Copyright
©The Author(s) 2022.
World J Gastrointest Oncol. Mar 15, 2022; 14(3): 724-733
Published online Mar 15, 2022. doi: 10.4251/wjgo.v14.i3.724
Published online Mar 15, 2022. doi: 10.4251/wjgo.v14.i3.724
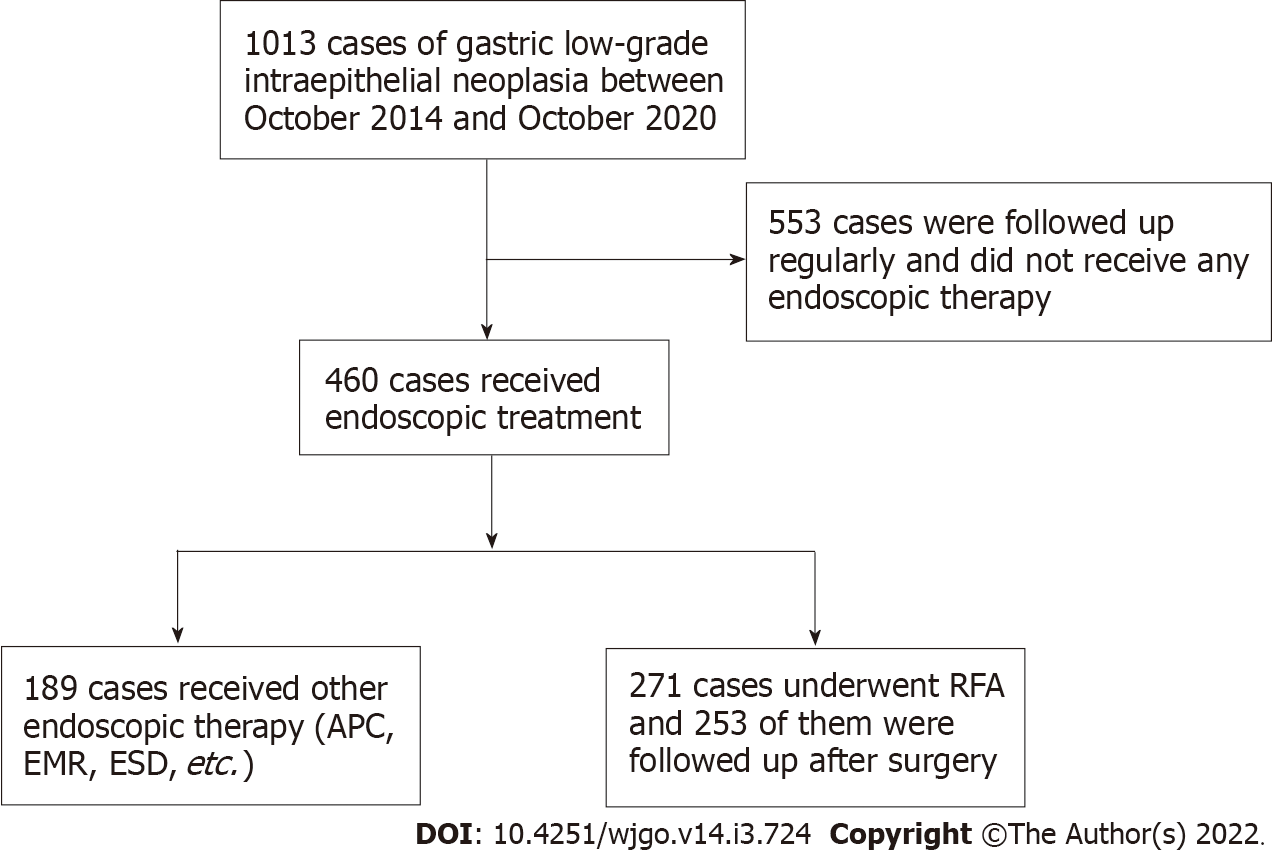
Figure 1 Flowchart of the patients enrolled in this study.
RFA: Radiofrequency ablation; APC: Argon plasma coagulation; EMR: Endoscopic mucosal resection; ESD: Endoscopic submucosal dissection.
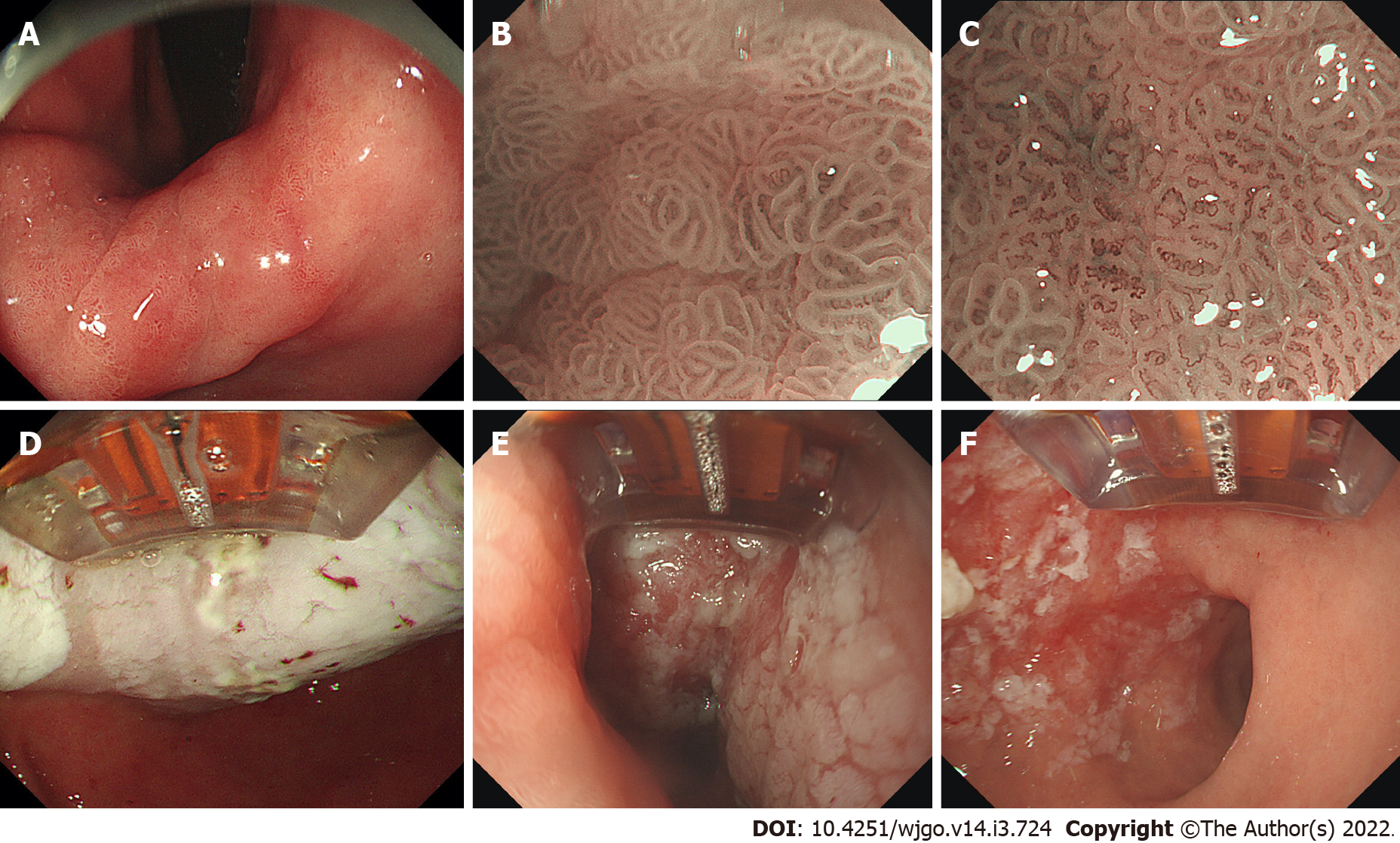
Figure 2 The radiofrequency ablation procedure of gastric low-grade intraepithelial neoplasia.
A: White-light imaging of the lesion (reversed view); B: Magnifying endoscopy with narrow-band imaging of the lesion (weak magnification); C: Magnifying endoscopy with narrow-band imaging of the lesion (strong magnification); D: After ablation, the surface of the lesions showed white coagulation and necrosis; E: Radiofrequency ablation for the same area was repeated three times; F: After scraping off the necrotic mucosal tissue on the surface.
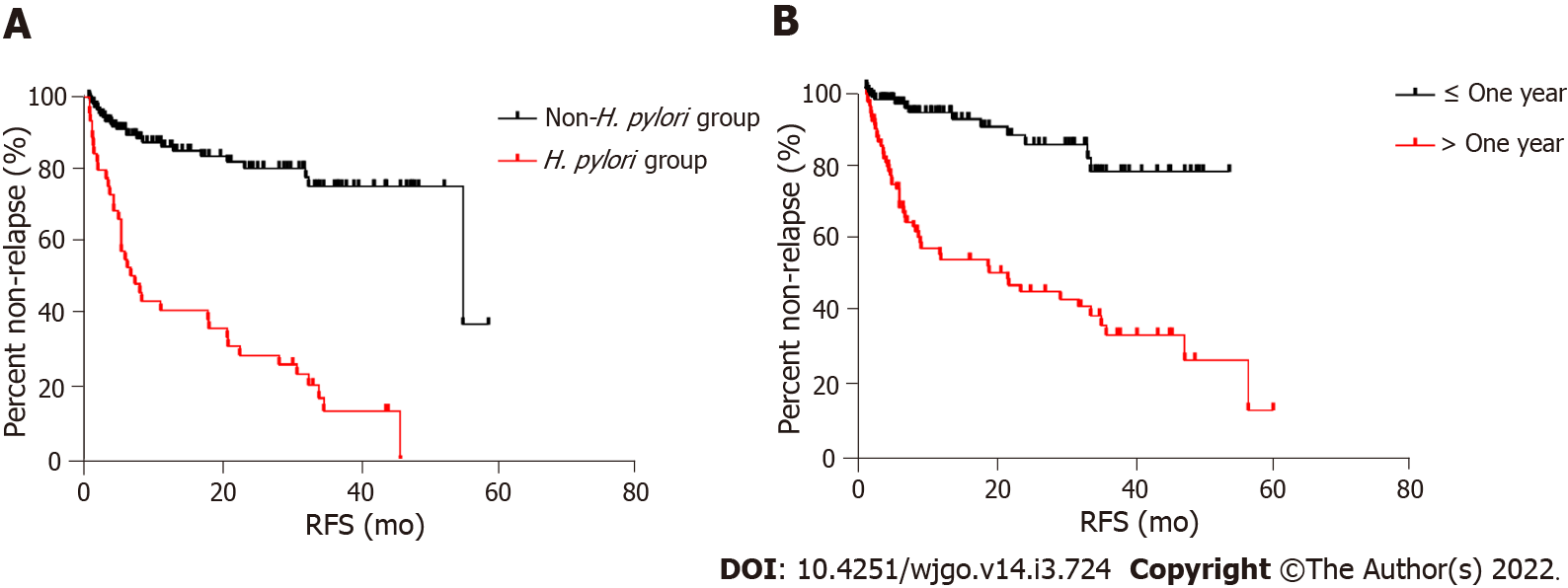
Figure 3 Relapse-free survival curves.
A: Non-Helicobacter pylori (H. pylori) infection vs H. pylori infection (P < 0.001); B: Disease course less than 1 year vs disease course over 1 year (P = 0.013). RFS: Relapse-free survival.
- Citation: Wang NJ, Chai NL, Tang XW, Li LS, Zhang WG, Linghu EQ. Clinical efficacy and prognostic risk factors of endoscopic radiofrequency ablation for gastric low-grade intraepithelial neoplasia. World J Gastrointest Oncol 2022; 14(3): 724-733
- URL: https://www.wjgnet.com/1948-5204/full/v14/i3/724.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i3.724