Published online Oct 15, 2019. doi: 10.4251/wjgo.v11.i10.830
Peer-review started: February 26, 2019
First decision: April 15, 2019
Revised: May 29, 2019
Accepted: August 27, 2019
Article in press: August 28, 2019
Published online: October 15, 2019
Processing time: 234 Days and 11.7 Hours
Esophageal cancer (EC) generally consists of squamous cell carcinoma (which arise from squamous epithelium) and adenocarcinoma (which arise from columnar epithelium). Due to the increased recognition of risk factors associated with EC and the development of screening programs, there has been an increase in the diagnosis of early EC. Early EC is amenable to curative therapy by endoscopy, which can be performed by either endoscopic resection or endoscopic ablation. Endoscopic resection consists of either endoscopic mucosal resection (preferred in cases of adenocarcinoma) or endoscopic submucosal dissection (preferred in cases of squamous cell carcinoma). Endoscopic ablation can be performed by either radiofrequency ablation, cryotherapy, argon plasma coagulation or photodynamic therapy, amongst others. Endoscopy can also assist in the management of complications post-esophageal surgery, such as anastomotic leaks and perforations. Finally, there is a growing role for endoscopy to manage end-of-life palliative symptoms, especially dysphagia. The growing use of esophageal stents, debulking therapy and dilation can assist in improving a patient’s quality of life. In this review, we examine the multiple roles of endoscopy in the management of patients with EC.
Core tip: The endoscopic management of esophageal cancer is continuously evolving. Although, endoscopy was generally reserved for diagnosis, but due to the growing evidence around screening, early cancers are now being detected. Therefore, endoscopy has now grown to include an increasing therapeutic role in esophageal cancer. This includes resection by either endoscopic mucosal resection or endoscopic mucosal dissection. Ablative therapies by endoscopy including the use of radiofrequency ablation and photodynamic therapies are also growing. Finally, the role of endoscopy entails palliative management, such as the use of esophageal stent placements.
- Citation: Ahmed O, Ajani JA, Lee JH. Endoscopic management of esophageal cancer. World J Gastrointest Oncol 2019; 11(10): 830-841
- URL: https://www.wjgnet.com/1948-5204/full/v11/i10/830.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v11.i10.830
Esophageal cancer (EC) is an overarching term generally used to describe two separate malignancies, esophageal squamous cell carcinoma (SCC) and esophageal adenocarcinoma. Esophageal SCCs arise in the squamous epithelium (generally in the mid-proximal esophagus but can occur throughout the esophagus) whereas esophageal adenocarcinomas arise in the columnar epithelium and are generally found in the distal esophagus.
The epidemiology of EC is evolving. Although ECs only make up one percent of all new cancer cases in the United States, they make up 2.6% of all cancer deaths. The overall incidence of all types of EC has remained steady over the past two decades with an estimated 17000 new cases annually in the United States. The 5-year survival rate of EC varies according to how advanced the tumor is at diagnosis. Those with localized disease have a 5-year survival rate of 45.2%, while those with distant metastases have a 5-year survival rate of only 4.8%[1,2].
Due to the aggressive nature of the disease and the high mortality rate, it is imperative to identify patients early in the course of the disease. Currently, only 19% of cases are staged as localized disease at diagnosis. The benefit of localized disease is that it opens up a whole array of treatment options including the use of endoscopic therapy. The increasing recognition of risk factors associated with metaplasia and dysplasia has led to an increased interest in screening and surveillance programs. For example, the role of gender, obesity and gastroesophageal reflux disease in the development of Barrett’s esophagus (BE) has allowed for the development of screening and surveillance guidelines, which has then lead to treatment guidelines for pre-cancerous and early cancerous lesions[3,4].
Although endoscopy was initially limited to the diagnosis of EC, recent advancements have allowed the modality to play a growing role in the management of the tumor. The development of advance camera technology has allowed better recognition of the disease, while simultaneously the introduction of novel endoscopic techniques and instruments has allowed endoscopists to treat pre-cancerous lesions and even early ECs.
In this review, the current indications for endoscopy in the management of EC are reviewed. The pre-endoscopic management work-up, endoscopic options for curative therapy, the role of endoscopy in managing complications of surgery as well as how endoscopy can play an essential part in the palliative management of EC are described.
The first step in performing endoscopic management in patients with EC is to recognize the setting where it is appropriate. Multiple studies have demonstrated improved outcomes and less complications in high-volume centers, and therefore consideration should be given to referring patients to centers with experience when endoscopic curative management is an option[5,6]. Certain guidelines recommend that endoscopic resection (ER) of early EC only be done in high-volume centers. Similarly, a multi-disciplinary approach, with involvement of surgery, oncology and pathology is critical as the diagnosis of dysplasia can be controversial with poor intra- and inter-observer agreement[8]. A second opinion, ideally from a gastrointestinal pathologist, should be sought if there are doubts about the presence of dysplasia. Additionally, a multi-disciplinary approach will allow for more flexibility and options for the patients and assist in managing any potential complications.
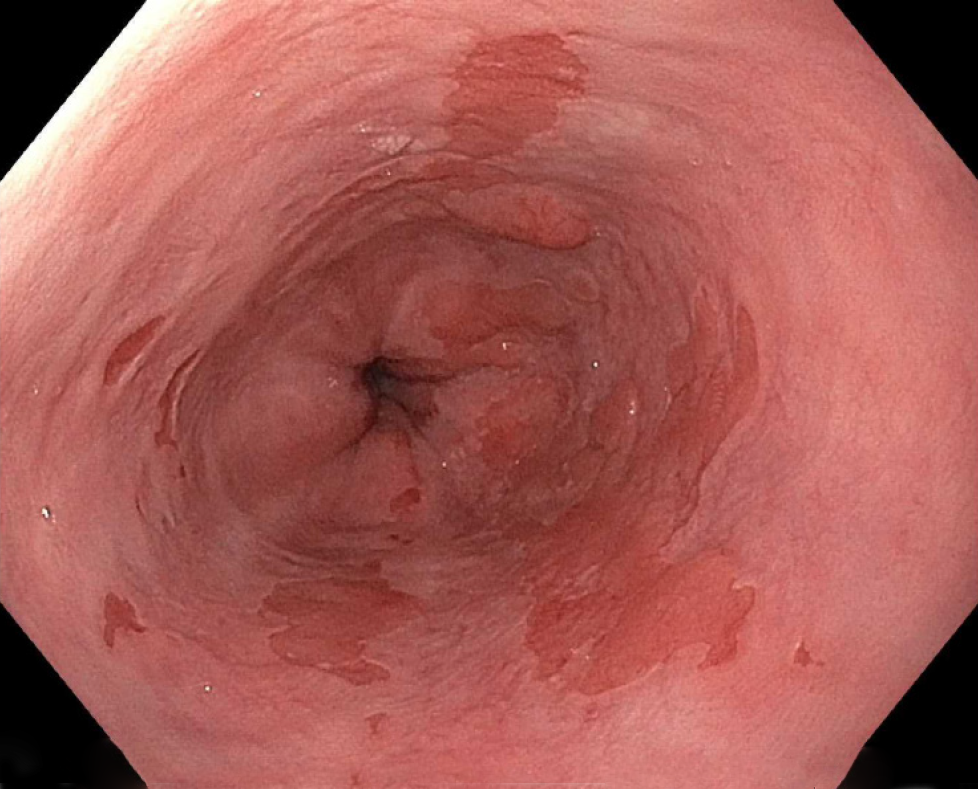
Once a patient has been referred for endoscopic management of pre-cancerous lesions or early EC, it is vital to establish the stage and characteristics of the tumor. This is done through a combination of endoscopic investigations, as well as potentially other modalities to ensure the tumor has not progressed. In terms of endoscopy, careful examination of the lesion is essential prior to any decision regarding endoscopic therapy. After washing the esophagus to remove any food, liquid or debris, careful examination of affected areas with white-light endoscopy should be performed. Recent studies have demonstrated that high-definition endoscopy is superior to standard definition in assessing mucosal changes in patients with BE (Figure 1)[9].
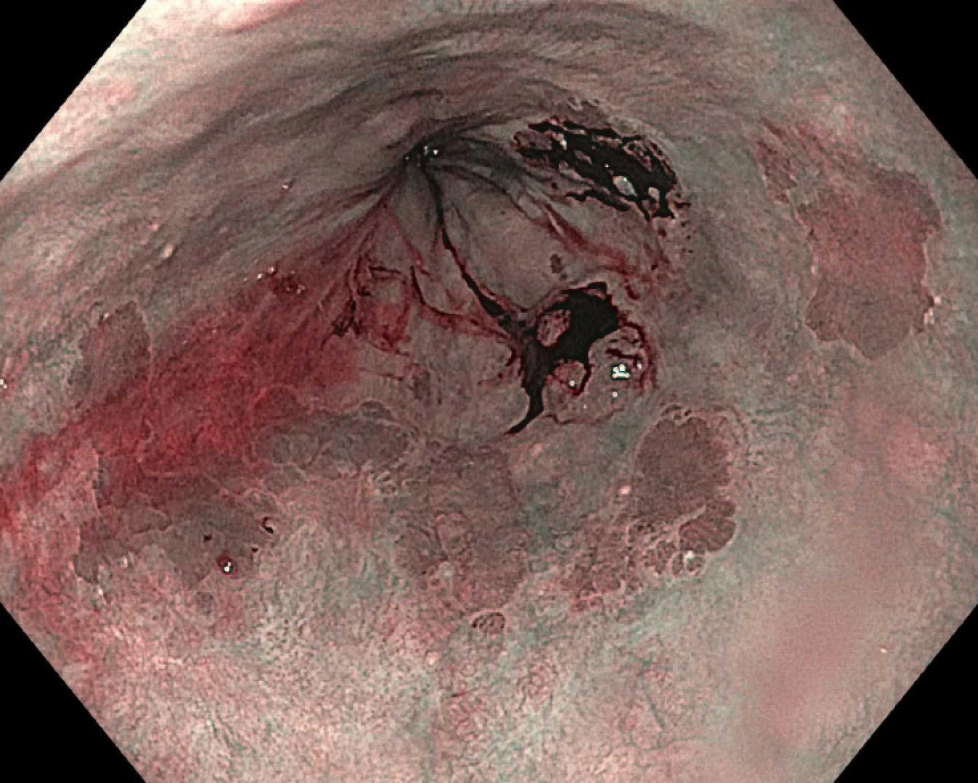
In addition, although there has been an increase in the use of adjuncts to white-light imaging, their evidence in the diagnosis of EC is still controversial with the exception of narrow-band imaging (NBI). NBI is a technique that allows increased highlighting of mucosa and the mucosal vasculature (Figure 2). A meta-analysis on the use of NBI to identify high-grade dysplasia (HGD) in patients with BE demonstrated a pooled sensitivity of 0.96 (95% confidence interval: 0.93-0.99) and a pooled specificity of 0.94 (95% confidence interval: 0.84-1.0). The meta-analysis included eight studies with 446 patients and a total of 2194 lesions. Based on these studies, there has been an increasing use of NBI to identify high-risk lesions].
Similar to NBI, there has been extensive investigation into the use of chromoendoscopy. Chromoendoscopy is the use of selective dyes to highlight specific features on the mucosa and potentially increase the contrast between normal mucosa and abnormal mucosa. The most commonly used dye in chromoendoscopy is methylene blue, which is thought to selectively stain intestinal metaplasia. A previous randomized control trial on the use of methylene blue as compared to random 4-quadrant biopsies showed that although there was no increased detection of dysplasia, the use of methylene blue led to a smaller requirement for the number of biopsies[11]. On the other hand, a separate randomized control trial showed that methylene blue detected less dysplasia compared to random 4-quadrant biopsies]. Finally, a systematic review and meta-analysis was performed in 2009 and included nine studies with a total of 450 patients. The study demonstrated no incremental yield in the use of chromoendoscopy as compared to standard 4-quadrant biopsies]. Subsequently, current guidelines do not recommend the routine use of chromoendoscopy when assessing esophageal lesions for advanced or high-risk features.
When inspecting a lesion with white-light endoscopy or NBI, there are certain features that should be carefully sought for in the mucosa as they will likely change therapy. When examining BE, it is important to document landmarks including any potential hiatal hernia, the location of the gastroesophageal junction, the top of the gastric folds, the location of the squamo-columnar junction and the length of columnar mucosa both circumferentially and the maximal longitudinal length. One commonly used classification for reporting BE is the Prague classification, which documents circumferential and maximal longitudinal length and has been found to have high validity and inter-observer agreement[14,15].
In addition, it is critical to document any nodularity found and the location of the nodularity as it will likely require separate management from the remainder of the BE. Nodules are also suggestive of advanced lesions requiring therapy. In addition to nodules, other high-risk features that portend to malignancy include the presence of ulceration or structuring[16]. Careful examination should be done in the 12 o’clock to 6 o’clock (or the right hemisphere) as these have higher rates of EC in BE[17].
Although a careful examination of a lesion using white-light endoscopy is the gold standard, there have been previous studies looking into adjunctive methods to determine resectability. One potential option was the use of endoscopic ultrasound (EUS). EUS would allow the clinician to determine the depth of the lesion as well as any potential locoregional lymph nodes. Initially, the thought was that EUS could provide the ability to determine whether any invasive cancer was present and therefore assist in determining which lesions endoscopic therapy should be avoided. Although initial results were promising, they have not been followed up by similar outcomes in subsequent studies[18].
A systematic review and meta-analysis examining the role of EUS found that EUS only had a 65% concordance for T-staging when compared to surgical or endoscopic mucosal resection (EMR) based pathology[19]. A follow-up meta-analysis found better results but was limited due to the heterogeneity between studies]. A more recent study examined the same utility of EUS in pre-malignant lesions and found poor correlation with a sensitivity of 50% and a specificity of 93%[21,22]. Interestingly, previous studies have found that EUS-guided mini-probe based examinations have better sensitivity than radial echoendoscopes]. Due to all the previous studies, the use of EUS to determine resectability is limited and should not be done to guide management decisions in patients with pre-malignant lesions.
Nevertheless, EUS can provide a helpful role in patients with early EC. Although EUS has difficulty staging cancers, it can be a useful tool in both identifying and sampling lymph nodes (Figure 3). EUS generally has been found to over-stage T2 malignancies and therefore caution should be taken before labelling a lesion as unresectable[24]. When it comes to lymph nodes, EUS was found to have fairly high sensitivity and specificity as compared to positive electron-transmission scans and has the added benefit of being able to sample nodes through a fine needle aspiration or biopsy[25,26].
In general, when approaching a patient for potential endoscopic management, it is important to ensure that care is provided in a center with expertise not only in endoscopy but also in surgery, pathology and radiology. The most important investigation is a careful examination during upper endoscopy both with white light endoscopy and NBI. Although adjunctive investigations have so far not yielded fruit, consideration can be given to performing EUS if there is concern for locoregional invasion.
When it comes to the endoscopic management of EC, it can generally be divided into two categories, curative and palliative therapy. Curative therapy is generally reserved for early ECs limited to the mucosa with no lymph node involvement. In this section, we will review the common methods for endoscopic management, as well as upcoming frontiers.
ER is the mainstay of endoscopic management of early ECs. ER can be performed in two ways, by EMR or by endoscopic submucosal dissection (ESD). ER can be performed for both adenocarcinomas and SCCs. In adenocarcinoma patients, the spectrum of disease where ER can be performed generally includes pre-malignant low-grade dysplasia in a patient with BE up to in some cases stage T1b adenocarcinoma (as per the TNM staging of tumors). For SCCs, ER can be performed in patients with early EC that is staged as T1 or intramucosal.
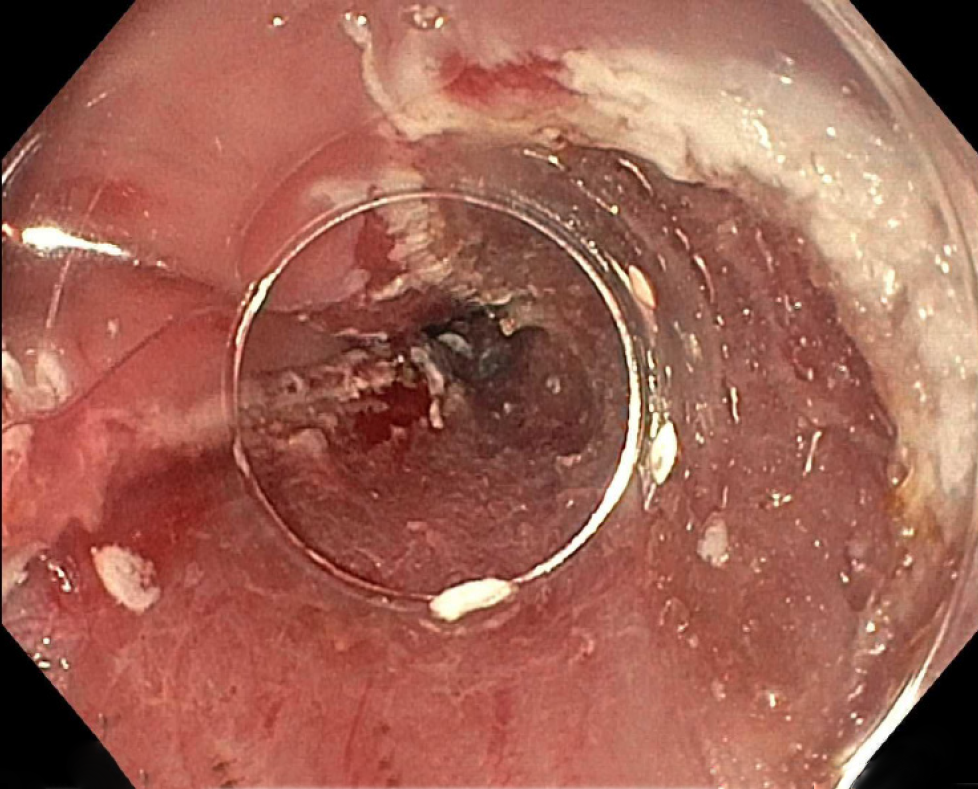
EMR is generally performed by two distinct methods: the cap-assisted method and the ligation-assisted method. The cap-assisted method, also known as the “suck and cut” method involves suctioning the mucosa into a cap-fitted endoscope and then using a snare to cut the mucosa. The snare is pre-opened prior to suctioning and generally comes as part of a pre-assembled ensemble kit. In the ligation-assisted method, or multi-band ligator method, the upper endoscope is fitted with an apparatus similar to a variceal band ligator, and the mucosa is suctioned and has a band placed around it. Subsequently, a snare is passed, and the mucosa upheld by the band is resected (Figure 4).
The evidence comparing the two methods of EMR showed that they are generally comparable. In a randomized control trial comparing the techniques, the ligation-assisted method was shown to be quicker with smaller resection specimens compared to the cap-assisted method. However, both techniques had similar maximal thickness in their resection specimens and similar adverse event rates (Figure 5)[27]. Previous studies that compared the two techniques in a non-randomized manner also demonstrated similar results[28,29]. The use of the lifting and then direct snare technique that is commonly used in the colon is discouraged in the esophagus due to an increased risk of perforation[30].
ESD is a more recent technique that involves careful dissection of the submucosa of the lesion in systematic fashion followed by en bloc removal of the desired tissue. Although the benefit is that it provides en bloc specimen and can give information about the margins of resection, the disadvantage is that it is time consuming and requires a deeper resection potentially leading to increase adverse events. Indeed, in a systematic review and meta-analysis comprising of 15 non-randomized trials comparing ESD to EMR, they found that although ESD had higher curative resection rates and lesser local recurrence rates, it was balanced by more time-consuming procedures and higher rates of bleeding and perforation]. Another meta-analysis looking specifically at esophageal neoplasms found no difference between EMR and ESD in terms of margins, lymph node positivity or metachronous cancers but found less recurrence with ESD though balanced by an increased risk of strictures[32].
The one situation where ESD has had positive results (as compared to EMR) is in the setting of SCCs. A previous study examining resection techniques found less recurrence when en bloc resection was performed by ESD in patients with SCC as compared to patients that had piecemeal resection[33]. Based on this study, EMR is generally considered sufficient for small lesions (less than 10 mm) if the diagnosis is SCC, but patients with larger lesions should ideally undergo ESD. Overall, current guidelines recommend EMR for resection of BE or early esophageal adenocarcinomas unless the lesions are larger than 15 mm, are poorly lifting or are at risk for submucosal invasion in which case ESD should be performed. For patients with SCC, current guidelines generally recommend ESD though EMR is acceptable in smaller lesions[34].
Ablative therapy is generally reserved for flat lesions or treatment of BE after ER. There are many ways to perform ablative therapy with the most common being radiofrequency ablation (RFA) (Figure 6). Other methods that are less commonly used include photodynamic therapy (PDT) and cryoablation. The main purpose of ablative therapy is to destroy the remaining residual malignant or pre-malignant tissue to prevent recurrence.
RFA is the application of thermal energy that is generated by radiofrequency waves to destroy tissue. It involves contact ablation and can be done in localized areas or in a circumferential manner. The seminal study examining the effects of RFA was published in 2009. It was a multi-center randomized control trial that compared RFA to sham therapy in patients with dysplastic BE. The primary outcome (complete eradication) was followed until 12 mo post-therapy. In the RFA group, when using intention-to-treat analysis, 90.5% of patients had complete eradication whereas in the sham group only 22.7% had eradication. The main adverse event related to RFA was the development of chest pain post-treatment[35]. Similar results have been shown in the other multi-center studies including European and Asian populations[36,37].
The role of endoscopic therapy in patients with low-grade dysplasia has been controversial, and there has been debate on whether to pursue endoscopic management or only perform careful observation. A previous study examining patients with BE with only low-grade dysplasia found a decrease in the progression of the dysplasia and the development of cancer with the use of RFA[38]. Finally, there have been studies on whether RFA should be applied to patients with BE but no evidence of dysplasia. A study looking at the cost-effectiveness of RFA therapy found that treatment of patients with BE without dysplasia did not provide cost-effective therapy[39].
Current guidelines generally recommend RFA in patients with dysplasia with non-nodular lesions or intra-mucosal cancer. RFA should also be performed to treat residual BE in patients who have undergone ER. Additionally, although RFA has become well-established in the management of patients with BE or adenocarcinoma, its role in the management of SCC is still developing. Recent studies have showed promise in early SCC with high complete eradication rates and low recurrence rates[40,41].
Other types of ablative therapy include argon plasma coagulation (APC), cryoablation and PDT. APC is widely available, generally due to its use in multiple conditions and diseases and has been widely investigated in the management of BE. In one study examining the role of APC in patients with non-dysplastic BE, complete eradication was successful in 77% of the patients (37/48). The mean number of sessions required was 2.8 (range 1-5) though 9.8% (5/51) had major complications including perforation, hemorrhage and stricture formation[42]. Nevertheless, other studies have showed similar positive results with APC[43,44].
Cryoablation of the esophagus has also been studied in the management of pre-malignant and malignant conditions of the esophagus. The most widely used method is the application of liquid nitrogen therapy. Previous studies have shown high eradication rates in patients with intestinal metaplasia and HGD with minimal adverse events[45]. There have also been long-term retrospective studies to determine the sustained ability of cryotherapy. A 5-year follow-up of patients who received cryotherapy revealed complete eradication rates of 93% in HGD and 75% in intestinal metaplasia. The rate of progression to HGD or adenocarcinoma was 1.4% per patient-year in those treated with cryotherapy[46]. Cryotherapy has also been studied as rescue or salvage therapy in patients who have had recurrence after initial RFA therapy. The complete eradication of dysplasia rate was 75% in those subsequently treated with cryotherapy, including two patients who initially had intramucosal adenocarcinoma and were both successfully treated[47].
PDT is an ablative process in which a photosensitizer drug is activated by the use of laser light, which leads to mucosal destruction. PDT has evidence in the management of both SCC and esophageal adenocarcinomas. Treatment of either cancer staged as either T1 or T2 showed a complete response rate of 87% with the majority of the complications being either cutaneous photosensitization or esophageal strictures[48]. Long-term follow-up has shown sustained response and low rates of recurrence as well[49,50]. Comparisons between PDT and APC in the eradication of both BE and dysplasia have showed similar effectiveness though higher costs associated with PDT[51,52]. A study comparing RFA to PDT in patients with BE with dysplasia found that RFA had higher complete response rates and was significantly less costly. Though caution must be taken in interpreting these results as the study was non-randomized with major differences in the baseline characteristics of the two groups[53].
In summary, there are many methods that have evolved to treat flat mucosal lesions with pre-malignant or malignant findings. RFA is generally the most widespread method with increasing evidence of its utility backed by a strong safety record. The development of circumferential balloons as well as through-the-scope segmental pads has made it more user-friendly. In patients who have failed RFA after multiple attempts, consideration should be given to alternative modalities including APC, cryoablation and potentially PDT based on local expertise.
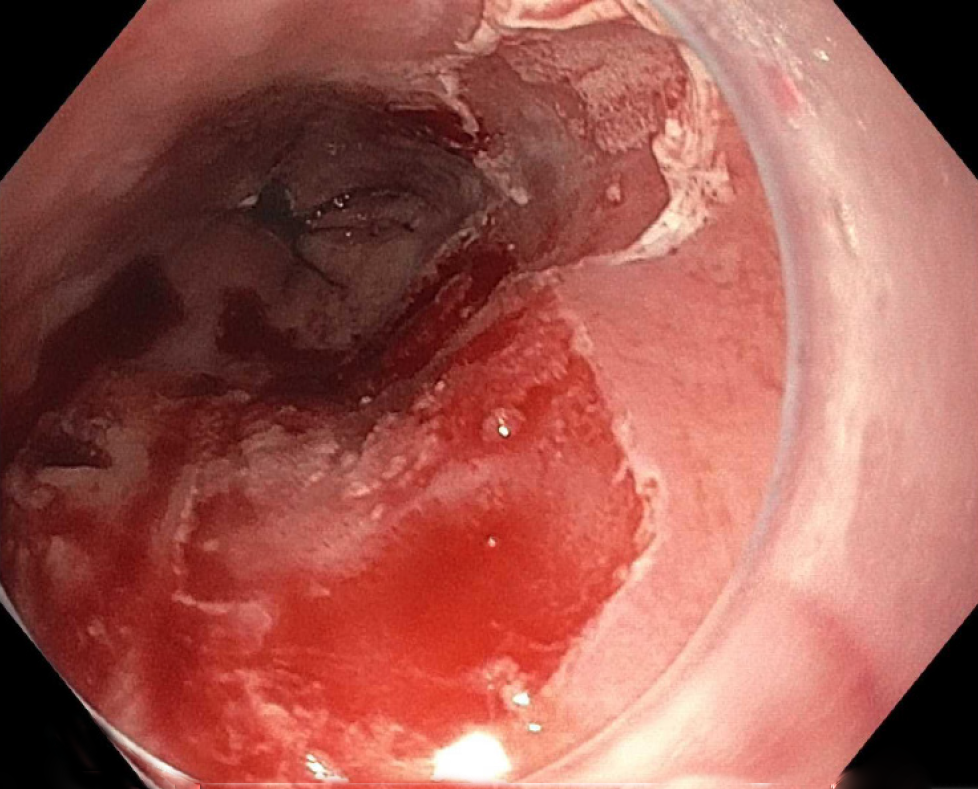
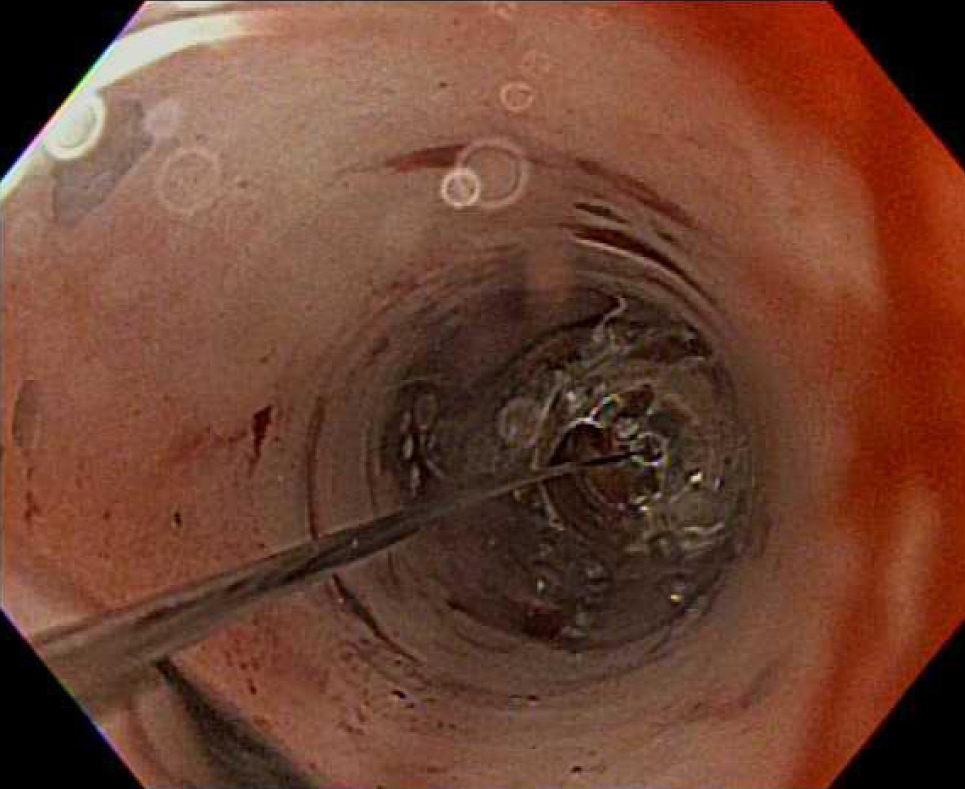
Although an increasing number of patients are being diagnosed with early EC that is amenable to curative resection by endoscopy, a large proportion still progress to surgery. Depending on the features of the tumor and its aggressiveness, the algorithm of neo-adjuvant therapy followed by surgery is generally followed. Nevertheless, endoscopy can play a central role in patients who develop post-operative complications after surgery for EC. The most common complication is the development of a post-operative leak generally at the anastomosis (Figure 7). The incidence of post-operative complications can be as high as 22.9% of post-esophageal resection cases[54]. The rates of esophageal leaks have been shown to be as high as 7.9% of all esophageal surgeries[55]. Prompt recognition and management of esophageal leaks is imperative as the mortality rate associated with leaks can be as high as 35%[56].
Esophageal stent placement is an alternative to a re-operation for an anastomotic leak. Most commonly, a self-expanding metal stent (SEMS) is placed to overlap the site of the leak and allow it to heal. Although SEMS generally come in varying sizes, consideration should be given to place the largest tolerable diameter to prevent migration of the stent as there likely is no narrowing to hold the stent in place. In our practice, we generally use SEMS with a diameter of 23 mm to treat esophageal anastomotic leaks. The securing of the esophageal stent can be done by a variety of methods, including placing a hemostatic clip between the stent and the mucosa or possibly using an endoscopic suturing device to secure the stent in place. The evidence for the role of esophageal stents in the post-operative setting is variable with studies ranging from a technical success (ability to place the stent) rate between 80% to 100% to a clinical success rate (resolution of the leak and removal of the stent) that can be as low as 45%[57,58]. The most common complications post-stent placement is pain, stent migration and bleeding[59].
Other methods can be considered for anastomotic leaks including endoscopic clip placement to close the defect. The development of over-the-scope clips have allowed larger defects to be closed endoscopically. Multiple trials on the use of endoscopic clip placement have demonstrated high rates of clinical success and closure. A recent large study examined the role of over-the-scope clips in closure of luminal defects. A total of 188 patients were included of which 108 had fistulas, 48 had perforations and 32 had leaks. Successful closure occurred in 90% of patients with perforations, 73% with leaks but only 42.9% of patients with fistulas[60].
Once a patient has advanced disease not amenable to curative therapy, the shift of care turns towards palliative management. The role of endoscopy in palliative care is generally the improvement of symptoms especially dysphagia. As patients focus more on end of life care, the need to ensure the ability to take oral contents becomes a matter of quality of life. The main components of endoscopic management in palliative care are dilation, debulking and esophageal stent placement.
In regard to dilation, the reducing caliber of the esophagus secondary to tumor is the main reason for dysphagia and intermittent periodic dilations are an option to treat the disease (Figure 8). Unfortunately, dilation alone rarely provides long-lasting efficacy, and this is compounded by high rates of complications especially perforations[61]. Endoscopic debulking therapy can be achieved by the use of laser therapy, PDT or chemical therapy. Chemical therapy, including the use of absolute alcohol, generally only provides transient relief and requires multiple ongoing sessions]. PDT has generally been found to be better than laser therapy as shown in randomized comparison trials that have showed similar efficacy between laser therapy (e.g., Nd : YAG) and PDT but less perforations associated with PDT[63].
Finally, the mainstay of esophageal palliation is the placement of esophageal stents. The most common form of esophageal stents are SEMS, and they can come in covered, partially covered and uncovered forms (Figure 9). The evidence for the role of esophageal stents is controversial. Although they have been shown to have durable effectiveness towards dysphagia and lower rates of perforation as compared to dilation alone, they are limited due to patient intolerance of chest pain as well as the risk of stent migration[64].
As the epidemiology and presentation of EC evolves, so does the role of endoscopy in its care. No longer relegated to diagnosis only, endoscopy can provide curative therapy in early EC as well as provide therapy for pre-malignant changes. It can also be used to manage complications related to the management of EC specifically post-operative complications. Finally, there is a growing role for endoscopy in the palliative management of EC with an increasing use of debulking therapy as well as the ongoing relief of dysphagia with esophageal stent placements.
Author contributions: Ahmed O was involved in review design and drafting of the manuscript; Ajani JA was involved in critical revision of the manuscript; Lee JH was involved in review design and critical revision of the manuscript.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Fogli L, Gkekas I, Lambrecht NW, Lee CL, Sami SS, Vynios D S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Zhou BX
| 1. | Cai X, Zhai J, Kaplan DE, Zhang Y, Zhou L, Chen X, Qian G, Zhao Q, Li Y, Gao L, Cong W, Zhu M, Yan Z, Shi L, Wu D, Wei L, Shen F, Wu M. Background progenitor activation is associated with recurrence after hepatectomy of combined hepatocellular-cholangiocarcinoma. Hepatology. 2012;56:1804-1816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Torre LA, Siegel RL, Ward EM, Jemal A. Global Cancer Incidence and Mortality Rates and Trends--An Update. Cancer Epidemiol Biomarkers Prev. 2016;25:16-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2004] [Cited by in RCA: 2488] [Article Influence: 248.8] [Reference Citation Analysis (0)] |
| 3. | Greene CL, Worrell SG, Attwood SE, Chandrasoma P, Chang K, DeMeester TR, Lord RV, Montgomery E, Pech O, Vallone J, Vieth M, Wang KK, DeMeester SR. Emerging Concepts for the Endoscopic Management of Superficial Esophageal Adenocarcinoma. J Gastrointest Surg. 2016;20:851-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Shaheen NJ, Falk GW, Iyer PG, Gerson LB; American College of Gastroenterology. ACG Clinical Guideline: Diagnosis and Management of Barrett's Esophagus. Am J Gastroenterol. 2016;111:30-50; quiz 51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 990] [Cited by in RCA: 1058] [Article Influence: 117.6] [Reference Citation Analysis (0)] |
| 5. | van Vilsteren FG, Pouw RE, Herrero LA, Peters FP, Bisschops R, Houben M, Peters FT, Schenk BE, Weusten BL, Visser M, Ten Kate FJ, Fockens P, Schoon EJ, Bergman JJ. Learning to perform endoscopic resection of esophageal neoplasia is associated with significant complications even within a structured training program. Endoscopy. 2012;44:4-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Fudman DI, Lightdale CJ, Poneros JM, Ginsberg GG, Falk GW, Demarshall M, Gupta M, Iyer PG, Lutzke L, Wang KK, Abrams JA. Positive correlation between endoscopist radiofrequency ablation volume and response rates in Barrett's esophagus. Gastrointest Endosc. 2014;80:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | di Pietro M, Fitzgerald RC; BSG Barrett's guidelines working group. Revised British Society of Gastroenterology recommendation on the diagnosis and management of Barrett's oesophagus with low-grade dysplasia. Gut. 2018;67:392-393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 8. | Curvers WL, ten Kate FJ, Krishnadath KK, Visser M, Elzer B, Baak LC, Bohmer C, Mallant-Hent RC, van Oijen A, Naber AH, Scholten P, Busch OR, Blaauwgeers HG, Meijer GA, Bergman JJ. Low-grade dysplasia in Barrett's esophagus: overdiagnosed and underestimated. Am J Gastroenterol. 2010;105:1523-1530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 332] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 9. | Sami SS, Subramanian V, Butt WM, Bejkar G, Coleman J, Mannath J, Ragunath K. High definition versus standard definition white light endoscopy for detecting dysplasia in patients with Barrett's esophagus. Dis Esophagus. 2015;28:742-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Mannath J, Subramanian V, Hawkey CJ, Ragunath K. Narrow band imaging for characterization of high grade dysplasia and specialized intestinal metaplasia in Barrett's esophagus: a meta-analysis. Endoscopy. 2010;42:351-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 136] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 11. | Horwhat JD, Maydonovitch CL, Ramos F, Colina R, Gaertner E, Lee H, Wong RK. A randomized comparison of methylene blue-directed biopsy versus conventional four-quadrant biopsy for the detection of intestinal metaplasia and dysplasia in patients with long-segment Barrett's esophagus. Am J Gastroenterol. 2008;103:546-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Lim CH, Rotimi O, Dexter SP, Axon AT. Randomized crossover study that used methylene blue or random 4-quadrant biopsy for the diagnosis of dysplasia in Barrett's esophagus. Gastrointest Endosc. 2006;64:195-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Ngamruengphong S, Sharma VK, Das A. Diagnostic yield of methylene blue chromoendoscopy for detecting specialized intestinal metaplasia and dysplasia in Barrett's esophagus: a meta-analysis. Gastrointest Endosc. 2009;69:1021-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 106] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Vahabzadeh B, Seetharam AB, Cook MB, Wani S, Rastogi A, Bansal A, Early DS, Sharma P. Validation of the Prague C & M criteria for the endoscopic grading of Barrett's esophagus by gastroenterology trainees: a multicenter study. Gastrointest Endosc. 2012;75:236-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Sharma P, Dent J, Armstrong D, Bergman JJ, Gossner L, Hoshihara Y, Jankowski JA, Junghard O, Lundell L, Tytgat GN, Vieth M. The development and validation of an endoscopic grading system for Barrett's esophagus: the Prague C & M criteria. Gastroenterology. 2006;131:1392-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 731] [Cited by in RCA: 716] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 16. | Switzer-Taylor V, Schlup M, Lübcke R, Livingstone V, Schultz M. Barrett's esophagus: a retrospective analysis of 13 years surveillance. J Gastroenterol Hepatol. 2008;23:1362-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Enestvedt BK, Lugo R, Guarner-Argente C, Shah P, Falk GW, Furth E, Ginsberg GG. Location, location, location: does early cancer in Barrett's esophagus have a preference? Gastrointest Endosc. 2013;78:462-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Larghi A, Lightdale CJ, Memeo L, Bhagat G, Okpara N, Rotterdam H. EUS followed by EMR for staging of high-grade dysplasia and early cancer in Barrett's esophagus. Gastrointest Endosc. 2005;62:16-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 143] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 19. | Young PE, Gentry AB, Acosta RD, Greenwald BD, Riddle M. Endoscopic ultrasound does not accurately stage early adenocarcinoma or high-grade dysplasia of the esophagus. Clin Gastroenterol Hepatol. 2010;8:1037-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 20. | Thosani N, Singh H, Kapadia A, Ochi N, Lee JH, Ajani J, Swisher SG, Hofstetter WL, Guha S, Bhutani MS. Diagnostic accuracy of EUS in differentiating mucosal versus submucosal invasion of superficial esophageal cancers: a systematic review and meta-analysis. Gastrointest Endosc. 2012;75:242-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 165] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 21. | Bartel MJ, Wallace TM, Gomez-Esquivel RD, Raimondo M, Wolfsen HC, Woodward TA, Wallace MB. Role of EUS in patients with suspected Barrett's esophagus with high-grade dysplasia or early esophageal adenocarcinoma: impact on endoscopic therapy. Gastrointest Endosc. 2017;86:292-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Pouw RE, Heldoorn N, Alvarez Herrero L, ten Kate FJ, Visser M, Busch OR, van Berge Henegouwen MI, Krishnadath KK, Weusten BL, Fockens P, Bergman JJ. Do we still need EUS in the workup of patients with early esophageal neoplasia? A retrospective analysis of 131 cases. Gastrointest Endosc. 2011;73:662-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 23. | Pech O, Günter E, Dusemund F, Ell C. Value of high-frequency miniprobes and conventional radial endoscopic ultrasound in the staging of early Barrett's carcinoma. Endoscopy. 2010;42:98-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Pech O, Günter E, Dusemund F, Origer J, Lorenz D, Ell C. Accuracy of endoscopic ultrasound in preoperative staging of esophageal cancer: results from a referral center for early esophageal cancer. Endoscopy. 2010;42:456-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 25. | Buskens CJ, Westerterp M, Lagarde SM, Bergman JJ, ten Kate FJ, van Lanschot JJ. Prediction of appropriateness of local endoscopic treatment for high-grade dysplasia and early adenocarcinoma by EUS and histopathologic features. Gastrointest Endosc. 2004;60:703-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 178] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 26. | Keswani RN, Early DS, Edmundowicz SA, Meyers BF, Sharma A, Govindan R, Chen J, Kohlmeier C, Azar RR. Routine positron emission tomography does not alter nodal staging in patients undergoing EUS-guided FNA for esophageal cancer. Gastrointest Endosc. 2009;69:1210-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Pouw RE, van Vilsteren FG, Peters FP, Alvarez Herrero L, Ten Kate FJ, Visser M, Schenk BE, Schoon EJ, Peters FT, Houben M, Bisschops R, Weusten BL, Bergman JJ. Randomized trial on endoscopic resection-cap versus multiband mucosectomy for piecemeal endoscopic resection of early Barrett's neoplasia. Gastrointest Endosc. 2011;74:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 124] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 28. | Peters FP, Kara MA, Curvers WL, Rosmolen WD, Fockens P, Krishnadath KK, Ten Kate FJ, Bergman JJ. Multiband mucosectomy for endoscopic resection of Barrett's esophagus: feasibility study with matched historical controls. Eur J Gastroenterol Hepatol. 2007;19:311-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | May A, Gossner L, Behrens A, Kohnen R, Vieth M, Stolte M, Ell C. A prospective randomized trial of two different endoscopic resection techniques for early stage cancer of the esophagus. Gastrointest Endosc. 2003;58:167-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 131] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 30. | di Pietro M, Canto MI, Fitzgerald RC. Endoscopic Management of Early Adenocarcinoma and Squamous Cell Carcinoma of the Esophagus: Screening, Diagnosis, and Therapy. Gastroenterology. 2018;154:421-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 173] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 31. | Cao Y, Liao C, Tan A, Gao Y, Mo Z, Gao F. Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy. 2009;41:751-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 283] [Article Influence: 17.7] [Reference Citation Analysis (1)] |
| 32. | Sgourakis G, Gockel I, Lang H. Endoscopic and surgical resection of T1a/T1b esophageal neoplasms: a systematic review. World J Gastroenterol. 2013;19:1424-1437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 90] [Cited by in RCA: 101] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 33. | Ishihara R, Iishi H, Takeuchi Y, Kato M, Yamamoto S, Yamamoto S, Masuda E, Tatsumi K, Higashino K, Uedo N, Tatsuta M. Local recurrence of large squamous-cell carcinoma of the esophagus after endoscopic resection. Gastrointest Endosc. 2008;67:799-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 89] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 34. | Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 817] [Cited by in RCA: 927] [Article Influence: 92.7] [Reference Citation Analysis (0)] |
| 35. | Shaheen NJ, Sharma P, Overholt BF, Wolfsen HC, Sampliner RE, Wang KK, Galanko JA, Bronner MP, Goldblum JR, Bennett AE, Jobe BA, Eisen GM, Fennerty MB, Hunter JG, Fleischer DE, Sharma VK, Hawes RH, Hoffman BJ, Rothstein RI, Gordon SR, Mashimo H, Chang KJ, Muthusamy VR, Edmundowicz SA, Spechler SJ, Siddiqui AA, Souza RF, Infantolino A, Falk GW, Kimmey MB, Madanick RD, Chak A, Lightdale CJ. Radiofrequency ablation in Barrett's esophagus with dysplasia. N Engl J Med. 2009;360:2277-2288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1146] [Cited by in RCA: 973] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 36. | Pouw RE, Wirths K, Eisendrath P, Sondermeijer CM, Ten Kate FJ, Fockens P, Devière J, Neuhaus H, Bergman JJ. Efficacy of radiofrequency ablation combined with endoscopic resection for barrett's esophagus with early neoplasia. Clin Gastroenterol Hepatol. 2010;8:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 206] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 37. | Pasricha S, Li N, Bulsiewicz WJ, Rothstein RI, Infantolino A, Ertan A, Camara DS, Dellon ES, Triadafilopoulos G, Lightdale CJ, Madanick RD, Lyday WD, Muthusamy RV, Overholt BF, Shaheen NJ. Sex and race and/or ethnicity differences in patients undergoing radiofrequency ablation for Barrett's esophagus: results from the U.S. RFA Registry. Gastrointest Endosc. 2015;82:276-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 38. | Small AJ, Araujo JL, Leggett CL, Mendelson AH, Agarwalla A, Abrams JA, Lightdale CJ, Wang TC, Iyer PG, Wang KK, Rustgi AK, Ginsberg GG, Forde KA, Gimotty PA, Lewis JD, Falk GW, Bewtra M. Radiofrequency Ablation Is Associated With Decreased Neoplastic Progression in Patients With Barrett's Esophagus and Confirmed Low-Grade Dysplasia. Gastroenterology. 2015;149:567-76.e3; quiz e13-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 39. | Hur C, Choi SE, Rubenstein JH, Kong CY, Nishioka NS, Provenzale DT, Inadomi JM. The cost effectiveness of radiofrequency ablation for Barrett's esophagus. Gastroenterology. 2012;143:567-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 119] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 40. | He S, Bergman J, Zhang Y, Weusten B, Xue L, Qin X, Dou L, Liu Y, Fleischer D, Lu N, Dawsey SM, Wang GQ. Endoscopic radiofrequency ablation for early esophageal squamous cell neoplasia: report of safety and effectiveness from a large prospective trial. Endoscopy. 2015;47:398-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 41. | Bergman JJ, Zhang YM, He S, Weusten B, Xue L, Fleischer DE, Lu N, Dawsey SM, Wang GQ. Outcomes from a prospective trial of endoscopic radiofrequency ablation of early squamous cell neoplasia of the esophagus. Gastrointest Endosc. 2011;74:1181-1190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 42. | Manner H, May A, Miehlke S, Dertinger S, Wigginghaus B, Schimming W, Krämer W, Niemann G, Stolte M, Ell C. Ablation of nonneoplastic Barrett's mucosa using argon plasma coagulation with concomitant esomeprazole therapy (APBANEX): a prospective multicenter evaluation. Am J Gastroenterol. 2006;101:1762-1769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 66] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 43. | Pereira-Lima JC, Busnello JV, Saul C, Toneloto EB, Lopes CV, Rynkowski CB, Blaya C. High power setting argon plasma coagulation for the eradication of Barrett's esophagus. Am J Gastroenterol. 2000;95:1661-1668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 84] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 44. | Basu KK, Pick B, Bale R, West KP, de Caestecker JS. Efficacy and one year follow up of argon plasma coagulation therapy for ablation of Barrett's oesophagus: factors determining persistence and recurrence of Barrett's epithelium. Gut. 2002;51:776-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 88] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 45. | Gosain S, Mercer K, Twaddell WS, Uradomo L, Greenwald BD. Liquid nitrogen spray cryotherapy in Barrett's esophagus with high-grade dysplasia: long-term results. Gastrointest Endosc. 2013;78:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 46. | Ramay FH, Cui Q, Greenwald BD. Outcomes after liquid nitrogen spray cryotherapy in Barrett's esophagus-associated high-grade dysplasia and intramucosal adenocarcinoma: 5-year follow-up. Gastrointest Endosc. 2017;86:626-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 47. | Sengupta N, Ketwaroo GA, Bak DM, Kedar V, Chuttani R, Berzin TM, Sawhney MS, Pleskow DK. Salvage cryotherapy after failed radiofrequency ablation for Barrett's esophagus-related dysplasia is safe and effective. Gastrointest Endosc. 2015;82:443-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 48. | Sibille A, Lambert R, Souquet JC, Sabben G, Descos F. Long-term survival after photodynamic therapy for esophageal cancer. Gastroenterology. 1995;108:337-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 148] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 49. | Overholt BF, Panjehpour M, Halberg DL. Photodynamic therapy for Barrett's esophagus with dysplasia and/or early stage carcinoma: long-term results. Gastrointest Endosc. 2003;58:183-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 211] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 50. | Overholt BF, Wang KK, Burdick JS, Lightdale CJ, Kimmey M, Nava HR, Sivak MV, Nishioka N, Barr H, Marcon N, Pedrosa M, Bronner MP, Grace M, Depot M; International Photodynamic Group for High-Grade Dysplasia in Barrett's Esophagus. Five-year efficacy and safety of photodynamic therapy with Photofrin in Barrett's high-grade dysplasia. Gastrointest Endosc. 2007;66:460-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 229] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 51. | Ragunath K, Krasner N, Raman VS, Haqqani MT, Phillips CJ, Cheung I. Endoscopic ablation of dysplastic Barrett's oesophagus comparing argon plasma coagulation and photodynamic therapy: a randomized prospective trial assessing efficacy and cost-effectiveness. Scand J Gastroenterol. 2005;40:750-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 52. | Kelty CJ, Ackroyd R, Brown NJ, Stephenson TJ, Stoddard CJ, Reed MW. Endoscopic ablation of Barrett's oesophagus: a randomized-controlled trial of photodynamic therapy vs. argon plasma coagulation. Aliment Pharmacol Ther. 2004;20:1289-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 53. | Ertan A, Zaheer I, Correa AM, Thosani N, Blackmon SH. Photodynamic therapy vs radiofrequency ablation for Barrett's dysplasia: efficacy, safety and cost-comparison. World J Gastroenterol. 2013;19:7106-7113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 54. | Rutegård M, Lagergren P, Rouvelas I, Mason R, Lagergren J. Surgical complications and long-term survival after esophagectomy for cancer in a nationwide Swedish cohort study. Eur J Surg Oncol. 2012;38:555-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 55. | Rutegård M, Lagergren P, Rouvelas I, Lagergren J. Intrathoracic anastomotic leakage and mortality after esophageal cancer resection: a population-based study. Ann Surg Oncol. 2012;19:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 139] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 56. | Alanezi K, Urschel JD. Mortality secondary to esophageal anastomotic leak. Ann Thorac Cardiovasc Surg. 2004;10:71-75. [PubMed] |
| 57. | Schubert D, Scheidbach H, Kuhn R, Wex C, Weiss G, Eder F, Lippert H, Pross M. Endoscopic treatment of thoracic esophageal anastomotic leaks by using silicone-covered, self-expanding polyester stents. Gastrointest Endosc. 2005;61:891-896. [PubMed] |
| 58. | Rodrigues-Pinto E, Pereira P, Ribeiro A, Moutinho-Ribeiro P, Lopes S, Macedo G. Self-expanding metal stents in postoperative esophageal leaks. Rev Esp Enferm Dig. 2016;108:133-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 59. | Watkins JR, Farivar AS. Endoluminal Therapies for Esophageal Perforations and Leaks. Thorac Surg Clin. 2018;28:541-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 60. | Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M, Sharaiha RZ, Poley JW, Kahaleh M, Thompson CC, Ryan MB, Choksi N, Elmunzer BJ, Gosain S, Goldberg EM, Modayil RJ, Stavropoulos SN, Schembre DB, DiMaio CJ, Chandrasekhara V, Hasan MK, Varadarajulu S, Hawes R, Gomez V, Woodward TA, Rubel-Cohen S, Fluxa F, Vleggaar FP, Akshintala VS, Raju GS, Khashab MA. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc. 2014;80:610-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 207] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 61. | Adler DG, Baron TH. Endoscopic palliation of malignant dysphagia. Mayo Clin Proc. 2001;76:731-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 38] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 62. | Axelrad AM, al-Kawas FH. Palliation of malignant oesophageal obstruction by endoscopic alcohol injection. Gastrointest Endosc. 1995;41:272-274. [PubMed] |
| 63. | Lightdale CJ, Heier SK, Marcon NE, McCaughan JS, Gerdes H, Overholt BF, Sivak MV, Stiegmann GV, Nava HR. Photodynamic therapy with porfimer sodium versus thermal ablation therapy with Nd:YAG laser for palliation of esophageal cancer: a multicenter randomized trial. Gastrointest Endosc. 1995;42:507-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 193] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 64. | Madhusudhan C, Saluja SS, Pal S, Ahuja V, Saran P, Dash NR, Sahni P, Chattopadhyay TK. Palliative stenting for relief of dysphagia in patients with inoperable esophageal cancer: impact on quality of life. Dis Esophagus. 2009;22:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |