Copyright
©The Author(s) 2021.
World J Stem Cells. Jul 26, 2021; 13(7): 841-860
Published online Jul 26, 2021. doi: 10.4252/wjsc.v13.i7.841
Published online Jul 26, 2021. doi: 10.4252/wjsc.v13.i7.841
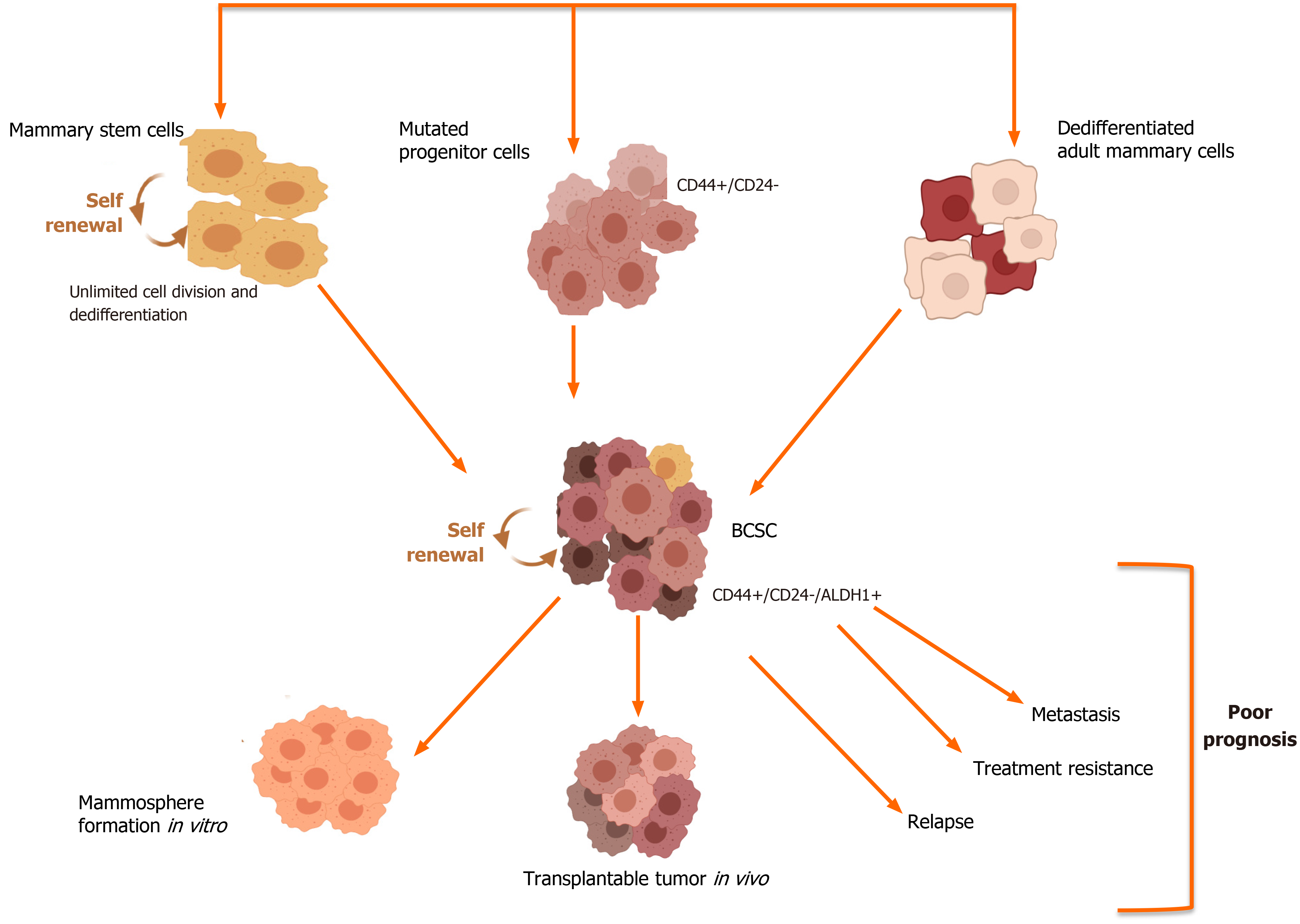
Figure 1 Breast cancer stem cells: Origin and outcome.
Breast cancer stem cells (BCSCs) can arise from normal mammary stem cells which have undergone mutations or from mutated progenitor cells or dedifferentiated cells, which comprise the mammary tissue. The subpopulation of BCSCs can be identified based on the altered expression of cell surface markers such as CD44 and CD24 as well as higher activity of the enzyme aldehyde dehydrogenase (ALDH1). These BCSCs when transplanted in SCID/nude mice have the ability to form mammospheres, which are three-dimensional spheres generated through the clonal expansion of single cancer stem cells. These cancerous stem cells have been implicated in the poor outcomes associated with aggressive breast cancer subtypes.
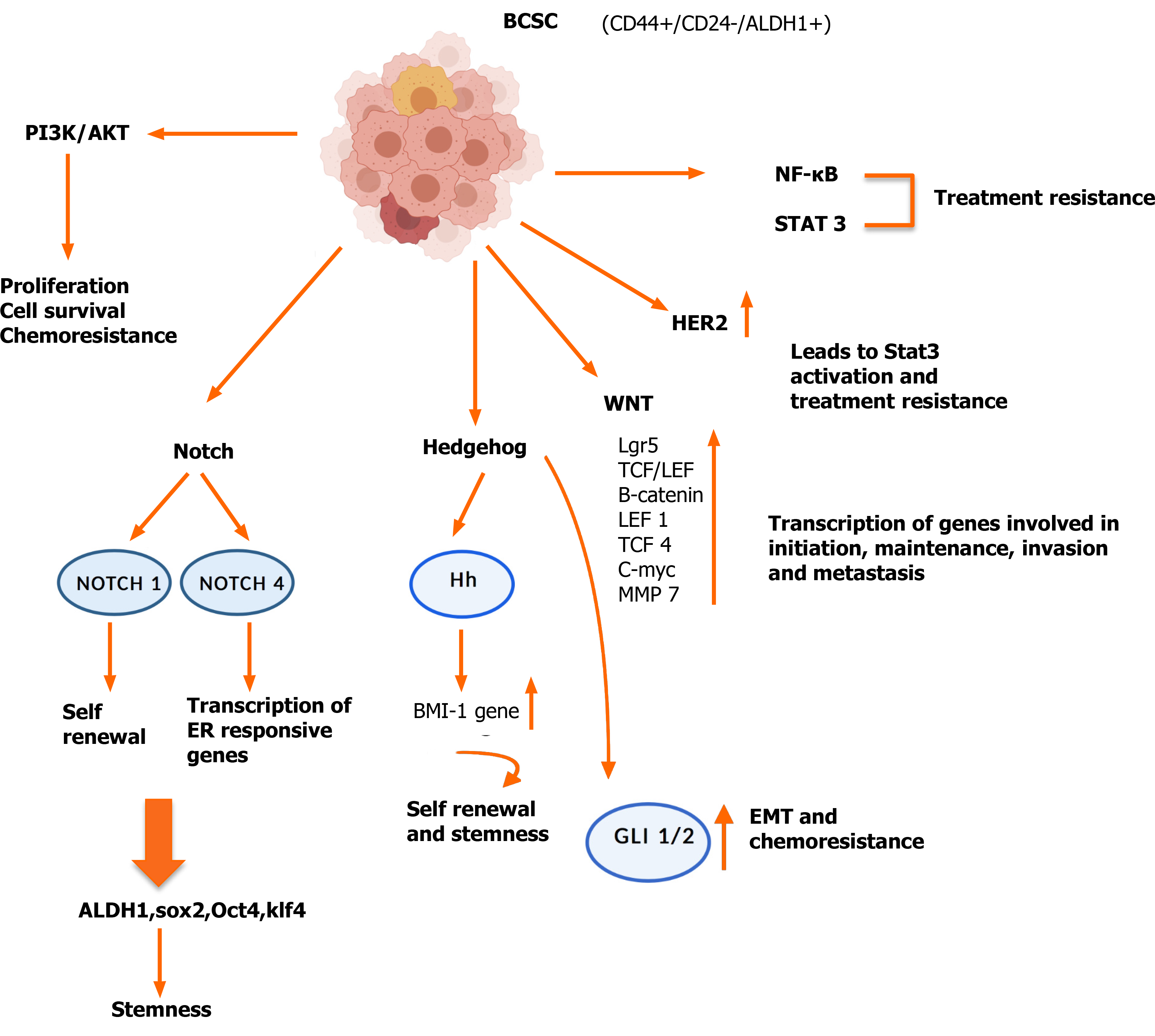
Figure 2 Dysregulated pathways operative in breast cancer stem cells.
A number of pathways have been shown to be upregulated in breast cancer stem cells, which are due to mutations, resulting in amplification or loss of key effector genes. The gene products of the aberrant pathways impart a growth and survival advantage and allow these cells to metastasize and become resistant to conventional therapy. BCSC: Breast cancer stem cell; NF-κB: Nuclear factor kappa beta; PI3K: Phosphatidylinositol 3-kinase; ER: Estrogen receptor; EMT: Epithelial mesenchymal transitions; HER2: Epidermal growth factor receptor 2; ALDH1: Aldehyde dehydrogenase; Hh: Hedgehog.
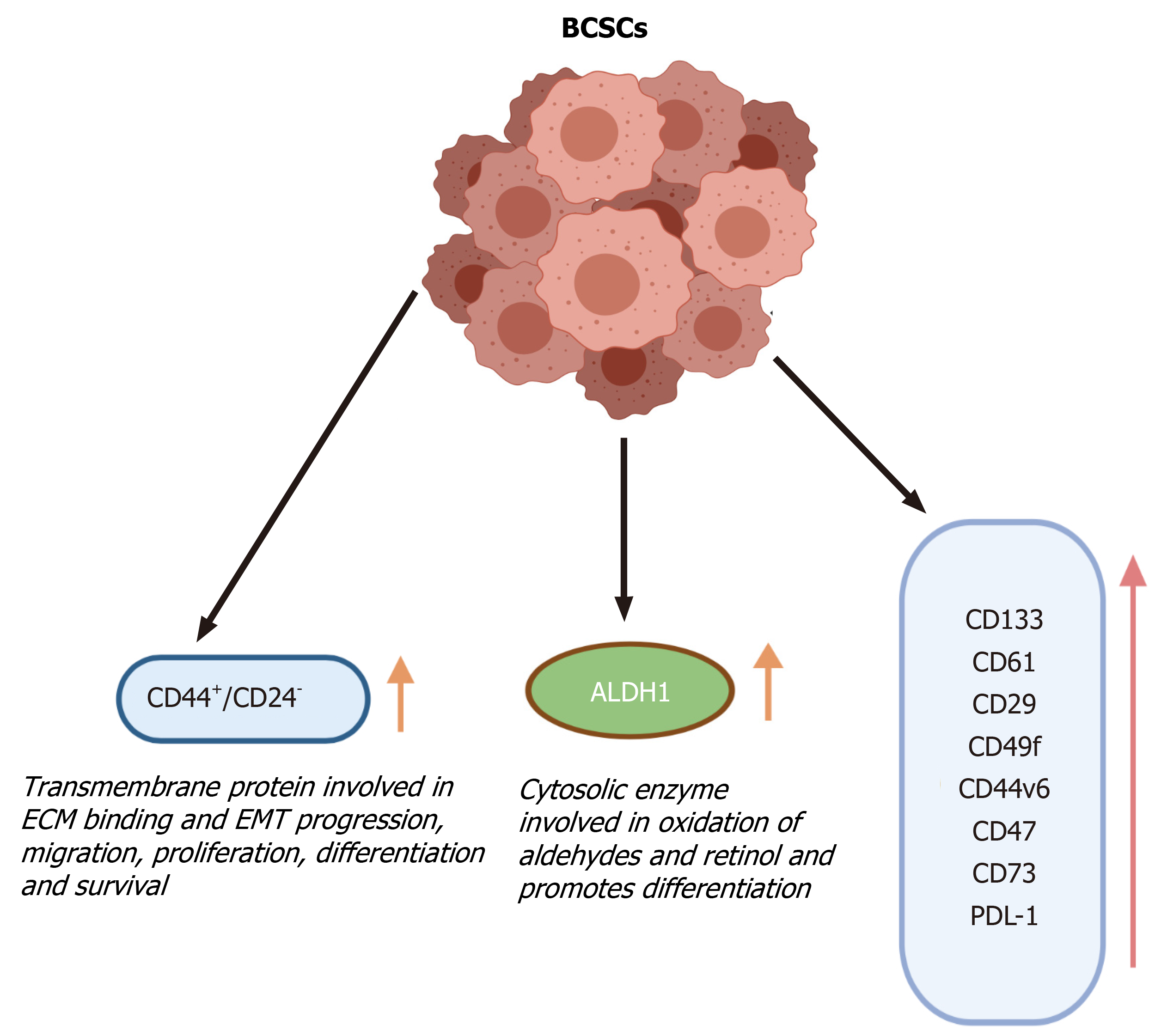
Figure 3 Breast cancer stem cell markers.
The breast cancer stem cells can be differentiated from cancer and normal cells based on the increased or altered expression of various cell surface markers. These marker proteins have various functions that are responsible for the development and survival of breast cancer stem cells and can be used to isolate the cancer stem cells from the bulk of the tumor. BCSCs: Breast cancer stem cells; ECM: Extracellular matrix; EMT: Epithelial mesenchymal transitions; ALDH: Aldehyde dehydrogenase.
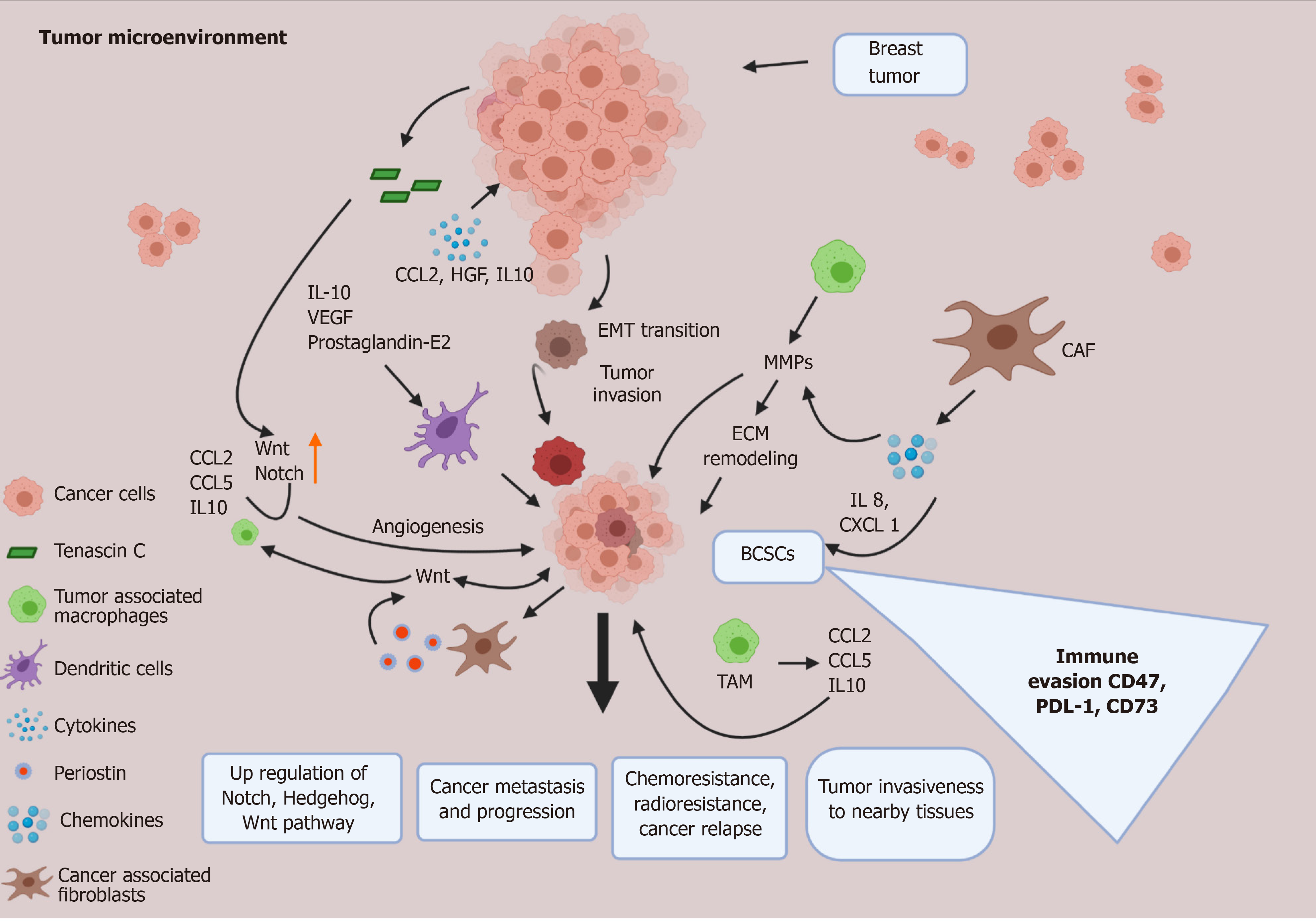
Figure 4 Tumor microenvironment and breast cancer stem cell crosstalk.
The tumor microenvironment (TME) plays a critical role in the development as well as the maintenance of breast cancer stem cells. Various signaling molecules secreted by the normal and transformed cells of the TME, such as cancer associated fibroblasts, M2 tumor associated macrophages, endothelial cells and other immune cells, act in a paracrine manner to influence the breast cancer stem cells, which in turn use a positive feedback system to sustain the cells of the TME. In this way the TME and breast cancer stem cells work in a concerted manner to support stemness, chemoresistance, immune evasion and metastatic potential of breast cancer. CAF: Cancer associated fibroblasts; IL: Interleukin; VEGF: Vascular endothelial growth factor; EMT: Epithelial mesenchymal transitions; BCSCs: Breast cancer stem cells; TAM: M2 tumor associated macrophages; PD-L1: Programmed cell death-ligand 1; ECM: Extracellular matrix; HGF: Hepatocyte growth factor.
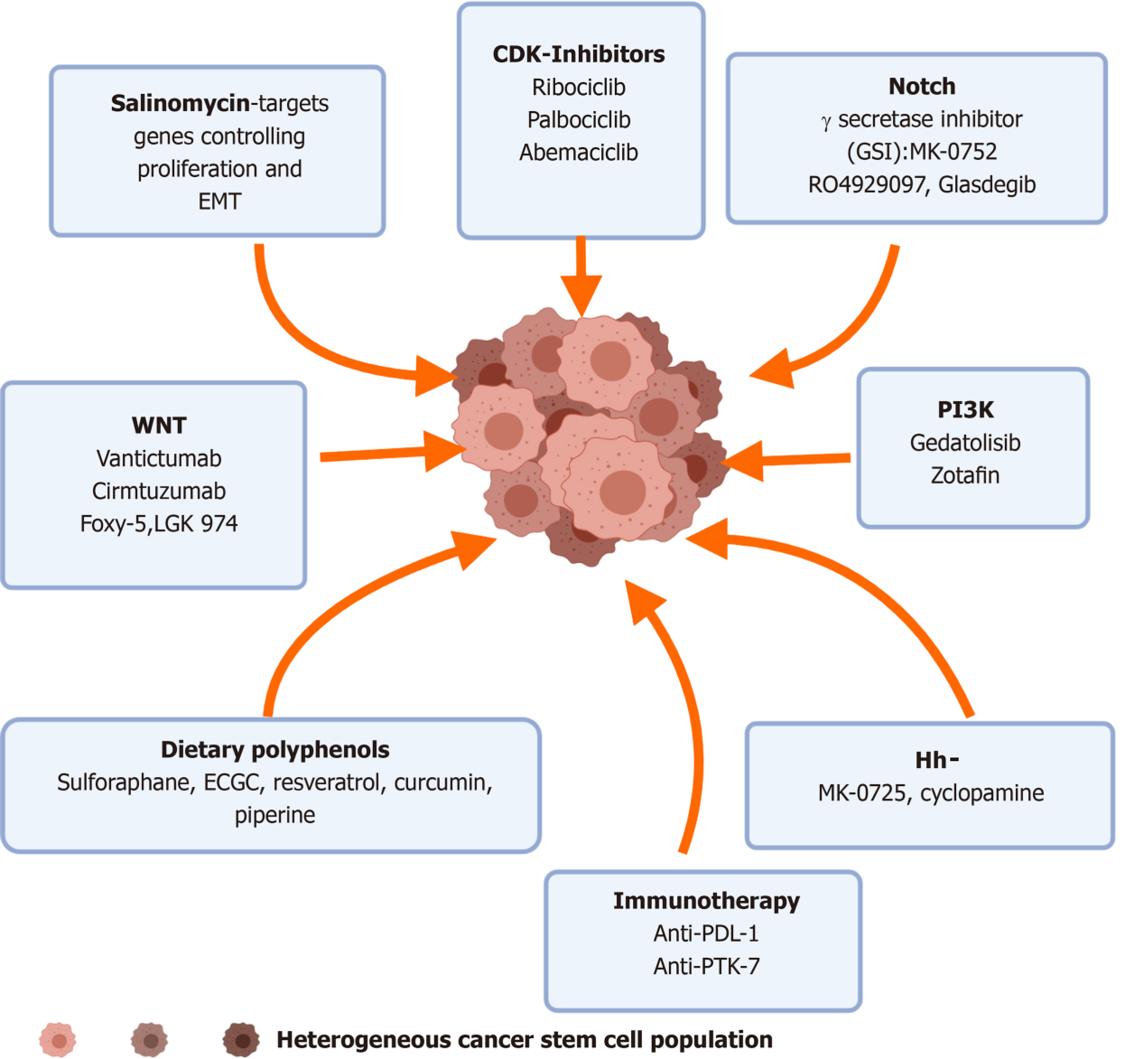
Figure 5 Pharmacological targeting of breast cancer stem cells.
Insights from preclinical and clinical studies have shown that various small molecular inhibitors and antibodies against the effectors of the aberrantly expressed pathways can be targeted to downregulate the stemness and altered phenotype of breast cancer stem cells. EMT: Epithelial mesenchymal transitions; CDK: Cyclin dependent kinase; GSI: γ-secretase inhibitors; PI3K: Phosphatidylinositol 3-kinase; PTK: Protein tyrosine kinase.
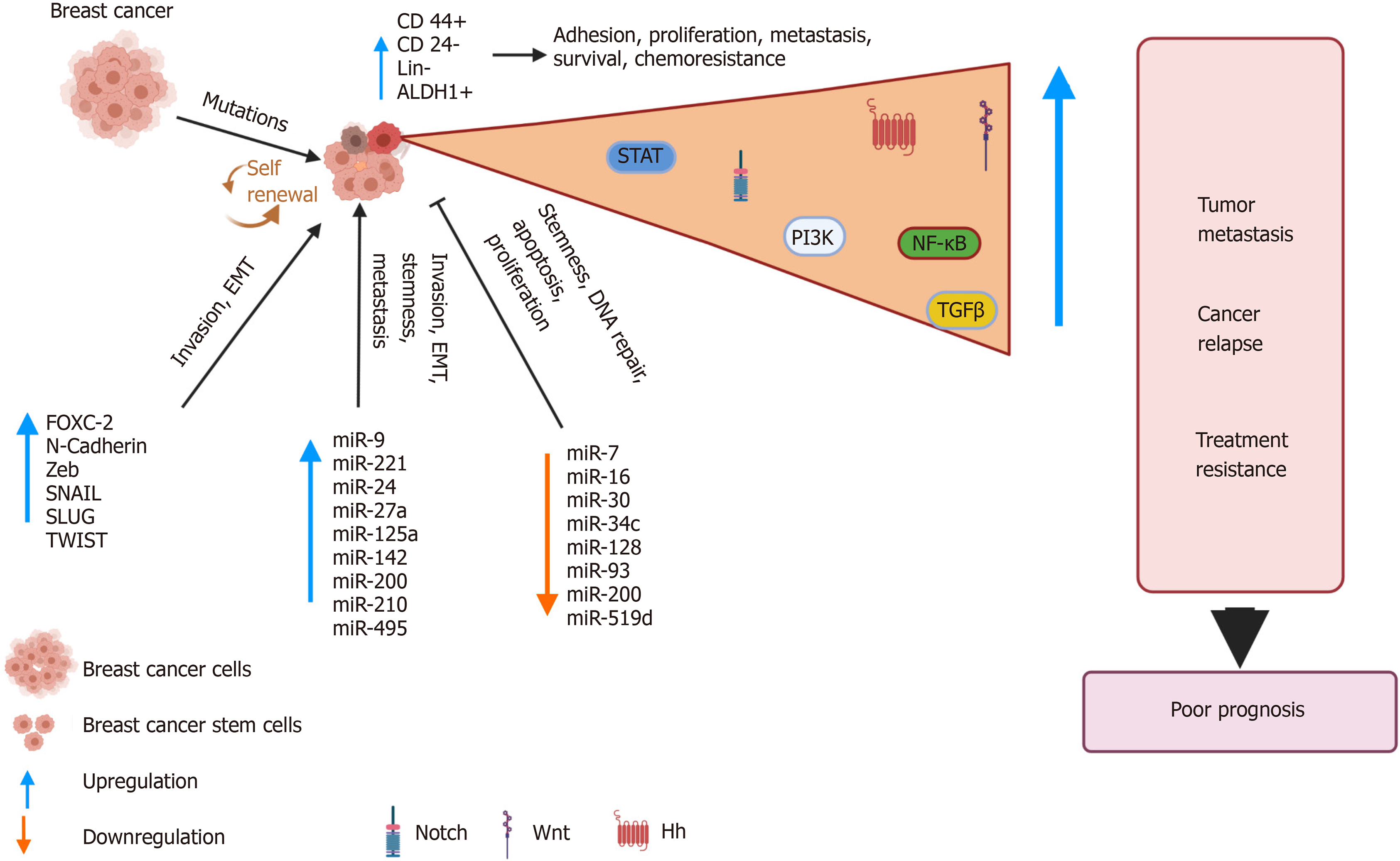
Figure 6 Breast cancer stem cells: drivers of tumorigenesis and cancer relapse.
Genomic instability due to inherent mutations or in response to treatment results in alterations in various pathways. This abnormal signaling drives the development of a distinct subpopulation of breast cancer stem cells (BCSCs), which display characteristic cell surface markers and express genes that allows unlimited self-renewal and differentiation abilities. The BCSCs also display altered microRNA profiles that are used by the BCSCs to invade, metastasize and acquire stemness features. The net result is the development of an aggressive, treatment resistant tumor, which results in relapse. BCSCs: Breast cancer stem cells; NF-κB: Nuclear factor kappa beta; PI3K: Phosphatidylinositol 3-kinase; TGFβ: Transforming growth factor beta; EMT: Epithelial mesenchymal transitions; Hh: Hedgehog; ALDH: Aldehyde dehydrogenase.
- Citation: Khan S, Suryavanshi M, Kaur J, Nayak D, Khurana A, Manchanda RK, Tandon C, Tandon S. Stem cell therapy: A paradigm shift in breast cancer treatment. World J Stem Cells 2021; 13(7): 841-860
- URL: https://www.wjgnet.com/1948-0210/full/v13/i7/841.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v13.i7.841