Published online Sep 16, 2013. doi: 10.4253/wjge.v5.i9.446
Revised: July 18, 2013
Accepted: August 4, 2013
Published online: September 16, 2013
Processing time: 112 Days and 13.2 Hours
SJ is a 37-year-old male who presented with one year history of dysphagia, odynophagia and 15 pounds weight loss. He underwent endoscopic evaluation which showed mid esophageal ulcers. It was thought that the cause of the ulcer was the multivitamins and the patient was asked to stop them. Furthermore Esomeprazole therapy was also initiated. Patient’s symptoms persisted but he did not seek any medical attention until about one year later. Meanwhile the patient reported additional 15 pounds of weight loss. We repeated upper endoscopy again which showed evidence of two chronic non bleeding irregular friable ulcerations seen in the mid esophagus, 31 cm from the incisors. Biopsies and frozen section were taken and sent for assessment to the Pathology lab. Immunoperoxidase studies on frozen sections showed the presence of IgM and for most plasma cells IgG. The microscopic and histologic findings were consistent with mucous associated lymphoid tissue lymphoma with plasmocytic differentiation. Computed tomographic scan done showed no evidence of spread to adjacent structures. The patient was referred to oncology and several cycles of radiation and Rituximab therapy were initiated which cured the disease. Subsequent endoscopies with blind biopsies were done which were negative for any neoplastic process.
Core tip: This is a case of a 37-year-old gentleman presenting with chronic esophageal ulcers. Endoscopic biopsy samples were taken. Immunohistochemistry and hematoxylin and eosin staining of the biopsy samples were consistent with mucous associated lymphoid tissue (MALT) lymphoma. There was no sign of disease process in the stomach, and radiological studies revealed no evidence of metastasis. In consideration of these findings a diagnosis of primary esophageal MALT lymphoma was made, which is an extremely rare occurrence. On the basis of our experiences we recommend keeping primary esophageal MALT lymphoma in the differential diagnosis of chronic esophageal ulcers that are resistant to conservative management.
- Citation: Malik AO, Baig Z, Ahmed A, Qureshi N, Malik FN. Extremely rare case of primary esophageal mucous associated lymphoid tissue lymphoma. World J Gastrointest Endosc 2013; 5(9): 446-449
- URL: https://www.wjgnet.com/1948-5190/full/v5/i9/446.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i9.446
We present a very rare case of primary esophageal B cell mucous associated lymphoid tissue (MALT) lymphoma. Gastrointestinal (GI) lymphoma is an uncommon disease but is the most frequently occurring extra nodal lymphoma and is almost exclusively Non-Hodgkin’s type[1]. Esophageal lymphomas occur most often secondary to cervical and mediastinal lymph node invasion or contiguous spread from gastric lymphoma[1]. Primary esophageal lymphomas is a very rare condition accounting for less than one percent of GI lymphomas, with B cell lymphomas being the most common histological subtype[2]. The predominant presentation is that of sub mucosal infiltration but the tumor can also manifest as a polyploidy mass into the lumen, ulceration or nodularity[3].
We report a very rare case of primary esophageal MALT lymphoma in a middle aged patient.
The patient is a 37-year-old Indian gentleman, who presented with complains of difficulty swallowing, which started about a year ago. Shortly thereafter he started experiencing pain with swallowing as well. He was treated for three months with Esomeprazole and had resolution of his symptoms. However his symptoms recurred 6 mo later. An endoscopy was performed, and biopsies were taken. These slides were sent to be reviewed by pathology which indicated focally dense lymphoplasmacytic infiltrate with Kappa light chain excess, most consistent with a B cell MALT lymphoma with plasmocytic differentiation.
Previous medical history was significant for hypertension and recurrent bouts of sinusitis. Surgical history was significant for endoscopic surgery for sinusitis and appendectomy done several years ago. The patient had recently travelled to Pakistan, and denied any substance abuse. Medications included nifedipine (calcium channel blocker) and Losartan (angiotensin receptor blocker) for hypertension. Furthermore the patient’s father had died from Non-Hodgkin’s lymphoma of unknown histologic subtype. The rest of his immediate family members were alive and healthy.
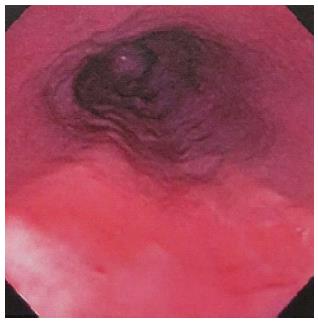
The endoscopy showed two superficial serpingious friable chronic ulcers visualized 31 cm and 33 cm from the incisors, and measuring 1.2 cm and 1.5 cm respectively. Multiple core biopsies were taken from the affected region. The two ulcers seemed to be merged together with evidence of cicatrix formation between them. The gastro esophageal junction was at the level of 40 cm from the gums. The stomach, pylorus and the duodenum appeared to be normal. The endoscopic photograph of the ulcers is shown in Figure 1.
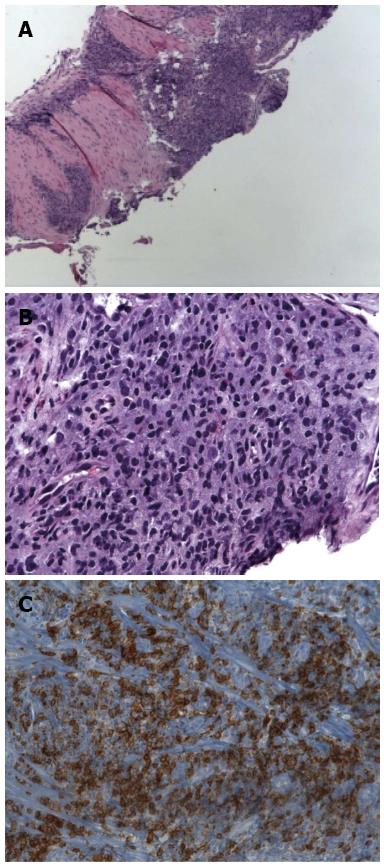
Hematoxylin and eosin (HE) staining of the cold biopsies, showed fragments of squamous epithelium with separate fragments of ulcer bed including acute and chronic inflammation with associated markedly atypical lymphoid infiltration. These findings were concerning for underlying lymphoma with superimposed ulcer bed. Photographs from the HE, and immunohistochemistry staining, of the biopsy samples are shown in Figure 2.
Additional immunoperoxidase staining showed small aggregates of CD20 positive cells and a small number of CD3 positive cells within the nodules. Stains for immunoglobulin kappa and lambda light chains showed only very rare plasma cells positive for lambda, with the majority being positive for kappa. These microscopic and histological finding were most consistent with MALT lymphoma with plasmocytic differentiation.
A bone marrow biopsy and flowcytometry were also done, which were negative for any disease process.
Computed tomography (CT) scan showed mild thickening of the mid esophagus, most likely suggestive of a neoplasm. Except for an incidental finding of an 8 mm parenchymal density within the posteromedial right lung base, there were no other positive findings. A thoracic esophagram was also performed which showed adequate primary contractions observed fluoroscopically. The contrast was noted to flow freely into the stomach.
An endoscopic ultrasound was also done which showed diffuse obliteration of normal echo architecture of esophageal layers 1-3. No mediastinal, celiac axis or peripancreatic lymphadenopathy was observed.
The endoscopic findings were suggestive of esophageal ulcers with possible eosinophilic esophagitis. However Immunohistochemistry staining of the biopsy samples confirmed the diagnosis of MALT lymphoma and excluded eosinophilic esophagitis from the list of differentials. As there was no evidence of disease in the stomach on endoscopy, and in consideration of immunohistochemistry and HE staining a diagnosis of Primary Esophageal MALT lymphoma was made. EUS findings were in contrast to the usual presentation of esophageal lymphoma, that is a hypo echoic lesion[4]. A possible reason for this could be that the MALT lymphoma was diagnosed at an early stage.
On the basis of radiological, bone marrow biopsy and microscopic findings the tumor was staged as 1A. The patient received a 4 cycles of 36 Gy external beam radiotherapy. After radiation therapy the he received four doses of Rituximab, as consolidative treatment.
After the treatment complete remission was achieved. The patient is seen at our institute regularly. Follow up endoscopies every 6 mo over last three years with targeted biopsies at the site of previous ulcers as evidenced by cicatrix formation have been negative.
Lymphoid tissue neoplasms compromise a diverse yet closely related group of neoplasms, including hodgkin’s lymphoma, non-hodgkin’s lymphoma, multiple myeloma, MALT lymphomas and several other types.[5] MALT lymphomas can arise in various anatomic locations where lymphocytes are usually absent due to acquisition of MALT, including the gut, lung, thyroid, salivary glands and liver[6]. Primary esophageal lymphoma is extremely rare[7]. Esophageal involvement by lymphoma is usually secondary to local spread from the stomach or the mediastinum[8]. Very few cases of primary esophageal lymphomas were reported in literature[6-11]. There are many morphological variants with most of the common being large B cell type and Non-Hodgkin’s lymphoma[9]. We report a case of primary esophageal B cell MALT lymphoma in an immune competent patient. Only a few other cases of this particular morphological type of primary esophageal lymphoma have been reported in literature[7,12].
Patients with acquired immunodeficiency syndrome (AIDS) are at an increased risk of developing malignant lymphomas, with the gastro intestinal tract being the most common site[13]. Chronic immunosuppression has also been suggested to be linked with the development of primary esophageal lymphomas[10]. MALT lymphomas of the stomach have closely been linked to Helicobacter Pylori infection, however no such relationship has been proven for primary esophageal MALT lymphoma[14].
Esophageal cancer generally presents with symptoms of dysphagia and weight loss[15]. There has been a trend of increased incidence of esophageal cancers in population less than 55 years[15]. In the case that we report the patient presented with classical sign and symptoms but the rare nature of the histological classification of the disease made the diagnosis difficult to make.
In summation this case illustrates an instance of biopsy proven primary esophageal MALT lymphoma in a 37 years old man, with history of dysphagia, odynophagia and weight loss. The malignancy presented as persistent ulcers seen in mid esophagus, 31 cm from the incisors. Radiographic studies including CT scanning done at the time revealed localized disease without any spread to surrounding structures. The patient was referred to oncology where he received several cycles of radiation therapy. On subsequent follow ups the patient was found to be cured of the disease with normal endoscopic findings. Blind biopsy samples were taken from the esophagus which proved to be negative for any neoplastic process.
On the basis of our experience we suggest MALT lymphoma in the differential diagnosis of chronic esophageal ulcers that are resistant to conservative therapy.
P- Reviewers Imagawa A, Rajeshwari K, Wasko-Czopnik D S- Editor Wen LL L- Editor A E- Editor Wang CH
| 1. | Ghai S, Pattison J, Ghai S, O’Malley ME, Khalili K, Stephens M. Primary gastrointestinal lymphoma: spectrum of imaging findings with pathologic correlation. Radiographics. 2007;27:1371-1388. [PubMed] |
| 2. | Miyazaki T, Kato H, Masuda N, Nakajima M, Manda R, Fukuchi M, Tsukada K, Kojima M, Nakajima T, Kuwano H. Mucosa-associated lymphoid tissue lymphoma of the esophagus: case report and review of the literature. Hepatogastroenterology. 2004;51:750-753. [PubMed] |
| 3. | Carnovale RL, Goldstein HM, Zornoza J, Dodd GD. Radiologic manifestations of esophageal lymphoma. AJR Am J Roentgenol. 1977;128:751-754. [PubMed] |
| 4. | Ogura T, Tajika M, Hijioka S, Hara K, Haba S, Hosoda W, Yatabe Y, Asano S, Higuchi K, Yamao K. First report of a mucosa-associated lymphoid tissue (MALT) lymphoma of the esophagus diagnosed by endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA). Endoscopy. 2012;44 Suppl 2 UCTN:E167-E168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107:265-276. [PubMed] |
| 6. | Chung JJ, Kim MJ, Kie JH, Kim KW. Mucosa-associated lymphoid tissue lymphoma of the esophagus coexistent with bronchus-associated lymphoid tissue lymphoma of the lung. Yonsei Med J. 2005;46:562-566. [PubMed] |
| 7. | Hosaka S, Nakamura N, Akamatsu T, Fujisawa T, Ogiwara Y, Kiyosawa K, Hidaka E, Ota H, Katsuyama T, Inagaki H. A case of primary low grade mucosa associated lymphoid tissue (MALT) lymphoma of the oesophagus. Gut. 2002;51:281-284. [PubMed] |
| 8. | Chadha KS, Hernandez-Ilizaliturri FJ, Javle M. Primary esophageal lymphoma: case series and review of the literature. Dig Dis Sci. 2006;51:77-83. [PubMed] |
| 9. | Ghimire P, Wu GY, Zhu L. Primary esophageal lymphoma in immunocompetent patients: Two case reports and literature review. World J Radiol. 2010;2:334-338. [PubMed] |
| 10. | Golioto M, McGrath K. Primary lymphoma of the esophagus in a chronically immunosuppressed patient with hepatitis C infection: case report and review of the literature. Am J Med Sci. 2001;321:203-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Gupta NM, Goenka MK, Jindal A, Behera A, Vaiphei K. Primary lymphoma of the esophagus. J Clin Gastroenterol. 1996;23:203-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Shim CS, Lee JS, Kim JO, Cho JY, Lee MS, Jin SY, Youm W. A case of primary esophageal B-cell lymphoma of MALT type, presenting as a submucosal tumor. J Korean Med Sci. 2003;18:120-124. [PubMed] |
| 13. | Sabaté JM, Franquet T, Palmer J, Monill JM. AIDS-related primary esophageal lymphoma. Abdom Imaging. 1997;22:11-13. [PubMed] |
| 14. | Wotherspoon AC, Doglioni C, Diss TC, Pan L, Moschini A, de Boni M, Isaacson PG. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet. 1993;342:575-577. [PubMed] |
| 15. | McLarty AJ, Deschamps C, Trastek VF, Allen MS, Pairolero PC, Harmsen WS. Esophageal resection for cancer of the esophagus: long-term function and quality of life. Ann Thorac Surg. 1997;63:1568-1572. [PubMed] |