Copyright
©The Author(s) 2023.
World J Stem Cells. Apr 26, 2023; 15(4): 150-164
Published online Apr 26, 2023. doi: 10.4252/wjsc.v15.i4.150
Published online Apr 26, 2023. doi: 10.4252/wjsc.v15.i4.150
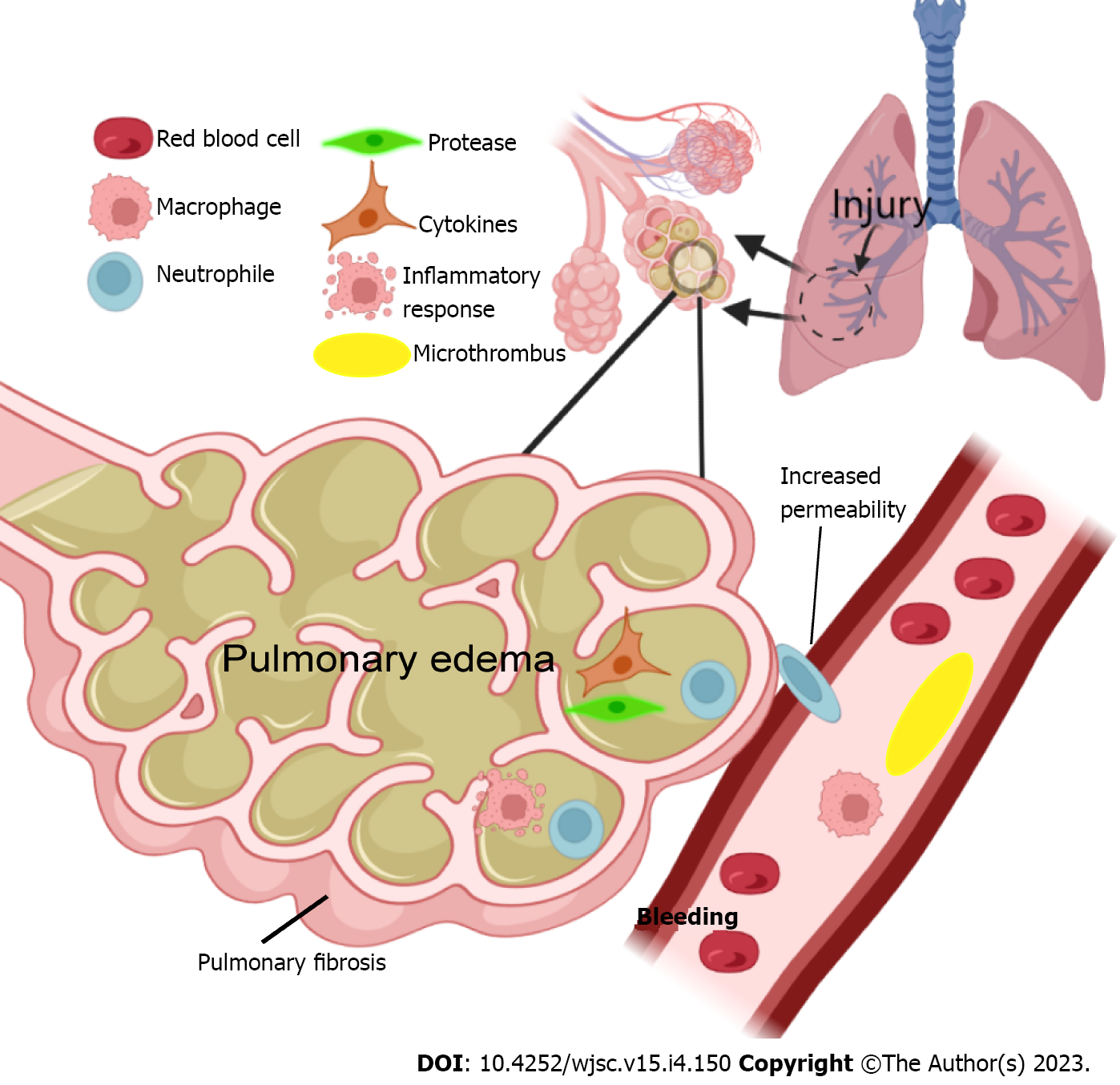
Figure 1 Following acute lung injury, pulmonary vascular macrophages produce chemokines to increase vascular permeability, resulting in neutrophil aggregation.
Neutrophils reach the pulmonary interstitium and alveolar space and release proteases, cytokines, and other harmful substances to destroy the alveolar microstructure, leading to cell dysfunction and eventually causing exudates and lung fluid to enter the alveolar space, resulting in the development of pulmonary fibrosis. Additionally, the disorder of pulmonary vascular coagulation and fibrinolysis caused by inflammation leads to pulmonary vascular microthrombosis, which is also one of the causes of pulmonary edema.
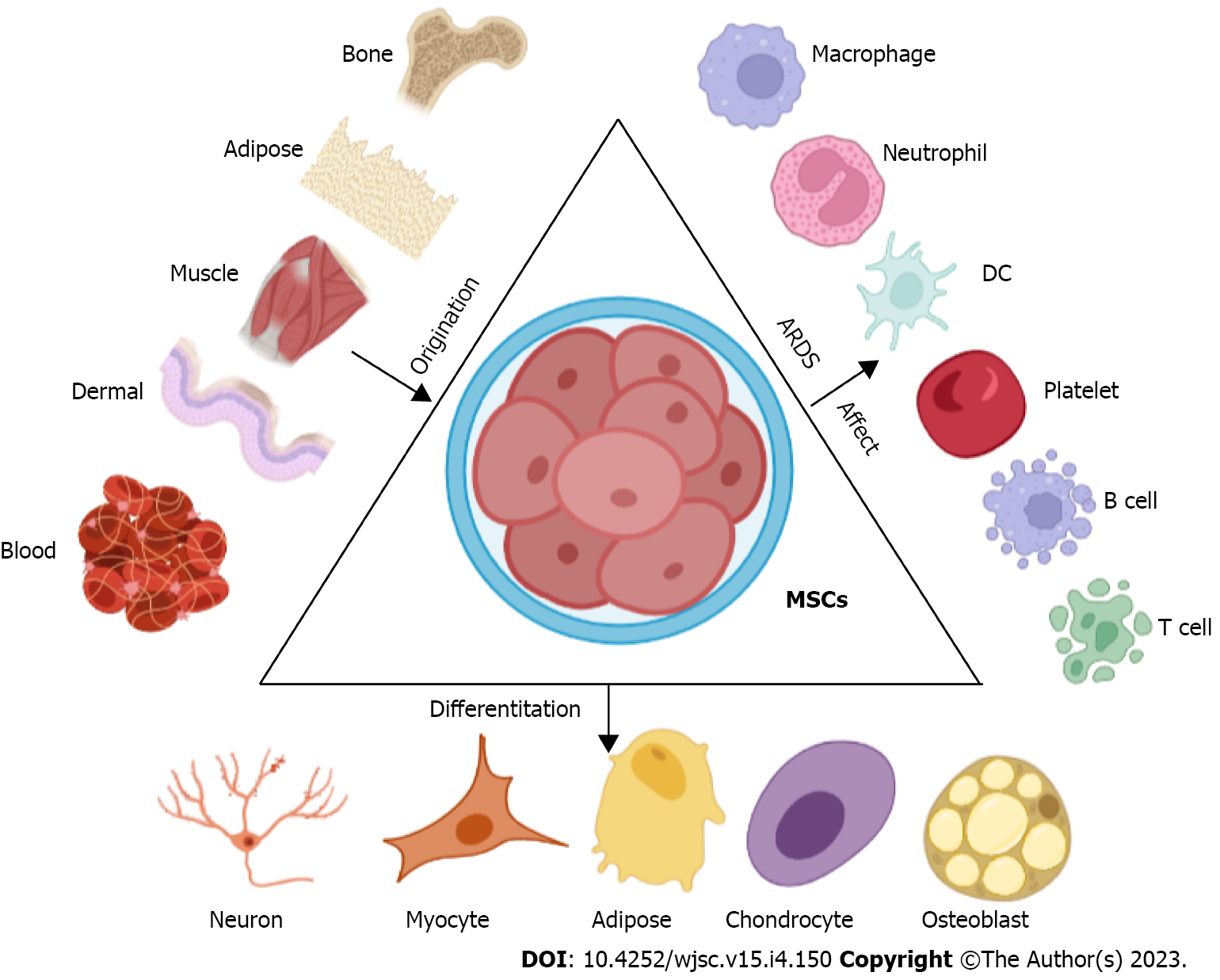
Figure 2 Mesenchymal stem cells can be derived from a variety of cell types and can differentiate into different types of cells to play specific roles.
In the pathological process of acute respiratory distress syndrome, mesenchymal stem cells can act on a variety of cells to play a protective role. MSC: Mesenchymal stem cell; DC: Dendritic cell.
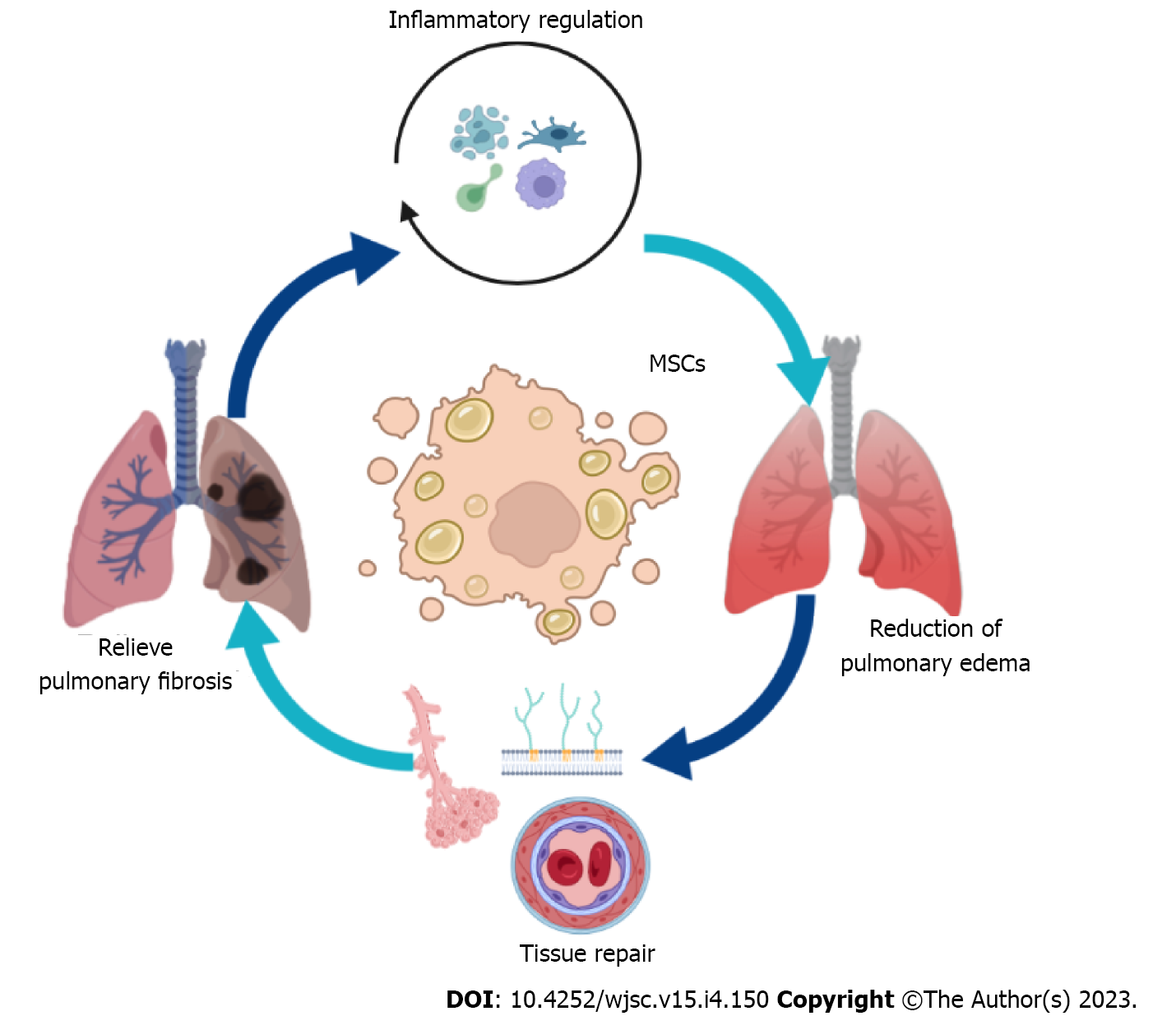
Figure 3 The main mechanism of mesenchymal stem cell therapy for acute respiratory distress syndrome.
Mesenchymal stem cell can treat acute respiratory distress syndrome by regulating inflammatory response, reducing pulmonary edema, alleviating pulmonary fibrosis, and promoting tissue repair. MSC: Mesenchymal stem cell.
- Citation: Liang TY, Lu LH, Tang SY, Zheng ZH, Shi K, Liu JQ. Current status and prospects of basic research and clinical application of mesenchymal stem cells in acute respiratory distress syndrome. World J Stem Cells 2023; 15(4): 150-164
- URL: https://www.wjgnet.com/1948-0210/full/v15/i4/150.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v15.i4.150