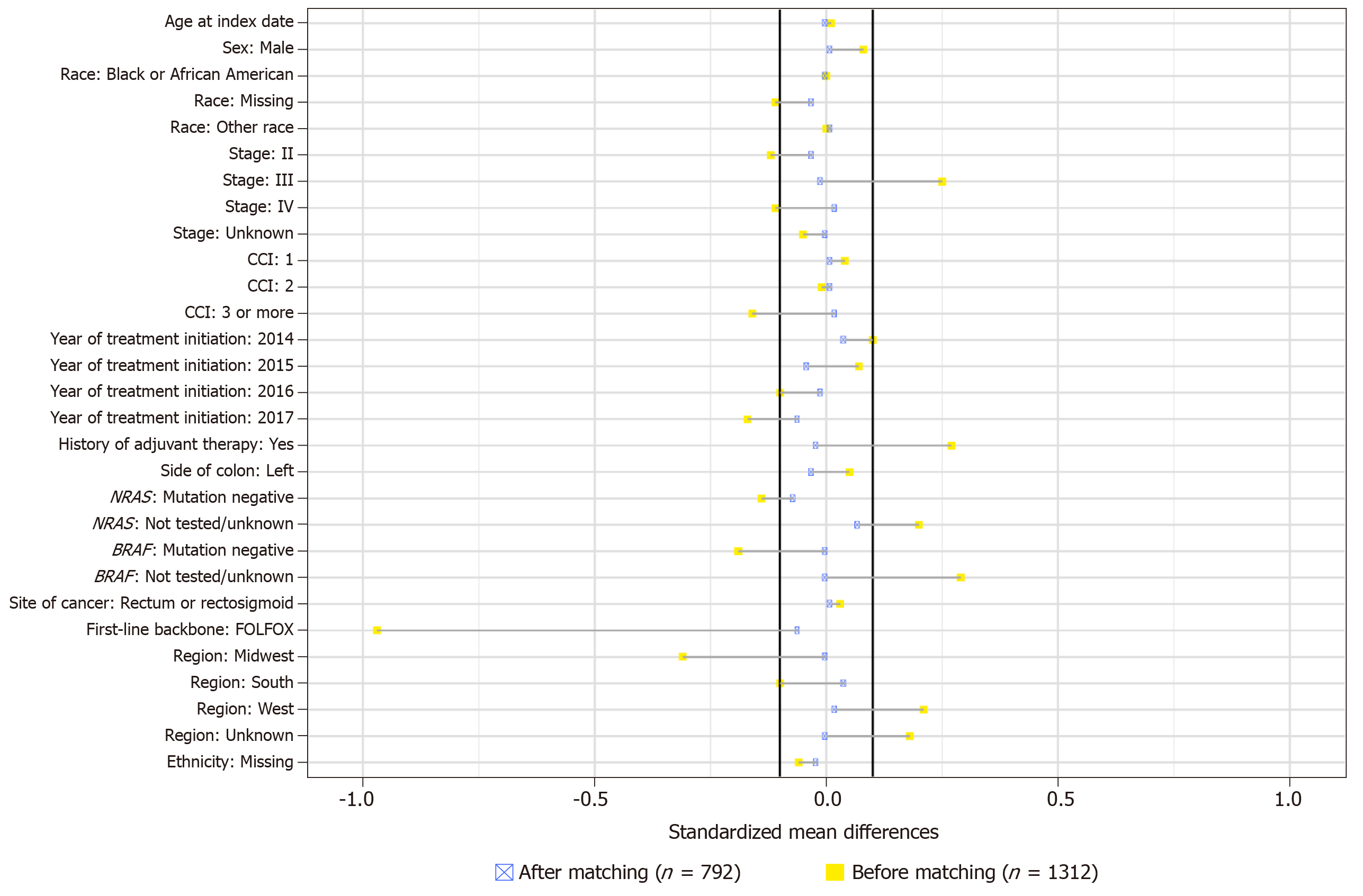
Table 2 shows the characteristics of patients in the cetuximab and bevacizumab cohorts after propensity score matching. With the exception of practice type, there were no significant differences across the observed covariates between the two cohorts after matching. Figure 2 shows the standardized mean differences across covariates between treatment cohorts before and after propensity score matching. The average absolute difference in standardized means, which assesses the overall covariate balance, was 0.15 before matching and 0.02 after matching, indicating an improvement in the overall balance across the observed covariates after matching. After propensity score matching, the overall sample size decreased to 792 patients; 228 patients who received first-line cetuximab plus FOLFIRI or FOLFOX (147 with LPTL and 81 with RPTL), and 564 patients who received first-line bevacizumab plus FOLFIRI or FOLFOX (372 with LPTL and 192 with RPTL).
| Total (n = 792) | Cetuximab (n = 228) | Bevacizumab (n = 564) | P value | |
| Age at index date1, years | 0.923 | |||
| Median | 64.0 | 64.0 | 63.0 | |
| Sex, n (%) | 0.914 | |||
| Female | 334 (42.2) | 92 (40.4) | 242 (42.9) | |
| Male | 458 (57.8) | 136 (59.6) | 322 (57.1) | |
| Race, n (%) | 0.905 | |||
| Black or African American | 71 (9.0) | 22 (9.6) | 49 (8.7) | |
| White | 549 (69.3) | 158 (69.3) | 391 (69.3) | |
| Other race | 111 (14.0) | 32 (14.0) | 79 (14.0) | |
| Missing | 61 (7.7) | 16 (7.0) | 45 (8.0) | |
| Region, n (%) | 0.620 | |||
| Northeast | 185 (23.4) | 54 (23.7) | 131 (23.2) | |
| Midwest | 113 (14.3) | 26 (11.4) | 87 (15.4) | |
| South | 253 (31.9) | 75 (32.9) | 178 (31.6) | |
| West | 158 (19.9) | 48 (21.1) | 110 (19.5) | |
| Unknown | 83 (10.5) | 25 (11.0) | 58 (10.3) | |
| Practice type, n (%) | <0.001 | |||
| Academic | 35 (4.4) | 0 | 35 (6.2) | |
| Community | 757 (95.6) | 228 (100) | 529 (93.8) | |
| Site of disease, n (%) | 1.000 | |||
| Colon | 630 (79.5) | 180 (78.9) | 450 (79.8) | |
| Rectum | 162 (20.5) | 48 (21.1) | 114 (20.2) | |
| Group stage at initial diagnosis, n (%) | 0.763 | |||
| Stage I | 9 (1.1) | 3 (1.3) | 6 (1.1) | |
| Stage II | 68 (8.6) | 18 (7.9) | 50 (8.9) | |
| Stage III | 245 (30.9) | 79 (34.6) | 166 (29.4) | |
| Stage IV | 458 (57.8) | 124 (54.4) | 334 (59.2) | |
| Unknown | 12 (1.5) | 4 (1.8) | 8 (1.4) | |
| ECOG PS at index date1, 2, n (%) | 0.379 | |||
| 0 | 197 (24.9) | 61 (26.8) | 136 (24.1) | |
| 1 | 130 (16.4) | 30 (13.2) | 100 (17.7) | |
| 2+ | 35 (4.4) | 6 (2.6) | 29 (5.1) | |
| Missing | 430 (54.3) | 131 (57.5) | 299 (53.0) | |
| Modified CCI at index date1, 3, n (%) | 0.861 | |||
| 0 | 650 (82.1) | 185 (81.1) | 465 (82.4) | |
| 1 | 104 (13.1) | 32 (14.0) | 72 (12.8) | |
| 2 | 34 (4.3) | 10 (4.4) | 24 (4.3) | |
| 3+ | 4 (0.5) | 1 (0.4) | 3 (0.5) | |
| NRAS tested, n (%) | 274 (34.6) | 70 (30.7) | 204 (36.2) | 0.410 |
| NRAS status among those tested4, n (%) | 0.908 | |||
| Mutation negative | 268 (97.8) | 68 (97.1) | 200 (98.0) | |
| Mutation positive | 0 | 0 | 0 | |
| Results pending | 1 (0.4) | 0 | 1 (0.5) | |
| Unknown | 1 (0.4) | 1 (1.4) | 0 | |
| Unsuccessful/indeterminate | 4 (1.5) | 1 (1.4) | 3 (1.5) | |
| BRAF tested, n (%) | 290 (36.6) | 76 (33.3) | 214 (37.9) | 0.955 |
| BRAF status among those tested4, n (%) | 0.881 | |||
| Mutation negative | 248 (85.5) | 64 (84.2) | 184 (86.0) | |
| Mutation positive | 39 (13.4) | 10 (13.2) | 29 (13.6) | |
| Results pending | 1 (0.3) | 0 | 1 (0.5) | |
| Unknown | 1 (0.3) | 1 (1.3) | 0 | |
| Unsuccessful/indeterminate | 1 (0.3) | 1 (1.3) | 0 | |
| First-line chemotherapy backbone, n (%) | 0.485 | |||
| FOLFIRI | 387 (48.9) | 149 (65.4) | 238 (42.2) | |
| FOLFOX | 405 (51.1) | 79 (34.6) | 326 (57.8) | |
| History of adjuvant chemotherapy5, n (%) | 0.789 | |||
| No/not documented | 519 (65.5) | 140 (61.4) | 379 (67.2) | |
| Yes | 273 (34.5) | 88 (38.6) | 185 (32.8) | |
| First-line therapy duration6, days | 0.424 | |||
| Median | 179.0 | 162.0 | 190.0 | |
| Length of follow-up7, days | 0.533 | |||
| Median | 434.0 | 428.5 | 434.5 | |
| Side of colon, n (%) | 0.868 | |||
| Left side | 283 (35.7) | 78 (34.2) | 205 (36.3) | |
| Rectosigmoid | 62 (7.8) | 17 (7.5) | 45 (8.0) | |
| Rectum | 154 (19.4) | 47 (20.6) | 107 (19.0) | |
| Splenic flexure | 19 (2.4) | 5 (2.2) | 14 (2.5) | |
| Right side | 231 (29.2) | 68 (29.8) | 163 (28.9) | |
| Transverse colon | 43 (5.4) | 13 (5.7) | 30 (5.3) |
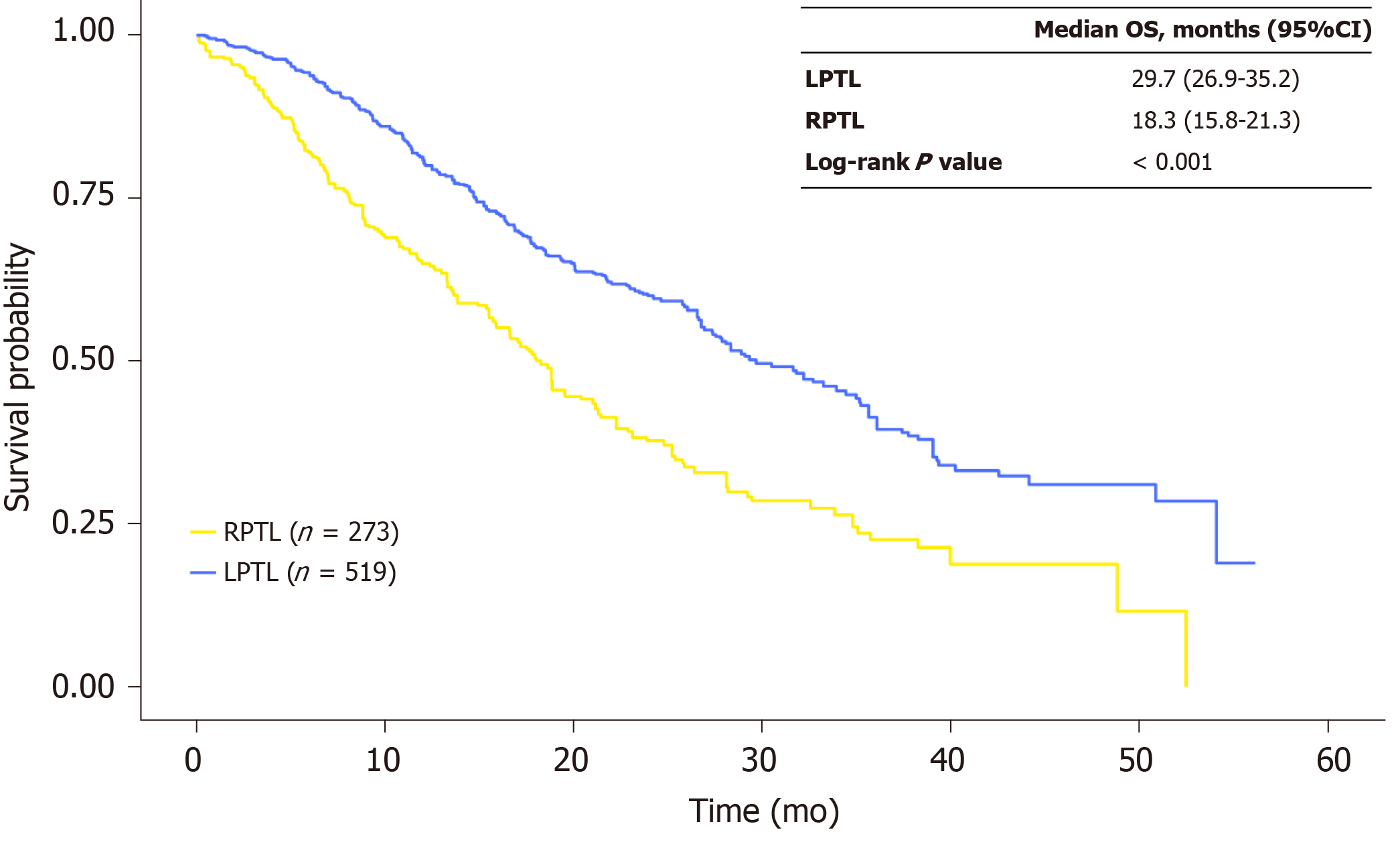
In the propensity score-matched sample, median OS was 29.7 mo (95%CI: 26.9-35.2) for patients with LPTL and 18.3 mo (95%CI: 15.8-21.3) for patients with RPTL (P < 0.001), indicating that there was a statistically significant difference in OS between patients with LPTL vs RPTL (Figure 3). Among the cetuximab cohort, the HR for patients with LPTL vs RPTL was 0.48 (95%CI: 0.32-0.74; P < 0.001), and among the bevacizumab cohort the HR for LPTL vs RPTL was 0.56 (95%CI: 0.42-0.75; P < 0.001).
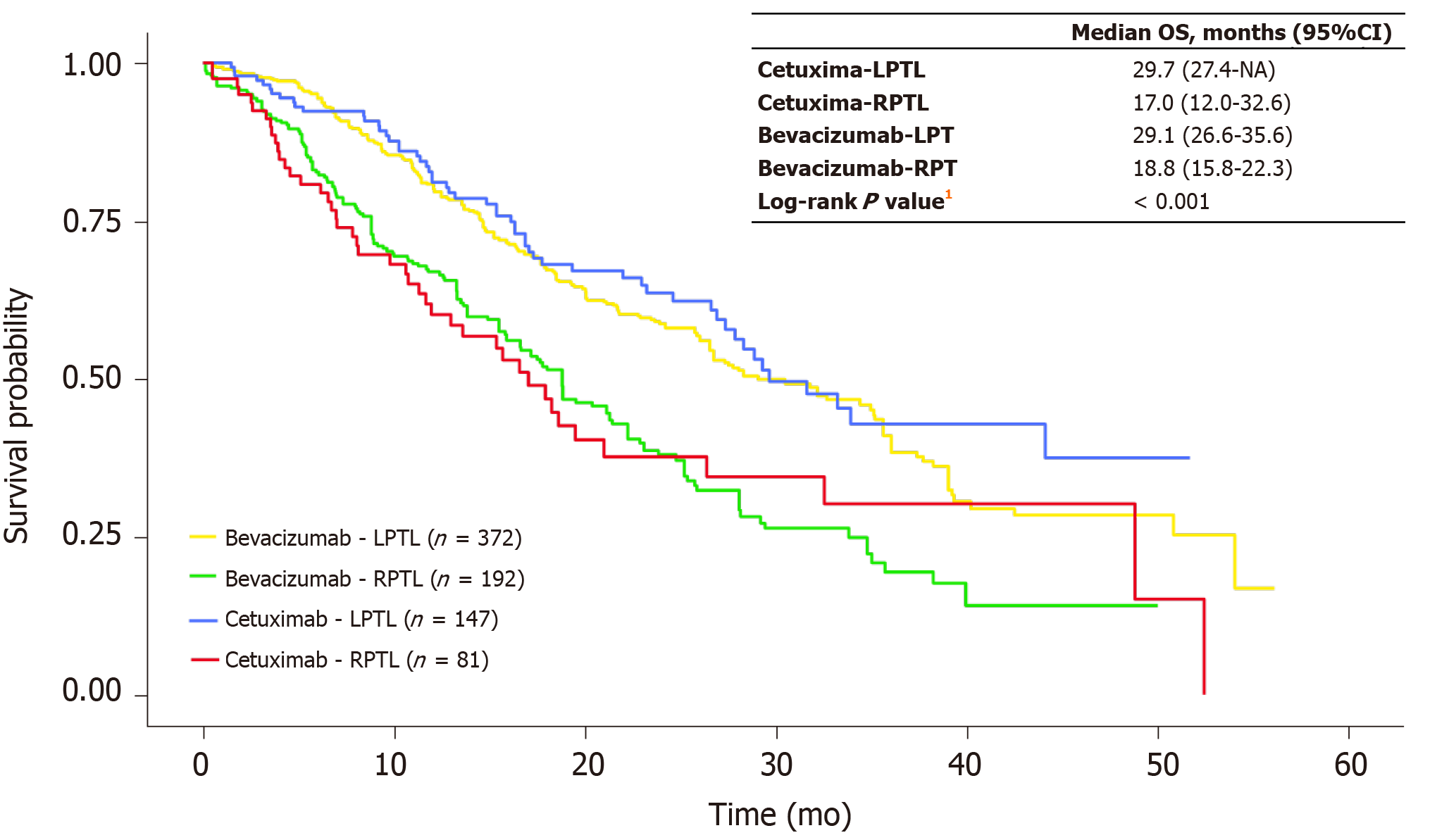
In the propensity score-matched sample, median OS was 29.7 mo (95%CI: 27.4-NA) for patients with LPTL who received cetuximab and 29.1 mo (95%CI: 26.6-35.6) for patients with LPTL who received bevacizumab (Figure 4). Median OS was 17.0 mo (95%CI: 12.0-32.6) for patients with RPTL who received cetuximab and 18.8 mo (95%CI: 15.8-22.3) for patients with RPTL who received bevacizumab (Figure 4). The Cox proportional hazards model to test for differences in OS by primary tumor location and treatment after matching showed no significant difference in OS; the interaction term between primary tumor location and treatment was 0.87 (P = 0.566) (Table 3). The HR for cetuximab vs bevacizumab for patients with RPTL was 1.00 (95%CI: 0.68-1.46; P = 0.996) and the HR for cetuximab vs bevacizumab with LPTL was 0.87 (95%CI: 0.63-1.19; P = 0.378).
| Log (HR) | HR | SE [Log (HR)] | Robust SE [Log (HR)] | Z | P value | |
| Cetuximab | 0 | 1.00 | 0.18 | 0.19 | 0 | 0.996 |
| LPTL | -0.58 | 0.56 | 0.13 | 0.15 | -3.89 | < 0.001 |
| Cetuximab × LPTL | -0.14 | 0.87 | 0.24 | 0.25 | -0.57 | 0.566 |
Sensitivity analyses using different methodologic approaches to account for potential imbalance in the observed confounders confirmed the main OS analysis findings in terms of magnitude, significance, and directionality (Table 4). After IPTW among patients who were NRAS WT (n = 149), median OS was 28.9 mo for patients who received cetuximab and 26.0 mo for patients who received bevacizumab; the HR for cetuximab vs bevacizumab was 0.77 (95%CI: 0.40-1.50) for patients with LPTL, and 1.03 (95%CI: 0.54-1.97) for patients with RPTL. Among patients who received a backbone of FOLFIRI (n = 336), median OS was 24.6 mo for those who received cetuximab and 23.1 mo for those who received bevacizumab after IPTW; the HR for cetuximab vs bevacizumab was 0.96 (95%CI: 0.64-1.44) for patients with LPTL, and 1.05 (95%CI: 0.62-1.77) for patients with RPTL. Among patients who received a backbone of FOLFOX (n = 158), median OS was not reached for those who received cetuximab and 25.9 mo for those who received bevacizumab after IPTW; the HR for cetuximab vs bevacizumab was 0.63 (95%CI: 0.37-1.08) for patients with LPTL and 0.52 (95%CI: 0.23-1.17) for patients with RPTL.
| Matched/weighted | HR (95%CI) of cetuximab vs bevacizumab, for LPTL | HR (95%CI) of cetuximab vs bevacizumab, for RPTL | |
| mOS (mo) for cetuximab vs bevacizumab | |||
| Main analysis with propensity score matching | 27.9 vs 25.4 | 0.87 (0.63-1.19) | 1.00 (0.68-1.46) |
| Planned sensitivity analyses | |||
| 1:1 matching without a caliper (propensity score matching) | 27.9 vs 21.7 | 0.76 (0.55-1.06) | 0.91 (0.59-1.41) |
| 2:1 matching without a caliper (propensity score matching) | 27.9 vs 22.3 | 0.82 (0.61-1.11) | 0.87 (0.58-1.29) |
| IPTW | 27.9 vs 25.6 | 0.87 (0.63-1.19) | 0.98 (0.65-1.49) |
| LPTL only (propensity score matching) | 29.4 vs 30.5 | 0.88 (0.61-1.28) | NA |
| RPTL only (propensity score matching) | 17.9 vs 20.4 | NA | 1.09 (0.74-1.63) |
| Change definition of tumor location (IPTW) | |||
| RPTL: C/A/HF; LPTL: transverse to rectum | 27.9 vs 25.6 | 0.89 (0.66-1.20) | 0.96 (0.61-1.53) |
| RPTL: C/A/HF to transverse; LPTL: splenic flexure to rectosigmoid | 27.9 vs 26.6 | 0.98 (0.66-1.44) | 0.98 (0.64-1.50) |
| RPTL: C/A/HF to transverse; LPTL: splenic flexure to descending/sigmoid | 27.4 vs 25.8 | 0.93 (0.61-1.43) | 0.98 (0.65-1.48) |
| RPTL: C/A/HF; LPTL: transverse to rectosigmoid | 27.9 vs 26.6 | 1.02 (0.71-1.46) | 0.95 (0.60-1.52) |
| RPTL: C/A/HF; LPTL: transverse to descending/sigmoid | 27.4 vs 25.8 | 0.98 (0.67-1.45) | 0.95 (0.60-1.50) |
| RPTL: C/A/HF; LPTL: splenic flexure to rectum | 28.3 vs 25.8 | 0.88 (0.64-1.21) | 0.96 (0.60-1.51) |
| RPTL: C/A/HF; LPTL: splenic flexure to rectosigmoid | 28.3 vs 26.6 | 1.00 (0.68-1.47) | 0.93 (0.59-1.48) |
| RPTL: C/A/HF; LPTL: splenic flexure to descending/sigmoid | 28.3 vs 26.0 | 0.95 (0.62-1.46) | 0.94 (0.60-1.47) |
| NRAS mutation–negative patients only (IPTW) | 28.9 vs 26.0 | 0.77 (0.40-1.50) | 1.03 (0.54-1.97) |
| Restricted to patients with chemotherapy backbone of FOLFIRI (IPTW) | 24.6 vs 23.1 | 0.96 (0.64-1.44) | 1.05 (0.62-1.77) |
| Restricted to patients with chemotherapy backbone of FOLFOX (IPTW) | Not reached vs 25.91 | 0.63 (0.37-1.08) | 0.52 (0.23-1.17) |
| Change definition of index date (propensity score matching)2 | 27.8 vs 24.8 | 0.86 (0.61-1.20) | 0.96 (0.64-1.44) |
| Restrict to stage IV patients (IPTW) | 29.7 vs 29.4 | 0.98 (0.61-1.57) | 0.99 (0.51-1.90) |
In this retrospective cohort study of real-world patients from clinical practice in the United States, median OS was significantly longer for mCRC KRAS WT patients with LPTL than for those with RPTL, regardless of first-line treatment, substantiating the prognostic effect of primary tumor location. The prognostic role of primary tumor location has been demonstrated in other studies[17-20]. A more favorable prognosis for LPTL was demonstrated in a retrospective pooled analysis of mCRC randomized controlled studies of first-line chemotherapy plus bevacizumab (PROVETTA, AVF2107, and NO16966)[21] and of six studies of chemotherapy plus anti-EGFR therapies (first-line: CALGB 80405, FIRE-3, and CRYSTAL; second-line: PEAK, PRIME, and 20050181)[22]. An updated meta-analysis that included the Chinese phase 3 TAILOR study showed that cetuximab or panitumumab plus FOLFOX significantly benefited PFS and ORR in patients with RAS WT LPTL mCRC[23]. Furthermore, a meta-analysis of 66 mCRC clinical studies conducted over several decades to evaluate different treatments demonstrated that LPTL was associated with improved prognosis compared with RPTL[8]. An analysis of the Surveillance, Epidemiology and End Results program confirmed the prognostic effect of primary tumor location[24]. These studies vary in their design for selection of patients and treatment plan and some lack data about stage at diagnosis.
Primary tumor location was not predictive of treatment effect for cetuximab compared with bevacizumab in this study. There was no significant difference in median OS between patients who received cetuximab and those who received bevacizumab by primary tumor location. A number of sensitivity analyses to test the robustness of the analytic approach, as well as additional subgroup analyses, confirmed the results obtained in the main analysis in terms of magnitude, significance, and directionality. However, subgroup analyses by chemotherapy backbone showed a significant treatment benefit for cetuximab compared with bevacizumab, regardless of primary tumor location, in patients who received FOLFOX as the chemotherapy backbone. Among these patients, median OS was not reached in the cetuximab group vs 25.9 mo in the bevacizumab group. The analyses (IPTW) by primary tumor location showed an HR of 0.63 (95%CI: 0.37-1.08) in patients with LPTL and 0.52 (95%CI: 0.23-1.17) in patients with RPTL, favoring cetuximab in both LPTL and RPTL patients who received FOLFOX. In a subgroup of patients who received a backbone of FOLFIRI, a treatment benefit for cetuximab compared with bevacizumab was not observed. Among these patients, median OS was 24.6 mo in the cetuximab group vs 23.1 mo in the bevacizumab group, with an HR of 0.96 (95%CI: 0.64-1.44) in patients with LPTL and 1.05 (95%CI: 0.62-1.77) in patients with RPTL.
The choice of 5-fluorouracil-based chemotherapy backbone for the treatment of metastatic disease depends on, among other factors, prior adjuvant chemotherapy use and response, and adjuvant therapy regimen choice for earlier stage disease. In this study, patients who received FOLFIRI (n = 430) as the chemotherapy backbone in the metastatic setting more often had a group stage of III at initial diagnosis (55.1% for FOLFIRI vs 8.6% for FOLFOX), whereas patients who received FOLFOX (n = 882) more often had a group stage of IV at initial diagnosis (30.0% for FOLFIRI vs 76.8% for FOLFOX) (P < 0.001) (data not shown). This translated into a greater proportion of FOLFIRI patients having a documented history of adjuvant chemotherapy compared with patients who received FOLFOX (64.0% for FOLFIRI vs 7.9% for FOLFOX, P < 0.001).
The lack of evidence of predictive effect of primary tumor location in this real-world cohort contrasts with post hoc analyses of the CALGB/SWOG 80405 trial, which closely mirrors the current study, and other studies (a meta-analysis of FIRE-3, CRYSTAL, PRIME, CALGB/SWOG 80405, and other studies as well as a population-based cohort study)[11,17,18]. We explored differences in patient characteristics and treatment-related variables between this study and CALGB/SWOG 80405 to elucidate the divergent findings of our analysis. One of the key differences between the two studies is that 32% of cetuximab patients in the current study received FOLFOX whereas 74% of cetuximab patients received FOLFOX in the CALGB/SWOG 80405 study[25]. Although the chemotherapy backbone data by biologic type are not published for the CALGB/SWOG 80405 study patients included in post hoc primary tumor location analyses[11,22], it is likely that the proportion of cetuximab patients receiving FOLFOX was also higher than in the current study.
In the current study, a smaller proportion of patients who received cetuximab compared with bevacizumab were stage IV at initial diagnosis (57.3% vs 62.4%), and a greater proportion were stage III at initial diagnosis (32.7% vs 21.8%) (P = 0.003). This difference in stage distribution between the cetuximab and bevacizumab groups was primarily observed in patients with RPTL. In contrast, the proportion of patients with stage IV disease at initial diagnosis was almost the same for the cetuximab (77.3%) and bevacizumab (79.6%) groups in the CALGB/SWOG 80405 study, although the stage distribution by biologic type was not reported in primary tumor location analyses[11,22]. A greater proportion of cetuximab vs bevacizumab patients in the current study had a documented history of adjuvant therapy (36.3% vs 24.0%, P < 0.001), whereas the proportion of patients who had a documented history of adjuvant therapy was similar for the cetuximab vs bevacizumab cohorts in the CALGB/SWOG 80405 study (13.7% vs 14.5%)[11]. Overall, these findings suggest that the chemotherapy backbone, among other factors, may contribute to outcomes, either alone, by interacting with the biologic agent, or as a proxy for disease biology if the backbone choice is driven by clinical history: Stage at initial diagnosis and features of prior adjuvant chemotherapy (use, regimen choice, disease response, and the time since completion of adjuvant therapy).
Classification of colorectal tumors as right- and left-sided is considered a surrogate for biological differences associated with embryologic differences by location in the large intestine. However, more granular information about specific tumor location (e.g. ascending colon, transverse colon, or descending colon) may add more nuance about the underlying biology, particularly for the transverse colon, for which there is no anatomical divide between the first portion, which is associated with RPTL embryonal biology, and the latter portion, which is associated with LPTL embryonal biology[26]. The sensitivity analysis in this study defining RPTL vs LPTL using different granular tumor location groupings (e.g. transverse colon considered RPTL vs LPTL) did not change outcomes (Table 4).
Based on post hoc analyses of clinical trials, such as CALGB/SWOG 80405, FIRE-3, CRYSTAL, PEAK, PRIME and others, the National Comprehensive Cancer Network has recommended that only patients with LPTL should be offered cetuximab or panitumumab in combination with 5-fluorouracil-based chemotherapy as first-line treatment for mCRC[14]. However, the findings from this real-world cohort found no significant difference in survival benefit between cetuximab and bevacizumab by primary tumor location. The difference in these results compared with published post hoc analyses of randomized clinical trials highlights potential limitations of post hoc analyses and points to differences between clinical trials and the real-world study population that may warrant further research.
In conclusion, the analysis of this real-world cohort of mCRC KRAS WT patients who received first-line treatment found a prognostic effect by primary tumor location, but not a predictive effect for survival by biologic agent given with 5-fluoroucil-based chemotherapy. These findings contribute to the growing body of literature describing the potential impact of chemotherapy backbone on survival benefit associated with biologic therapy for patients with mCRC. Future research is needed to better understand if biologic treatment recommendations by side of colon should incorporate the potential impact of chemotherapy backbone, expanded RAS and BRAF mutations, and history of adjuvant chemotherapy. Furthermore, additional studies are required to elucidate tumor, patient, and treatment factors that contributed to these real-world findings, as well as differences between real-world and clinical trial populations that may have contributed to the divergent results.
The limitations of this real-world study include those common in retrospective observational studies based on EHR data, such as selection biases and unobserved confounders, which may impact treatment effect estimates. For example, ECOG PS was missing for over 50% of patients in this study. It is not known if the beneficial effect of a therapy is lost if the regimen is used for a patient with an ECOG PS of 2 or 3 compared with an ECOG PS of 0 or 1. This loss of efficacy may be more pronounced with the addition of a biologic therapy that can significantly add to the toxicity of the chemotherapy backbone. Furthermore, in this study, approximately 60% of patients were untested for NRAS mutations and 57% of patients were untested for the BRAF mutation. If BRAF or NRAS mutations were present in these patients, they may have impacted the study results and explained, in part, why the predictive effect of primary tumor location on treatment with cetuximab vs bevacizumab in combination with 5-fluorouracil-based chemotherapy was not observed. The study may also not be generalizable to other patient populations. A further limitation was missing data, since data availability was limited to what was documented in the EHR; for example, if patients moved from or to the oncology practices represented within this EHR database, there may have been periods of missing data when care was received elsewhere. Patients with greater than a 90-d gap between advanced diagnosis and structured activity were excluded to mitigate the possibility of including data from patients who received some of their initial care outside of the Flatiron network. The relatively short follow-up time may have impacted findings due to the number of events for evaluation, consequently leading to insufficient study power; that is, there were 366 events observed over the follow-up period in the 792 patients from the matched analysis; the median length of follow-up time available was 434 d (data not shown). Furthermore, some potential confounders for propensity score-based estimation procedures may not have been observed.
Metastatic colorectal cancer (mCRC) is a heterogeneous disease with differing outcomes and clinical responses, in part due to differences in chromosomal and molecular profiles between primary tumors that arise from the left (distal) and right (proximal) sides of the colon. Primary tumor location has been shown to be a prognostic factor, with left-sided primary tumor location (LPTL) demonstrating significantly longer survival than right-sided primary tumor location (RPTL). Additionally, primary tumor location may be a predictive factor of survival outcomes associated with cetuximab or bevacizumab in combination with 5-fluorouracil-based chemotherapy. Current first-line treatment recommendations for mCRC per the National Comprehensive Cancer Network are cetuximab or panitumumab only for patients with LPTL RAS wild-type (WT) disease or bevacizumab for patients with RPTL RAS WT disease; second-line treatment recommendations for subsequent lines are cetuximab or panitumumab for all patients with RAS WT tumors. However, most of the studies that investigated the effect of primary tumor location on biologic therapy efficacy and that led to treatment recommendations were post hoc analyses of large randomized controlled trials (such as CALGB/SWOG 80405, FIRE-3, CRYSTAL, PEAK, PRIME and others) not designed to examine tumor sidedness, or were single institution analyses of small cohorts. Consequently, there is a need for real-world evidence from large mCRC populations describing the association of primary tumor location with survival outcomes from biologic therapy, which is the aim of the current study.
This study was conducted to evaluate the prognostic and/or predictive roles of primary tumor location in real-world mCRC patients treated with cetuximab or bevacizumab plus 5-fluorouracil-based chemotherapy. The findings of this study are important because they contribute to the growing body of literature describing the potential impact of primary tumor location on survival benefit associated with biologic therapy for patients with mCRC.
The main objectives of this study were to evaluate the prognostic and predictive role of primary tumor location and its association with survival benefit in real-world patients with KRAS WT mCRC who initiated first-line therapy with cetuximab plus 5-fluorouracil/leucovorin/irinotecan (FOLFIRI) or 5-fluorouracil/leucovorin/oxaliplatin (FOLFOX) vs with bevacizumab plus FOLFIRI or FOLFOX in the United States. The analysis of this real-world cohort of mCRC KRAS WT patients who received first-line treatment found a prognostic effect by primary tumor location, but not a predictive effect for survival by biologic agent given with 5-fluoroucil-based chemotherapy. The difference in these real-world results regarding predictive findings compared with published post hoc analyses of randomized clinical trials highlights challenges with the generalizability of clinical trial findings and the need for further research to elucidate tumor, patient, and treatment factors that contributed to these real-world findings, as well as differences between real-world and clinical trial populations that may have contributed to the divergent results.
This retrospective cohort study selected patients with KRAS wild-type mCRC who initiated first-line therapy with cetuximab or bevacizumab in combination with FOLFIRI or FOLFOX between January 2013 and April 2017 from the Flatiron Health electronic health record derived database of de-identified patient-level data in the United States. Primary tumor location was abstracted from patients’ charts. LPTL was defined as tumors that originated in the splenic flexure, descending colon, sigmoid colon, or rectum; RPTL was defined as tumors that originated from the appendix, cecum, ascending colon, hepatic flexure, or transverse colon. Propensity score matching was used to balance the baseline demographic and clinical characteristics between patients treated with cetuximab and patients treated with bevacizumab. Kaplan-Meier and Cox regression methods were used for survival analyses.
In this retrospective cohort study of real-world patients from clinical practice in the United States, median OS was significantly longer for mCRC KRAS WT patients with LPTL than for those with RPTL, regardless of first-line treatment, substantiating the prognostic effect of primary tumor location reported in previous studies. Primary tumor location was not predictive of treatment effect for cetuximab compared with bevacizumab in this study; there was no significant difference in median OS between patients who received cetuximab and those who received bevacizumab by primary tumor location. However, subgroup analyses by chemotherapy backbone showed a significant treatment benefit for cetuximab compared with bevacizumab, regardless of primary tumor location, in patients who received FOLFOX as the chemotherapy backbone. Factors that may have affected treatment-related findings include that cetuximab patients were more likely to receive FOLFIRI vs bevacizumab patients; cetuximab RPTL patients were more likely to have stage III disease while bevacizumab RPTL patients were more likely to have stage IV disease; and cetuximab RPTL patients were more likely to have a documented history of adjuvant chemotherapy vs bevacizumab RPTL patients. In addition, mutations in NRAS and KRAS exons 3 and 4 may have impacted the study results, yet approximately 70% of patients were not evaluated for expanded RAS mutations in this study. Future research should examine these treatment factors further.
Although the analysis of this real-world cohort of mCRC KRAS WT patients who received first-line treatment found a prognostic effect by primary tumor location, it did not confirm a predictive effect for survival by biologic agent given with 5-fluoroucil-based chemotherapy as expected from previous post hoc analyses of clinical trials and treatment guidelines. Possible reasons for this divergence from previously reported findings, current guidelines, and current practice regarding treatment recommendations for mCRC by primary tumor location may include limitations of post hoc analyses; the potential impact of chemotherapy backbone on survival benefit associated with biologic therapy; tumor, patient, and treatment factors that contributed to these real-world findings; and differences between real-world and clinical trial populations. Future research is needed to definitively confirm these reasons in order to optimize treatment for patients with mCRC.
These findings confirmed primary tumor location as a prognostic factor in mCRC but did not confirm its predictive effect in contrast with previous findings. Chemotherapy backbone may contribute to outcomes, either alone, by interacting with the biologic agent, or as a proxy for disease biology if the backbone choice is driven by clinical history: Stage at initial diagnosis and features of prior adjuvant chemotherapy (use, regimen choice, disease response, and the time since completion of adjuvant therapy). Future research is needed to better understand if biologic treatment recommendations by side of colon should incorporate the potential impact of chemotherapy backbone and other factors, such as expanded RAS and BRAF mutations, and history of adjuvant chemotherapy. Furthermore, additional studies are required to elucidate tumor, patient, and treatment factors that contributed to these real-world findings, as well as differences between real-world and clinical trial populations.
This study was sponsored by Eli Lilly and Company. Medical writing support was provided by Andrew Sakko, PhD, CMPP, and editorial support was provided by Noelle Gasco of Syneos Health and funded by Eli Lilly and Company in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mulder KE, Sunakawa Y S-Editor: Wang YQ L-Editor: A E-Editor: Wu YXJ
| 1. | Stintzing S, Tejpar S, Gibbs P, Thiebach L, Lenz HJ. Understanding the role of primary tumour localisation in colorectal cancer treatment and outcomes. Eur J Cancer. 2017;84:69-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 184] [Cited by in RCA: 211] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 2. | Sadler TW. Langman’s medical embryology. Philadelphia: Lippincott Williams & Wilkins 2011; 222-231. |
| 3. | Missiaglia E, Jacobs B, D'Ario G, Di Narzo AF, Soneson C, Budinska E, Popovici V, Vecchione L, Gerster S, Yan P, Roth AD, Klingbiel D, Bosman FT, Delorenzi M, Tejpar S. Distal and proximal colon cancers differ in terms of molecular, pathological, and clinical features. Ann Oncol. 2014;25:1995-2001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 494] [Article Influence: 44.9] [Reference Citation Analysis (0)] |
| 4. | Yamauchi M, Morikawa T, Kuchiba A, Imamura Y, Qian ZR, Nishihara R, Liao X, Waldron L, Hoshida Y, Huttenhower C, Chan AT, Giovannucci E, Fuchs C, Ogino S. Assessment of colorectal cancer molecular features along bowel subsites challenges the conception of distinct dichotomy of proximal versus distal colorectum. Gut. 2012;61:847-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 493] [Article Influence: 37.9] [Reference Citation Analysis (0)] |
| 5. | Mouradov D, Sloggett C, Jorissen RN, Love CG, Li S, Burgess AW, Arango D, Strausberg RL, Buchanan D, Wormald S, O'Connor L, Wilding JL, Bicknell D, Tomlinson IP, Bodmer WF, Mariadason JM, Sieber OM. Colorectal cancer cell lines are representative models of the main molecular subtypes of primary cancer. Cancer Res. 2014;74:3238-3247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 294] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 6. | Baran B, Mert Ozupek N, Yerli Tetik N, Acar E, Bekcioglu O, Baskin Y. Difference between left-sided and right-sided colorectal cancer: a focused review of literature. Gastroenterology Res. 2018;11:264-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 339] [Article Influence: 48.4] [Reference Citation Analysis (1)] |
| 7. | Jess P, Hansen IO, Gamborg M, Jess T; Danish Colorectal Cancer Group. A nationwide Danish cohort study challenging the categorisation into right-sided and left-sided colon cancer. BMJ Open. 2013;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 8. | Petrelli F, Tomasello G, Borgonovo K, Ghidini M, Turati L, Dallera P, Passalacqua R, Sgroi G, Barni S. Prognostic survival associated with left-sided vs right-sided colon cancer: a systematic review and meta-analysis. JAMA Oncol. 2017;3:211-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 538] [Article Influence: 67.3] [Reference Citation Analysis (0)] |
| 9. | Maus MK, Hanna DL, Stephens CL, Astrow SH, Yang D, Grimminger PP, Loupakis F, Hsiang JH, Zeger G, Wakatsuki T, Barzi A, Lenz HJ. Distinct gene expression profiles of proximal and distal colorectal cancer: implications for cytotoxic and targeted therapy. Pharmacogenomics J. 2015;15:354-362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Tejpar S, Stintzing S, Ciardiello F, Tabernero J, Van Cutsem E, Beier F, Esser R, Lenz HJ, Heinemann V. Prognostic and predictive relevance of primary tumor location in patients with RAS wild-type metastatic colorectal cancer: retrospective analyses of the CRYSTAL and FIRE-3 Trials. JAMA Oncol. 2017;3:194-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 441] [Cited by in RCA: 528] [Article Influence: 66.0] [Reference Citation Analysis (0)] |
| 11. | Venook AP, Niedzwiecki D, Innocenti F, Fruth B, Greene C, O'Neil BH, Shaw JE, Atkins JN, Horvath LE, Polite BN, Meyerhardt JA, O'Reilly EM, Goldberg RM, Hochster HS, Blanke CD, Richard L. Schilsky RL, Mayer RJ, Bertagnolli MM, Lenz HJ. Impact of primary (1o) tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol. 2016;34 Suppl:abstr 3504. [RCA] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 209] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 12. | Modest DP, Stintzing S, von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran SE, Heintges T, Kahl C, Seipelt G, Kullmann F, Scheithauer W, Moehler M, Holch JW, von Einem JC, Held S, Heinemann V. Exploring the effect of primary tumor sidedness on therapeutic efficacy across treatment lines in patients with metastatic colorectal cancer: analysis of FIRE-3 (AIOKRK0306). Oncotarget. 2017;8:105749-105760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Brulé SY, Jonker DJ, Karapetis CS, O'Callaghan CJ, Moore MJ, Wong R, Tebbutt NC, Underhill C, Yip D, Zalcberg JR, Tu D, Goodwin RA. Location of colon cancer (right-sided versus left-sided) as a prognostic factor and a predictor of benefit from cetuximab in NCIC CO.17. Eur J Cancer. 2015;51:1405-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 254] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 14. | Benson AB, Venook AP, Cederquist L, Chan E, Chen YJ, Cooper HS, Deming D, Engstrom PF, Enzinger PC, Fichera A, Grem JL, Grothey A, Hochster HS, Hoffe S, Hunt S, Kamel A, Kirilcuk N, Krishnamurthi S, Messersmith WA, Mulcahy MF, Murphy JD, Nurkin S, Saltz L, Sharma S, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Wu CS, Gregory KM, Freedman-Cass D. Colon Cancer, Version 1.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2017;15:370-398. [PubMed] |
| 15. | Curtis MD, Griffith SD, Tucker M, Taylor MD, Capra WB, Carrigan G, Holzman B, Torres AZ, You P, Arnieri B, Abernethy AP. Development and validation of a high-quality composite real-world mortality endpoint. Health Serv Res. 2018;53:4460-4476. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 166] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 16. | Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014;33:1242-1258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 787] [Cited by in RCA: 1116] [Article Influence: 93.0] [Reference Citation Analysis (0)] |
| 17. | Holch JW, Ricard I, Stintzing S, Modest DP, Heinemann V. The relevance of primary tumour location in patients with metastatic colorectal cancer: a meta-analysis of first-line clinical trials. Eur J Cancer. 2017;70:87-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 401] [Article Influence: 44.6] [Reference Citation Analysis (0)] |
| 18. | Aljehani MA, Morgan JW, Guthrie LA, Jabo B, Ramadan M, Bahjri K, Lum SS, Selleck M, Reeves ME, Garberoglio C, Senthil M. Association of primary tumor site with mortality in patients receiving bevacizumab and cetuximab for metastatic colorectal cancer. JAMA Surg. 2018;153:60-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Wang B, Yang J, Li S, Lv M, Chen Z, Li E, Yi M, Yang J. Tumor location as a novel high risk parameter for stage II colorectal cancers. PLoS One. 2017;12:e0179910. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Sunakawa Y, Ichikawa W, Tsuji A, Denda T, Segawa Y, Negoro Y, Shimada K, Kochi M, Nakamura M, Kotaka M, Tanioka H, Takagane A, Tani S, Yamaguchi T, Watanabe T, Takeuchi M, Fujii M, Nakajima T. Prognostic impact of primary tumor location on clinical outcomes of metastatic colorectal cancer treated with cetuximab plus oxaliplatin-based chemotherapy: a subgroup analysis of the JACCRO CC-05/06 trials. Clin Colorectal Cancer. 2017;16:e171-e180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Loupakis F, Yang D, Yau L, Feng S, Cremolini C, Zhang W, Maus MK, Antoniotti C, Langer C, Scherer SJ, Müller T, Hurwitz HI, Saltz L, Falcone A, Lenz HJ. Primary tumor location as a prognostic factor in metastatic colorectal cancer. J Natl Cancer Inst. 2015;107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 357] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 22. | Arnold D, Lueza B, Douillard JY, Peeters M, Lenz HJ, Venook A, Heinemann V, Van Cutsem E, Pignon JP, Tabernero J, Cervantes A, Ciardiello F. Prognostic and predictive value of primary tumour side in patients with RAS wild-type metastatic colorectal cancer treated with chemotherapy and EGFR directed antibodies in six randomized trials. Ann Oncol. 2017;28:1713-1729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 628] [Article Influence: 89.7] [Reference Citation Analysis (0)] |
| 23. | Wang ZX, Wu HX, He MM, Wang YN, Luo HY, Ding PR, Xie D, Chen G, Li YH, Wang F, Xu RH. Chemotherapy with or without anti-EGFR agents in left- and right-sided metastatic colorectal cancer: an updated meta-analysis. J Natl Compr Canc Netw. 2019;17:805-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 24. | Meguid RA, Slidell MB, Wolfgang CL, Chang DC, Ahuja N. Is there a difference in survival between right- versus left-sided colon cancers? Ann Surg Oncol. 2008;15:2388-2394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 370] [Cited by in RCA: 387] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 25. | Venook AP, Niedzwiecki D, Lenz HJ, Innocenti F, Fruth B, Meyerhardt JA, Schrag D, Greene C, O'Neil BH, Atkins JN, Berry S, Polite BN, O'Reilly EM, Goldberg RM, Hochster HS, Schilsky RL, Bertagnolli MM, El-Khoueiry AB, Watson P, Benson AB, Mulkerin DL, Mayer RJ, Blanke C. Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients with KRAS wild-type advanced or metastatic colorectal cancer: a randomized clinical trial. JAMA. 2017;317:2392-2401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 507] [Cited by in RCA: 681] [Article Influence: 85.1] [Reference Citation Analysis (0)] |
| 26. | Benedix F, Schmidt U, Mroczkowski P, Gastinger I, Lippert H, Kube R; Study Group "Colon/Rectum Carcinoma (Primary Tumor)". Colon carcinoma-classification into right and left sided cancer or according to colonic subsite?-analysis of 29,568 patients. Eur J Surg Oncol. 2011;37:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |